Thyroid Eye Disease: Advancements in Orbital and Ocular Pathology Management
Abstract
1. Introduction
2. Materials and Methods
3. Thyroid Eye Disease
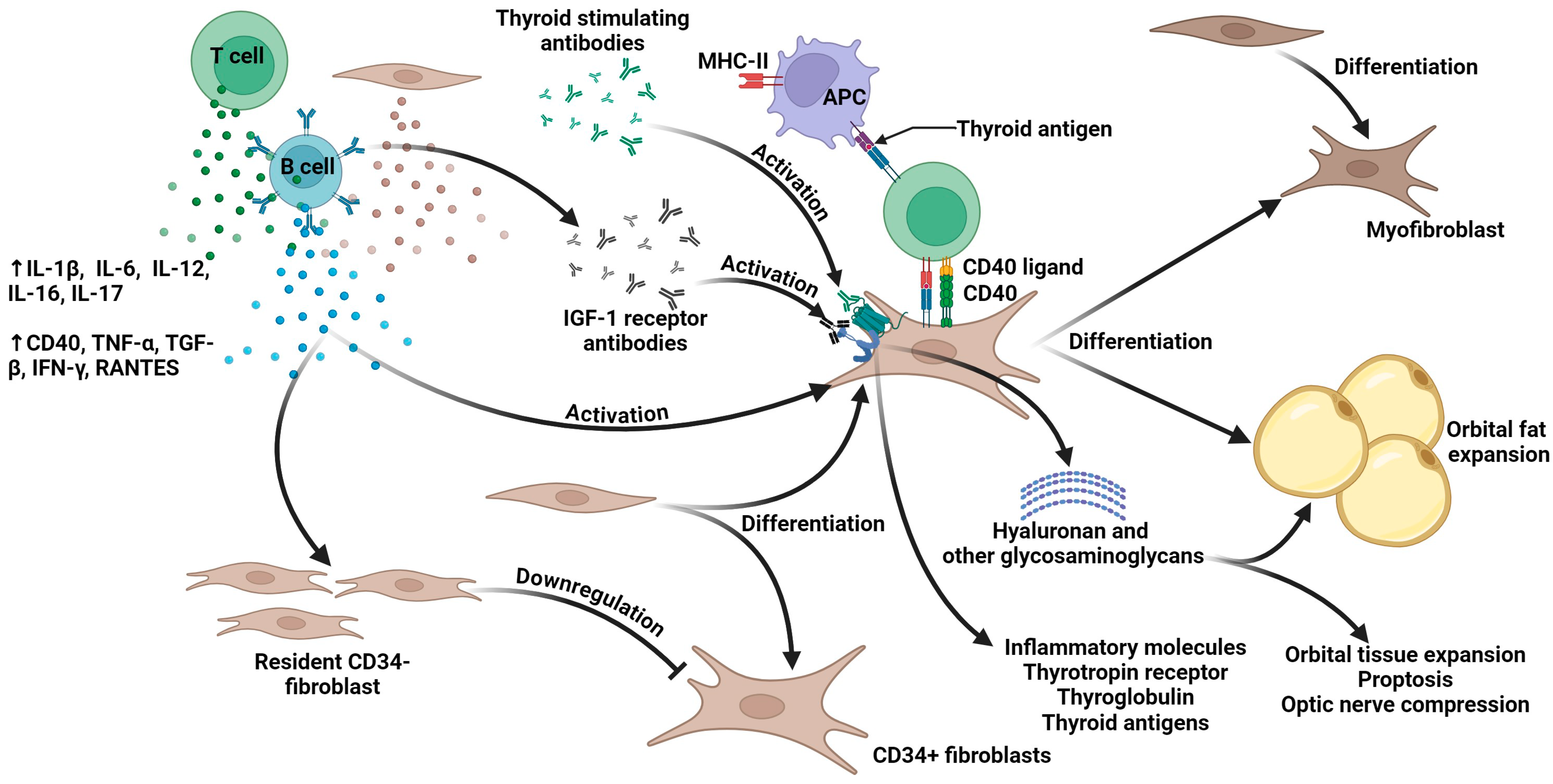
3.1. Pathophysiology
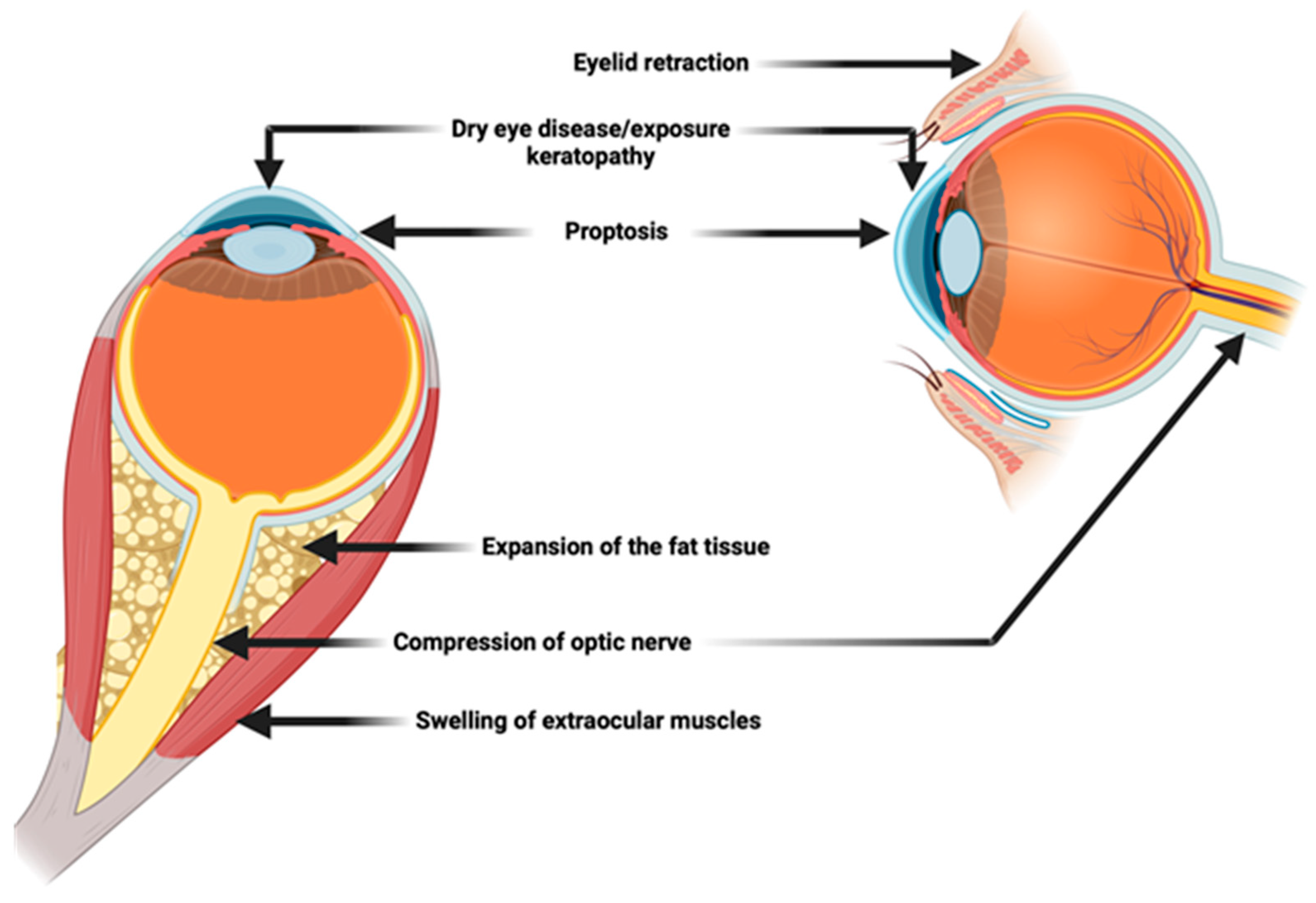
3.2. Clinical Manifestations
3.3. Management
3.3.1. Orbital Decompression Surgery
3.3.2. Eyelid Surgery
3.3.3. Strabismus Surgery
3.3.4. Adjunctive Procedures: Periorbital Fat Management
4. Teprotumumab in Thyroid Eye Disease
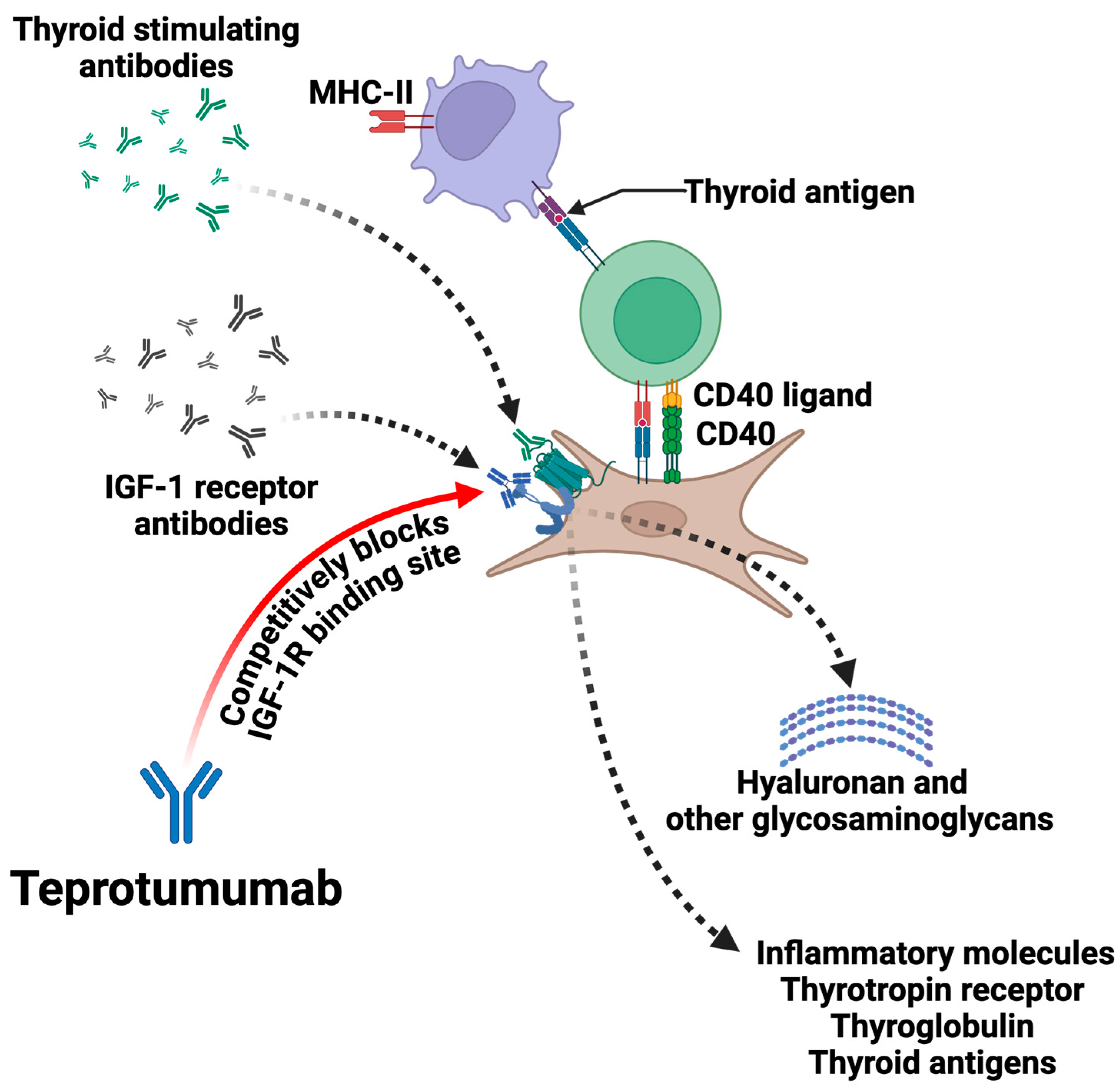
4.1. Mechanism of Action and Efficacy: How Does It Work?
4.2. Indications and Guidelines for Teprotumumab Use
4.3. Potential Adverse Effects and Their Management
4.4. A Huge Limit: The Cost
5. Other Drugs
6. Multidisciplinary Approach
7. Patient Selection and Customized Plans: When to Perform Surgery
8. Future Directions and Emerging Therapeutic Strategies
9. Limitations of the Study
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bahn, R.S. Graves’ Ophthalmopathy. N. Engl. J. Med. 2010, 362, 726–738. [Google Scholar] [CrossRef] [PubMed]
- Weiler, D.L. Thyroid Eye Disease: A Review. Clin. Exp. Optom. 2017, 100, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Vasanthapuram, V.H.; Naik, M.N. Lower Eyelid Entropion in Thyroid Eye Disease. Orbit 2022, 41, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Cypen, S.G.; Conger, J.R.; Chen, L.E.; Tao, J.P. Treatment Options for Lower Eyelid Retraction in Thyroid Eye Disease. Int. Ophthalmol. Clin. 2021, 61, 145–159. [Google Scholar] [CrossRef]
- Naik, M.N.; Walvekar, P.; Vasanthapuram, V.H.; Shankar, L. Eyelid Surgery in Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2023, 39, S92–S104. [Google Scholar] [CrossRef]
- Rosenblatt, T.R.; Chiou, C.A.; Yoon, M.K.; Lee, N.G.; Wolkow, N.; Freitag, S.K. Change in Upper Eyelid Position after Teprotumumab Treatment for Thyroid Eye Disease. Orbit 2024, 10, e4287. [Google Scholar] [CrossRef]
- Ozzello, D.J.; Dallalzadeh, L.O.; Liu, C.Y. Teprotumumab for Chronic Thyroid Eye Disease. Orbit 2022, 41, 539–546. [Google Scholar] [CrossRef]
- Bartalena, L.; Kahaly, G.J.; Baldeschi, L.; Dayan, C.M.; Eckstein, A.; Marcocci, C.; Marinò, M.; Vaidya, B.; Wiersinga, W.M.; Ayvaz, G.; et al. The 2021 European Group on Graves’ Orbitopathy (EUGOGO) Clinical Practice Guidelines for the Medical Management of Graves’ Orbitopathy. Eur. J. Endocrinol. 2021, 185, G43–G67. [Google Scholar] [CrossRef]
- Hoang, T.D.; Stocker, D.J.; Chou, E.L.; Burch, H.B. 2022 Update on Clinical Management of Graves Disease and Thyroid Eye Disease. Endocrinol. Metab. Clin. N. Am. 2022, 51, 287–304. [Google Scholar] [CrossRef]
- Pouso-Diz, J.M.; Abalo-Lojo, J.M.; Gonzalez, F. Thyroid Eye Disease: Current and Potential Medical Management. Int. Ophthalmol. 2020, 40, 1035–1048. [Google Scholar] [CrossRef]
- Kahaly, G.J.; Douglas, R.S.; Holt, R.J.; Sile, S.; Smith, T.J. Teprotumumab for Patients with Active Thyroid Eye Disease: A Pooled Data Analysis, Subgroup Analyses, and off-Treatment Follow-up Results from Two Randomised, Double-Masked, Placebo-Controlled, Multicentre Trials. Lancet Diabetes Endocrinol. 2021, 9, 360–372. [Google Scholar] [CrossRef]
- Tran, L.; Klainguti, G.; Hoeckele, N.; Kaeser, P.F. Torsional Strabismus and Vertical Rectus Muscle Surgery in Thyroid Eye Disease. J. Fr. Ophtalmol. 2023, 46, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Bernardini, F.P.; Skippen, B.; Zambelli, A.; Riesco, B.; Devoto, M.H. Simultaneous Aesthetic Eyelid Surgery and Orbital Decompression for Rehabilitation of Thyroid Eye Disease: The One-Stage Approach. Aesthet. Surg. J. 2018, 38, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- Araya, J.; Sabharwal, S.; Briceño, C.A. Surgery in Thyroid Eye Disease. Int. Ophthalmol. Clin. 2023, 63, 91–107. [Google Scholar] [CrossRef] [PubMed]
- Barbesino, G.; Salvi, M.; Freitag, S.K. Future Projections in Thyroid Eye Disease. J. Clin. Endocrinol. Metab. 2022, 107, S47–S56. [Google Scholar] [CrossRef] [PubMed]
- Moledina, M.; Damato, E.M.; Lee, V. The Changing Landscape of Thyroid Eye Disease: Current Clinical Advances and Future Outlook. Eye 2024, 38, 1425–1437. [Google Scholar] [CrossRef] [PubMed]
- Perros, P.; Hegedüs, L. Teprotumumab in Thyroid Eye Disease: Wonder Drug or Great Divider? Eur. Thyroid. J. 2023, 12, e230043. [Google Scholar] [CrossRef] [PubMed]
- Spadaro, J.Z.; Kohli, A.A. Pathogenesis of Thyroid Eye Disease. Int. Ophthalmol. Clin. 2023, 63, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J. Understanding Pathogenesis Intersects With Effective Treatment for Thyroid Eye Disease. J. Clin. Endocrinol. Metab. 2022, 107, S13–S26. [Google Scholar] [CrossRef] [PubMed]
- Khong, J.J.; McNab, A.A.; Ebeling, P.R.; Craig, J.E.; Selva, D. Pathogenesis of Thyroid Eye Disease: Review and Update on Molecular Mechanisms. Br. J. Ophthalmol. 2016, 100, 142–150. [Google Scholar] [CrossRef]
- Wall, J.R.; Lahooti, H. Pathogenesis of Thyroid Eye Disease—Does Autoimmunity against the TSH Receptor Explain All Cases? Endokrynol. Pol. 2010, 61, 222–227. [Google Scholar] [PubMed]
- Shu, X.; Shao, Y.; Chen, Y.; Zeng, C.; Huang, X.; Wei, R. Immune Checkpoints: New Insights into the Pathogenesis of Thyroid Eye Disease. Front. Immunol. 2024, 15, 1392956. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Hegedüs, L.; Lesser, I.; Perros, P.; Dorris, K.; Kinrade, M.; Troy-Ott, P.; Wuerth, L.; Nori, M. How Patients Experience Thyroid Eye Disease. Front. Endocrinol. 2023, 14, 1283374. [Google Scholar] [CrossRef] [PubMed]
- Qian, L.; Wei, W. Identified Risk Factors for Dry Eye Syndrome: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0271267. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Baek, S. Dry Eye Syndrome in Thyroid Eye Disease Patients: The Role of Increased Incomplete Blinking and Meibomian Gland Loss. Acta Ophthalmol. 2019, 97, e800–e806. [Google Scholar] [CrossRef]
- Lo, C.; Yang, M.; Rootman, D. Natural History of Inflammatory and Non-Inflammatory Dry Eye in Thyroid Eye Disease. Orbit 2021, 40, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Sadeghi, P.B.; Akpek, E.K. Occult Thyroid Eye Disease in Patients Presenting with Dry Eye Symptoms. Am. J. Ophthalmol. 2009, 147, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.; Bunya, V.; Maguire, M.; Asbell, P.; Ying, G.S. Systemic Conditions Associated with Severity of Dry Eye Signs and Symptoms in the Dry Eye Assessment and Management Study. Ophthalmology 2021, 128, 1384–1392. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Lai, K.K.H.; Aljufairi, F.M.A.A.; Chen, W.; Hu, Z.; Wong, H.Y.M.; Jia, R.; Wei, Y.; Tham, C.C.Y.; Pang, C.P.; et al. Ocular Surface Changes in Treatment-Naive Thyroid Eye Disease. J. Clin. Med. 2023, 12, 3066. [Google Scholar] [CrossRef]
- Rana, H.S.; Akella, S.S.; Clabeaux, C.E.; Skurski, Z.P.; Aakalu, V.K. Ocular Surface Disease in Thyroid Eye Disease: A Narrative Review. Ocul. Surf. 2022, 24, 67–73. [Google Scholar] [CrossRef]
- Jones, L.; Downie, L.E.; Korb, D.; Benitez-del-Castillo, J.M.; Dana, R.; Deng, S.X.; Dong, P.N.; Geerling, G.; Hida, R.Y.; Liu, Y.; et al. TFOS DEWS II Management and Therapy Report. Ocul. Surf. 2017, 15, 575–628. [Google Scholar] [CrossRef]
- Lahoti, S.; Weiss, M.; Johnson, D.A.; Kheirkhah, A. Superior Limbic Keratoconjunctivitis: A Comprehensive Review. Surv. Ophthalmol. 2022, 67, 331–341. [Google Scholar] [CrossRef]
- Bron, A.J.; de Paiva, C.S.; Chauhan, S.K.; Bonini, S.; Gabison, E.E.; Jain, S.; Knop, E.; Markoulli, M.; Ogawa, Y.; Perez, V.; et al. TFOS DEWS II Pathophysiology Report. Ocul. Surf. 2017, 15, 438–510. [Google Scholar] [CrossRef]
- Takahashi, Y.; Vaidya, A.; Kakizaki, H. Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease. J. Clin. Med. 2021, 10, 3687. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Ichinose, A.; Kakizaki, H. Topical Rebamipide Treatment for Superior Limbic Keratoconjunctivitis in Patients with Thyroid Eye Disease. Am. J. Ophthalmol. 2014, 157, 807–812. [Google Scholar] [CrossRef]
- Passons, G.A.; Wood, T.O. Conjunctival Resection for Superior Limbic Keratoconjunctivitis. Ophthalmology 1984, 91, 966–968. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Margolis, M.S.; Iovieno, A.; Ling, J.; Ng, T.; Djalilian, A.R.; Yeung, S.N. Superior Limbic Keratoconjunctivitis: Update on Pathophysiology and Management. Ocul. Surf. 2023, 28, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Mourits, M.P.; Prummel, M.F.; Wiersinga, W.M.; Koornneef, L. Clinical Activity Score as a Guide in the Management of Patients with Graves’ Ophthalmopathy. Clin. Endocrinol. 1997, 47, 9–14. [Google Scholar] [CrossRef]
- Ugradar, S.; Rootman, D.B. Noninflammatory Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2019, 35, 461–464. [Google Scholar] [CrossRef]
- Dolman, P.J. Grading Severity and Activity in Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2018, 34, S34–S40. [Google Scholar] [CrossRef]
- Dutton, J.J. Anatomic Considerations in Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2018, 34, S7–S12. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.T.; Jameyfield, E.; Aakalu, V.K. Optic Neuropathy and Diplopia from Thyroid Eye Disease: Update on Pathophysiology and Treatment. Curr. Opin. Neurol. 2021, 34, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Young, S.M.; Kim, Y.D.; Woo, K.I. Course of Upper Eyelid Retraction in Thyroid Eye Disease. Br. J. Ophthalmol. 2020, 104, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, A.B.D.; Couso, R.C.; Matayoshi, S.; Douglas, R.S.; Briceño, C.A. Non-Surgical Treatment for Eyelid Retraction in Thyroid Eye Disease (TED). Br. J. Ophthalmol. 2017, 102, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.P.; Jaru-Ampornpan, P.; Douglas, R.S. Thyroid Eye Disease: Redefining Its Management—A Review. Clin. Exp. Ophthalmol. 2021, 49, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Rootman, D.B. Orbital Decompression for Thyroid Eye Disease. Surv. Ophthalmol. 2018, 63, 86–104. [Google Scholar] [CrossRef] [PubMed]
- Jefferis, J.M.; Jones, R.K.; Currie, Z.I.; Tan, J.H.; Salvi, S.M. Orbital Decompression for Thyroid Eye Disease: Methods, Outcomes, and Complications. Eye 2018, 32, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.A.; Simmons, B.; Potter, N.J.; Al-Qurayshi, Z.; Carter, K.D.; Graham, S.M. Revision Orbital Decompression for Thyroid Eye Disease. Am. J. Otolaryngol.—Head. Neck Med. Surg. 2022, 43, 103196. [Google Scholar] [CrossRef]
- Dallan, I.; Cristofani-Mencacci, L.; Fiacchini, G.; Benettini, G.; Picariello, M.; Lanzolla, G.; Lazzerini, F.; Rocchi, R.; Turri-Zanoni, M.; Menconi, F.; et al. Functional Outcomes and Complications in Refractory Dysthyroid Optic Neuropathy Management: Experience with 3 Different Surgical Protocols. Am. J. Otolaryngol. 2022, 43, 103451. [Google Scholar] [CrossRef] [PubMed]
- Juniat, V.; Abbeel, L.; Anthony McGilligan, J.; Curragh, D.; Selva, D.; Rajak, S. Endoscopic Orbital Decompression by Oculoplastic Surgeons for Proptosis in Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2019, 35, 590–593. [Google Scholar] [CrossRef]
- Korn, B.S.; Kikkawa, D.O.; Cohen, S.R.; Hartstein, M.; Annunziata, C.C. Treatment of Lower Eyelid Malposition with Dermis Fat Grafting. Ophthalmology 2008, 115, 744–751. [Google Scholar] [CrossRef]
- Osaki, T.H.; Monteiro, L.G.; Osaki, M.H. Management of Eyelid Retraction Related to Thyroid Eye Disease. Taiwan. J. Ophthalmol. 2022, 12, 12–21. [Google Scholar] [CrossRef]
- Boulakh, L.; Nygaard, B.; Bek, T.; Faber, J.; Heegaard, S.; Toft, P.B.; Poulsen, H.E.; Toft-Petersen, A.P.; Hesgaard, H.B.; Ellervik, C. Nationwide Incidence of Thyroid Eye Disease and Cumulative Incidence of Strabismus and Surgical Interventions in Denmark. JAMA Ophthalmol. 2022, 140, 667–673. [Google Scholar] [CrossRef]
- Harrad, R. Management of Strabismus in Thyroid Eye Disease. Eye 2015, 29, 234–237. [Google Scholar] [CrossRef]
- Akbari, M.R.; Mirmohammadsadeghi, A.; Mahmoudzadeh, R.; Veisi, A. Management of Thyroid Eye Disease-Related Strabismus. J. Curr. Ophthalmol. 2020, 32, 1–13. [Google Scholar] [CrossRef]
- Hwang, B.; Heo, H.; Lambert, S.R. Risk Factors for Reoperation after Strabismus Surgery among Patients with Thyroid Eye Disease. Am. J. Ophthalmol. 2022, 238, 10–15. [Google Scholar] [CrossRef]
- Doumit, G.; Abouhassan, W.; Yaremchuk, M.J. Aesthetic Refinements in the Treatment of Graves Ophthalmopathy. Plast. Reconstr. Surg. 2014, 134, 519–526. [Google Scholar] [CrossRef]
- Choudhary, M.M.; Zhang, K.R.; Johnson, S.; Hwang, C.J.; Chon, B.H.; Perry, J.D. Temporal Fat Pad Volume in Patients With Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2020, 36, 194–197. [Google Scholar] [CrossRef]
- Roncevic, R. Correction of Exophthalmos and Eyelid Deformities in Patients with Severe Thyroid Ophthalmopathy. J. Craniofacial Surg. 2008, 19, 628–636. [Google Scholar] [CrossRef]
- Valencia, M.R.P.; Miyazaki, H.; Kakizaki, H.; Takahashi, Y. Thickness of Retro- and Sub-Orbicularis Oculi Fat in Thyroid Eye Disease: Comparison With Controls and Its Influential Factors. Ophthalmic Plast. Reconstr. Surg. 2020, 36, 463–468. [Google Scholar] [CrossRef]
- Rončević, R.; Rončević, D. Surgical Treatment of Severe Dysthyroid Ophthalmopathy—Long-Term Results. J. Cranio-Maxillofac. Surg. 1995, 23, 355–362. [Google Scholar] [CrossRef]
- Smith, T.J.; Kahaly, G.J.; Ezra, D.G.; Fleming, J.C.; Dailey, R.A.; Tang, R.A.; Harris, G.J.; Antonelli, A.; Salvi, M.; Goldberg, R.A.; et al. Teprotumumab for Thyroid-Associated Ophthalmopathy. N. Engl. J. Med. 2017, 376, 1748–1761. [Google Scholar] [CrossRef]
- Douglas, R.S.; Couch, S.; Wester, S.T.; Fowler, B.T.; Liu, C.Y.; Subramanian, P.S.; Tang, R.; Nguyen, Q.T.; Maamari, R.N.; Ugradar, S.; et al. Efficacy and Safety of Teprotumumab in Patients With Thyroid Eye Disease of Long Duration and Low Disease Activity. J. Clin. Endocrinol. Metab. 2024, 109, 25–35. [Google Scholar] [CrossRef]
- Ding, Y.; Yang, S.; Gao, H. Teprotumumab: The Dawn of Therapies in Moderate-to-Severe Thyroid-Associated Ophthalmopathy. Horm. Metab. Res. 2021, 53, 211–218. [Google Scholar] [CrossRef]
- Yu, C.Y.; Keen, J.A.; Shriver, E.M. Teprotumumab. Adv. Ophthalmol. Optom. 2022, 7, 383–400. [Google Scholar] [CrossRef]
- Douglas, R.S.; Kahaly, G.J.; Patel, A.; Sile, S.; Thompson, E.H.Z.; Perdok, R.; Fleming, J.C.; Fowler, B.T.; Marcocci, C.; Marinò, M.; et al. Teprotumumab for the Treatment of Active Thyroid Eye Disease. N. Engl. J. Med. 2020, 382, 341–352. [Google Scholar] [CrossRef]
- Douglas, R.S.; Kahaly, G.J.; Ugradar, S.; Elflein, H.; Ponto, K.A.; Fowler, B.T.; Dailey, R.; Harris, G.J.; Schiffman, J.; Tang, R.; et al. Teprotumumab Efficacy, Safety, and Durability in Longer-Duration Thyroid Eye Disease and Re-Treatment: OPTIC-X Study. Ophthalmology 2022, 129, 438–449. [Google Scholar] [CrossRef]
- Toro-Tobon, D.; Rachmasari, K.N.; Bradley, E.A.; Wagner, L.H.; Tooley, A.A.; Stokken, J.K.; Stan, M.N. Medical Therapy in Patients with Moderate to Severe, Steroid-Resistant, Thyroid Eye Disease. Thyroid. 2023, 33, 1237–1244. [Google Scholar] [CrossRef]
- Stan, M.N.; Krieger, C.C. The Adverse Effects Profile of Teprotumumab. J. Clin. Endocrinol. Metab. 2023, 108, E654–E662. [Google Scholar] [CrossRef]
- Hubschman, S.; Sojitra, B.; Ghiam, S.; Sears, C.; Hwangbo, N.; Goldberg, R.A.; Rootman, D.B. Teprotumumab and Orbital Decompression for the Management of Proptosis in Patients With Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2024, 40, 270–275. [Google Scholar] [CrossRef]
- Slentz, D.H.; Nelson, C.C.; Smith, T.J. Teprotumumab: A Novel Therapeutic Monoclonal Antibody for Thyroid-Associated Ophthalmopathy. Expert. Opin. Investig. Drugs 2020, 29, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Sears, C.M.; Azad, A.D.; Amarikwa, L.; Pham, B.H.; Men, C.J.; Kaplan, D.N.; Liu, J.; Hoffman, A.R.; Swanson, A.; Alyono, J.; et al. Hearing Dysfunction After Treatment With Teprotumumab for Thyroid Eye Disease. Am. J. Ophthalmol. 2022, 240, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Keen, J.A.; Correa, T.; Pham, C.; Claussen, A.D.; Hansen, M.R.; Carter, K.D.; Shriver, E.M. Frequency and Patterns of Hearing Dysfunction in Patients Treated with Teprotumumab. Ophthalmology 2024, 131, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Dallalzadeh, L.O.; Ting, M.; Topilow, N.; Robbins, S.L.; Liu, C.Y.; Burkat, C.N.; Korn, B.S.; Kikkawa, D.O. Teprotumumab-Related Cutaneous Hypersensitivity Reactions. Ophthalmic Plast. Reconstr. Surg. 2023, 39, E208–E210. [Google Scholar] [CrossRef] [PubMed]
- Ugradar, S.; Kossler, A.L.; Douglas, R.; Cockerham, K. A Paradigm Shift in the Management of Thyroid Eye Disease How Teprotumumab Has Changed the Therapeutic Interface. J. Neuro-Ophthalmol. 2022, 42, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Allen, R.C.; Bradley, E.A.; Fante, R.G.; Lucarelli, M.J. A Perspective on the Current Role of Teprotumumab in Treatment of Thyroid Eye Disease. Ophthalmology 2021, 128, 1125–1128. [Google Scholar] [CrossRef]
- Xavier, N.F.; Lucena, D.T.; Cruz, A.A.V. Monoclonal Antibodies for the Treatment of Graves Orbitopathy: Precision Medicine? Ophthalmic Plast. Reconstr. Surg. 2023, 39, 307–315. [Google Scholar] [CrossRef]
- Mishra, S.; Maurya, V.K.; Kumar, S.; Ankita; Kaur, A.; Saxena, S.K. Clinical Management and Therapeutic Strategies for the Thyroid-Associated Ophthalmopathy: Current and Future Perspectives. Curr. Eye Res. 2020, 45, 1325–1341. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Hammond, C.L.; Roztocil, E.; Gonzalez, M.O.; Feldon, S.E.; Woeller, C.F. Thinking inside the Box: Current Insights into Targeting Orbital Tissue Remodeling and Inflammation in Thyroid Eye Disease. Surv. Ophthalmol. 2022, 67, 858–874. [Google Scholar] [CrossRef] [PubMed]
- Pampín-Sánchez, R.; Martínez-Mugica-Barbosa, C.; Fonseca-Aizpuru, E.M.; Barbazán-Vázquez, F.J.; Fernández-González, B.; Buznego-Súárez, L. Outcome of Tocilizumab Treatment in Corticosteroid-Resistant Thyroid Eye Disease. Med. Clin. 2023, 160, 113–117. [Google Scholar] [CrossRef]
- Strianese, D. Efficacy and Safety of Immunosuppressive Agents for Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2018, 34, S56–S59. [Google Scholar] [CrossRef]
- Insull, E.A.; Sipkova, Z.; David, J.; Turner, H.E.; Norris, J.H. Early Low-Dose Rituximab for Active Thyroid Eye Disease: An Effective and Well-Tolerated Treatment. Clin. Endocrinol. 2019, 91, 179–186. [Google Scholar] [CrossRef]
- Savino, G.; Mandarà, E.; Gari, M.; Battendieri, R.; Corsello, S.M.; Pontecorvi, A. Intraorbital Injection of Rituximab versus High Dose of Systemic Glucocorticoids in the Treatment of Thyroid-Associated Orbitopathy. Endocrine 2015, 48, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Lanzolla, G.; Maglionico, M.N.; Comi, S.; Menconi, F.; Piaggi, P.; Posarelli, C.; Figus, M.; Marcocci, C.; Marinò, M. Sirolimus as a Second-Line Treatment for Graves’ Orbitopathy. J. Endocrinol. Investig. 2022, 45, 2171–2180. [Google Scholar] [CrossRef]
- Kahaly, G.J.; Riedl, M.; König, J.; Pitz, S.; Ponto, K.; Diana, T.; Kampmann, E.; Kolbe, E.; Eckstein, A.; Moeller, L.C.; et al. Mycophenolate plus Methylprednisolone versus Methylprednisolone Alone in Active, Moderate-to-Severe Graves’ Orbitopathy (MINGO): A Randomised, Observer-Masked, Multicentre Trial. Lancet Diabetes Endocrinol. 2018, 6, 287–298. [Google Scholar] [CrossRef]
- Lanzolla, G.; Sabini, E.; Leo, M.; Menconi, F.; Rocchi, R.; Sframeli, A.; Piaggi, P.; Nardi, M.; Marcocci, C.; Marinò, M. Statins for Graves’ Orbitopathy (STAGO): A Phase 2, Open-Label, Adaptive, Single Centre, Randomised Clinical Trial. Lancet Diabetes Endocrinol. 2021, 9, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Chaganti, S.; Mundy, K.; DeLisi, M.P.; Nelson, K.M.; Harrigan, R.L.; Galloway, R.L.; Landman, B.A.; Mawn, L.A. Assessment of Orbital Computed Tomography (CT) Imaging Biomarkers in Patients with Thyroid Eye Disease. J. Digit. Imaging 2019, 32, 987–994. [Google Scholar] [CrossRef]
- Rana, K.; Juniat, V.; Patel, S.; Selva, D. Extraocular Muscle Enlargement. Graefe’s Arch. Clin. Exp. Ophthalmol. 2022, 260, 3419–3435. [Google Scholar] [CrossRef]
- Tran, C.; Pham, C.M.; Simmons, B.A.; Warner, L.L.; Fuhrmeister, L.J.; Shriver, E.M. Echographic Assessment of Extraocular Muscle Response to Teprotumumab. Ophthalmic Plast. Reconstr. Surg. 2022, 38, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Lima, W.T.A.; Perches, M.; Valera, F.C.P.; Demarco, R.C. Orbital Endoscopic Decompression in Graves Ophthalmopathy. Braz. J. Otorhinolaryngol. 2006, 72, 283–287. [Google Scholar] [CrossRef]
- Tu, Y.; Wu, S.; Pan, Z.; Hu, X.; Zhou, G.; Shi, J.; Xu, M.; Liu, W.; Wu, W. Endoscopic Transconjunctival Deep Lateral Wall Decompression for Thyroid-Associated Orbitopathy: A Minimally Invasive Alternative: Transconjunctival Endoscopic with Wall Decompression for TAO. Am. J. Ophthalmol. 2022, 235, 71–79. [Google Scholar] [CrossRef]
- Park, E.; Lewis, K.; Alghoul, M.S. Comparison of Efficacy and Complications Among Various Spacer Grafts in the Treatment of Lower Eyelid Retraction: A Systematic Review. Aesthet. Surg. J. 2017, 37, 743–754. [Google Scholar] [CrossRef]
- Liao, S.L.; Wei, Y.H. Correction of Lower Lid Retraction Using TarSys Bioengineered Grafts for Graves Ophthalmopathy. Am. J. Ophthalmol. 2013, 156, 38–392. [Google Scholar] [CrossRef]
- Kim, K.Y.; Woo, Y.J.; Jang, S.Y.; Lee, E.J.; Yoon, J.S. Correction of Lower Eyelid Retraction Using Acellular Human Dermis During Orbital Decompression. Ophthalmic Plast. Reconstr. Surg. 2017, 33, 168–172. [Google Scholar] [CrossRef]
- Tao, J.P.; Aakalu, V.K.; Wladis, E.J.; Sobel, R.K.; Freitag, S.K.; Foster, J.A.; Yen, M.T. Bioengineered Acellular Dermal Matrix Spacer Grafts for Lower Eyelid Retraction Repair: A Report by the American Academy of Ophthalmology. Ophthalmology 2020, 127, 689–695. [Google Scholar] [CrossRef]
- Ayabe, R.; Rootman, D.B.; Hwang, C.J.; Ben-Artzi, A.; Goldberg, R. Adalimumab as Steroid-Sparing Treatment of Inflammatory-Stage Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2014, 30, 415–419. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarabosio, A.; Surico, P.L.; Singh, R.B.; Tereshenko, V.; Musa, M.; D’Esposito, F.; Russo, A.; Longo, A.; Gagliano, C.; Agosti, E.; et al. Thyroid Eye Disease: Advancements in Orbital and Ocular Pathology Management. J. Pers. Med. 2024, 14, 776. https://doi.org/10.3390/jpm14070776
Scarabosio A, Surico PL, Singh RB, Tereshenko V, Musa M, D’Esposito F, Russo A, Longo A, Gagliano C, Agosti E, et al. Thyroid Eye Disease: Advancements in Orbital and Ocular Pathology Management. Journal of Personalized Medicine. 2024; 14(7):776. https://doi.org/10.3390/jpm14070776
Chicago/Turabian StyleScarabosio, Anna, Pier Luigi Surico, Rohan Bir Singh, Vlad Tereshenko, Mutali Musa, Fabiana D’Esposito, Andrea Russo, Antonio Longo, Caterina Gagliano, Edoardo Agosti, and et al. 2024. "Thyroid Eye Disease: Advancements in Orbital and Ocular Pathology Management" Journal of Personalized Medicine 14, no. 7: 776. https://doi.org/10.3390/jpm14070776
APA StyleScarabosio, A., Surico, P. L., Singh, R. B., Tereshenko, V., Musa, M., D’Esposito, F., Russo, A., Longo, A., Gagliano, C., Agosti, E., Jhanji, E., & Zeppieri, M. (2024). Thyroid Eye Disease: Advancements in Orbital and Ocular Pathology Management. Journal of Personalized Medicine, 14(7), 776. https://doi.org/10.3390/jpm14070776









