Mid-Regional Pro-Adrenomedullin Is Associated with Adverse Cardiovascular Outcomes After Cardiac Surgery
Abstract
1. Introduction
2. Materials and Methods
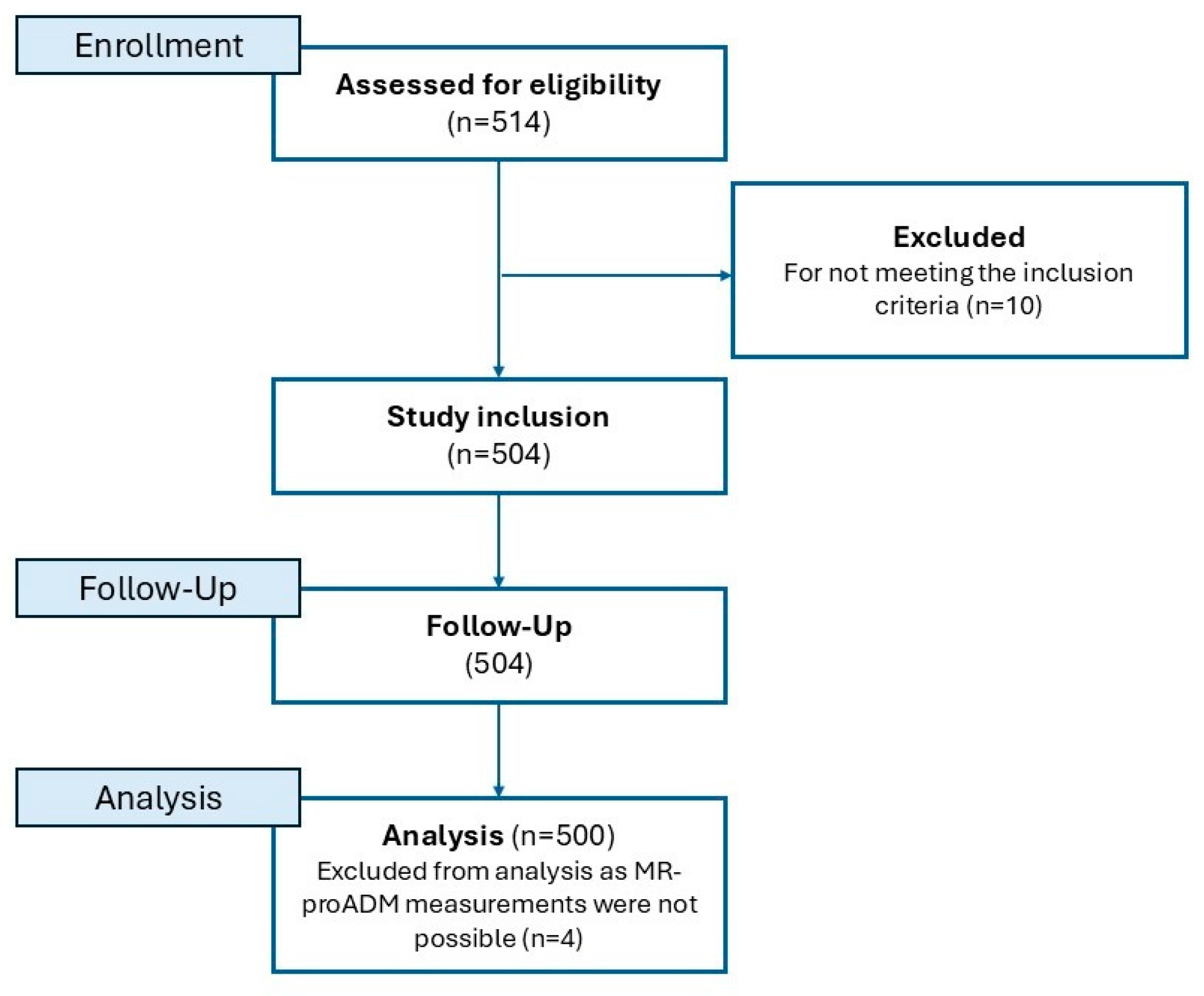
2.1. Study Population
2.2. Data Acquisition and MR-proADM Measures
2.3. Follow-Up and Endpoints
2.4. Statistical Analysis
3. Results
3.1. Study Population
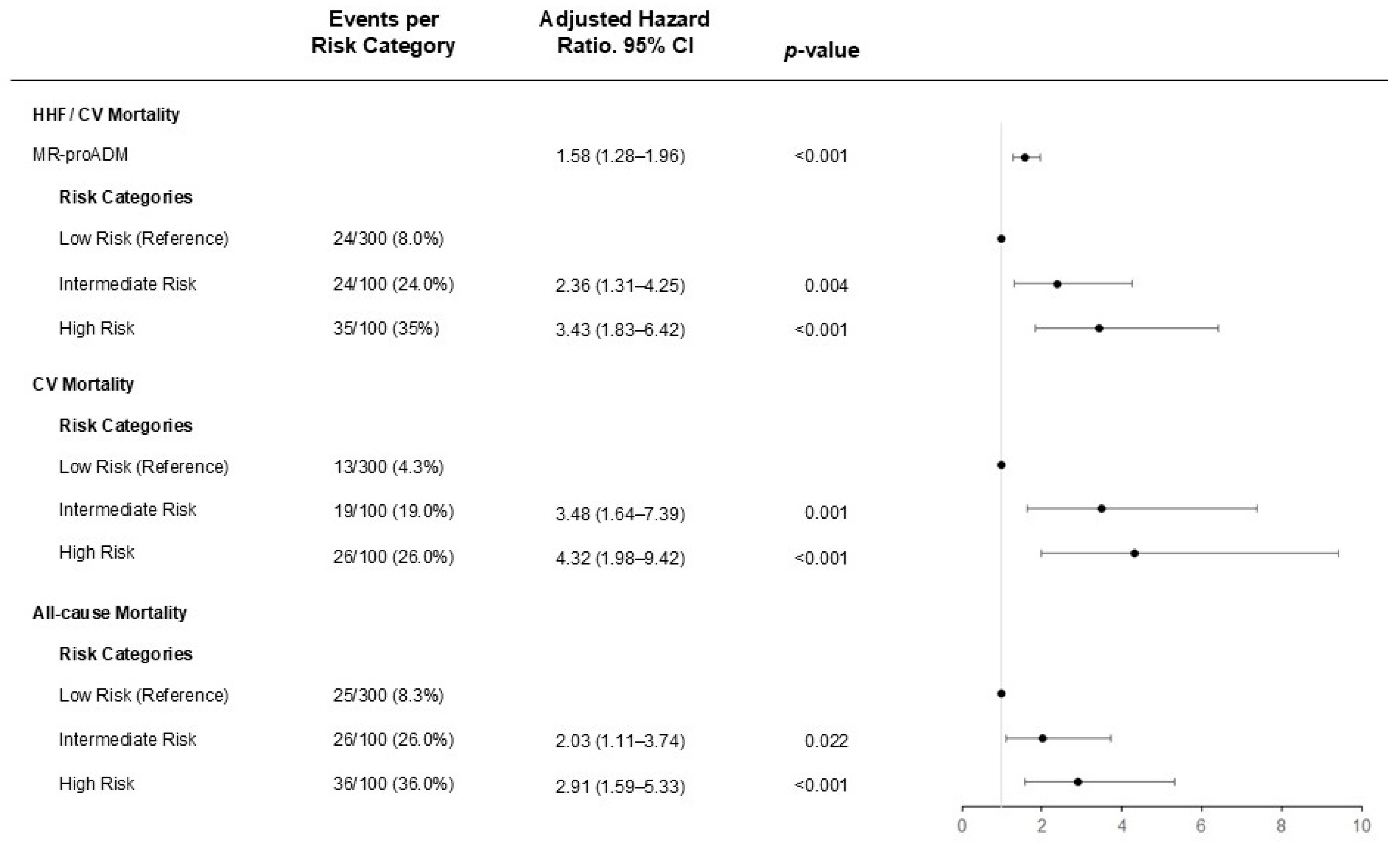
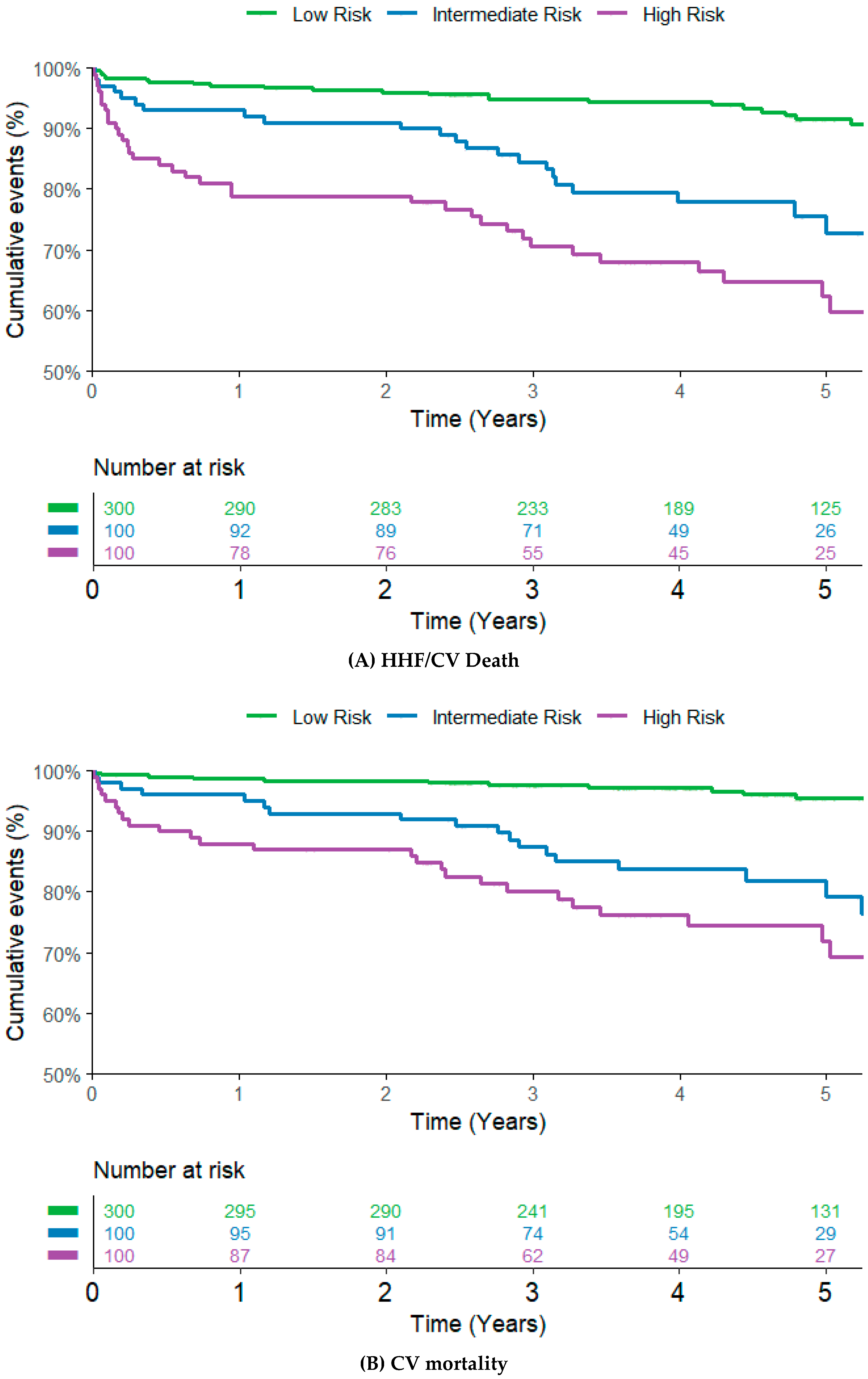
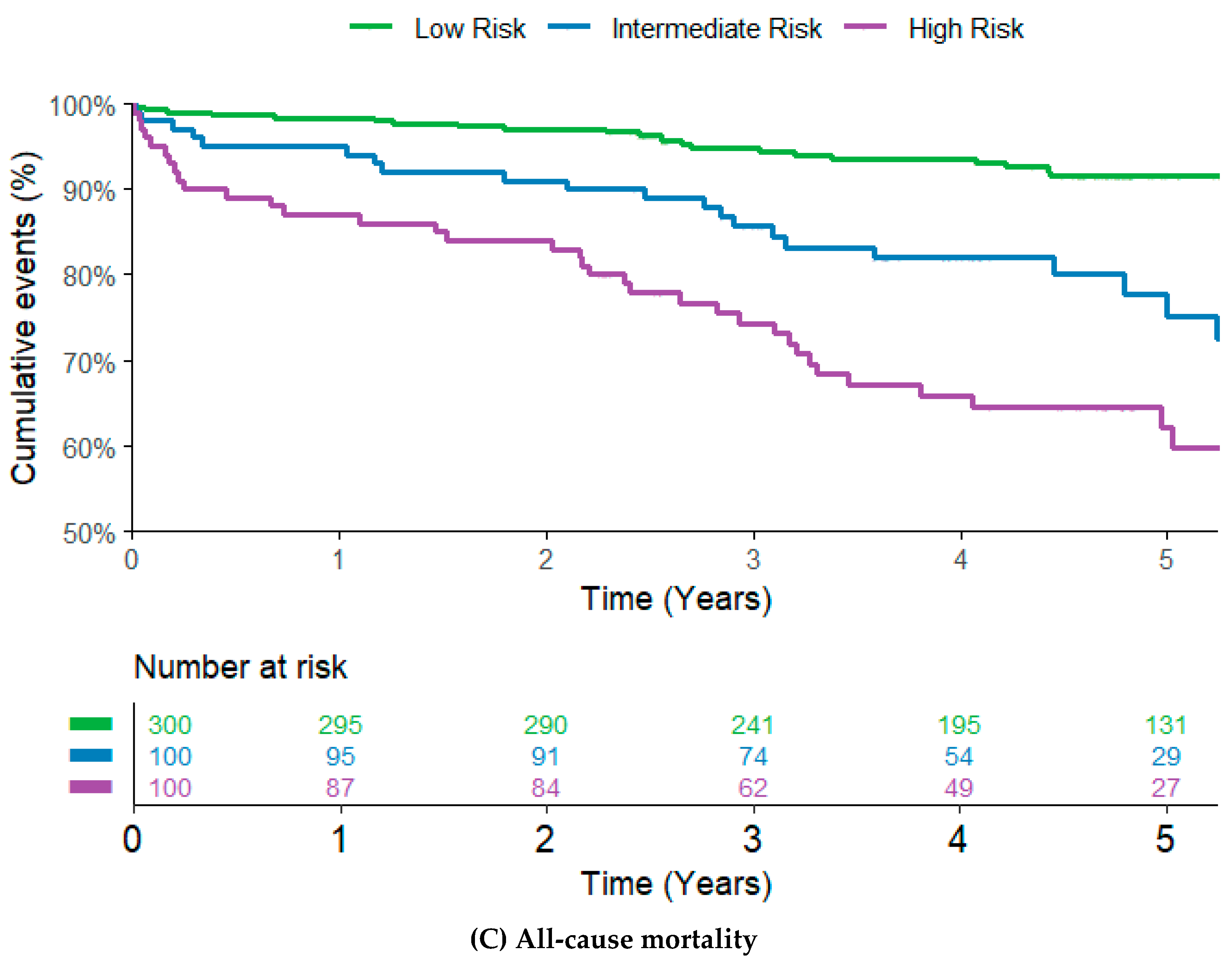
3.2. Impact of MR-proADM on Cardiovascular Outcomes
3.3. Association of MR-proADM and Postoperative Atrial Fibrillation
4. Discussion
4.1. MR-proADM as Prognostic Biomarker for Cardiovascular Outcomes
4.2. Postoperative Atrial Fibrillation
4.3. Risk Assessment in Cardiac Surgery
4.4. Clinical Implementation and Personalized Risk Assessment
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CABG | Coronary artery bypass graft |
| CART | Classification And Regression Tree |
| CRP | C-reactive protein |
| CV | Cardiovascular |
| HF | Heart failure |
| HHF | Hospitalization for heart failure |
| IQR | Interquartile range |
| MR-proADM | Mid-regional pro adrenomedullin |
| NT-pro BNP | N-terminal prohormone of brain natriuretic peptide |
| POAF | Postoperative atrial fibrillation |
References
- Pahwa, S.; Bernabei, A.; Schaff, H.; Stulak, J.; Greason, K.; Pochettino, A.; Daly, R.; Dearani, J.; Bagameri, G.; King, K.; et al. Impact of postoperative complications after cardiac surgery on long-term survival. J. Card. Surg. 2021, 36, 2045–2052. [Google Scholar] [CrossRef] [PubMed]
- Castiglione, V.; Aimo, A.; Vergaro, G.; Saccaro, L.; Passino, C.; Emdin, M. Biomarkers for the diagnosis and management of heart failure. Heart Fail. Rev. 2022, 27, 625–643. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.-K.; Yuan, H.-X.; Jian, Y.-P.; Chen, Y.-T.; Liang, K.-F.; Liu, X.-J.; Ou, Z.-J.; Liu, J.-S.; Li, Y.; Ou, J.-S. Pentraxin 3 in Circulating Microvesicles: A Potential Biomarker for Acute Heart Failure After Cardiac Surgery with Cardiopulmonary Bypass. J. Cardiovasc. Transl. Res. 2022, 15, 1414–1423. [Google Scholar] [CrossRef] [PubMed]
- Hinson, J.P.; Kapas, S.; Smith, D.M. Adrenomedullin, a Multifunctional Regulatory Peptide. Endocr. Rev. 2000, 21, 138–167. [Google Scholar] [PubMed]
- Struck, J.; Tao, C.; Morgenthaler, N.G.; Bergmann, A. Identification of an Adrenomedullin precursor fragment in plasma of sepsis patients. Peptides 2004, 25, 1369–1372. [Google Scholar] [CrossRef]
- Kuan, W.S.; Ibrahim, I.; Chan, S.P.; Li, Z.; Liew, O.W.; Frampton, C.; Troughton, R.; Pemberton, C.J.; Chong, J.P.C.; Tan, L.L.; et al. Mid-regional pro-adrenomedullin outperforms N-terminal pro-B-type natriuretic peptide for the diagnosis of acute heart failure in the presence of atrial fibrillation. Eur. J. Heart Fail. 2020, 22, 692–700. [Google Scholar] [CrossRef]
- Peacock, W.F. Novel biomarkers in acute heart failure: MR-pro-adrenomedullin. Clin. Chem. Lab. Med. 2014, 52, 1433–1435. [Google Scholar] [CrossRef] [PubMed]
- Angeletti, S.; Spoto, S.; Fogolari, M.; Cortigiani, M.; Fioravanti, M.; De Florio, L.; Curcio, B.; Cavalieri, D.; Costantino, S.; Dicuonzo, G. Diagnostic and prognostic role of procalcitonin (PCT) and MR-pro-Adrenomedullin (MR-proADM) in bacterial infections. Apmis 2015, 123, 740–748. [Google Scholar] [CrossRef]
- Fialek, B.; De Roquetaillade, C.; Pruc, M.; Navolokina, A.; Chirico, F.; Ladny, J.R.; Peacock, F.W.; Szarpak, L. Systematic review with meta-analysis of mid-regional pro-adrenomedullin (MR-proadm) as a prognostic marker in COVID-19-hospitalized patients. Ann. Med. 2023, 55, 379–387. [Google Scholar] [CrossRef]
- Špinarová, M.; Špinar, J.; Špinarová, L.; Krejčí, J.; Goldbergová-Pávková, M.; Pařenica, J.; Ludka, O.; Malek, F.; Ošťádal, P.; Benešová, K.; et al. Relation between Mid-Regional Pro-Adrenomedullin in Patients with Chronic Heart Failure and the Dose of Diuretics in 2-Year Follow-Up—Data from FAR NHL Registry. Medicina 2022, 58, 1477. [Google Scholar] [CrossRef] [PubMed]
- Spoto, S.; Argemi, J.; Di Costanzo, R.; Gavira Gomez, J.J.; Salterain Gonzales, N.; Basili, S.; Cangemi, R.; Abbate, A.; Locorriere, L.; Masini, F.; et al. Mid-Regional Pro-Adrenomedullin and N-Terminal Pro-B-Type Natriuretic Peptide Measurement: A Multimarker Approach to Diagnosis and Prognosis in Acute Heart Failure. J. Pers. Med. 2023, 13, 1155. [Google Scholar] [CrossRef] [PubMed]
- Cruciat, R.C.; Gazi, G.; Ismaiel, A.; Leucuta, D.-C.; Al Srouji, N.; Popa, S.-L.; Ismaiel, M.; Ensar, D.; Dumitrascu, D.L. Unlocking the potential of biomarkers: The promise of adrenomedullin and its precursors in diagnosing and assessing heart failure. Int. J. Cardiol. 2025, 418, 132659. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart. J. 2020, 42, 373–498. [Google Scholar] [CrossRef]
- Voors, A.A.; Kremer, D.; Geven, C.; Ter Maaten, J.M.; Struck, J.; Bergmann, A.; Pickkers, P.; Metra, M.; Mebazaa, A.; Düngen, H.D.; et al. Adrenomedullin in heart failure: Pathophysiology and therapeutic application. Eur. J. Heart Fail. 2019, 21, 163–171. [Google Scholar] [CrossRef]
- Gar, C.; Thorand, B.; Herder, C.; Sujana, C.; Heier, M.; Meisinger, C.; Peters, A.; Koenig, W.; Rathmann, W.; Roden, M.; et al. Association of circulating MR-proADM with all-cause and cardiovascular mortality in the general population: Results from the KORA F4 cohort study. PLoS ONE 2022, 17, e0262330. [Google Scholar] [CrossRef] [PubMed]
- Marino, R.; Struck, J.; Maisel, A.S.; Magrini, L.; Bergmann, A.; Somma, S.D. Plasma adrenomedullin is associated with short-term mortality and vasopressor requirement in patients admitted with sepsis. Crit. Care 2014, 18, R34. [Google Scholar] [CrossRef]
- Richards, A.M.; Doughty, R.; Nicholls, M.G.; MacMahon, S.; Sharpe, N.; Murphy, J.; Espiner, E.A.; Frampton, C.; Yandle, T.G. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin. J. Am. Coll. Cardiol. 2001, 37, 1781–1787. [Google Scholar] [CrossRef] [PubMed]
- Dobrev, D.; Aguilar, M.; Heijman, J.; Guichard, J.-B.; Nattel, S. Postoperative atrial fibrillation: Mechanisms, manifestations and management. Nat. Rev. Cardiol. 2019, 16, 417–436. [Google Scholar] [CrossRef] [PubMed]
- Hofer, F.; Hammer, A.; Steininger, M.; Kazem, N.; Koller, L.; Steinlechner, B.; Laufer, G.; Andreas, M.; Marculescu, R.; Hengstenberg, C.; et al. The Prognostic Potential of Atrial Natriuretic Peptide on the Development of Postoperative Atrial Fibrillation after Cardiac Surgery. Thromb. Haemost. 2021, 121, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Richter, B.; Koller, L.; Hofer, F.; Kazem, N.; Hammer, A.; Silbert, B.I.; Laufer, G.; Steinlechner, B.; Wojta, J.; Hengstenberg, C.; et al. Galectin-3 is an independent predictor of postoperative atrial fibrillation and survival after elective cardiac surgery. Heart Rhythm. 2022, 19, 1774–1780. [Google Scholar] [CrossRef] [PubMed]
- Kazem, N.; Hammer, A.; Koller, L.; Hofer, F.; Steinlechner, B.; Laufer, G.; Hengstenberg, C.; Wojta, J.; Sulzgruber, P.; Niessner, A. The Prognostic Potential of Growth Differentiation Factor-15 on Bleeding Events and Patient Outcome after Cardiac Surgery—A Prospective Cohort Study. Thromb. Haemost. 2022, 122, 703–714. [Google Scholar] [CrossRef] [PubMed]
- Hofer, F.; Hammer, A.; Pailer, U.; Koller, L.; Kazem, N.; Steinacher, E.; Steinlechner, B.; Andreas, M.; Laufer, G.; Wojta, J.; et al. Relationship of Fibroblast Growth Factor 23 with Hospitalization for Heart Failure and Cardiovascular Outcomes in Patients Undergoing Cardiac Surgery. J. Am. Heart Assoc. 2023, 12, e027875. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, R.B.; Wild, P.S.; Wilde, S.; Ojeda, F.M.; Schulz, A.; Zeller, T.; Sinning, C.R.; Kunde, J.; Lackner, K.J.; Munzel, T.; et al. Multiple Biomarkers and Atrial Fibrillation in the General Population. PLoS ONE 2014, 9, e112486. [Google Scholar] [CrossRef] [PubMed]
- Parwani, A.S.; von Haehling, S.; Kolodziejski, A.I.; Huemer, M.; Wutzler, A.; Attanasio, P.; Stojakovic, T.; Scharnagl, H.; Haverkamp, W.; Boldt, L.-H. Mid-regional proadrenomedullin levels predict recurrence of atrial fibrillation after catheter ablation. Int. J. Cardiol. 2015, 180, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Clayton, B.; Morgan-Hughes, G.; Roobottom, C. Transcatheter aortic valve insertion (TAVI): A review. Br. J. Radiol. 2014, 87, 20130595. [Google Scholar] [CrossRef]
- Schoe, A.; Schippers, E.F.; Struck, J.; Ebmeyer, S.; Klautz, R.J.M.; de Jonge, E.; van Dissel, J.T. Postoperative Pro-Adrenomedullin Levels Predict Mortality in Thoracic Surgery Patients: Comparison with Acute Physiology and Chronic Health Evaluation IV Score. Crit. Care Med. 2015, 43, 373–381. [Google Scholar] [CrossRef]
- Hillinger, P.; Mayr, V.D.; Luger, M.; Tauber, H.; Luckner, G.; Morgenthaler, N.G.; Dünser, M.; Jochberger, S. The course of adrenomedullin and endothelin levels in patients with vasodilatory shock after cardiac surgery compared to patients after uncomplicated elective cardiac surgery. J. Crit. Care 2022, 69, 154009. [Google Scholar] [CrossRef] [PubMed]
- Baldenhofer, G.; Laule, M.; Mockel, M.; Sanad, W.; Knebel, F.; Dreger, H.; Leonhardt, F.; Sander, M.; Grubitzsch, H.; Baumann, G.; et al. Mid-regional pro-adrenomedullin (MR-proADM) and mid-regional pro-atrial natriuretic peptide (MR-proANP) in severe aortic valve stenosis: Association with outcome after transcatheter aortic valve implantation (TAVI). Clin. Chem. Lab. Med. 2017, 55, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Pousset, F.; Masson, F.; Chavirovskaia, O.; Isnard, R.; Carayon, A.; Golmard, J.L.; Lechat, P.; Thomas, D.; Komajda, M. Plasma adrenomedullin, a new independent predictor of prognosis in patients with chronic heart failure. Eur. Heart J. 2000, 21, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Di Franco, A.; Rong, L.Q.; Piccini, J.; Mack, M. Postoperative atrial fibrillation: From mechanisms to treatment. Eur. Heart J. 2023, 44, 1020–1039. [Google Scholar] [CrossRef] [PubMed]
- Stavrakis, S.; Humphrey, M.B.; Scherlag, B.; Iftikhar, O.; Parwani, P.; Abbas, M.; Filiberti, A.; Fleming, C.; Hu, Y.; Garabelli, P.; et al. Low-Level Vagus Nerve Stimulation Suppresses Post-Operative Atrial Fibrillation and Inflammation: A Randomized Study. JACC Clin. Electrophysiol. 2017, 3, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Trooboff, S.W.; Magnus, P.C.; Ross, C.S.; Chaisson, K.; Kramer, R.S.; Helm, R.E.; Desaulniers, H.; De La Rosa, R.C.; Westbrook, B.M.; Duquette, D.; et al. A multi-center analysis of readmission after cardiac surgery: Experience of The Northern New England Cardiovascular Disease Study Group. J. Card. Surg. 2019, 34, 655–662. [Google Scholar] [CrossRef]
| Variable | All Patients (n = 500) | Low Risk (n = 300) | Intermediate Risk (n = 100) | High Risk (n = 100) | p-Value |
|---|---|---|---|---|---|
| Clinical Presentation | |||||
| Age, years (median, IQR) | 70 (61–76) | 67 (58–24) | 73 (66–78) | 72 (66–78) | <0.001 |
| Sex, female, (n, %) | 146 (29.2) | 82 (27.3) | 31 (31.0) | 33 (33.0) | 0.506 |
| Body mass index, kg/m2 (median, IQR) | 27.2 (24.3–30.2) | 26.8 (24.1–29.7)) | 27.7 (24.9–30.9) | 28.2 (24.3–30.9) | 0.095 |
| Type of surgery | |||||
| Valve replacement (n, %) | 214 (42.8) | 130 (43.3) | 43 (43.0) | 41 (41.0) | 0.919 |
| CABG, (n, %) | 160 (32.0) | 109 (36.3) | 26 (26.0) | 25 (25.0) | 0.039 |
| Valve replacement and CABG, (n, %) | 126 (25.2) | 61 (20.3) | 31 (31.0) | 34 (34.0) | 0.008 |
| NYHA Class, (n, %) | 0.059 | ||||
| I | 26 (9) | 15 (9.6) | 8 (12.5) | 3 (4.4) | |
| II | 125 (43.3) | 79 (50.3) | 24 (37.5) | 22 (32.4) | |
| III | 120 (41.5) | 55 (35.0) | 28 (43.8) | 37 (54.4) | |
| IV | 18 (6.2) | 8 (5.1) | 4 (6.3) | 6 (8.8) | |
| LVEF | 60 (54.2–60) | 60 (60–60) | 60 (50–60) | 55 (40–60) | <0.001 |
| Left atrial Diameter, mm (median, IQR) | 55 (45–65) | 55 (45–60) | 55 (45–65) | 60 (55–65) | <0.001 |
| CHA2DS2VASc score (median, IQR) | 4 (3–5) | 3 (2–4) | 4 (3–5) | 4 (4–5) | <0.001 |
| EuroSCORE II (median, IQR) | 2.3 (1.2–4.5) | 1.7 (1.0–2.8) | 2.7 (1.6–4.8) | 6.7 (3.2–12.2) | <0.001 |
| Comorbidities (n, %) | |||||
| Coronary artery disease | 302 (60.4) | 178 (59.3) | 61 (61.0) | 63 (63.0) | 0.802 |
| Previous MCI | 130 (26.0) | 69 (23.0) | 28 (28.0) | 33 (33.0) | 0.125 |
| Hypertension | 405 (81.0) | 234 (78.0) | 84 (84.0) | 87 (87.0) | 0.096 |
| Diabetes mellitus | 144 (28.8) | 69 (23.0) | 31 (31.0) | 44 (44.0) | <0.001 |
| Heart failure | 289 (57.8) | 157 (52.3) | 64 (64) | 68 (68) | 0.009 |
| COPD | 69 (13.8) | 30 (10) | 14 (14) | 25 (25) | <0.001 |
| Current smoker | 61 (12.2) | 38 (12.7) | 10 (10.0) | 13 (13.0) | 0.751 |
| Laboratory measures at admission | |||||
| MR-proADM nmol/L (median, IQR) | 0.58 (0.44–0.79) | 0.48 (0.36–0.56) | 0.73 (0.67–0.79) | 1.12 (0.94–1.43) | <0.001 |
| NT-proBNP, pg/mL (median, IQR) | 539.6 (209.4–1455.0) | 324.3 (140.5–694.3) | 573.2 (241.7–1289.0) | 2116.0 (957.1–6062.0) | <0.001 |
| C-reactive protein, mg/dL (median, IQR) | 0.2 (0.1–0.5) | 0.2 (0.1–0.4) | 0.2 (0.1–0.5) | 0.4 (0.2–1.1) | <0.001 |
| Creatinine, mg/dL (median, IQR) | 0.95 (0.8–1.2) | 0.87 (0.75–1.0) | 1.04 (0.91–1.18) | 1.39 (1.16–1.87) | <0.001 |
| HR | 95% CI | p-Value | |
|---|---|---|---|
| HHF/CV Mortality | |||
| MR-proADM | 1.77 | 1.23–2.55 | 0.002 |
| Intermediate Risk | 2.34 | 1.30–4.24 | 0.005 |
| High Risk | 2.76 | 1.52–5.02 | <0.001 |
| CV Mortality | |||
| MR-proADM | 2.11 | 1.42–3.13 | <0.001 |
| Intermediate Risk | 3.63 | 1.76–7.49 | <0.001 |
| High Risk | 3.87 | 1.90–7.85 | <0.001 |
| All-cause mortality | |||
| MRpro-ADM | 2.23 | 1.63–3.07 | <0.001 |
| Intermediate Risk | 2.22 | 1.24–3.97 | 0.007 |
| High Risk | 2.89 | 1.67–4.97 | <0.001 |
| POAF | OR | 95% CI | p-Value |
|---|---|---|---|
| MR-proADM | 1.70 | 1.13–2.55 | 0.010 |
| Intermediate Risk | 1.25 | 0.79–1.98 | 0.344 |
| High Risk | 2.02 | 1.28–3.20 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baumer, U.; Kazem, N.; Hammer, A.; Hofer, F.; Steinacher, E.; Koller, L.; Zimpfer, D.; Andreas, M.; Steinlechner, B.; Hengstenberg, C.; et al. Mid-Regional Pro-Adrenomedullin Is Associated with Adverse Cardiovascular Outcomes After Cardiac Surgery. J. Pers. Med. 2025, 15, 47. https://doi.org/10.3390/jpm15020047
Baumer U, Kazem N, Hammer A, Hofer F, Steinacher E, Koller L, Zimpfer D, Andreas M, Steinlechner B, Hengstenberg C, et al. Mid-Regional Pro-Adrenomedullin Is Associated with Adverse Cardiovascular Outcomes After Cardiac Surgery. Journal of Personalized Medicine. 2025; 15(2):47. https://doi.org/10.3390/jpm15020047
Chicago/Turabian StyleBaumer, Ulrike, Niema Kazem, Andreas Hammer, Felix Hofer, Eva Steinacher, Lorenz Koller, Daniel Zimpfer, Martin Andreas, Barbara Steinlechner, Christian Hengstenberg, and et al. 2025. "Mid-Regional Pro-Adrenomedullin Is Associated with Adverse Cardiovascular Outcomes After Cardiac Surgery" Journal of Personalized Medicine 15, no. 2: 47. https://doi.org/10.3390/jpm15020047
APA StyleBaumer, U., Kazem, N., Hammer, A., Hofer, F., Steinacher, E., Koller, L., Zimpfer, D., Andreas, M., Steinlechner, B., Hengstenberg, C., Niessner, A., & Sulzgruber, P. (2025). Mid-Regional Pro-Adrenomedullin Is Associated with Adverse Cardiovascular Outcomes After Cardiac Surgery. Journal of Personalized Medicine, 15(2), 47. https://doi.org/10.3390/jpm15020047







