Prevalence of Osteosarcopenic Adiposity in Apparently Healthy Adults and Appraisal of Age, Sex, and Ethnic Differences
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropometric and Bioimpedance Measurements
2.3. Statistical Analysis
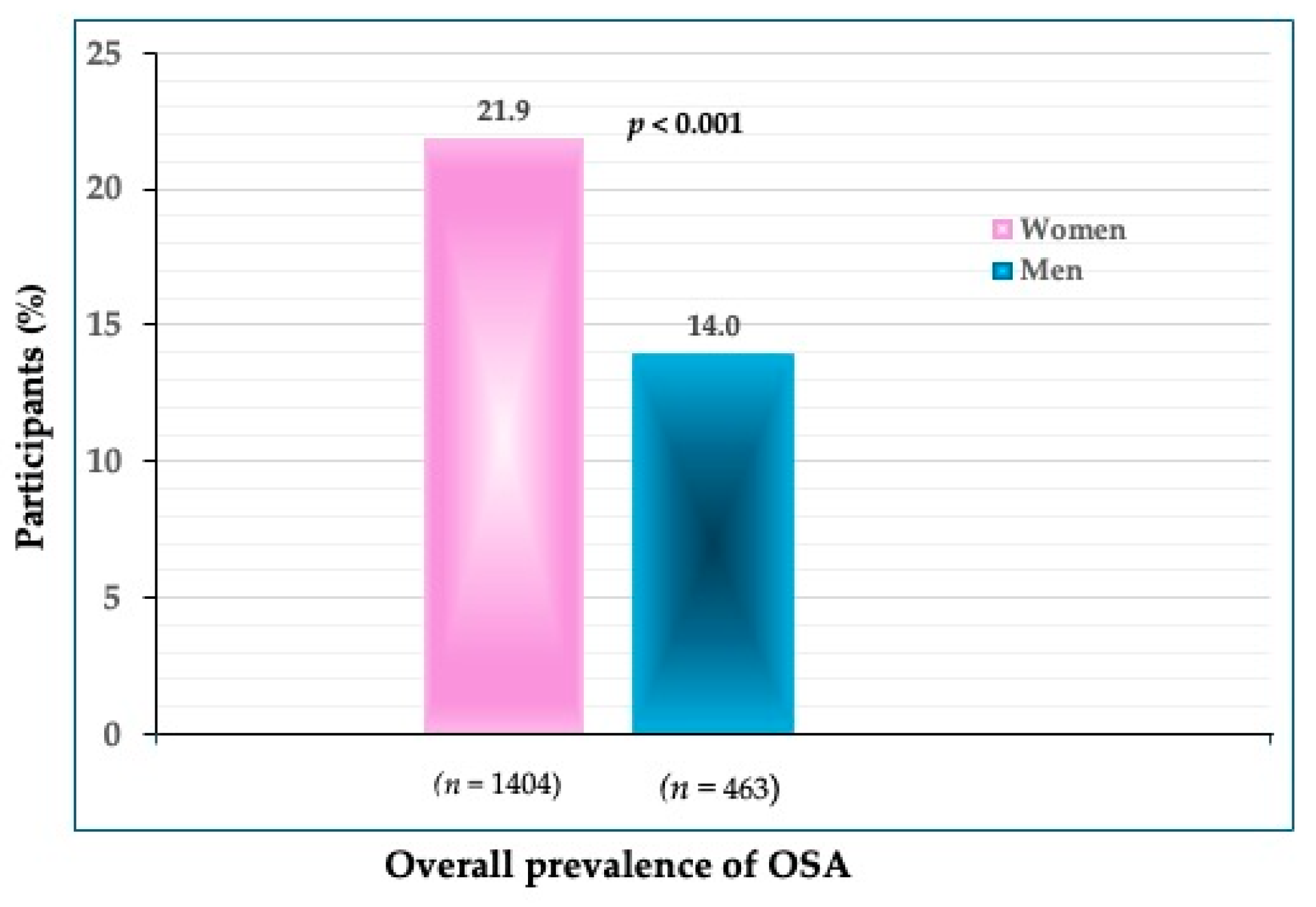
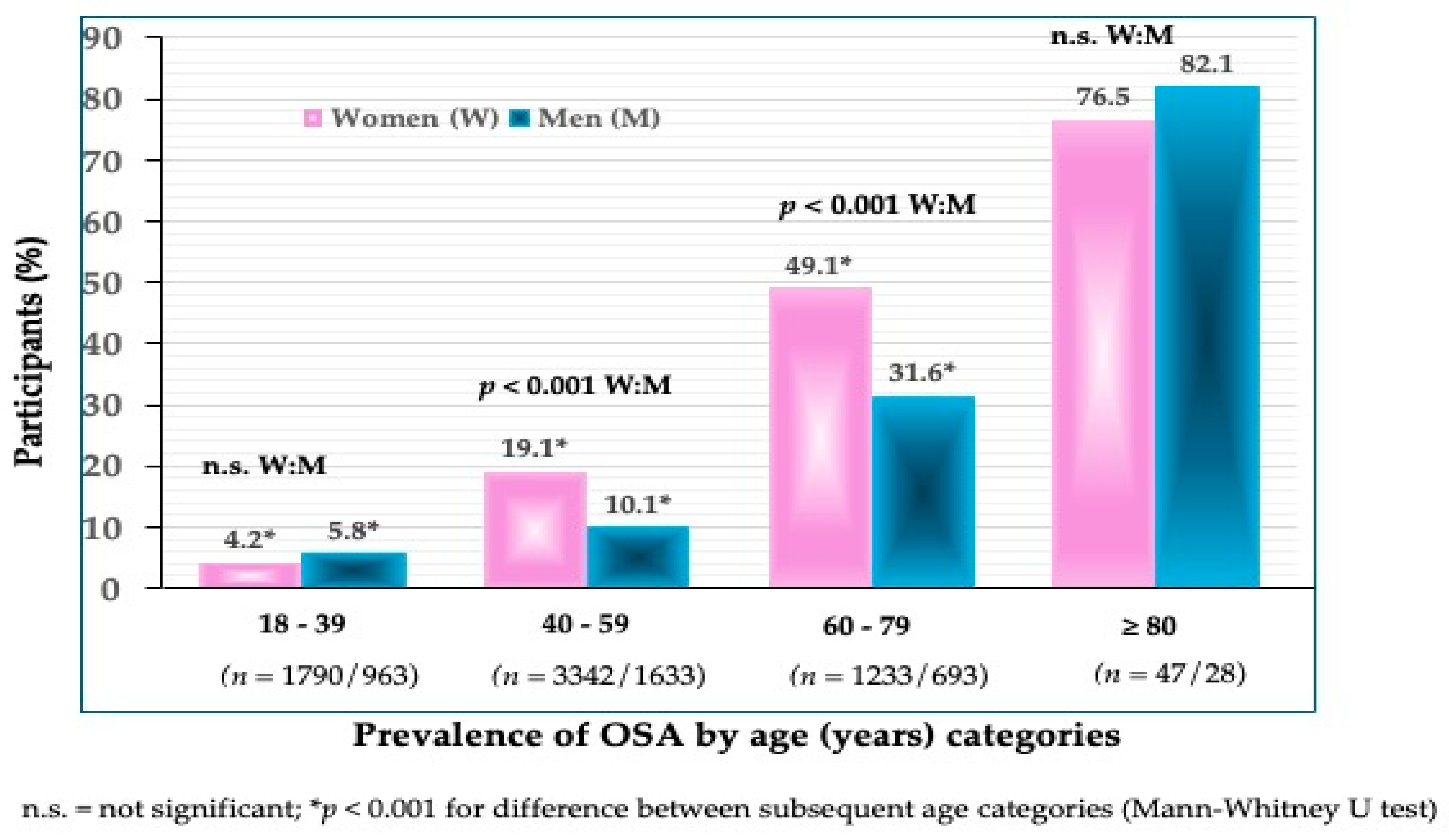
3. Results
4. Discussion
5. Conclusions and Implications for Future Research
- While the majority of the studies were conducted in older women (either White or Asian), equally important would be the studies in younger individuals, as the evidence from the current study and earlier work [21] identified OSA phenotypes in healthy, young, obese individuals.
- ○
- Therefore, both men and women of different ages and races/ethnicities (there are no studies on African Americans), as well as critical populations (e.g., institutionalized individuals), would provide for better diagnostic criteria.
- ▪
- For example, a close approximation of its prevalence in the general population could be obtained from large population databases like NHANES, KNHANES, or the UK Biobank, which comprise relatively healthy participants of a wide age range and the same regional and environmental influences; however, the ethnic differences must be accounted for.
- Body composition could be measured by various devices (e.g., DXA, BIA, ultrasound for bones, BMI for obesity—not recommended); however, the prevalence of OSA should be compared among studies that used the same/similar technology.
- ○
- Furthermore, to differentiate the OSA from other body composition impairments, the comparison should be made with those having osteopenia/osteoporosis, osteopenic adiposity, sarcopenia, sarcopenic adiposity, or osteopenic sarcopenia, or adiposity-alone, and most importantly with those of normal body composition parameters. This will provide more insight into OSA and its association with other health issues.
- The development of biomarkers for each tissue and their combination could also help in the identification of OSA; however, the investigation of these biomarkers in the context of OSA syndrome is still in the early stages.
- ○
- Some pilot studies specified the combination of increased levels of serum sclerostin (a bone resorption marker), skeletal muscle troponin (a muscle breakdown marker), leptin (an indicator of higher adiposity), and an inferior lipid profile as possible markers for OSA. However, some fine-tuning and more studies are necessary. In this context, a series of omics will need to be determined to serve as potential biomarkers.
- Additionally, given the fast genomic developments (sequencing and molecular drug exploitation), “the precision medicine concepts can also be utilized to outline OSA using multiple data sources, from genomics to digital health metrics to artificial intelligence, to facilitate individualized yet “evidence-based” decisions regarding diagnostic and therapeutic approaches. In this way, therapeutics can be centered toward patients based on their molecular presentation rather than grouping them into broad categories with a “one-size-fits-all” approach” citation from [7].
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Genton, L.; Karsegard, V.L.; Chevalley, T.; Kossovsky, M.P.; Darmon, P.; Pichard, C. Body composition changes over 9 years in healthy elderly subjects and impact of physical activity. Clin. Nutr. 2011, 30, 436–442. [Google Scholar] [CrossRef]
- JafariNasabian, P.; Inglis, J.E.; Reilly, W.; Kelly, O.J.; Ilich, J.Z. Aging human body: Changes in bone, muscle, and body fat with consequent changes in nutrient intake. J. Endocrinol. 2017, 234, R37–R51. [Google Scholar] [CrossRef]
- Wells, J.C.K.; Shirley, M.K. Body composition and the monitoring of non-communicable chronic disease risk. Glob. Health Epidemiol. Genom. 2016, 1, e18. [Google Scholar] [CrossRef]
- Ilich, J.Z.; Kelly, O.J.; Inglis, J.E.; Panton, L.B.; Duque, G.; Ormsbee, M.J. Interrelationship among muscle, fat, and bone: Connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Rev. 2014, 15, 51–60. [Google Scholar] [CrossRef]
- Hu, K.; Edelen, E.D.; Zhuo, W.; Khan, A.; Orbegoso, J.; Greenfield, L.; Rahi, B.; Griffin, M.; Ilich, J.Z.; Kelly, O.J. Understanding the consequences of fatty bone and fatty muscle: How the osteosarcopenic adiposity phenotype uncovers the deterioration of body composition. Metabolites 2023, 13, 1056. [Google Scholar] [CrossRef]
- Kelly, O.J.; Gilman, J.C.; Boschiero, D.; Ilich, J.Z. Osteosarcopenic obesity: Current knowledge, revised identification criteria and treatment principles. Nutrients 2019, 11, 747. [Google Scholar] [CrossRef]
- Vucic, V.; Ristic-Medic, D.; Arsic, A.; Petrovic, S.; Paunovic, M.; Vasiljevic, N.; Ilich, J.Z. Nutrition and physical activity as modulators of osteosarcopenic adiposity: A scoping review and recommendations for future research. Nutrients 2023, 15, 1619. [Google Scholar] [CrossRef]
- Ilich, J.Z.; Pokimica, B.; Ristić-Medić, D.; Petrović, S.; Arsić, A.; Vasiljević, N.; Vučić, V.; Kelly, O.J. Osteosarcopenic adiposity and its relation to cancer and chronic diseases: Implications for research to delineate mechanisms and improve clinical outcomes. Aging Res. Rev. 2024, under review. [Google Scholar]
- Kim, H.; Yoo, S.; Park, S.G. Young cancer survivors have lower bone mineral density compared with healthy controls: A nationwide population-based study in Korea. Sci. Rep. 2020, 10, 654. [Google Scholar] [CrossRef]
- Guarnotta, V.; Prinzi, A.; Pitrone, M.; Pizzolanti, G.; Giordano, C. Circulating Irisin Levels as a Marker of Osteosarcopenic-Obesity in Cushing’s Disease. Diabetes Metab. Syndr. Obes. 2020, 13, 1565–1574. [Google Scholar] [CrossRef] [PubMed]
- Davenport, A. Frailty, appendicular lean mass, osteoporosis, and osteosarcopenia in peritoneal dialysis patients. J. Nephrol. 2022, 35, 2333–2340. [Google Scholar] [CrossRef] [PubMed]
- Martín-González, C.; Fernández-Alonso, P.; Pérez-Hernández, O.; Abreu-González, P.; Espelosín-Ortega, E.; Fernández-Rodríguez, C.M.; Martín-Ponce, E.; González-Reimers, E. Sarcopenic Obesity in People with Alcoholic Use Disorder: Relation with Inflammation, Vascular Risk Factors and Serum Vitamin D Levels. Int. J. Mol. Sci. 2023, 24, 9976. [Google Scholar] [CrossRef]
- Toomey, C.M.; Cremona, A.; Hughes, K.; Norton, C.; Jakeman, P. A Review of Body Composition Measurement in the Assessment of Health. Top. Clin. Nutr. 2015, 30, 16–32. [Google Scholar] [CrossRef]
- Borazan, F.Y.; Dazıroglu, M.E.; Gövez, N.E.; Acar-Tek, N.; Göker, B.; Varan, H.D. Body composition analyses in older adults may vary significantly depending on the bioelectrical impedance analyzer modality. Top. Clin. Nutr. 2024, 39, 104–111. [Google Scholar] [CrossRef]
- Su, Y.-H.; Chang, Y.-M.; Kung, C.-Y.; Sung, C.-K.; Foo, W.-S.; Wu, M.-H.; Chiou, S.-J. A study of correlations between metabolic syndrome factors and osteosarcopenic adi-posity. BMC Endocr. Disord. 2021, 21, 216. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Association of osteosarcopenic obesity and its components: Osteoporosis, sarcopenia and obesity with insulin resistance. J. Bone Miner. Metab. 2020, 38, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.K.; Bae, Y.J. Protein intake and osteosarcopenic adiposity in Korean adults aged 50 years and older. Osteoporos. Int. 2020, 31, 2363–2372. [Google Scholar] [CrossRef]
- Choi, M.K.; Bae, Y.J. Dietary calcium, phosphorus, and osteosarcopenic adiposity in Korean adults aged 50 years and older. Arch. Osteoporos. 2021, 16, 89. [Google Scholar] [CrossRef]
- Kashiwagi, K.; Takayama, M.; Ichikawa, H.; Takaishi, H.; Iwao, Y.; Kanai, T. A significant association of non-obese non-alcoholic fatty liver disease with osteosarcopenic obesity in females 50 years and older. Clin. Nutr. ESPEN 2021, 42, 166–172. [Google Scholar] [CrossRef]
- Nie, Y.-Z.; Yan, Z.-Q.; Yin, H.; Shan, L.-H.; Wang, J.-H.; Wu, Q.-H. Osteosarcopenic obesity and its components-osteoporosis, sarcopenia, and obesity-are associated with blood cell count-derived inflammation indices in older Chinese people. BMC Geriatr. 2022, 22, 532. [Google Scholar] [CrossRef]
- Stefanaki, C.; Peppa, M.; Boschiero, D.; Chrousos, G.P. Healthy overweight/obese youth: Early osteosarcopenic obesity features. Eur. J. Clin. Invest. 2016, 46, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Ahmadinezhad, M.; Fahimfar, N.; Shafiee, G.; Nabipour, I.; Sanjari, M.; Khalagi, K.; Mansourzadeh, M.J.; Larijani, B.; Ostovar, A. Prevalence of osteosarcopenic obesity and related factors among Iranian older people: Bushehr Elderly Health (BEH) program. Arch. Osteoporos. 2023, 18, 137. [Google Scholar] [CrossRef] [PubMed]
- Szlejf, C.; Parra-Rodríguez, L.; Rosas-Carrasco, O. Osteosarcopenic obesity: Prevalence and relation with frailty and physical performance in middle-aged and older women. J. Am. Med. Dir. Assoc. 2017, 18, 733.e1–733.e5. [Google Scholar] [CrossRef] [PubMed]
- Peppa, M.; Stefanaki, C.; Papaefstathiou, A.; Boschiero, D.; Dimitriadis, G.; Chrousos, G.P. Bioimpedance analysis vs. DEXA as a screening tool for osteosarcopenia in lean, overweight and obese Caucasian postmenopausal females. Hormones 2017, 16, 181–193. [Google Scholar] [CrossRef]
- Pang, B.W.J.; Wee, S.-L.; Chen, K.K.; Lau, L.K.; Jabbar, K.A.; Seah, W.T.; Ng, D.H.M.; Tan, Q.L.L.; Jagadish, M.U.; Ng, T.P. Coexistence of osteoporosis, sarcopenia and obesity in community-dwelling adults—The Yishun Study. Osteoporos. Sarcopenia 2021, 7, 17–23. [Google Scholar] [CrossRef]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Mo, D.; Hsieh, P.; Yu, H.; Zhou, L.; Gong, J.; Xu, L.; Liu, P.; Chen, G.; Chen, Z.; Deng, Q. Osteosarcopenic obesity and its relationship with dyslipidemia in women from different ethnic groups of China. Arch. Osteoporos. 2018, 13, 65. [Google Scholar] [CrossRef]
- Dhurandhar, E.J. The downfalls of BMI-focused policies. Int. J. Obes. 2016, 40, 729–730. [Google Scholar] [CrossRef]
- Kim, Y.M.; Kim, S.; Won, Y.J.; Kim, S.H. Clinical manifestations and factors associated with osteosarcopenic obesity syndrome: A cross-sectional study in Koreans with obesity. Calcif. Tissue Int. 2019, 105, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Soen, S.; Fukunaga, M.; Sugimoto, T.; Sone, T.; Fujiwara, S.; Endo, N.; Gorai, I.; Shiraki, M.; Hagino, H.; Hosoi, T.; et al. Diagnostic criteria for primary osteoporosis: Year 2012 revision. J. Bone Miner. Metab. 2013, 31, 247–257. [Google Scholar] [CrossRef]
- Cvijetić, S.; Keser, I.; Boschiero, D.; Ilich, J.Z. Osteosarcopenic adiposity and nutritional status in older nursing home residents during the COVID-19 pandemic. Nutrients 2023, 15, 227. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Ghasemi, H.; Mohammadi, L.; Behzadi, M.H.; Rabieenia, E.; Shohaimi, S.; Mohammadi, M. The global prevalence of osteoporosis in the world: Comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 609. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Balntzi, V.; Gray, S.R.; Lara, J.; Ho, F.K.; Pell, J.P.; Celis-Morales, C. Global prevalence of sarcopenia and severe sarcopenia: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2022, 13, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Gallagher, D.; Visser, M.; Nuñez, C.; Wang, Z.M. Measurement of skeletal muscle: Laboratory and epidemiological methods. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, 23–29. [Google Scholar] [CrossRef]
- Keser, I.; Cvijetić, S.; Ilić, A.; Barić, I.C.; Boschiero, D.; Ilich, J.Z. Assessment of body composition and dietary intake in nursing-home residents: Could lessons learned from the COVID-19 pandemic be used to prevent future casualties in older individuals? Nutrients 2021, 13, 1510. [Google Scholar] [CrossRef]
- Han, P.; Kang, L.; Guo, Q.; Wang, J.; Zhang, W.; Shen, S.; Wang, X.; Dong, R.; Ma, Y.; Shi, Y.; et al. Prevalence and factors associated with sarcopenia in suburb-dwelling older Chinese using the Asian Working Group for Sarcopenia Definition. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Park, S. Gender-specific risk factors and prevalence for sarcopenia among community-dwelling young-old adults. Int. J. Environ. Res. Public Health 2022, 19, 7232. [Google Scholar] [CrossRef]
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: A systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 2017, 16, 21. [Google Scholar] [CrossRef]
- Fielding, R.A. Sarcopenia: An emerging syndrome of advancing age. Calcif. Tissue Int. 2024, 114, 1–2. [Google Scholar] [CrossRef]
- Ji, M.X.; Yu, Q. Primary osteoporosis in postmenopausal women. Chronic Dis. Transl. Med. 2015, 1, 9–13. [Google Scholar] [CrossRef]
- Lovejoy, J.C.; Champagne, C.M.; de Jonge, L.; Xie, H.; Smith, S.R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. 2008, 32, 949–958. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.; Varghese, M.; Singer, K. Gender and sex differences in adipose tissue. Curr. Diab. Rep. 2018, 18, 69. [Google Scholar] [CrossRef] [PubMed]
- Perna, S.; Spadaccini, D.; Nichetti, M.; Avanzato, I.; Faliva, M.A.; Rondanelli, M. Osteosarcopenic Visceral Obesity and Osteosarcopenic Subcutaneous Obesity, Two New Phenotypes of Sarcopenia: Prevalence, Metabolic Profile, and Risk Factors. J. Aging Res. 2018, 2018, 6147426. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Kong, C.; Yu, H.; Gong, J.; Lan, L.; Zhou, L.; Gong, J.; Liu, P.; Xu, L.; Deng, Q. Association between osteosarcopenic obesity and hypertension among four minority populations in China: A cross-sectional study. BMJ Open 2019, 9, e026818. [Google Scholar] [CrossRef]
- Ma, Y.; Zhang, W.; Han, P.; Kohzuki, M.; Guo, Q. Osteosarcopenic obesity is associated with poor physical performance in the elderly Chinese community. Clin. Interv. Aging 2020, 15, 1343–1352. [Google Scholar] [CrossRef]
| Variables | Women (n = 6412) | Men (n = 3307) | p * | Reference Values |
|---|---|---|---|---|
| Age (y) | 47.6 ± 13.3 | 47.8 ± 14.1 | 0.412 | |
| Weight (cm) | 66.7 ± 14.4 | 82.9 ± 15.1 | <0.001 | |
| Height (kg) | 163.1 ± 6.6 | 176.4 ± 7.0 | <0.001 | |
| BMI (kg/m2) | 25.1 ± 5.4 | 26.6 ± 4.6 | <0.001 | 18–24.9 |
| T–score | −1.1 ± 0.8 | −0.3 ± 0.7 | <0.001 | >−1.0 |
| S–score | −0.9 ± 1.4 | −0.1 ± 1.2 | <0.001 | >−1.0 |
| FM (%) | 33.2 ± 8.6 | 32.5 ± 7.3 | <0.001 | 12–31.9% W 7–24.9% M |
| IMAT (%) | 2.0 ± 0.5 | 2.2 ± 0.4 | <0.001 | <2.0% |
| 18–39 (y) | 40–59 (y) | 60–79 (y) | ≥80 (y) | |||||
|---|---|---|---|---|---|---|---|---|
| Variables | W n = 1790 | M n = 953 | W n = 3342 | M n = 1633 | W n = 1233 | M n = 693 | W n = 47 | M n = 28 |
| Osteopenia/ osteoporosis | 52.0 a | 14.2 | 62.9 a | 15.6 | 75.3 a | 37.9 | 89.3 | 82.1 |
| Sarcopenia | 42.0 a | 20.8 | 56.4 a | 23.1 | 67.9 a | 47.6 | 89.3 | 89.2 |
| Obesity (based on FM%) | 39.1 a | 72.2 | 56.4 a | 90.3 | 81.3 a | 94.5 | 87.2 b | 100.0 |
| Obesity (based on BMI ≥ 25 kg/m2 | 39.2 a | 53.5 | 48.6 a | 72.8 | 61.5 a | 78.9 | 87.2 | 85.7 |
| Age (y) | BMI (kg/m2) | FM (%) | IMAT (%) | S-Score | T-Score | |
|---|---|---|---|---|---|---|
| Women | ||||||
| With OSA (n = 1358) | 58.1 ± 11.5 a | 24.6 ± 2.2 a | 36.7 ± 3.9 a | 2.4 ± 0.3 a | −1.8 ± 0.6 a | −1.7 ± 0.4 a |
| Without OSA (n = 5054) | 44.7 ± 12.5 | 25.2 ± 6.0 | 32.2 ± 9.3 | 1.9 ± 0.5 | −0.6 ± 1.4 | −0.9 ± 0.8 |
| Men | ||||||
| With OSA (n = 464) | 58.2 ± 14.5 a | 24.0 ± 2.4 a | 33.0 ± 4.8 | 2.4 ± 0.3 a | −1.6 ± 1.4 a | −1.3 ± 0.3 a |
| Without OSA (n = 2843) | 46.1 ± 13.3 | 27.0 ± 4.7 | 32.5 ± 7.6 | 2.2 ± 0.4 | −0.0 ± 1.1 | −0.1 ± 0.6 |
| Age Group (y) | Age (y) | BMI (kg/m2) | FM% | IMAT% | S-Score | T-Score |
|---|---|---|---|---|---|---|
| Women | ||||||
| 18–39 (n = 1790) | 31.1 ± 5.8 a | 24.1 ± 5.1 a | 29.9 ± 8.6 a | 1.6 ± 0.5 a | −0.5 ± 1.2 a | −0.8 ± 0.7 a |
| 40–59 (n = 3342) | 49.1 ± 5.4 a | 25.0 ± 5.3 a | 33.2 ± 8.3 a | 2.0 ± 0.4 a | −0.9 ± 1.4 a | −1.1 ± 0.8 a |
| 60–79 (n = 1233) | 66.2 ± 4.9 a | 26.6 ± 5.7 | 37.8 ± 7.4 | 2.5 ± 0.3 a | −1.4 ± 1.5 a | −1.5 ± 0.9 a |
| ≥80 (n = 47) | 83.3 ± 2.8 | 25.5 ± 4.3 | 39.0 ± 6.8 | 2.8 ± 0.3 | −2.6 ± 1.1 | −2.2 ± 0.6 |
| Men | ||||||
| 18–39 (n = 953) | 30.6 ± 5.8 a | 25.4 ± 4.7 a | 29.1 ± 7.5 a | 1.8 ± 0.4 a | 0.0 ± 1.1 b | −0.1 ± 0.7 c |
| 40–59 (n = 1633) | 49.3 ± 5.5 a | 27.0 ± 4.5 d | 33.2 ± 6.8 a | 2.2 ± 0.3 a | −0.1 ± 1.1 a | −0.2 ± 0.7 a |
| 60–79 (n = 693) | 66.7 ± 4.9 a | 27.3 ± 4.5 | 35.5 ± 6.3 | 2.6 ± 0.3 a | −0.7 ± 1.6 a | −0.7 ± 0.7 a |
| ≥80 (n = 28) | 82.9 ± 3.4 | 26.4 ± 2.8 | 37.6 ± 4.5 | 2.9 ± 0.2 | −1.7 ± 0.7 | −1.3 ± 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cvijetić, S.; Keser, I.; Boschiero, D.; Ilich, J.Z. Prevalence of Osteosarcopenic Adiposity in Apparently Healthy Adults and Appraisal of Age, Sex, and Ethnic Differences. J. Pers. Med. 2024, 14, 782. https://doi.org/10.3390/jpm14080782
Cvijetić S, Keser I, Boschiero D, Ilich JZ. Prevalence of Osteosarcopenic Adiposity in Apparently Healthy Adults and Appraisal of Age, Sex, and Ethnic Differences. Journal of Personalized Medicine. 2024; 14(8):782. https://doi.org/10.3390/jpm14080782
Chicago/Turabian StyleCvijetić, Selma, Irena Keser, Dario Boschiero, and Jasminka Z. Ilich. 2024. "Prevalence of Osteosarcopenic Adiposity in Apparently Healthy Adults and Appraisal of Age, Sex, and Ethnic Differences" Journal of Personalized Medicine 14, no. 8: 782. https://doi.org/10.3390/jpm14080782
APA StyleCvijetić, S., Keser, I., Boschiero, D., & Ilich, J. Z. (2024). Prevalence of Osteosarcopenic Adiposity in Apparently Healthy Adults and Appraisal of Age, Sex, and Ethnic Differences. Journal of Personalized Medicine, 14(8), 782. https://doi.org/10.3390/jpm14080782







