Pericapsular Nerve Group (PENG) Associated with Lateral Femoral Cutaneous Nerve (LFCN) Block Versus Fascia Iliaca Compartment Block (FICB) for Total Hip Replacement Surgery: Double-Blind Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
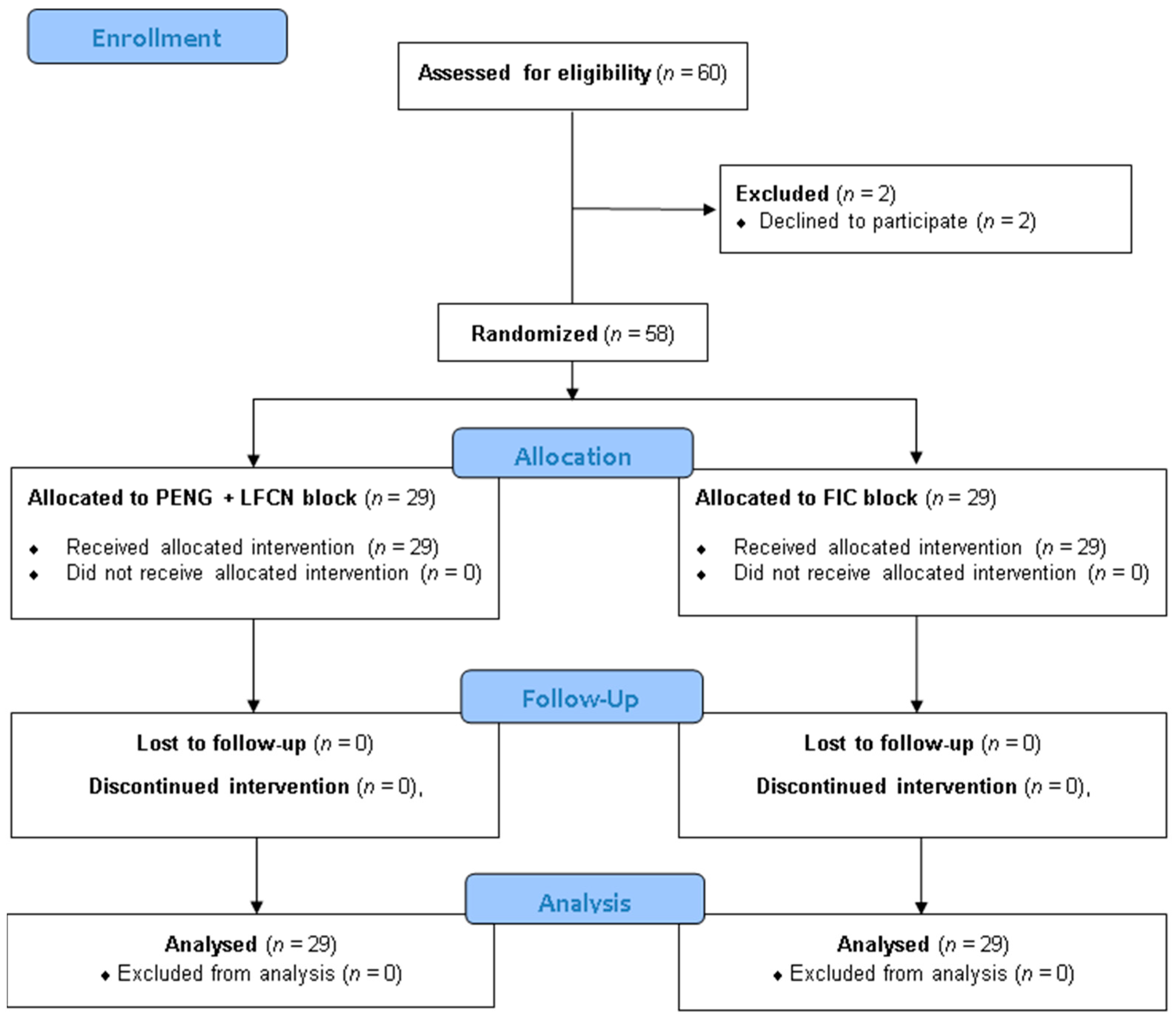
2.1. Randomization Process and Blinding Procedures
2.2. Anesthetic Protocol
2.3. Outcome Variables
2.4. Sample Size Estimation and Statistical Analysis
3. Results
3.1. Motor Function
3.2. Hip Flexion
3.3. Time to Ambulation
3.4. Pain Outcomes
3.5. Opioid Consumption and PONV
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| THA | Total hip arthroplasty |
| PENG | Pericapsular Nerve Group |
| LFCN | Lateral femoral cutaneous nerve |
| FICB | Fascia Iliaca Compartment Block |
| RCT | Randomized clinical trial |
| PROSPECT | Procedure-Specific Postoperative Pain Management |
| ICAROS | International Consensus on Anaesthesia-Related Outcomes after Surgery group |
| INR | International normalized ratio |
| aPTT | Activated partial thromboplastin time |
| ASA | American Society of Anesthesiologists |
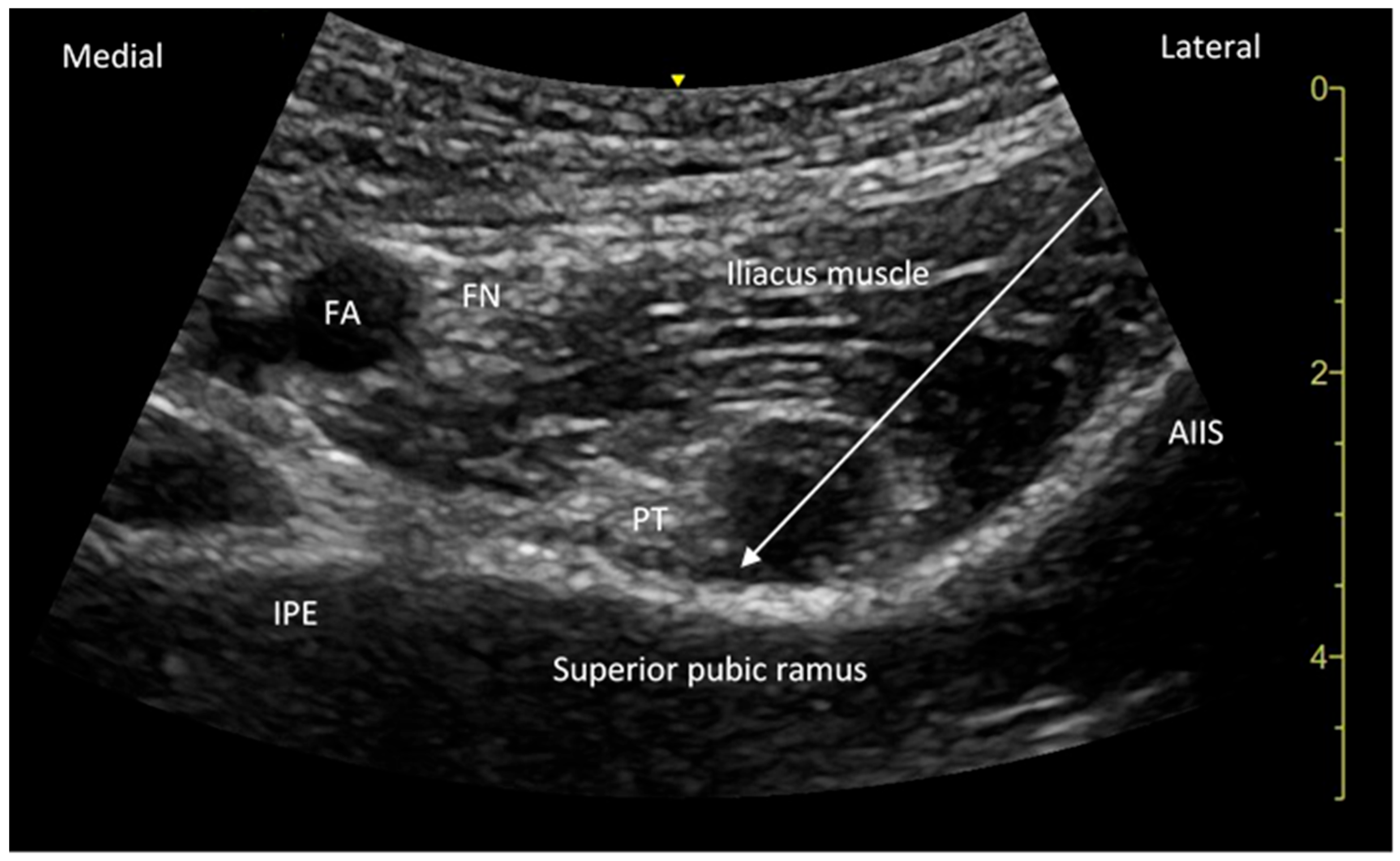
| AIIS | Anterior inferior iliac spine |
| IPE | Iliopubic eminence |
| FFFT | Fat-filled flat tunnel |
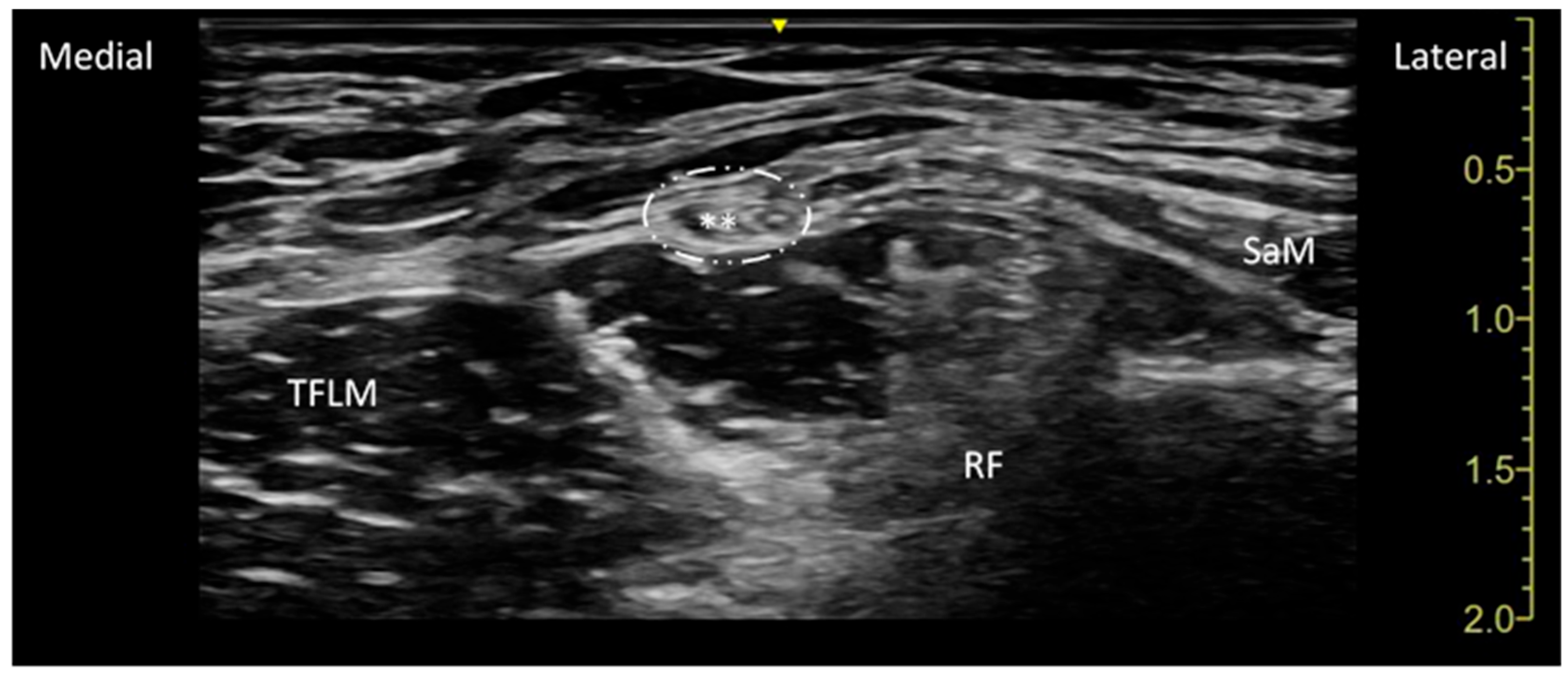
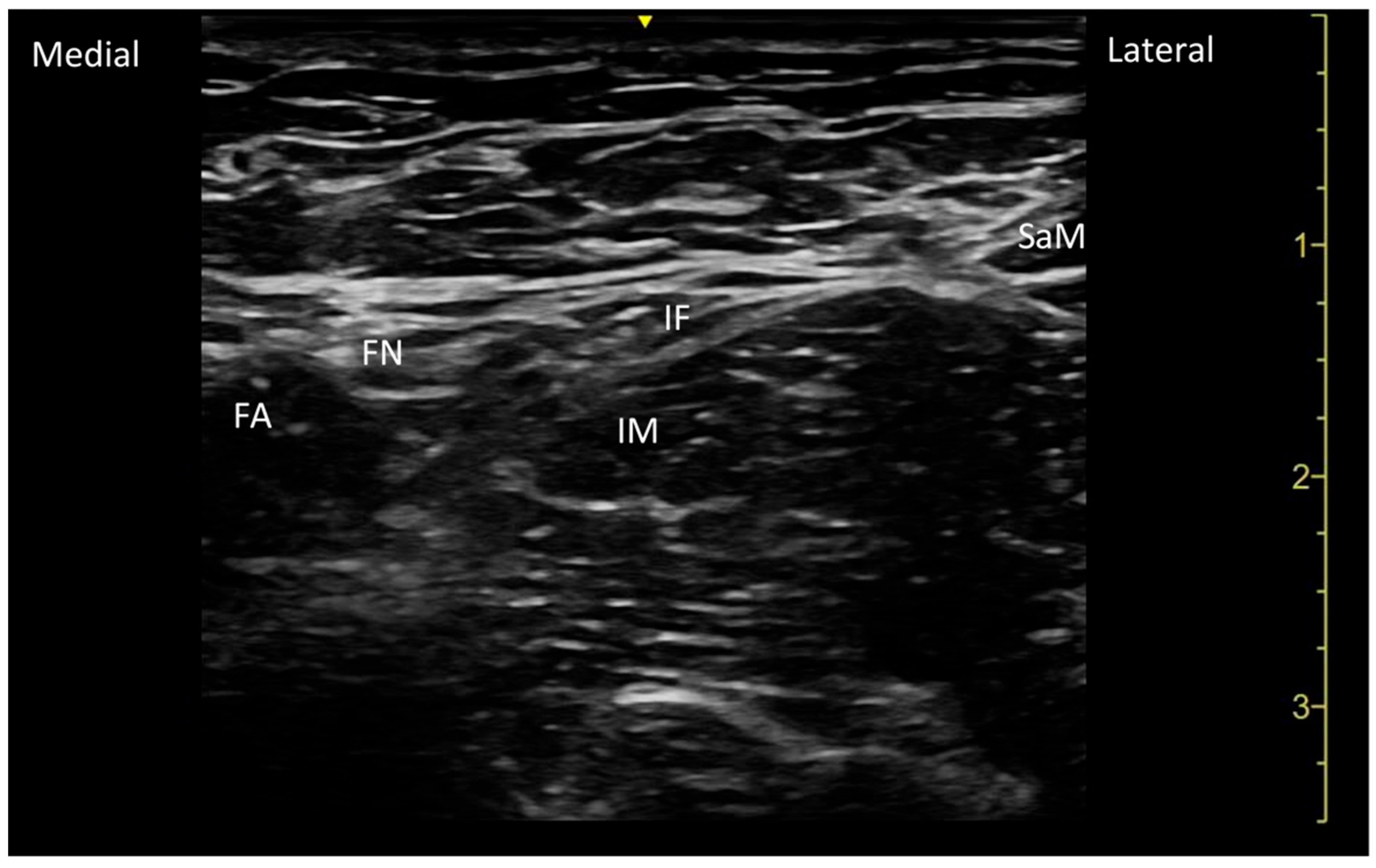
| SaM | Sartorius muscle |
| TFLM | Tensor fascia latae muscle |
| RF | Rectus Femoris Muscle. |
| MRC | Medical Research Council Scale for Muscle Strength |
| NRS | Numerical Rating Scale |
| ERAS | Early Recovery After Surgery |
| BMI | Body Mass Index |
| PRN | Pro Re Nata |
| MME | Morphine Milligram Equivalent |
| PONV | Postoperative nausea and vomiting |
| MCID | Minimal clinically important difference |
| VAS | Visual analog scale |
| DAA | Direct anterior approach |
References
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of Total Hip and Knee Replacement in the United States. J. Bone Jt. Surg.-Am. Vol. 2015, 97, 1386–1397. [Google Scholar] [CrossRef]
- Short, A.J.; Barnett, J.J.G.; Gofeld, M.; Baig, E.; Lam, K.; Agur, A.M.; Peng, P.W. Anatomic Study of Innervation of the Anterior Hip Capsule. Reg. Anesth. Pain Med. 2017, 43, 186–192. [Google Scholar] [CrossRef]
- Judge, A.; Arden, N.K.; Batra, R.N.; Thomas, G.; Beard, D.; Javaid, M.K.; Cooper, C.; Murray, D.; Exeter Primary Outcomes Study (EPOS) group. The association of patient characteristics and surgical variables on symptoms of pain and function over 5 years following primary hip-replacement surgery: A prospective cohort study. BMJ Open 2013, 3, e002453. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beswick, A.D.; Wylde, V.; Gooberman-Hill, R.; Blom, A.; Dieppe, P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012, 2, e000435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Richebé, P.; Capdevila, X.; Rivat, C. Persistent Postsurgical Pain: Pathophysiology and Preventative Pharmacologic Considerations. Anesthesiology 2018, 129, 590–607. [Google Scholar] [CrossRef] [PubMed]
- Aprisunadi; Nursalam, N.; Mustikasari, M.; Ifadah, E.; Hapsari, E.D. Effect of Early Mobilization on Hip and Lower Extremity Postoperative: A Literature Review. SAGE Open Nurs. 2023, 9, 23779608231167825. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhu, S.; Qian, W.; Jiang, C.; Ye, C.; Chen, X. Enhanced recovery after surgery for hip and knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2017, 93, 736–742. [Google Scholar] [CrossRef]
- Okamoto, T.; Ridley, R.J.; Edmondston, S.J.; Visser, M.; Headford, J.; Yates, P.J. Day-of-Surgery Mobilization Reduces the Length of Stay After Elective Hip Arthroplasty. J. Arthroplast. 2016, 31, 2227–2230. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J. Pain Res. 2017, 10, 2287–2298. [Google Scholar] [CrossRef]
- Ang, J.J.M.; Onggo, J.R.; Stokes, C.M.; Ambikaipalan, A. Comparing direct anterior approach versus posterior approach or lateral approach in total hip arthroplasty: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 2773–2792. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barrett, W.P.; Turner, S.E.; Murphy, J.A.; Flener, J.L.; Alton, T.B. Prospective, Randomized Study of Direct Anterior Approach vs Posterolateral Approach Total Hip Arthroplasty: A Concise 5-Year Follow-Up Evaluation. J. Arthroplast. 2019, 34, 1139–1142. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.W.; Zhang, L.; Chu, X.B.; Lv, S.J.; Zhang, J.J.; Tong, P.J.; Pan, Y. Comparison of clinical efficacy between direct anterior approach and posterolateral approach in primary total hip arthroplasty. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 5604–5613. [Google Scholar] [CrossRef] [PubMed]
- Fransen, B.; Hoozemans, M.; Vos, S. Direct anterior approach versus posterolateral approach in total hip arthroplasty: One surgeon, two approaches. Acta Orthop. Belg. 2016, 82, 240–248. [Google Scholar] [PubMed]
- Memtsoudis, S.G.; Cozowicz, C.; Bekeris, J.; Bekere, D.; Liu, J.; Soffin, E.M.; Mariano, E.R.; Johnson, R.L.; Hargett, M.J.; Lee, B.H.; et al. Anaesthetic care of patients undergoing primary hip and knee arthroplasty: Consensus recommendations from the International Consensus on Anaesthesia-Related Outcomes after Surgery group (ICAROS) based on a systematic review and meta-analysis. Br. J. Anaesth. 2019, 123, 269–287. [Google Scholar] [CrossRef]
- Anger, M.; Valovska, T.; Beloeil, H.; Lirk, P.; Joshi, G.P.; Van de Velde, M.; Raeder, J.; PROSPECT Working Group* and the European Society of Regional Anaesthesia and Pain Therapy. PROSPECT guideline for total hip arthroplasty: A systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2021, 76, 1082–1097. [Google Scholar] [CrossRef] [PubMed]
- Gasanova, I.; Alexander, J.C.; Estrera, K.; Wells, J.; Sunna, M.; Minhajuddin, A.; Joshi, G.P. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infltration for pain management after total hip arthroplasty: A randomized controlled trial. Reg. Anesth. Pain Med. 2019, 44, 206–211. [Google Scholar] [CrossRef]
- Eshag, M.M.E.; Hasan, L.O.M.; Elshenawy, S.; Ahmed, M.S.; Mostafa, A.E.-M.E.; Abdelghafar, Y.A.; Althawadi, Y.J.; Ibraheem, N.M.; Badr, H.; AbdelQadir, Y.H. Fascia iliaca compartment block for postoperative pain after total hip arthroplasty: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2024, 24, 95. [Google Scholar] [CrossRef]
- Ke, J.; Yang, Y.; Cao, Y.; Wang, Y.; Lin, C. Efficacy and safety of pericapsular nerve group block in total hip arthroplasty: A meta-analysis and systematic review. Minerva Anestesiol. 2024, 90, 200–209. [Google Scholar] [CrossRef] [PubMed]
- She, C.; Liu, H. The efficacy of pericapsular nerve group block for reducing pain and opioid consumption after total hip arthroplasty: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2024, 19, 229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zheng, J.; Du, L.; Chen, G.; Zhang, L.; Deng, X.; Zhang, W. Efficacy of pericapsular nerve group (PENG) block on perioperative pain management in elderly patients undergoing hip surgical procedures: A protocol for a systematic review with meta-analysis and trial sequential analysis. BMJ Open 2023, 13, e065304. [Google Scholar] [CrossRef]
- Farag, A.; Hendi, N.I.; Diab, R.A. Does pericapsular nerve group block have limited analgesia at the initial post-operative period? Systematic review and meta-analysis. J. Anesth. 2023, 37, 138–153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morrison, C.; Brown, B.; Lin, D.Y.; Jaarsma, R.; Kroon, H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: A scoping review. Reg. Anesth. Pain Med. 2021, 46, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.Y.; Brown, B.; Morrison, C.; Fraser, N.S.; Chooi, C.S.L.; Cehic, M.G.; McLeod, D.H.; Henningsen, M.D.; Sladojevic, N.; Kroon, H.M.; et al. The Pericapsular nerve group (PENG) block combined with local infltration analgesia (LIA) compared to placebo and LIA in hip arthroplasty surgery: A multi-center double-blinded randomized-controlled trial. BMC Anesthesiol. 2022, 22, 252. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Wang, Q.; Hu, J.; Kang, P.; Yang, J. Efficacy of Ultrasound-Guided Pericapsular Nerve Group (PENG) Block Combined with Local Infiltration Analgesia on Postoperative Pain after Total Hip Arthroplasty: A Prospective, Double-Blind, Randomized Controlled Trial. J. Arthroplast. 2023, 38, 1096–1103. [Google Scholar] [CrossRef]
- Bravo, D.; Aliste, J.; Layera, S.; Fernández, D.; Erpel, H.; Aguilera, G.; Arancibia, H.; Barrientos, C.; Wulf, R.; León, S. Randomized clinical trial comparing pericapsular nerve group (PENG) block and periarticular local anesthetic infiltration for total hip arthroplasty. Reg. Anesth. Pain Med. 2023, 48, 489–494. [Google Scholar] [CrossRef]
- Roy, R.; Agarwal, G.; Pradhan, C.; Kuanar, D. Total postoperative analgesia for hip surgeries, PENG block with LFCN block. Reg. Anesth. Pain Med. 2019, 44, 684.1. [Google Scholar] [CrossRef]
- Kim, D.H.; Hong, G.; Lin, E.; Kim, S.J.; Beathe, J.; Wetmore, D.; Liu, J. Combined Pericapsular Nerve Group Block and Intrapelvic Lateral Femoral Cutaneous Nerve Block Is Associated with Decreased Opioid Consumption After Hip Arthroscopy: A Retrospective Cohort Study. HSS J. 2024, 20, 530–538. [Google Scholar] [CrossRef]
- Gurbuz, H.; Okmen, K.; Gultekin, A. Postoperative pain management in patients with coxarthrosis undergoing total hip arthroplasty: PENG block combined with LFCN block or wound infiltration? Minerva Anestesiol. 2021, 87, 1154–1155. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Lee, M.J.; Beak, M.H.; Kim, W.J. Efficacy of Supplemental Ultrasound-Guided Pericapsular Nerve Group (PENG) Block Combined with Lateral Femoral Cutaneous Nerve Block in Patients Receiving Local Infiltration Analgesia after Hip Fracture Surgery: A Prospective Randomized Controlled Trial. Medicina 2024, 60, 315. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hopkins, P.M.; Ellis, F.R.; Halsall, P.J. Evaluation of local anesthetic blockade of the lateral femoral cutaneous nerve. Anaesthesia 1991, 46, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Corujo, A.; Franco, C.D.; Williams, J.M. The sensory territory of the lateral cutaneous nerve of the thigh as determined by anatomic dissections and ultrasound-guided blocks. Reg. Anesth. Pain Med. 2012, 37, 561–564. [Google Scholar] [CrossRef] [PubMed]
- Bergin, P.F.; Unger, A.S. Direct Anterior Total Hip Arthroplasty. JBJS Essent. Surg. Tech. 2011, 1, e15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Girombelli, A.; Vetrone, F.; Saglietti, F.; Galimberti, A.; Fusaro, A.; Umbrello, M.; Pezzi, A. Pericapsular nerve group block and lateral femoral cutaneous nerve block versus fascia iliaca block for multimodal analgesia after total hip replacement surgery: A retrospective analysis. Saudi J. Anaesth. 2024, 18, 218–223. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vetrone, F.; Saglietti, F.; Galimberti, A.; Pezzi, A.; Umbrello, M.; Cuttone, G.; La Via, L.; Vetrugno, L.; Deana, C.; Girombelli, A. Pericapsular Nerve Group Block Plus Lateral Femoral Cutaneous Nerve Block vs. Fascia Iliaca Compartment Block in Hip Replacement Surgery. J. Clin. Med. 2025, 14, 984. [Google Scholar] [CrossRef]
- Hopewell, S.; Chan, A.W.; Collins, G.S.; Hróbjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, R.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. CONSORT 2025 statement: Updated guideline for reporting randomised trials. BMJ 2025, 389, e081123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, B.; Rao, S.; Mekkawy, K.L.; Rahman, R.; Sarfraz, A.; Hollifield, L.; Runge, N.; Oni, J.K. Risk factors for pain after total hip arthroplasty: A systematic review. Arthroplasty 2023, 5, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain—United States, 2022. MMWR Recomm. Rep. 2022, 71, 1–95. [Google Scholar] [CrossRef] [PubMed]
- Gulotta, L.V.; Padgett, D.E.; Sculco, T.P.; Urban, M.; Lyman, S.; Nestor, B.J. Fast track THR: One hospital’s experience with a 2-day length of stay protocol for total hip replacement. HSS J. 2011, 7, 223–228. [Google Scholar] [CrossRef]
- Liang, L.; Zhang, C.; Dai, W.; He, K. Comparison between pericapsular nerve group (PENG) block with lateral femoral cutaneous nerve block and supra-inguinal fascia iliaca compartment block (S-FICB) for total hip arthroplasty: A randomized controlled trial. J. Anesth. 2023, 37, 503–510. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, M.; Gao, M.; Hu, Y.; Ren, X.; Li, Y.; Gao, F.; Dong, J.; Dong, J.; Wang, Q. Comparison of the Effect of Pericapsular Nerve Group Block Combined with Lateral Femoral Cutaneous Nerve Block and Fascia Iliaca Compartment Block in Patients Undergoing Hip Arthroscopy Under General Anesthesia: A Randomized, Double-Blind Trial. J. Pain Res. 2024, 17, 1651–1661. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pascarella, G.; Costa, F.; Del Buono, R.; Pulitanò, R.; Strumia, A.; Piliego, C.; De Quattro, E.; Cataldo, R.; Agrò, F.E.; Carassiti, M. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: A randomised, observer-masked, controlled trial. Anaesthesia 2021, 76, 1492–1498. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taylor, A.; McLeod, G. Basic pharmacology of local anaesthetics. BJA Educ. 2020, 20, 34–41, Erratum in BJA Educ. 2020, 20, 140. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shigeta, H.; Yasumura, R.; Kotake, Y. Comparison of plasma levobupivacaine concentrations with and without epinephrine following erector spinae plane block for breast cancer surgery: A randomized controlled trial. BMC Anesthesiol. 2022, 22, 86. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Cassai, A.; Bonanno, C.; Padrini, R.; Geraldini, F.; Boscolo, A.; Navalesi, P.; Munari, M. Pharmacokinetics of lidocaine after bilateral ESP block. Reg. Anesth. Pain Med. 2021, 46, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Laigaard, J.; Pedersen, C.; Rønsbo, T.N.; Mathiesen, O.; Karlsen, A.P.H. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: A systematic review. Br. J. Anaesth. 2021, 126, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Dizdarevic, A.; Farah, F.; Ding, J.; Shah, S.; Bryan, A.; Kahn, M.; Kaye, A.D.; Gritsenko, K. A Comprehensive Review of Analgesia and Pain Modalities in Hip Fracture Pathogenesis. Curr. Pain Headache Rep. 2019, 23, 72. [Google Scholar] [CrossRef] [PubMed]
- Pascarella, G.; Costa, F.; Strumia, A.; Ruggiero, A.; Remore, L.M.; Lanteri, T.; Hazboun, A.; Longo, F.; Gargano, F.; Schiavoni, L.; et al. Lateral Femoral Cutaneous Nerve Block or Wound Infiltration Combined with Pericapsular Nerve Group (PENG) Block for Postoperative Analgesia following Total Hip Arthroplasty through Posterior Approach: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 2674. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variable | FICB (n = 29) | PENG + LFCN (n = 29) | Standardized Difference | p |
|---|---|---|---|---|
| Age (years) | 71 ± 9 | 71 ± 10 | 0.0319 | 0.9053 |
| Body weight (kg) | 78.4 ± 16.6 | 79.8 ± 14.3 | −0.0868 | 0.7423 |
| Height (cm) | 164.9 ± 8.9 | 169.1 ± 7.3 | −0.5028 | 0.0606 |
| BMI (kg/m2) | 28.8 ± 5.7 | 27.8 ± 3.9 | 0.1196 | 0.4065 |
| Male sex | 14 (48.2%) | 19 (65.5%) | −0.1474 | 0.1850 |
| ASA status | 2 [2; 2] | 2 [2; 2] | 0.0001 | 0.8283 |
| Chronic pain medication | 2 (6.9%) | 3 (10.3%) | −0.1209 | 0.6402 |
| Diabetes mellitus | 5 (17.2%) | 6 (20.7%) | −0.0865 | 0.7381 |
| Italian nationality | 29 (100%) | 29 (100%) | 0.0001 | >0.9999 |
| Variable | FICB (n = 29) | PENG + LFCN (n = 29) | P (Group) | P (Time) | P (Interaction) |
|---|---|---|---|---|---|
| MRC scale | <0.0001 | 0.0304 | 0.0777 | ||
| 6 h | 3 [3; 4] | 4 [4; 4] | |||
| 24 h | 4 [3; 4] | 4 [4; 4] | |||
| 48 h | 4 [3; 4] | 4 [4; 5] | |||
| Degree of hip flexion | <0.0001 | <0.0001 | 0.7405 | ||
| 6 h | 30 [25; 43] | 45 [37; 60] | |||
| 24 h | 47 [36; 50] | 59 [49; 66] | |||
| 48 h | 50 [40; 55] | 62 [55; 70] | |||
| Static NRS | <0.0001 | 0.4825 | 0.3585 | ||
| 6 h | 2 [0; 3] | 0 [0; 1] | |||
| 24 h | 1 [0; 3] | 0 [0; 2] | |||
| 48 h | 1 [0; 3] | 0 [0; 1] | |||
| Dynamic NRS | 0.0001 | 0.0381 | 0.1029 | ||
| 6 h | 3 [2; 5] | 1 [0; 2] | |||
| 24 h | 3 [2; 4] | 2 [2; 4] | |||
| 48 h | 3 [1; 3] | 2 [1; 2] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vetrone, F.; Marelli, S.; Galimberti, A.; Umbrello, M.; Gotti, M.; Pezzi, A.; Girombelli, A. Pericapsular Nerve Group (PENG) Associated with Lateral Femoral Cutaneous Nerve (LFCN) Block Versus Fascia Iliaca Compartment Block (FICB) for Total Hip Replacement Surgery: Double-Blind Randomized Controlled Trial. J. Pers. Med. 2025, 15, 230. https://doi.org/10.3390/jpm15060230
Vetrone F, Marelli S, Galimberti A, Umbrello M, Gotti M, Pezzi A, Girombelli A. Pericapsular Nerve Group (PENG) Associated with Lateral Femoral Cutaneous Nerve (LFCN) Block Versus Fascia Iliaca Compartment Block (FICB) for Total Hip Replacement Surgery: Double-Blind Randomized Controlled Trial. Journal of Personalized Medicine. 2025; 15(6):230. https://doi.org/10.3390/jpm15060230
Chicago/Turabian StyleVetrone, Francesco, Stefano Marelli, Andrea Galimberti, Michele Umbrello, Miriam Gotti, Angelo Pezzi, and Alessandro Girombelli. 2025. "Pericapsular Nerve Group (PENG) Associated with Lateral Femoral Cutaneous Nerve (LFCN) Block Versus Fascia Iliaca Compartment Block (FICB) for Total Hip Replacement Surgery: Double-Blind Randomized Controlled Trial" Journal of Personalized Medicine 15, no. 6: 230. https://doi.org/10.3390/jpm15060230
APA StyleVetrone, F., Marelli, S., Galimberti, A., Umbrello, M., Gotti, M., Pezzi, A., & Girombelli, A. (2025). Pericapsular Nerve Group (PENG) Associated with Lateral Femoral Cutaneous Nerve (LFCN) Block Versus Fascia Iliaca Compartment Block (FICB) for Total Hip Replacement Surgery: Double-Blind Randomized Controlled Trial. Journal of Personalized Medicine, 15(6), 230. https://doi.org/10.3390/jpm15060230







