The Public Knowledge of Precision Medicine and Genomic Research: A Survey in the Aosta Valley
Abstract
1. Introduction
2. Materials and Methods
2.1. Respondents
2.2. Questionnaire
2.3. Data Analysis
3. Results
3.1. Concerns About Participating
3.2. Willingness to Provide Personal Information and Biological Samples
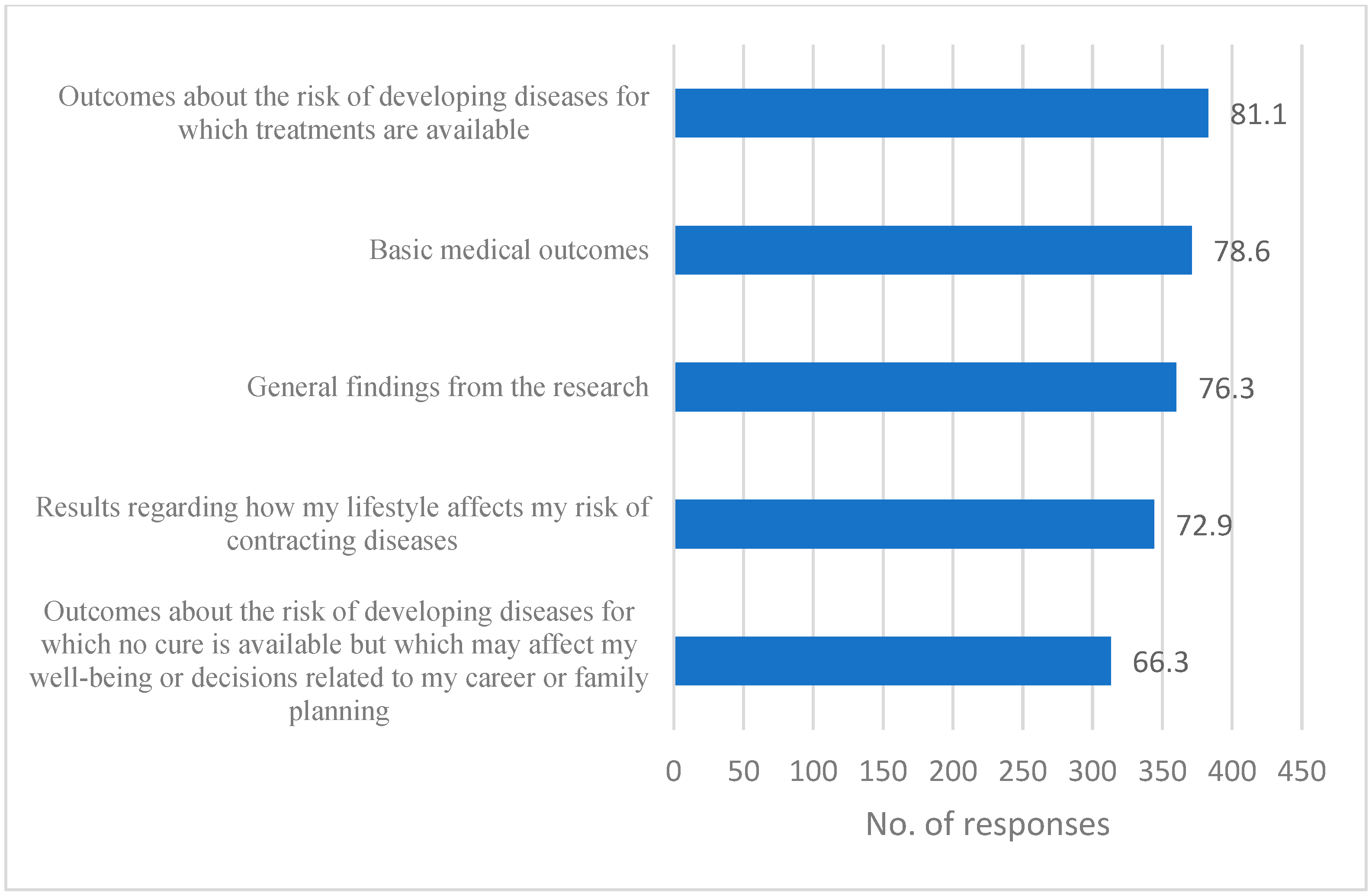
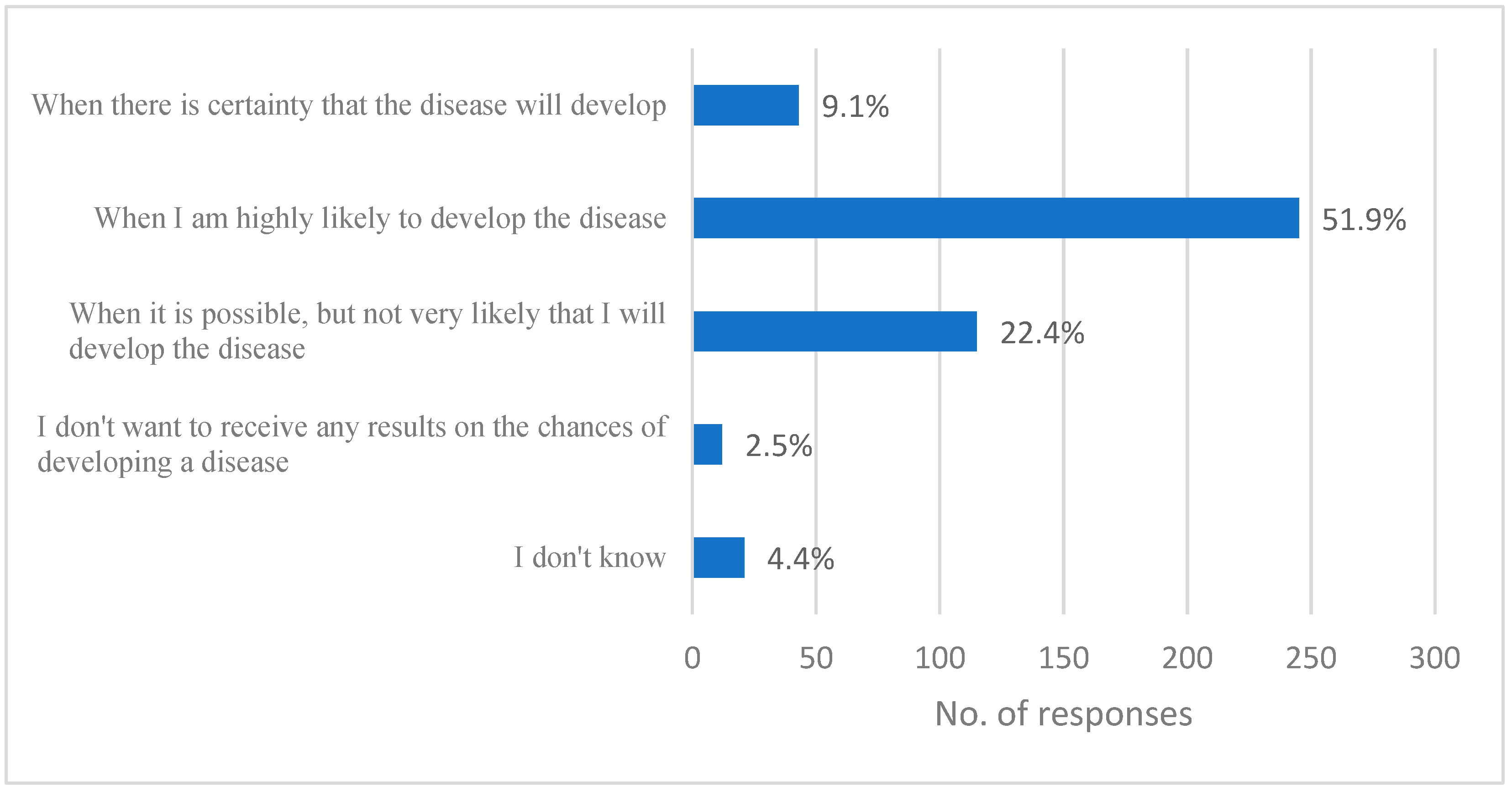
3.3. Data Management and Sharing
3.4. Concerns About Not Participating
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schwarze, K.; Buchanan, J.; Fermont, J.M.; Dreau, H.; Tilley, M.W.; Taylor, J.M.; Antoniou, P.; Knight, S.J.L.; Camps, C.; Pentony, M.M.; et al. The complete costs of genome sequencing: A microcosting study in cancer and rare diseases from a single center in the United Kingdom. Genet. Med. 2020, 22, 85–94. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, E.L.; Auger, H.; Jaszczyszyn, Y.; Thermes, C. Ten years of next-generation sequencing technology. Trends Genet. 2014, 30, 418–426. [Google Scholar] [CrossRef] [PubMed]
- van Nimwegen, K.J.; van Soest, R.A.; Veltman, J.A.; Nelen, M.R.; van der Wilt, G.J.; Vissers, L.E.; Grutters, J.P. Is the $1000 Genome as near as we think? A cost analysis of next-generation sequencing. Clin. Chem. 2016, 62, 1458–1464. [Google Scholar] [CrossRef]
- Fahr, P.; Buchanan, J.; Wordsworth, S. A review of the challenges of using biomedical big data for economic evaluations of Precision Medicine. Appl. Health Econ. Health Policy 2019, 17, 443–452. [Google Scholar] [CrossRef]
- Shendure, J.; Findlay, G.M.; Snyder, M.W. Genomic medicine-progress, pitfalls, and promise. Cell 2019, 177, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Kikano, S.; Kannankeril, P.J. Precision medicine in pediatric cardiology. Pediatr. Ann. 2022, 51, e390–e395. [Google Scholar] [CrossRef] [PubMed]
- Xie, F.; Chan, J.C.; Ma, R.C. Precision medicine in diabetes prevention, classification, and management. J. Diabetes Investig. 2018, 9, 998–1015. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, K.R.; Bebiak, J.; Brown, K.; Campbell, C.; Dighe, A.; Hyashi, L.; Jefferson, N.; Roberts, G.V.; Stutzke, C.; Knight, R.; et al. Patient perspectives and involvement in precision medicine research. Kidney Int. 2021, 99, 511–514. [Google Scholar] [CrossRef]
- Gavriilaki, M.; Kimiskidis, V.K.; Gavriilaki, E. Precision medicine in neurology: The inspirational paradigm of complement therapeutics. Pharmaceuticals 2020, 13, 341. [Google Scholar] [CrossRef] [PubMed]
- Hampel, H.; Caraci, F.; Cuello, A.C.; Caruso, G.; Nisticò, R.; Corbo, M.; Baldacci, F.; Toschi, N.; Garaci, F.; Chiesa, P.A.; et al. A path toward precision medicine for neuroinflammatory mechanisms in Alzheimer’s disease. Front. Immunol. 2020, 11, 456. [Google Scholar] [CrossRef]
- McGinn, R.J.; Von Stein, E.L.; Summers Stromberg, J.E.; Li, Y. Precision medicine in epilepsy. Prog. Mol. Biol. Transl. Sci. 2022, 190, 147–188. [Google Scholar] [CrossRef] [PubMed]
- Mateo, J.; Steuten, L.; Aftimos, P.; André, F.; Davies, M.; Garralda, E.; Geissler, J.; Husereau, D.; Martinez-Lopez, I.; Normanno, N.; et al. Delivering precision oncology to patients with cancer. Nat. Med. 2022, 28, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.K.; Oluoha, O.; Patel, K.; VanderWalde, A. Precision Medicine in oncology: A review of multi-tumor actionable molecular targets with an emphasis on non-small cell lung cancer. J. Pers. Med. 2021, 11, 518. [Google Scholar] [CrossRef]
- Jin, K.; Zhang, C. Personalized Medicine in ophthalmic Diseases: Challenges and opportunities. J. Pers. Med. 2023, 13, 893. [Google Scholar] [CrossRef]
- Pardiñas, A.F.; Owen, M.J.; Walters, J.T.R. Pharmacogenomics: A road ahead for precision medicine in psychiatry. Neuron 2021, 109, 3914–3929. [Google Scholar] [CrossRef]
- Quinlan, E.B.; Banaschewski, T.; Barker, G.J.; Bokde, A.L.W.; Bromberg, U.; Büchel, C.; Desrivières, S.; Flor, H.; Frouin, V.; Garavan, H.; et al. Identifying biological markers for improved precision medicine in psychiatry. Mol. Psychiatry 2020, 25, 243–253. [Google Scholar] [CrossRef]
- Sankar, P.L.; Parker, L.S. The Precision Medicine initiative’s All of Us Research Program: An agenda for research on its ethical, legal, and social issues. Genet. Med. 2017, 19, 743–750. [Google Scholar] [CrossRef]
- Glynn, P.; Greenland, P. Contribution of the UK biobank high impact papers in the era of Precision Medicine. Eur. J. Epidemiol. 2020, 35, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Kaja, E.; Lejman, A.; Sielski, D.; Sypniewski, M.; Gambin, T.; Dawidziuk, M.; Suchocki, T.; Golik, P.; Wojtaszewska, M.; Mroczek, M.; et al. The Thousand Polish Genomes: A Database of Polish variant allele frequencies. Int. J. Mol. Sci. 2022, 23, 4532. [Google Scholar] [CrossRef] [PubMed]
- Borgheresi, R.; Barucci, A.; Colantonio, S.; Aghakhanyan, G.; Assante, M.; Bertelli, E.; Carlini, E.; Carpi, R.; Caudai, C.; Cavallero, D.; et al. NAVIGATOR: An Italian regional imaging biobank to promote precision medicine for oncologic patients. Eur. Radiol. Exp. 2022, 6, 53. [Google Scholar] [CrossRef] [PubMed]
- Leitsalu, L.; Alavere, H.; Tammesoo, M.L.; Leego, E.; Metspalu, A. Linking a population biobank with national health registries-the Estonian experience. J. Pers. Med. 2015, 5, 96–106. [Google Scholar] [CrossRef]
- Bochud, M.; Currat, C.; Chapatte, L.; Roth, C.; Mooser, V. High participation rate among 25 721 patients with broad age range in a hospital-based research project involving whole-genome sequencing—The Lausanne Institutional Biobank. Swiss. Med. Wkly. 2017, 147, w14528. [Google Scholar] [CrossRef] [PubMed]
- Brall, C.; Berlin, C.; Zwahlen, M.; Ormond, K.E.; Egger, M.; Vayena, E. Public willingness to participate in personalized health research and biobanking: A large-scale Swiss survey. PLoS ONE 2021, 16, e0249141. [Google Scholar] [CrossRef] [PubMed]
- Bühler, N.; Frahsa, A.; Jaramillo, N.G.; Bourqui, R.M.; Nusslé, S.G.; Zuppinger, C.; Bochud, M.; von Goetz, N. Willingness to participate in a personalized health cohort—Insights from the swiss health study pilot phase. BMC Public Health 2024, 24, 2140. [Google Scholar] [CrossRef]
- Pronicki, Ł.; Czech, M.; Gujski, M.; Boguszewska, N.D. Awareness, Attitudes and Willingness to Donate Biological Samples to a Biobank: A Survey of a Representative Sample of Polish Citizens. Healthcare 2023, 11, 2714. [Google Scholar] [CrossRef] [PubMed]
- Lysaght, T.; Ballantyne, A.; Toh, H.J.; Lau, A.; Ong, S.; Schaefer, O.; Shiraishi, M.; van den Boom, W.; Xafis, V.; Tai, E.S. Trust and trade-offs in sharing data for Precision Medicine: A national survey of Singapore. J. Pers. Med. 2021, 11, 921. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, H.R.; Kim, S. Public attitudes toward Precision Medicine: A nationwide survey on developing a national cohort program for citizen participation in the republic of Korea. Front. Genet. 2020, 11, 283. [Google Scholar] [CrossRef]
- Hishiyama, Y.; Minari, J.; Suganuma, N. The survey of public perception and general knowledge of genomic research and medicine in Japan conducted by the Japan Agency for Medical Research and Development. J. Hum. Genet. 2019, 64, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Addis, A.; Trotta, F.; Tafuri, G.; De Flore, L. Information needs on precision medicine: A survey of Italian health care professionals. Ann. Dell’istituto Super. Di Sanità 2018, 54, 316–323. [Google Scholar] [CrossRef]
- Porteri, C.; Pasqualetti, P.; Togni, E.; Parker, M. Public’s attitudes on participation in a biobank for research: An Italian survey. BMC Med. Ethics 2014, 15, 81. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Kettis-Lindblad, A.; Ring, L.; Viberth, E.; Hansson, M.G. Genetic research and donation of tissue samples to biobanks. What do potential sample donors in the Swedish general public think? Eur. J. Public Health 2006, 16, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Skirbekk, H.; Magelssen, M.; Conradsen, S. Trust in healthcare before and during the COVID-19 pandemic. BMC Public Health 2023, 23, 863. [Google Scholar] [CrossRef] [PubMed]
- Tosoni, S.; Voruganti, I.; Lajkosz, K.; Mustafa, S.; Phillips, A.; Kim, S.J.; Wong, R.K.S.; Willison, D.; Virtanen, C.; Heesters, A.; et al. Patient consent preferences on sharing personal health information during the COVID-19 pandemic: “The more informed we are, the more likely we are to help”. BMC Med. Ethics 2022, 23, 53. [Google Scholar] [CrossRef]
- Humphrey, A.; Forbes-Mewett, H. Social value systems and the mental health of international students during the COVID-19 pandemic. J. Int. Stud. 2021, 11 (Suppl. S2), 58–76. [Google Scholar] [CrossRef]
- Twenge, J.M.; Campbell, W.K.; Freeman, E.C. Generational differences in young adults’ life goals, concern for others, and civic orientation, 1966–2009. J. Pers. Soc. Psychol. 2012, 102, 1045–1062. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. The Changing Childhood Project 2021. UNICEF, New York. 2021. Available online: https://www.unicef.org/innocenti/media/566/file/UNICEF-Global-Insight-Gallup-Changing-Childhood-Survey-Report-English-2021.pdf (accessed on 25 September 2023).
- Zangiacomi Martinez, E.; Dos Santos Almeida, R.G.; Garcia Braz, A.C.; Duarte de Carvalho, A.C. Association between religiousness and blood donation among Brazilian postgraduate students from health-related areas. Rev. Bras. Hematol. Hemoter. 2014, 36, 184–190. [Google Scholar] [CrossRef]
- Charsetad, P. Role of religious beliefs in blood donation behavior among the youngster in Iran: A theory of planned behavior perspective. J. Islam. Mark. 2016, 7, 250–263. [Google Scholar] [CrossRef]
- Ramadhanty, Q. Emotional intelligence, religiosity, and prosocial behavior in blood donors. Int. J. Res. 2024, 11, 200–209. [Google Scholar] [CrossRef]
- Zucoloto, M.; Gonçalez, T.; McFarland, W.; Custer, B.; Martinez, E. Does religiosity predict blood donation in Brazil? J. Relig. Health 2022, 61, 2083–2101. [Google Scholar] [CrossRef] [PubMed]
- Benevento, M.; Mandarelli, G.; Carravetta, F.; Ferorelli, D.; Caterino, C.; Nicolì, S.; Massari, A.; Solarino, B. Measuring the willingness to share personal health information: A systematic review. Front. Public Health 2023, 11, 1213615. [Google Scholar] [CrossRef] [PubMed]
- Zeissig, E.; Lidynia, C.; Vervier, L.; Gadeib, A.; Ziefle, M. Online privacy perceptions of older adults. In International Conference on Human Aspects of IT for the Aged Population; Springer: New York, NY, USA, 2017; pp. 181–200. [Google Scholar] [CrossRef]
- Lee, C.; Owens, R.G. Issues for a psychology of men’s health. J. Health Psychol. 2002, 7, 209–217. [Google Scholar] [CrossRef] [PubMed]
| Willingness to Participate in a Genomic Study | Awareness of Precision Medicine | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||||||
| N (%) | N (%) | N (%) | χ2 (df) | p | N (%) | N (%) | N (%) | χ2 (df) | p | |
| Gender | 3.3 (2) | ns | 2.7 (2) | ns | ||||||
| Females | 328 (69.5) | 306 (93.3) | 22 (6.7) | 328 (69.5) | 117 (35.7) | 211 (64.3) | ||||
| Males | 128 (27.1) | 118 (92.2) | 10 (7.8) | 128 (27.1) | 54 (42.2) | 74 (57.8) | ||||
| Prefer not to say or other | 16 (3.4) | 13 (81.3) | 3 (18.8) | 16 (3.4) | 8 (50.0) | 8 (50.0) | ||||
| Age | 6.1 (6) | ns | 11.3 (5) | 0.046 | ||||||
| 18–24 | 48 (10.2) | 42 (87.5) | 6 (12.5) | 48 (10.2) | 9 (18.8) | 39 (81.3) | ||||
| 25–34 | 48 (10.2) | 46 (95.8) | 2 (4.2) | 48 (10.2) | 23 (47.9) | 25 (52.1) | ||||
| 35–44 | 100 (21.2) | 90 (90.0) | 10 (10.0) | 100 (21.2) | 37 (37.0) | 63 (63.0) | ||||
| 45–54 | 131 (27.8) | 124 (94.7) | 7 (5.3) | 131 (27.8) | 53 (40.5) | 78 (59.5) | ||||
| 55–64 | 123 (26.1) | 113 (91.9) | 10 (8.1) | 123 (26.1) | 46 (37.4) | 77 (62.6) | ||||
| >64 | 22 (4.7) | 22 (100.0) | 0 (0.0) | 22 (4.7) | 11 (50.0) | 11 (50.0) | ||||
| Having biological children | 2.1 (1) | ns | 1.4 (1) | ns | ||||||
| Yes | 269 (57.1) | 253 (94.1) | 16 (5.9) | 269 (57.1) | 108 (40.1) | 161 (59.9) | ||||
| No | 201 (42.8) | 182 (90.5) | 19 (9.5) | 201 (42.8) | 70 (34.8) | 131 (65.2) | ||||
| Education | 0.3 (3) | ns | 23.9 (3) | 0.001 | ||||||
| Compulsory education | 26 (5.5) | 24 (92.3) | 2 (7.7) | 26 (5.5) | 6 (23.1) | 20 (76.9) | ||||
| Secondary | 186 (39.4) | 172 (92.5) | 14 (7.5) | 186 (39.4) | 49 (26.3) | 137 (73.7) | ||||
| Tertiary | 205 (43.4) | 191 (93.2) | 14 (6.8) | 205 (43.4) | 96 (46.8) | 109 (53.2) | ||||
| Post-university degree | 55 (11.7) | 50 (90.9) | 5 (9.1) | 55 (11.7) | 28 (50.9) | 27 (49.1) | ||||
| Work experience in the healthcare sector | 0.1 (1) | ns | 7.9 (1) | 0.005 | ||||||
| Yes | 59 (12.6) | 54 (91.5) | 5 (8.5) | 59 (12.6) | 32 (54.2) | 27 (45.8) | ||||
| No | 411 (87.4) | 381 (92.7) | 30 (7.3) | 411 (87.4) | 145 (35.3) | 266 (64.7) | ||||
| Alcohol consumptions | 0.1 (1) | ns | 0.2 (1) | ns | ||||||
| Yes/More than twice a week | 152 (32.2) | 140 (92.1) | 12 (7.9) | 152 (32.2) | 60 (39.5) | 92 (60.5) | ||||
| No/Less than twice a week | 319 (67.6) | 296 (92.8) | 23 (7.2) | 319 (67.6) | 118 (37.0) | 201 (63.0) | ||||
| Smoker | 3.1 (1) | ns | 2.3 (1) | ns | ||||||
| Yes | 62 (13.1) | 54 (87.1) | 8 (12.9) | 62 (13.1) | 18 (29.0) | 44 (71.0) | ||||
| No | 409 (86.7) | 382 (93.4) | 27 (6.6) | 409 (86.7) | 160 (39.1) | 249 (60.9) | ||||
| Health self-perceived status | 0.9 (2) | ns | 2.8 (2) | ns | ||||||
| In health | 56 (11.9) | 53 (94.6) | 3 (5.4) | 56 (11.9) | 26 (46.4) | 30 (53.6) | ||||
| Good Health | 364 (77.1) | 337 (92.6) | 27 (7.4) | 364 (77.1) | 131 (36.0) | 233 (64.0) | ||||
| Excellent health | 49 (10.4) | 44 (89.8) | 5 (10.2) | 49 (10.4) | 28 (57.1) | 21 (42.9) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mongelli, M.; De Angelis, B.; delle Cave, V.; Greco, G.; De Arcangelis, A.; Bernagozzi, A.; Salvemini, C.; Calabrese, M.; Christille, J.M.; Cavalli, A.; et al. The Public Knowledge of Precision Medicine and Genomic Research: A Survey in the Aosta Valley. J. Pers. Med. 2025, 15, 80. https://doi.org/10.3390/jpm15030080
Mongelli M, De Angelis B, delle Cave V, Greco G, De Arcangelis A, Bernagozzi A, Salvemini C, Calabrese M, Christille JM, Cavalli A, et al. The Public Knowledge of Precision Medicine and Genomic Research: A Survey in the Aosta Valley. Journal of Personalized Medicine. 2025; 15(3):80. https://doi.org/10.3390/jpm15030080
Chicago/Turabian StyleMongelli, Matteo, Biagio De Angelis, Valeria delle Cave, Giuliano Greco, Arianna De Arcangelis, Andrea Bernagozzi, Chiara Salvemini, Matteo Calabrese, Jean Marc Christille, Andrea Cavalli, and et al. 2025. "The Public Knowledge of Precision Medicine and Genomic Research: A Survey in the Aosta Valley" Journal of Personalized Medicine 15, no. 3: 80. https://doi.org/10.3390/jpm15030080
APA StyleMongelli, M., De Angelis, B., delle Cave, V., Greco, G., De Arcangelis, A., Bernagozzi, A., Salvemini, C., Calabrese, M., Christille, J. M., Cavalli, A., Gustincich, S., & Monaci, M. G. (2025). The Public Knowledge of Precision Medicine and Genomic Research: A Survey in the Aosta Valley. Journal of Personalized Medicine, 15(3), 80. https://doi.org/10.3390/jpm15030080







