The Long Journey towards Personalized Targeted Therapy in Poorly Differentiated Thyroid Carcinoma (PDTC): A Case Report and Systematic Review
Abstract
1. Introduction
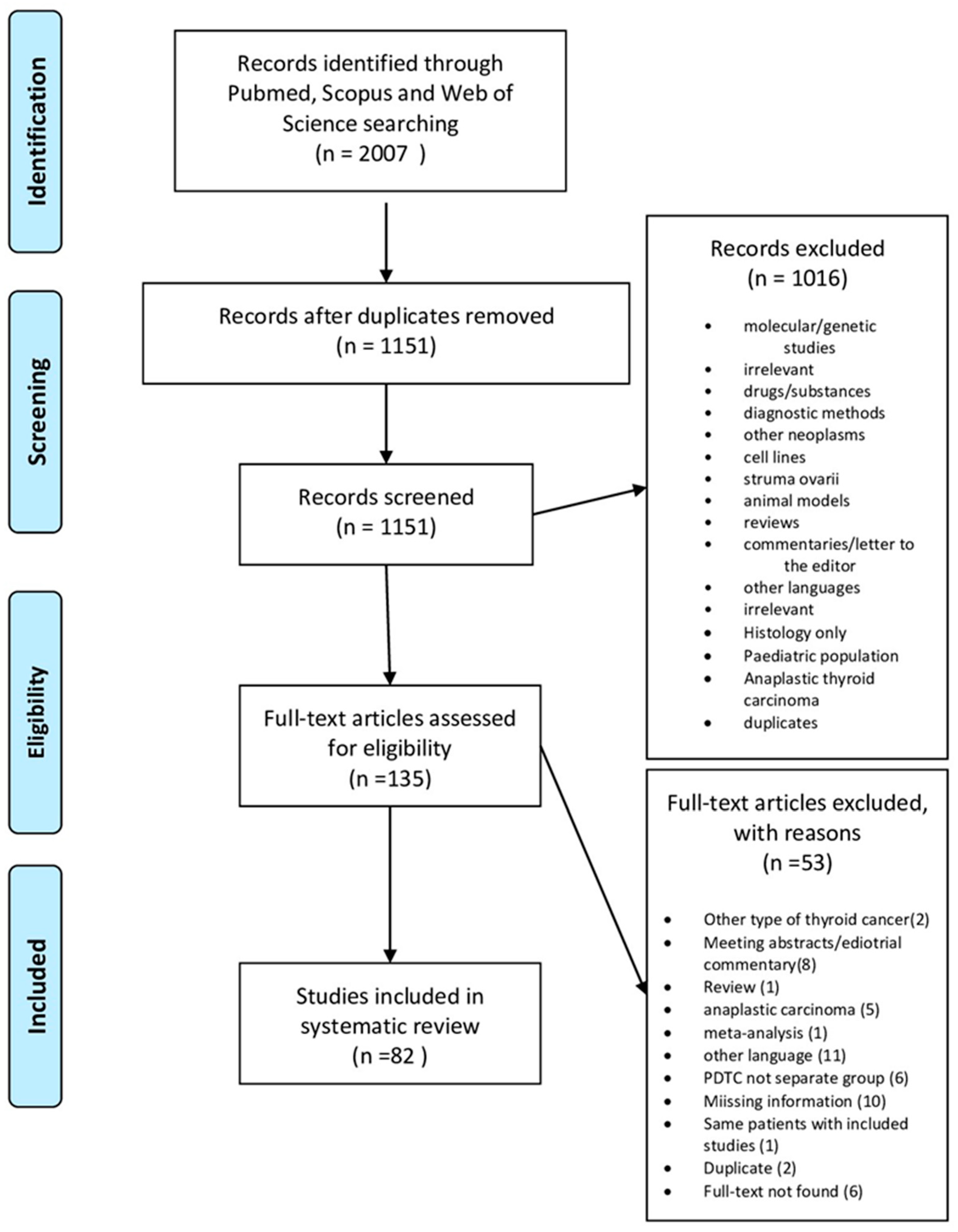
2. Materials and Methods
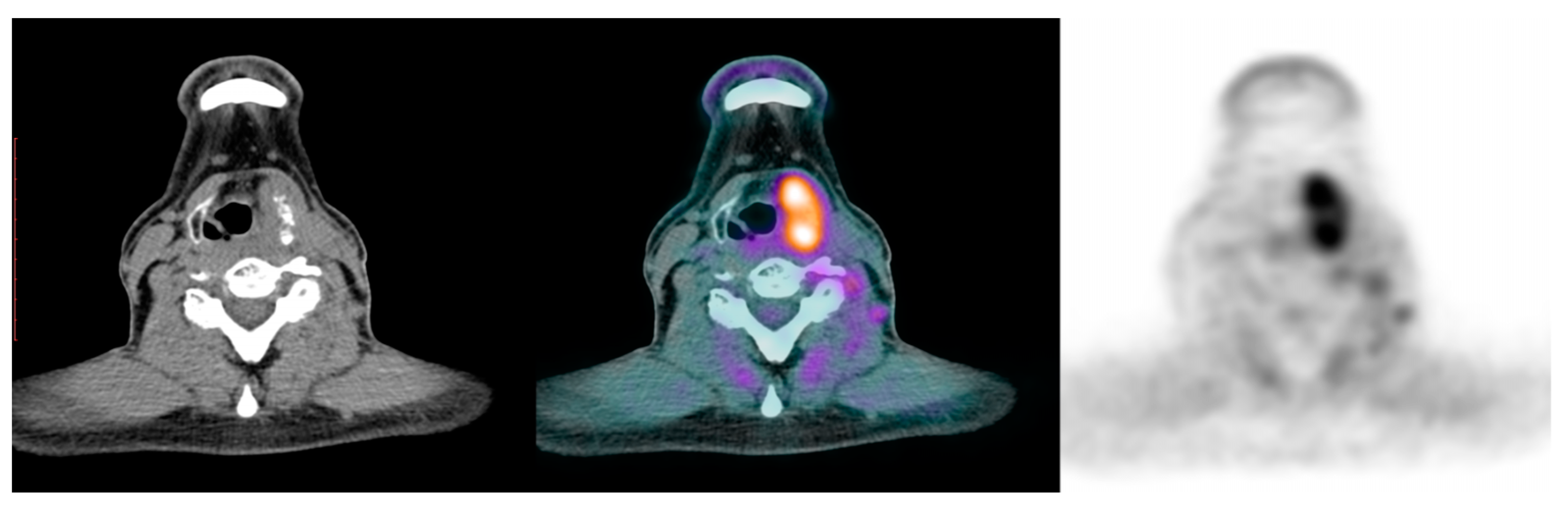
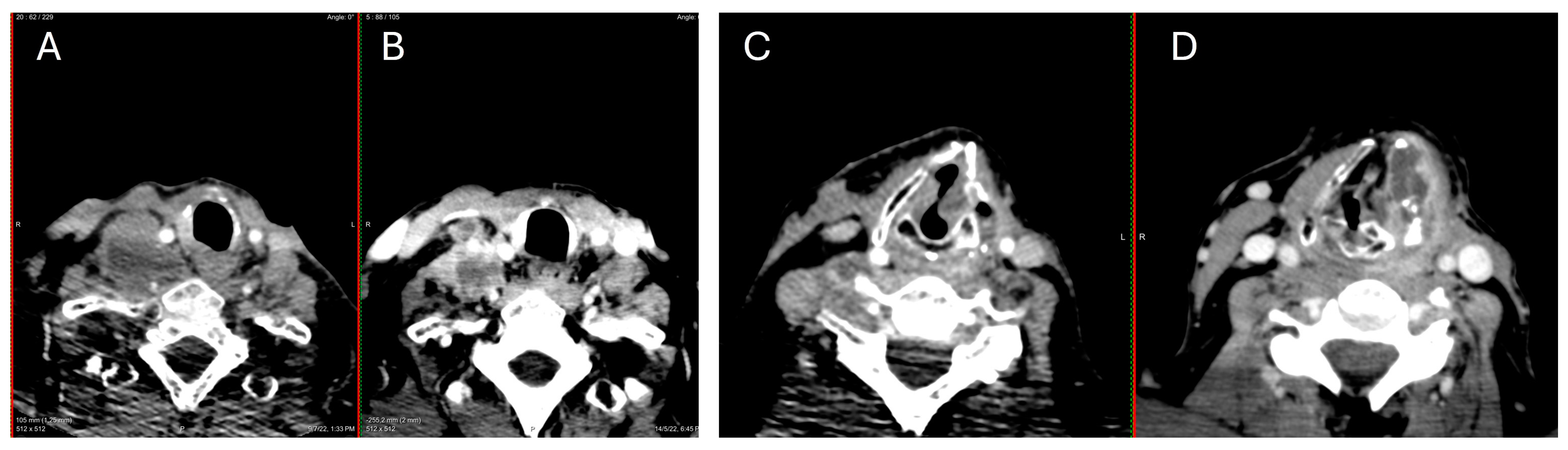
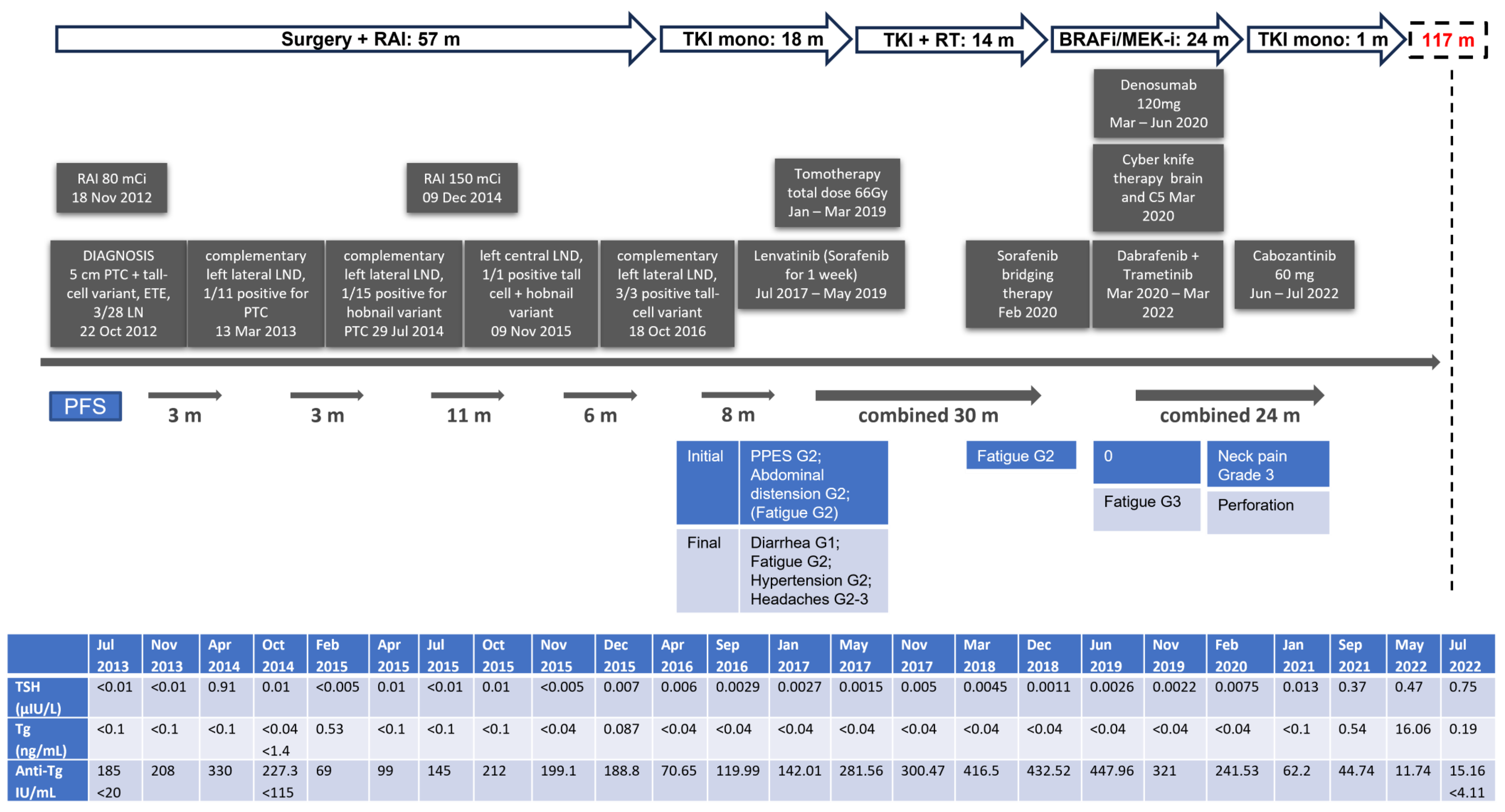
3. Case Presentation
4. Systematic Review Results
5. Discussion
5.1. Age and Sex
5.2. Surgery and RAI Treatment
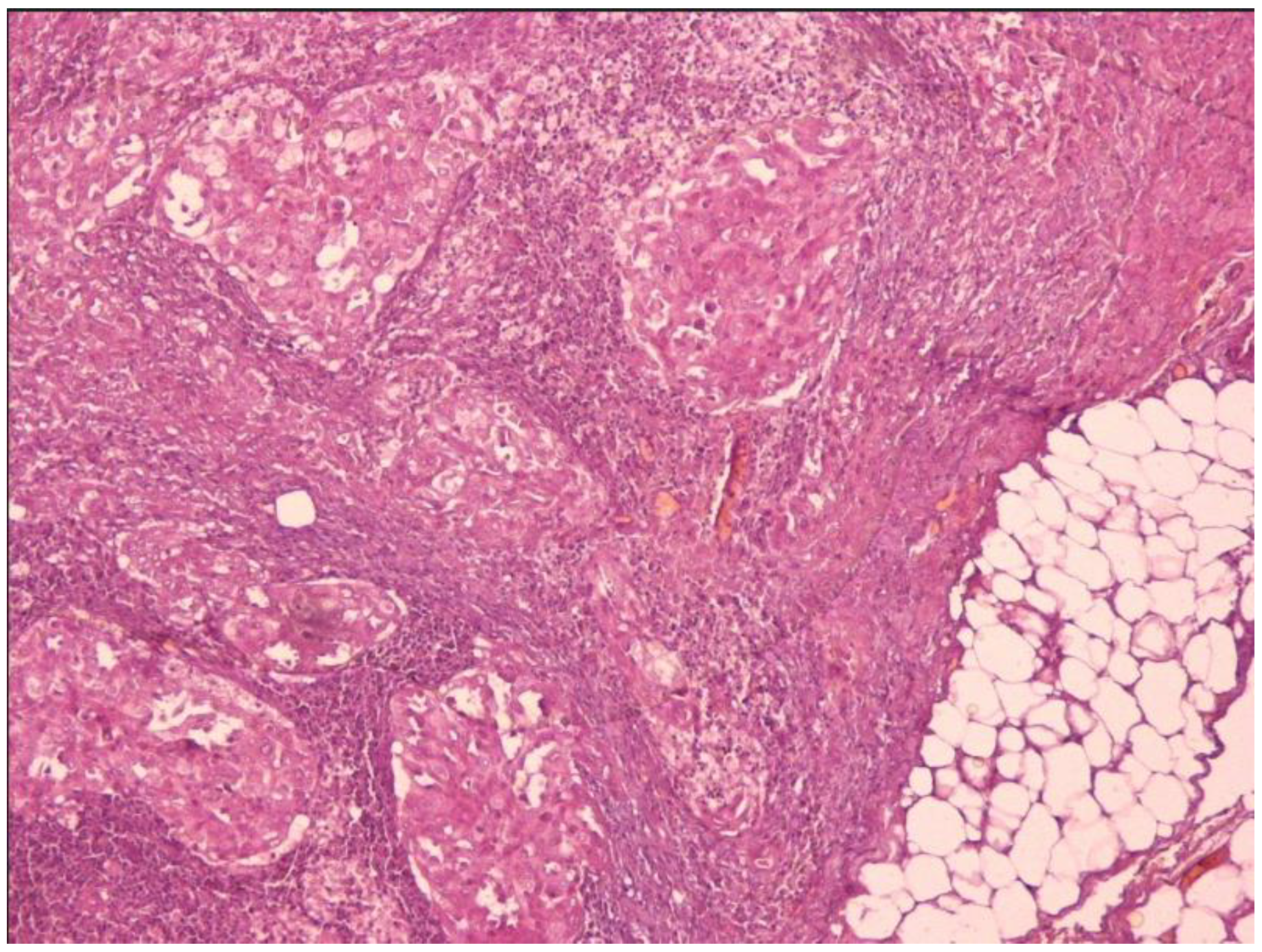
5.3. Histology
5.4. Molecular Events in PDTC
5.5. Survival
5.6. Chemotherapy
5.7. Tyrosine Kinase Inhibitors
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA A Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Seib, C.D.; Sosa, J.A. Evolving Understanding of the Epidemiology of Thyroid Cancer. Endocrinol. Metab. Clin. N. Am. 2018, 48, 23–35. [Google Scholar] [CrossRef]
- Davies, L.; Welch, H.G. Current Thyroid Cancer Trends in the United States. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 317–322. [Google Scholar] [CrossRef]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef]
- Howlader, N.; Noone, A.; Krapcho, M.; Miller, D.; Bishop, K.; Altekruse, S.F.; Kosary, C.L.; Yu, M.; Ruhl, J.; Tatalovich, Z.; et al. (Eds.) Seer Cancer Statistics Review, 1975–2013; National Cancer Institute: Bethesda, MD, USA, 2015.
- La Vecchia, C.; Malvezzi, M.; Bosetti, C.; Garavello, W.; Bertuccio, P.; Levi, F.; Negri, E. Thyroid cancer mortality and incidence: A global overview. Int. J. Cancer 2014, 136, 2187–2195. [Google Scholar] [CrossRef]
- Ahn, H.S.; Kim, H.J.; Welch, H.G. Korea’s thyroid-cancer “epidemic”—Screening and overdiagnosis. N. Engl. J. Med. 2014, 371, 1765–1767. [Google Scholar] [CrossRef]
- Aschebrook-Kilfoy, B.; Ward, M.H.; Sabra, M.M.; Devesa, S.S. Thyroid Cancer Incidence Patterns in the United States by Histologic Type, 1992–2006. Thyroid 2011, 21, 125–134. [Google Scholar] [CrossRef]
- Sanders, E.M., Jr.; LiVolsi, V.A.; Brierley, J.; Shin, J.; Randolph, G.W. An evidence-based review of poorly differentiated thyroid cancer. World J. Surg. 2007, 31, 934–945. [Google Scholar] [CrossRef]
- Asioli, S.; Erickson, L.A.; Righi, A.; Jin, L.; Volante, M.; Jenkins, S.; Papotti, M.; Bussolati, G.; Lloyd, R.V. Poorly differentiated carcinoma of the thyroid: Validation of the Turin proposal and analysis of IMP3 expression. Mod. Pathol. 2010, 23, 1269–1278. [Google Scholar] [CrossRef]
- Molinaro, E.; Romei, C.; Biagini, A.; Sabini, E.; Agate, L.; Mazzeo, S.; Materazzi, G.; Sellari-Franceschini, S.; Ribechini, A.; Torregrossa, L.; et al. Anaplastic thyroid carcinoma: From clinicopathology to genetics and advanced therapies. Nat. Rev. Endocrinol. 2017, 13, 644–660. [Google Scholar] [CrossRef]
- Pereira, M.M.; Williams, V.L.; Johnson, J.H.; Valderrabano, P. Thyroid Cancer Incidence Trends in the United States: Association with Changes in Professional Guideline Recommendations. Thyroid 2020, 30, 1132–1140. [Google Scholar] [CrossRef]
- Schneider, D.F.; Chen, H. New developments in the diagnosis and treatment of thyroid cancer. CA A Cancer J. Clin. 2013, 63, 373–394. [Google Scholar] [CrossRef]
- Singhal, S.; Sippel, R.S.; Chen, H.; Schneider, D.F. Distinguishing classical papillary thyroid microcancers from follicular-variant microcancers. J. Surg. Res. 2014, 190, 151–156. [Google Scholar] [CrossRef][Green Version]
- Englum, B.R.; Pura, J.; Reed, S.D.; Roman, S.A.; Sosa, J.A.; Scheri, R.P. A Bedside Risk Calculator to Preoperatively Distinguish Follicular Thyroid Carcinoma from Follicular Variant of Papillary Thyroid Carcinoma. World J. Surg. 2015, 39, 2928–2934. [Google Scholar] [CrossRef]
- Oyer, S.L.; Fritsch, V.A.; Lentsch, E.J. Comparison of Survival Rates Between Papillary and Follicular Thyroid Carcinomas Among 36,725 Patients. Ann. Otol. Rhinol. Laryngol. 2014, 123, 94–100. [Google Scholar] [CrossRef]
- Lloyd, R.V.; Osamura, R.; Kloppel, G.; Rosai, J. WHO Classification of Tumours of Endocrine Organs, 4th ed.; International Agency for Research on Cancer: Lyon, France, 2017. [Google Scholar]
- Asioli, S.; Erickson, L.A.; Righi, A.; Lloyd, R.V. Papillary thyroid carcinoma with hobnail features: Histopathologic criteria to predict aggressive behavior. Hum. Pathol. 2013, 44, 320–328. [Google Scholar] [CrossRef]
- Asioli, S.; Erickson, L.A.; Sebo, T.J.; Zhang, J.; Jin, L.; Thompson, G.B.; Lloyd, R.V. Papillary Thyroid Carcinoma with Prominent Hobnail Features: A New Aggressive Variant of Moderately Differentiated Papillary Carcinoma. A Clinicopathologic, Immunohistochemical, and Molecular Study of Eight Cases. Am. J. Surg. Pathol. 2010, 34, 44–52. [Google Scholar] [CrossRef]
- Ghossein, R.A.; Leboeuf, R.; Patel, K.N.; Rivera, M.; Katabi, N.; Carlson, D.L.; Tallini, G.; Shaha, A.; Singh, B.; Tuttle, R.M. Tall Cell Variant of Papillary Thyroid Carcinoma without Extrathyroid Extension: Biologic Behavior and Clinical Implications. Thyroid 2007, 17, 655–661. [Google Scholar] [CrossRef]
- Ito, Y.; Hirokawa, M.; Fukushima, M.; Inoue, H.; Yabuta, T.; Uruno, T.; Kihara, M.; Higashiyama, T.; Takamura, Y.; Miya, A.; et al. Prevalence and Prognostic Significance of Poor Differentiation and Tall Cell Variant in Papillary Carcinoma in Japan. World J. Surg. 2008, 32, 1535–1543. [Google Scholar] [CrossRef]
- Wenig, B.M.; Thompson, L.D.; Adair, C.F.; Shmookler, B.; Heffess, C.S. Thyroid papillary carcinoma of columnar cell type: A clinicopathologic study of 16 cases. Cancer 1998, 82, 740–753. [Google Scholar] [CrossRef]
- Chen, J.-H.; Faquin, W.C.; Lloyd, R.V.; Nosé, V. Clinicopathological and molecular characterization of nine cases of columnar cell variant of papillary thyroid carcinoma. Mod. Pathol. 2011, 24, 739–749. [Google Scholar] [CrossRef]
- Chereau, N.; Giudicelli, X.; Pattou, F.; Lifante, J.-C.; Triponez, F.; Mirallié, E.; Goudet, P.; Brunaud, L.; Trésallet, C.; Tissier, F.; et al. Diffuse Sclerosing Variant of Papillary Thyroid Carcinoma Is Associated with Aggressive Histopathological Features and a Poor Outcome: Results of a Large Multicentric Study. J. Clin. Endocrinol. Metab. 2016, 101, 4603–4610. [Google Scholar] [CrossRef]
- Uchino, S.; Ishikawa, H.; Miyauchi, A.; Hirokawa, M.; Noguchi, S.; Ushiama, M.; Yoshida, T.; Michikura, M.; Sugano, K.; Sakai, T. Age- and gender specific risk of thyroid cancer in patients with familial adenomatous polyposis. J. Clin. Endocrinol. Metab. 2016, 101, 4611–4617. [Google Scholar] [CrossRef]
- Lam, A.K.-Y.; Saremi, N. Cribriform-morular variant of papillary thyroid carcinoma: A distinctive type of thyroid cancer. Endocr. Relat. Cancer 2017, 24, R109–R121. [Google Scholar] [CrossRef]
- Hong, J.H.; Yi, H.; Yi, S.; Kim, H.; Lee, J.; Kim, K.S. Implications of oncocytic change in papillary thyroid cancer. Clin. Endocrinol. 2016, 85, 797–804. [Google Scholar] [CrossRef]
- Nilubol, N.; Kebebew, E. Should small papillary thyroid cancer be observed? A population-based study. Cancer 2014, 121, 1017–1024. [Google Scholar] [CrossRef]
- Landa, I.; Cabanillas, M.E. Genomic alterations in thyroid cancer: Biological and clinical insights. Nat. Rev. Endocrinol. 2023, 20, 93–110. [Google Scholar] [CrossRef]
- Brose, M.S.; Cabanillas, M.E.; Cohen, E.E.W.; Wirth, L.J.; Riehl, T.; Yue, H.; Sherman, S.I.; Sherman, E.J. Vemurafenib in patients with BRAFV600E-positive metastatic or unresectable papillary thyroid cancer refractory to radioactive iodine: A non-randomised, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016, 17, 1272–1282. [Google Scholar] [CrossRef]
- Nazarian, R.; Shi, H.; Wang, Q.; Kong, X.; Koya, R.C.; Lee, H.; Chen, Z.; Lee, M.-K.; Attar, N.; Sazegar, H.; et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature 2010, 468, 973–977. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tuttle, R.M.; Haugen, B.; Perrier, N.D. Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System for Differentiated and Anaplastic Thyroid Cancer (Eighth Edition): What Changed and Why? Thyroid 2017, 27, 751–756. [Google Scholar] [CrossRef]
- Spyroglou, A.; Kostopoulos, G.; Tseleni, S.; Toulis, K.; Bramis, K.; Mastorakos, G.; Konstadoulakis, M.; Vamvakidis, K.; Alexandraki, K.I. Hobnail Papillary Thyroid Carcinoma, A Systematic Review and Meta-Analysis. Cancers 2022, 14, 2785. [Google Scholar] [CrossRef]
- Busaidy, N.L.; Konda, B.; Wei, L.; Wirth, L.J.; Devine, C.; Daniels, G.A.; DeSouza, J.A.; Poi, M.; Seligson, N.D.; Cabanillas, M.E. Dabrafenib Versus Dabrafenib + Trametinib in BRAF-Mutated Radioactive Iodine Refractory Differentiated Thyroid Cancer: Results of a Randomized, Phase 2, Open-Label Multicenter Trial. Thyroid 2022, 32, 1184–1192. [Google Scholar] [CrossRef]
- Jeon, Y.; Park, S.; Lee, S.-H.; Kim, T.H.; Kim, S.W.; Ahn, M.-J.; Jung, H.A.; Chung, J.H. Combination of Dabrafenib and Trametinib in Patients with Metastatic BRAFV600E-Mutated Thyroid Cancer. Cancer Res. Treat. 2024. [Google Scholar] [CrossRef]
- Brose, M.S.; Robinson, B.G.; Sherman, S.I.; Jarzab, B.; Lin, C.; Vaisman, F.; Hoff, A.O.; Hitre, E.; Bowles, D.W.; Sen, S.; et al. Cabozantinib for previously treated radioiodine-refractory differentiated thyroid cancer: Updated results from the phase 3 COSMIC-311 trial. Cancer 2022, 128, 4203–4212. [Google Scholar] [CrossRef]
- Abdellaoui, W.; Assarrar, I.; Benyakhlef, S.; Tahri, A.; Messaoudi, N.; Haloui, A.; Rouf, S.; Bennani, A.; Latrech, H. Insular thyroid carcinoma in a young Moroccan man: Case report and review of the literature. Ann. Med. Surg. 2022, 77, 103592. [Google Scholar] [CrossRef]
- Abu Rumman, A.M.; Alsoudi, M.A.; Qasimeh, H.M.; Alnajada, W.A.; Alshunnaq, R.Y. Isolated poorly differentiated cancer (insular) in a thyroglossal cyst: A case report. Pan. Afr. Med. J. 2021, 39. [Google Scholar] [CrossRef]
- Agarwal, A.; George, N.; Kumari, N.; Krishnani, N.; Mishra, P.; Gupta, S. Poorly differentiated thyroid cancer: Clinical, pathological, mutational, and outcome analysis. Indian J. Pathol. Microbiol. 2024. [Google Scholar] [CrossRef]
- Ahmadian, S.S.; Jones, D.; Wakely, P., Jr.; Lott Limbach, A.A. Thyroid poorly differentiated carcinoma metastatic to pancreas diagnosed by fine-needle aspiration and demonstrating a novel BRAF fusion. Cytopathology 2024, 35, 408–411. [Google Scholar] [CrossRef]
- Alshehri, K.; Alqurashi, Y.; Merdad, M.; Samargandy, S.; Daghistani, R.; Marzouki, H. Neoadjuvant lenvatinib for inoperable thyroid cancer: A case report and literature review. Cancer Rep. 2021, 5, e1466. [Google Scholar] [CrossRef]
- Altiner, H.I.; Keskin, H.; Günel, C. Low Differential Thyroid Cancer Metastasizing to the Sphenoid Sinus and Orbital Apex: A Case Report. Eur. J. Rhinol. Allergy 2023, 6, 34–36. [Google Scholar] [CrossRef]
- Alzahrani, A.S.; Alswailem, M.; Alghamdi, B.; Al-Hindi, H. Fumarate Hydratase is a Novel Gene for Familial Non-Medullary Thyroid Cancer. J. Clin. Endocrinol. Metab. 2022, 107, 2539–2544. [Google Scholar] [CrossRef]
- Ambre, S.; Sultania, M.; Biswal, S.; Mitra, S.; Sahoo, B.; Muduly, D.K.; Kar, M. Poorly differentiated “insular” thyroid carcinoma with solitary vascular mandibular metastasis–A rare histology and management. Oral Oncol. 2021, 124, 105416. [Google Scholar] [CrossRef]
- Atif, Z.; Morante, J.; Curiel, L.; Doshi, K.; Babury, M. Hemoptysis as an Initial Presentation of Poorly Differentiated Thyroid Carcinoma: An Ominous Presentation. Am. J. Respir. Crit. Care Med. 2018, 197, A4152. [Google Scholar]
- Bellini, M.I.; Biffoni, M.; Patrone, R.; Borcea, M.C.; Costanzo, M.L.; Garritano, T.; Melcarne, R.; Menditto, R.; Metere, A.; Scorziello, C.; et al. Poorly Differentiated Thyroid Carcinoma: Single Centre Experience and Review of the Literature. J. Clin. Med. 2021, 10, 5258. [Google Scholar] [CrossRef]
- Bertrand, A.-S.; Iannessi, A.; Peyrottes, I.; Lacout, A.; Thyss, A.; Marcy, P.-Y. Myoma Hot Spot: Tumor-to-Tumor Metastasis of Thyroid Origin into Uterine Leiomyoma. Eur. Thyroid. J. 2019, 8, 273–277. [Google Scholar] [CrossRef]
- Beute, J.E.; Silberzweig, A.M.; Gold, B.S.; Shaari, A.L.; Kapustin, D.A.; Matloob, A.; Dowling, E.M.; Starc, M.T.; Fan, J.; Khorsandi, A.S.; et al. Thyroid cancer necrosis not evident on imaging: A cautionary case series on poorly differentiated thyroid carcinoma diagnosed only on final pathology. Am. J. Otolaryngol. 2024, 45, 104054. [Google Scholar] [CrossRef]
- Bicho, R.A.; Mishra, A.; Kumari, N.; Krishnani, N.; Chand, G.; Agarwal, G.; Agarwal, A.; Mishra, S.K. Poorly differentiated thyroid carcinoma and poorly differentiated area in differentiated thyroid carcinoma: Is there any difference? Langenbecks Arch. Surg. 2019, 404, 45–53. [Google Scholar] [CrossRef]
- Elsheikh, M.; Hemmings, C.B.; Rastogi, N.; Schultz, A.; Brijmohan, S.H. Unusual Clinical Manifestations of Thyroid Carcinoma. Cureus 2023, 15, e37474. [Google Scholar] [CrossRef]
- Ching, D.; Leslie, C. Atypical Features Resembling Poorly Differentiated Thyroid Carcinoma Presenting Entirely within a Follicular Adenoma. Case Rep. Pathol. 2018, 2018, 7290343. [Google Scholar] [CrossRef]
- Choi, J.H.; Hong, Y.O.; Kim, H.-J.; Jung, A.R. Poorly differentiated thyroid carcinoma arising from a lithium-induced goiter in a patient with schizophrenia: A case report. Thyroid. Res. 2021, 14, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Lee, J.-H.; Kim, Y.Y.; Chung, Y.S.; Choi, S.; Kim, N.R.; Kang, J.M.; Park, H.K.; Chun, Y.S. Poorly differentiated thyroid carcinoma: An institutional experience. Korean J. Clin. Oncol. 2020, 16, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Colombo, C.; Pogliaghi, G.; Tosi, D.; Muzza, M.; Bulfamante, G.; Persani, L.; Fugazzola, L.; Cirello, V. Thyroid cancer harboring PTEN and TP53 mutations: A peculiar molecular and clinical case report. Front. Oncol. 2022, 12, 949098. [Google Scholar] [CrossRef] [PubMed]
- Corean, J.; Furtado, L.V.; Kadri, S.; Segal, J.P.; Emerson, L.L. Cribriform-Morular Variant of Papillary Thyroid Carcinoma with Poorly Differentiated Features: A Case Report with Immunohistochemical and Molecular Genetic Analysis. Int. J. Surg. Pathol. 2018, 27, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Das, J.; Ghosh, J.; Zameer, L.; Ray, S. 18F-fluorodeoxyglucose positron emission tomography/computed tomography finding in a rare case of follicular carcinoma of thyroid with rhabdoid morphology. Indian J. Nucl. Med. 2021, 36, 56–58. [Google Scholar] [CrossRef] [PubMed]
- de la Fouchardière, C.; Decaussin-Petrucci, M.; Berthiller, J.; Descotes, F.; Lopez, J.; Lifante, J.-C.; Peix, J.-L.; Giraudet, A.-L.; Delahaye, A.; Masson, S.; et al. Predictive factors of outcome in poorly differentiated thyroid carcinomas. Eur. J. Cancer 2018, 92, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Dettmer, M.S.; Hürlimann, S.; Scheuble, L.; Vassella, E.; Perren, A.; Wicke, C. Cribriform Morular Thyroid Carcinoma-Ultimobranchial Pouch-Related? Deep Molecular Insights of a Unique Case. Endocr. Pathol. 2023, 34, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Dierks, C.; Seufert, J.; Aumann, K.; Ruf, J.; Klein, C.; Kiefer, S.; Rassner, M.; Boerries, M.; Zielke, A.; la Rosee, P.; et al. Combination of Lenvatinib and Pembrolizumab Is an Effective Treatment Option for Anaplastic and Poorly Differentiated Thyroid Carcinoma. Thyroid 2021, 31, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Elshafie, O.; Jain, A.; Bichpuria, S.; Rassou, Y.; Hashmi, S.F.; Khalil, A.B. Calcaneus metastasis: A rare presentation of poorly differentiated thyroid cancer. Endocrinol. Diabetes Metab. Case Rep. 2023, 2023, 23-0103. [Google Scholar] [CrossRef]
- Farahmandfar, F.; Shakeri, S.; Askari, E.; Jafarian, A.H.; Jashmidi, S.T.; Shafiri, S.; Zakavi, S.R. Parotid metastasis as the first presentation of papillary thyroid carcinoma. Iran. J. Nucl. Med. 2020, 28, 42–45. [Google Scholar]
- Feffer, J.B.; Usera, G.L.; Schulman, R.C. Unilateral Exophthalmos Due to Metastasis of Poorly Differentiated Thyroid Carcinoma to The Left Sphenoid Wing with Intra-Orbital Extension. AACE Clin. Case Rep. 2017, 3, e89–e92. [Google Scholar] [CrossRef]
- Gay, S.; Monti, E.; Antonelli, C.T.; Mora, M.; Spina, B.; Ansaldo, G.; Teliti, M.; Comina, M.; Conte, L.; Minuto, M.; et al. Case report: Lenvatinib in neoadjuvant setting in a patient affected by invasive poorly differentiated thyroid carcinoma. Futur. Oncol. 2019, 15 (Suppl. S24), 13–19. [Google Scholar] [CrossRef] [PubMed]
- Gazeu, A.; Lopez, J.; Guyetant, S.; Sobrinho-Simoes, M.; Lifante, J.C.; Cugnet-Anceau, C.; Decaussin-Petrucci, M. Poorly differentiated thyroid carcinoma with pleomorphic giant cells—A case report. Virchows Arch. 2020, 477, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.M.; Hassan, A.; Bashir, H.; Shafiq, W. I-131 Avid Tumor Thrombus in a Case of Poorly Differentiated Thyroid Cancer. Mol. Imaging Radionucl. Ther. 2023, 32, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Goto, H.; Kiyota, N.; Otsuki, N.; Imamura, Y.; Chayahara, N.; Suto, H.; Nagatani, Y.; Toyoda, M.; Mukohara, T.; Nibu, K.-I.; et al. Successful treatment switch from lenvatinib to sorafenib in a patient with radioactive iodine-refractory differentiated thyroid cancer intolerant to lenvatinib due to severe proteinuria. Auris Nasus Larynx 2018, 45, 1249–1252. [Google Scholar] [CrossRef] [PubMed]
- Grawe, F.; Cahya, A.; Fabritius, M.P.; Beyer, L.; Wenter, V.; Ruebenthaler, J.; Geyer, T.; Burgard, C.; Bartenstein, P.; Ilhan, H.; et al. Course of Disease and Clinical Management of Patients with Poorly Differentiated Thyroid Carcinoma. Cancers 2021, 13, 5309. [Google Scholar] [CrossRef] [PubMed]
- Gubbiotti, M.A.; Andrianus, S.; Sakhi, R.; Zhang, Q.; Montone, K.; Jalaly, J.B.; Baloch, Z. Does the presence of capsule influence prognosis in poorly differentiated thyroid carcinoma? Hum. Pathol. 2023, 136, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Gülbahar Ateş, S.; Demiral, B.B.; Ucmak, G. Poorly differentiated thyroid cancer with an extensive tumor thrombus in superior vena cava on 18F-FDG PET/CT: A case report. Med. Nucl. 2024, 48, 161–164. [Google Scholar] [CrossRef]
- Hu, J.; Xu, X.; Wang, S.; Dong, F.; Zhang, X.; Ming, J.; Huang, T. Case Report: Implantation of Dedifferentiated to Poorly Differentiated Thyroid Carcinoma After Endoscopic Thyroid Surgery. Front. Oncol. 2022, 12, 896942. [Google Scholar] [CrossRef]
- Ieni, A.; Fadda, G.; Alario, G.; Pino, A.; Ficarra, V.; Dionigi, G.; Tuccari, G. Metastatic thyroid carcinoma mimicking as a primary neoplasia of the kidney: A case report. Mol. Clin. Oncol. 2021, 15, 268. [Google Scholar] [CrossRef]
- Iravani, A.; Solomon, B.; Pattison, D.A.; Jackson, P.; Kumar, A.R.; Kong, G.; Hofman, M.S.; Akhurst, T.; Hicks, R.J. Mitogen-Activated Protein Kinase Pathway Inhibition for Redifferentiation of Radioiodine Refractory Differentiated Thyroid Cancer: An Evolving Protocol. Thyroid 2019, 29, 1634–1645. [Google Scholar] [CrossRef] [PubMed]
- Isaev, P.A.; Polkin, V.V.; Severskaya, N.V.; Ilyin, A.A.; Plugar, A.K.; Ivanov, S.A.; Kaprin, A.D. Results of treatment of patients with poorly differentiated carcinoma of the thyroid gland. Head Neck Tumors 2023, 12, 17–24. [Google Scholar] [CrossRef]
- Kalshetty, A.; Basu, S. Thyroglobulin "Nonsecretor" Metastatic Poorly Differentiated Thyroid Carcinoma with Noniodine Concentrating Disease and Aggressive Clinical Course: A Clinical Case Series. Indian J. Nucl. Med. 2018, 33, 218–223. [Google Scholar] [PubMed]
- Kersting, D.; Rischpler, C.; Plönes, T.; Aigner, C.; Umutlu, L.; Herrmann, K.; Hautzel, H. Atypical bilateral ventilation/perfusion mismatches in an asymptomatic patient suffering from metastatic thyroid cancer. Eur. J. Hybrid Imaging 2021, 5, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Khetrapal, S.; Rana, S.; Jetley, S.; Jairajpuri, Z. Poorly differentiated carcinoma of thyroid: Case report of an uncommon entity. J. Cancer Res. Ther. 2018, 14, 1142–1144. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.M.; Ahn, A.R.; Hong, Y.T.; Chung, M.J. Primary small cell thyroid carcinoma combined with poorly differentiated thyroid carcinoma, evidence for a common origin: A case report. Oncol. Lett. 2023, 25, 233. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Ahn, J.; Kim, Y.S. Subcutaneous implantation of thyroid carcinoma and benign tissue after thyroidectomy: Report on two cases and review of the current literature. Gland Surg. 2023, 12, 1305–1312. [Google Scholar] [CrossRef] [PubMed]
- Kunte, S.; Sharett, J.; Wei, W.; Nasr, C.; Prendes, B.; Lamarre, E.; Ku, J.; Lorenz, R.R.; Scharpf, J.; Burkey, B.B.; et al. Poorly Differentiated Thyroid Carcinoma: Single Institution Series of Outcomes. Anticancer. Res. 2022, 42, 2531–2539. [Google Scholar] [CrossRef] [PubMed]
- Kut, C.; Liang, A.; Kiess, A.P. A Case of Fistula After Adjuvant External Beam Radiotherapy and Lenvatinib for High-Risk Follicular Thyroid Cancer. In Thyroid Cancer: A Case-Based Approach; Grani, G., Cooper, D.S., Durante, C., Eds.; Springer: Cham, Switzerland, 2020; pp. 249–260. [Google Scholar]
- Laforga, J.B.; Cortés, V.A. Oncocytic poorly differentiated (insular) thyroid carcinoma mimicking metastatic adenocarcinoma. A case report and review of the literature. Diagn. Cytopathol. 2019, 47, 584–588. [Google Scholar] [CrossRef]
- Leboulleux, S.; Dupuy, C.; Lacroix, L.; Attard, M.; Grimaldi, S.; Corre, R.; Ricard, M.; Nasr, S.; Berdelou, A.; Hadoux, J.; et al. Redifferentiation of a BRAF(K601E)-Mutated Poorly Differentiated Thyroid Cancer Patient with Dabrafenib and Trametinib Treatment. Thyroid 2019, 29, 735–742. [Google Scholar] [CrossRef]
- Lee, C.-S.; Miao, E.; Das, K.; Seetharamu, N. Clinical efficacy with dabrafenib and trametinib in a T599_V600insT poorly differentiated metastatic thyroid carcinoma. BMJ Case Rep. 2021, 14, e243264. [Google Scholar] [CrossRef]
- Lukovic, J.; Petrovic, I.; Liu, Z.; Armstrong, S.M.; Brierley, J.D.; Tsang, R.; Pasternak, J.D.; Gomez-Hernandez, K.; Liu, A.; Asa, S.L.; et al. Oncocytic Papillary Thyroid Carcinoma and Oncocytic Poorly Differentiated Thyroid Carcinoma: Clinical Features, Uptake, and Response to Radioactive Iodine Therapy, and Outcome. Front. Endocrinol. 2021, 12, 795184. [Google Scholar] [CrossRef]
- Molinaro, E.; Viola, D.; Viola, N.; Falcetta, P.; Orsolini, F.; Torregrossa, L.; Vagli, P.; Ribechini, A.; Materazzi, G.; Vitti, P.; et al. Lenvatinib Administered via Nasogastric Tube in Poorly Differentiated Thyroid Cancer. Case Rep. Endocrinol. 2019, 2019, 6831237. [Google Scholar] [CrossRef]
- Morvan, J.-B.; Boudin, L.; Metivier, D.; Delarbre, D.; Bouquillon, E.; Thariat, J.; Pascaud, D.; Marcy, P.-Y. Internal Jugular Vein Tumor Thrombus: A Tricky Question for the Thyroid Surgeon. Curr. Oncol. 2022, 29, 9235–9241. [Google Scholar] [CrossRef] [PubMed]
- Nagaoka, R.; Saitou, M.; Nagahama, K.; Okamura, R.; Akasu, H.; Igarashi, T.; Yokoshima, K.; Ohashi, R.; Sugitani, I. Downhill Varices in the Hypopharynx of a Patient with a Large Thyroid Tumor: A Case Report. J. Nippon. Med. Sch. 2023, 90, 408–413. [Google Scholar] [CrossRef] [PubMed]
- O’Donohue, P.; Lisewski, D. Intra-abdominal ectopic metastatic poorly differentiated follicular thyroid cancer. ANZ J. Surg. 2022, 92, 3053–3054. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.; Park, J.H.; Djunadi, T.A.; Shah, Z.; Chung, L.I.-Y.; Chae, Y.K. Deep response to a combination of mTOR inhibitor temsirolimus and dual immunotherapy of nivolumab/ipilimumab in poorly differentiated thyroid carcinoma with PTEN mutation: A case report and literature review. Front. Endocrinol. 2024, 15, 1304188. [Google Scholar] [CrossRef]
- Panchangam, R.B.; Puthenveetil, P.; Mayilvaganan, S. Prognostic Impact of Focal Poorly Differentiated Areas in Follicular Differentiated Thyroid Cancer: Is It a Distinct Entity from Poorly Differentiated Thyroid Cancer? Indian J. Surg. Oncol. 2022, 13, 157–163. [Google Scholar] [CrossRef]
- Peng, X.; Lei, J.; Li, Z.; Zhang, K. Case report: Visibly curative effect of dabrafenib and trametinib on advanced thyroid carcinoma in 2 patients. Front. Oncol. 2023, 12, 1099268. [Google Scholar] [CrossRef]
- Pinto, A.; Drake, T.; Cayci, Z.; Burmeister, L.A. Thyroid Storm with Coma in a Patient with Metastatic Thyroid Carcinoma and Graves Disease: Won the Battle but Lost the War. AACE Clin. Case Rep. 2019, 5, e7–e12. [Google Scholar] [CrossRef]
- Prete, A.; Pieroni, E.; Marrama, E.; Bruschini, L.; Ferrari, M.; Scioti, G.; Aprile, V.; Guarracino, F.; Ambrosini, C.E.; Molinaro, E.; et al. Management of patients with extensive locally advanced thyroid cancer: Results of multimodal treatments. J. Endocrinol. Investig. 2023, 47, 1165–1173. [Google Scholar] [CrossRef]
- Purbhoo, K.; Vangu, M.; Bayat, Z.; Daya, R. A rare case of pituitary gland metastases of poorly differentiated thyroid carcinoma. J. Nucl. Med. 2023, 64, P208. [Google Scholar]
- Raffaelli, M.; Sessa, L.; De Crea, C. Total thyroidectomy with central and lateral neck dissection for poorly differentiated thyroid carcinoma (with video). J. Visc. Surg. 2023, 160, 76–77. [Google Scholar] [CrossRef]
- Roque, J.; Silva, T.N.; Regala, C.; Rodrigues, R.; Leite, V. Outcomes of lenvatinib therapy in poorly differentiated thyroid carcinoma. Eur. Thyroid. J. 2023, 12, e230003. [Google Scholar] [CrossRef]
- Temperley, T.S.; Temperley, H.C.; O’Sullivan, N.J.; Corr, A.; Brennan, I.; Kelly, M.E.; Prior, L. Tracheoesophageal fistula development following radiotherapy and tyrosine kinase inhibitors in a patient with advanced follicular thyroid carcinoma: A case-based review. Ir. J. Med. Sci. 2023, 193, 1143–1147. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Tsukahara, K.; Motohashi, R.; Wakiya, M.; Serizawa, H.; Kurata, A. Thyroid Carcinoma on the Side of the Absent Lobe in a Patient with Thyroid Hemiagenesis. Case Rep. Otolaryngol. 2017, 2017, 4592783. [Google Scholar] [CrossRef]
- Schopper, H.K.; Stence, A.; Ma, D.; Pagedar, N.A.; Robinson, R.A. Single thyroid tumour showing multiple differentiated morphological patterns and intramorphological molecular genetic heterogeneity. J. Clin. Pathol. 2016, 70, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, S.; Jahanpanah, P.; Divband, G.; Massoudi, T.; Aryana, K. 99m Tc-Octreotide-Avid Brain Mass in A Patient with Poorly Differentiated Papillary Thyroid Carcinoma, Hope in Despair. Nucl. Med. Rev. Cent. East Eur. 2020, 23, 49–50. [Google Scholar]
- Sonavane, S.N.; Upadhye, T.; Basu, S. Sellar-Parasellar and Petrous Bone Metastasis from Differentiated Thyroid Carcinoma: Imaging Characteristics and Follow-Up Profile Post Radioiodine Therapy. World J. Nucl. Med. 2023, 22, 144–149. [Google Scholar] [CrossRef]
- Suehiro, A.; Nagahara, K.; Moritani, S.; Omori, K. Axillary lymph node metastases from thyroid carcinoma: Report of seven cases. Auris Nasus Larynx 2021, 48, 718–722. [Google Scholar] [CrossRef]
- Sugawara, E.; Shibata, Y.; Katsumata, K. Werner syndrome associated with poorly differentiated thyroid carcinoma and systemic sclerosis-like skin manifestations: A case report. Mod. Rheumatol. Case Rep. 2023, 8, 95–100. [Google Scholar] [CrossRef]
- Sukrithan, V.; Kim, L.; Sipos, J.A.; Goyal, A.; Zhou, Y.; Addison, D.; Shah, M.; Konda, B.; Vallakati, A. Coronary Artery and Peripheral Vascular Disease in a Patient with Poorly Differentiated Thyroid Cancer Treated with the Tyrosine Kinase Inhibitor Lenvatinib. Case Rep. Endocrinol. 2023, 2023, 8841696. [Google Scholar] [CrossRef]
- Suman, S.; Basu, S. Solitary Metacarpophalangeal Metastasis from Poorly Differentiated Thyroid Carcinoma: Excellent Tumor Marker and Scan Response to Two Fractions of Radioiodine Therapy. Indian J. Nucl. Med. 2018, 33, 362–363. [Google Scholar] [PubMed]
- Thiagarajan, S.; Yousuf, A.; Shetty, R.; Dhar, H.; Mathur, Y.; Nair, D.; Basu, S.; Patil, A.; Kane, S.; Ghosh-Laskar, S.; et al. Poorly differentiated thyroid carcinoma (PDTC) characteristics and the efficacy of radioactive iodine (RAI) therapy as an adjuvant treatment in a tertiary cancer care center. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 1807–1814. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.D.R. High Grade Differentiated Follicular Cell-Derived Thyroid Carcinoma Versus Poorly Differentiated Thyroid Carcinoma: A Clinicopathologic Analysis of 41 Cases. Endocr. Pathol. 2023, 34, 234–246. [Google Scholar] [CrossRef]
- Toyoshima, M.T.K.; Domingues, R.B.; Soares, I.C.; Danilovic, D.L.S.; Amorim, L.C.; Cavalcante, E.R.C.; Antonacio, F.F.; Roitberg, F.S.R.; Hoff, A.O. Thyroid collision tumor containing oncocytic carcinoma, classical and hobnail variants of papillary carcinoma and areas of poorly differentiated carcinoma. Arq. Bras. Endocrinol. Metabol. 2021, 65, 495–499. [Google Scholar] [CrossRef]
- Tsuji, H.; Yasuoka, H.; Nakamura, Y.; Hirokawa, M.; Hiroshima, T.; Sakamaki, Y.; Miyauchi, A.; Tsujimoto, M. Aggressive cribriform-morular variant of papillary thyroid carcinoma: Report of an unusual case with pulmonary metastasis displaying poorly differentiated features. Pathol. Int. 2018, 68, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Uchida, T.; Yamaguchi, H.; Nagamine, K.; Yonekawa, T.; Nakamura, E.; Shibata, N.; Kawano, F.; Asada, Y.; Nakazato, M. Rapid pleural effusion after discontinuation of lenvatinib in a patient with pleural metastasis from thyroid cancer. Endocrinol. Diabetes Metab. Case Rep. 2019, 2019. [Google Scholar] [CrossRef]
- Wan, Z.; Wang, B.; Yao, J.; Li, Q.; Miao, X.; Jian, Y.; Huang, S.; Lai, S.; Li, C.; Tian, W. Predictive factors and clinicopathological characteristics of outcome in poorly differentiated thyroid carcinoma: A single-institution study. Front. Oncol. 2023, 13, 1102936. [Google Scholar] [CrossRef]
- Xu, B.; Lubin, D.J.; Dogan, S.; Ghossein, R.A.; Viswanathan, K. Significance of oncocytic features in poorly differentiated thyroid carcinoma—A bi-institutional experience. Virchows Arch. 2022, 482, 479–491. [Google Scholar] [CrossRef]
- Xue, F.; Li, D.; Hu, C.; Wang, Z.; He, X.; Wu, Y. Application of intensity-modulated radiotherapy in unresectable poorly differentiated thyroid carcinoma. Oncotarget 2016, 8, 15934–15942. [Google Scholar] [CrossRef]
- Yasuoka, H.; Nakamura, Y.; Hirokawa, M.; Yoshida, K.-I.; Anno, K.; Tori, M.; Tsujimoto, M. A rare case of poorly differentiated thyroid carcinoma probably arising from a nodular goiter. BMC Clin. Pathol. 2017, 17, 9. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Hou, S.; Hou, L.-L.; Pu, C.-C. Clinical characteristics and prognostic nomogram for patients with insular thyroid carcinoma: A population-based analysis. Endocrine 2022, 79, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.G.; Rivera, J.; Jimeno, C. Poorly Differentiated Thyroid Carcinoma: 10-Year Experience in a Southeast Asian Population. Endocrinol. Metab. 2017, 32, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Yuang, K.; Al-Bahadili, H.; Chang, A. An Unexpected Finding of Poorly Differentiated Thyroid Carcinoma in a Toxic Thyroid Nodule. JCEM Case Rep. 2023, 1, luad052. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zheng, S.; Qin, Y.; Chen, X.; Zhou, S. Combination therapy including immune checkpoint inhibitors for anaplastic and poorly differentiated thyroid carcinoma: A promising protocol. J. Biol. Regul. Homeost. Agents 2023, 37, 3115–3122. [Google Scholar]
- Walczyk, A.; Kopczyński, J.; Gąsior-Perczak, D.; Pałyga, I.; Kowalik, A.; Chrapek, M.; Hejnold, M.; Góźdź, S.; Kowalska, A. Poorly differentiated thyroid cancer in the context of the revised 2015 American Thyroid Association Guidelines and the Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System (eighth edition). Clin. Endocrinol. 2018, 91, 331–339. [Google Scholar] [CrossRef]
- Chernock, R.D.; Rivera, B.; Borrelli, N.; Hill, D.A.; Fahiminiya, S.; Shah, T.; Chong, A.-S.; Aqil, B.; Mehrad, M.; Giordano, T.J.; et al. Poorly differentiated thyroid carcinoma of childhood and adolescence: A distinct entity characterized by DICER1 mutations. Mod. Pathol. 2020, 33, 1264–1274. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.; Devesa, S.S.; Sosa, J.A.; Check, D.; Kitahara, C.M. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974–2013. J. Am. Med. Assoc. 2017, 317, 1338–1348. [Google Scholar] [CrossRef] [PubMed]
- Durante, C.; Haddy, N.; Baudin, E.; Leboulleux, S.; Hartl, D.; Travagli, J.P.; Caillou, B.; Ricard, M.; Lumbroso, J.D.; De Vathaire, F.; et al. Long-Term Outcome of 444 Patients with Distant Metastases from Papillary and Follicular Thyroid Carcinoma: Benefits and Limits of Radioiodine Therapy. J. Clin. Endocrinol. Metab. 2006, 91, 2892–2899. [Google Scholar] [CrossRef]
- Lee, J.; Soh, E.Y. Differentiated thyroid carcinoma presenting with distant metastasis at initial diagnosis clinical outcomes and prognostic factors. Ann. Surg. 2010, 251, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Hannallah, J.; Rose, J.; Guerrero, M.A. Comprehensive Literature Review: Recent Advances in Diagnosing and Managing Patients with Poorly Differentiated Thyroid Carcinoma. Int. J. Endocrinol. 2013, 2013, 317487. [Google Scholar] [CrossRef] [PubMed]
- Walczyk, A.; Kowalska, A.; Sygut, J. The clinical course of poorly differentiated thyroid carcinoma (insular carcinoma)–Own observations. Endokrynol. Pol. 2010, 61, 467–473. [Google Scholar] [PubMed]
- Morandi, L.; Righi, A.; Maletta, F.; Rucci, P.; Pagni, F.; Gallo, M.; Rossi, S.; Caporali, L.; Sapino, A.; Lloyd, R.V.; et al. Somatic mutation profiling of hobnail variant of papillary thyroid carcinoma. Endocr. Relat. Cancer 2017, 24, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Hirokawa, M.; Kihara, M.; Takamura, Y.; Kobayashi, K.; Miyauchi, A. The prognostic value of PDTC in a series of PTC patients of the Japanese Society of Thyroid Surgerymade a comparision with risk classification system in Kuma Hospital. Endocr. J. 2012, 59, 817–821. [Google Scholar] [CrossRef]
- Riesco-Eizaguirre, G.; Santisteban, P. ENDOCRINE TUMOURS: Advances in the molecular pathogenesis of thyroid cancer: Lessons from the cancer genome. Eur. J. Endocrinol. 2016, 175, R203–R217. [Google Scholar] [CrossRef]
- Capdevila, J.; Mayor, R.; Mancuso, F.M.; Iglesias, C.; Caratù, G.; Matos, I.; Zafón, C.; Hernando, J.; Petit, A.; Nuciforo, P.; et al. Early evolutionary divergence between papillary and anaplastic thyroid cancers. Ann. Oncol. 2018, 29, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, N.; Akbani, R.; Aksoy, B.A.; Ally, A.; Arachchi, H.; Asa, S.L.; Auman, J.T.; Balasundaram, M.; Balu, S.; Baylin, S.B.; et al. Integrated genomic characterization of papillary thyroid carcinoma. Cell 2014, 159, 676–690. [Google Scholar] [CrossRef]
- Landa, I.; Ibrahimpasic, T.; Boucai, L.; Sinha, R.; Knauf, J.A.; Shah, R.H.; Dogan, S.; Ricarte-Filho, J.C.; Krishnamoorthy, G.P.; Xu, B.; et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Investig. 2016, 126, 1052–1066. [Google Scholar] [CrossRef]
- Pozdeyev, N.; Gay, L.M.; Sokol, E.S.; Hartmaier, R.; Deaver, K.E.; Davis, S.; French, J.D.; Borre, P.V.; LaBarbera, D.V.; Tan, A.C.; et al. Genetic analysis of 779 advanced differentiated and anaplastic thyroid cancers. Clin. Cancer Res. 2018, 24, 3059–3068. [Google Scholar] [CrossRef]
- Zou, M.; Baitei, E.Y.; Alzahrani, A.S.; BinHumaid, F.S.; Alkhafaji, D.; Al-Rijjal, R.A.; Meyer, B.F.; Shi, Y. Concomitant RAS, RET/PTC, or BRAF mutations in advanced stage of papillary thyroid carcinoma. Thyroid 2014, 24, 1256–1266. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Yan, C.; Xiao, J.; Wang, T.; Ling, R. Relevance and clinicopathologic relationship of BRAF V600E, TERT and NRAS mutations for papillary thyroid carcinoma patients in Northwest China. Diagn. Pathol. 2019, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Hwang, T.S.; Choi, Y.L.; Han, H.S.; Kim, W.S.; Jang, M.H.; Kim, S.K.; Yang, J.H. Prognostic Significance of TERT Promoter Mutations in Papillary Thyroid Carcinomas in a BRAF(V600E) Mutation-Prevalent Population. Thyroid 2016, 26, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Qu, S.; Liu, R.; Sheng, C.; Shi, X.; Zhu, G.; Murugan, A.K.; Guan, H.; Yu, H.; Wang, Y.; et al. TERT promoter mutations and their association with BRAFV600E mutation and aggressive clinicopathological characteristics of thyroid cancer. J. Clin. Endocrinol. Metab. 2014, 99, E1130–E1136. [Google Scholar] [CrossRef] [PubMed]
- Vuong, H.G.; Altibi, A.M.A.; Duong, U.N.P.; Hassell, L. Prognostic implication of BRAF and TERT promoter mutation combination in papillary thyroid carcinoma-A meta-analysis. Clin. Endocrinol. 2017, 87, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Xing, M.; Alzahrani, A.S.; Carson, K.A.; Viola, D.; Elisei, R.; Bendlova, B.; Yip, L.; Mian, C.; Vianello, F.; Tuttle, R.M.; et al. Association Between BRAF V600E Mutation and Mortality in Patients with Papillary Thyroid Cancer. JAMA 2013, 309, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Tufano, R.P.; Teixeira, G.V.; Bishop, J.; Carson, K.A.; Xing, M. BRAF mutation in papillary thyroid cancer and its value in tailoring initial treatment: A systematic review and meta-analysis. Medicine 2012, 91, 274–286. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, Y.; Lin, Y.; Liang, J. Radioactive Iodine-Refractory Differentiated Thyroid Cancer and Redifferentiation Therapy. Endocrinol. Metab. 2019, 34, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Jonklaas, J.; Sarlis, N.J.; Litofsky, D.; Ain, K.B.; Bigos, S.T.; Brierley, J.D.; Cooper, D.S.; Haugen, B.R.; Ladenson, P.W.; Magner, J.; et al. Outcomes of Patients with Differentiated Thyroid Carcinoma Following Initial Therapy. Thyroid 2006, 16, 1229–1242. [Google Scholar] [CrossRef]
- Jonklaas, J.; Cooper, D.S.; Ain, K.B.; Bigos, T.; Brierley, J.D.; Haugen, B.R.; Ladenson, P.W.; Magner, J.; Ross, D.S.; Skarulis, M.C.; et al. Radioiodine Therapy in Patients with Stage I Differentiated Thyroid Cancer. Thyroid 2010, 20, 1423–1424. [Google Scholar] [CrossRef]
- Cracolici, V.; Cipriani, N.A. High-Grade Non-Anaplastic Thyroid Carcinomas of Follicular Cell Origin: A Review of Poorly Differentiated and High-Grade Differentiated Carcinomas. Endocr. Pathol. 2023, 34, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Sun, W.; Zhang, Q.; Wang, Z.; Dong, W.; Zhang, D.; Lv, C.; Shao, L.; Zhang, P.; Zhang, H. Clinicopathological Characteristics and Prognosis of Poorly Differentiated Thyroid Carcinoma Diagnosed According to the Turin Criteria. Endocr. Pr. 2021, 27, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Ibrahimpasic, T.; Ghossein, R.; Shah, J.P.; Ganly, I. Poorly Differentiated Carcinoma of the Thyroid Gland: Current Status and Future Prospects. Thyroid 2019, 29, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Brose, M.S.; Nutting, C.M.; Jarzab, B.; Elisei, R.; Siena, S.; Bastholt, L.; de la Fouchardiere, C.; Pacini, F.; Paschke, R.; Shong, Y.K.; et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: A randomised, double-blind, phase 3 trial. Lancet 2014, 384, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Schlumberger, M.; Tahara, M.; Wirth, L.J.; Robinson, B.; Brose, M.S.; Elisei, R.; Habra, M.A.; Newbold, K.; Shah, M.H.; Hoff, A.O.; et al. Lenvatinib versus Placebo in Radioiodine-Refractory Thyroid Cancer. N. Engl. J. Med. 2015, 372, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Hyman, D.M.; Puzanov, I.; Subbiah, V.; Faris, J.E.; Chau, I.; Blay, J.-Y.; Wolf, J.; Raje, N.S.; Diamond, E.L.; Hollebecque, A.; et al. Vemurafenib in Multiple Nonmelanoma Cancers with BRAF V600 Mutations. N. Engl. J. Med. 2015, 373, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Bible, K.C.; Kebebew, E.; Brierley, J.; Brito, J.P.; Cabanillas, M.E.; Clark, T.J., Jr.; Di Cristofano, A.; Foote, R.; Giordano, T.; Kasperbauer, J.; et al. American Thyroid Association Guidelines for Management of Patients with Anaplastic Thyroid Cancer. Thyroid 2021, 31, 337–386. [Google Scholar] [CrossRef]
- Study of Efficacy and Safety of Dabrafenib Plus Trametinib in Previously Treated Patients with Locally Advanced or Metastatic, Radio-Active Iodine Refractory BRAFV600E Mutation-Positive Differentiated Thyroid Cancer. Available online: https://www.novartis.com/clinicaltrials/study/nct04940052 (accessed on 1 May 2024).
- Wirth, L.J.; Tahara, M.; Robinson, B.; Francis, S.; Brose, M.S.; Habra, M.A.; Newbold, K.; Kiyota, N.; Dutcus, C.E.; Mathias, E.; et al. Treatment-Emergent Hypertension and Efficacy in the Phase 3 Study of (E7080) Lenvatinib in Differentiated Cancer of the Thyroid (SELECT). Cancer 2018, 124, 2365–2372. [Google Scholar] [CrossRef]
| Study | n | M/F | Age | Histological Combinations | ETE | Dm | Ln | Surgery | RAI | Systematic Treatment | Outcome | Molecular |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdellaoui, 2022 [38] | 1 | 1/0 | 27 | Insular, solid | 0 | 0 | 0 | Rt HTmy (first), TTmy | 1 | 0 | AND | NA |
| Abu Rumman, 2021 [39] | 1 | 1/0 | 23 | Insular, solid, trabecular (thyroglossal cyst) | * | 0 | 0 | Sistrunk procedure (first), TTmy | 1 | 0 | AND | NA |
| Agarwal, 2024 [40] | 39 | 1/2.9 | 55 (median) | Insular (32), solid (25), trabecular (18), PTC (2), FTC (14) | 67.7% | 57% | 45.1% | TTmy (+lateral dissection 10) | 25.6% (multiple) | 0 | 73% survival (12 m) | BRAF (5), NRAS (9) |
| Ahmadian, 2024 [41] | 1 | 1/0 | 71 | PTC (thyroid), PDTC (pancreas, liver) | 0 | Liver, pancreas, peritoneum, (adrenal glands) | NA | TTmy (+ND) | 1 | NA | NA | AGAP3: BRAF fusion |
| Alshehri K, 2022 [42] | 1 | 0/1 | 56 | PDTC | 1 | Lung, sternal osseous | 0 | TTmy (+central, Rt ND) | 1 | EBRT (15) + (paclitaxel, carboplatin, doxorubicin, sorafenib, lenvatinib) | AWD | HRAS-BCORL1 |
| Altiner, 2023 [43] | 1 | 0/1 | 70 | PDTC | 0 | Lung, rib, orbital | 0 | TTmy, rid resection | 1 | Paclitaxel | AWD | NA |
| Alzahrani, 2022 [44] | 1 | 0/1 | 43 | Insular | 1 | Lung, (adrenal) | 1 | PTmy | 0 | Lenvatinib | AWD | KRAS+ PIC3CA (missense), PICR1 (insertion), FH (nonsense) |
| Ambre, 2022 [45] | 1 | 0/1 | 74 | Insular, trabecular | 0 | Mandible | 0 | TTmy, hemi-mandibulectomy | 0 | 0 | AND | NA |
| Atif, 2018 [46] | 1 | 0/1 | 56 | PDTC | 0 | Lung, bones | 1 | TTmy (+CND) | 1 | KRAS | ||
| Bellini, 2021 [47] | 8 | 3/5 | 54–85 | PDTC, oncocytic | 5/6 | NA | 3/8 | TTmy (6), nodule removal (2), lymphadenectomy (5) | NA | NA | NA | NA |
| Bertrand, 2019 [48] | 1 | 0/1 | 53 | PTC (thyroid), PDTC–trabecular (uterus) | 0 | Lung, bones, uterus | 0 | TTmy (+CND) | 2 | NA | AWD | NA |
| Beute, 2024 [49] | 7 | 3/4 | 30–82 | PDTC (7/7), hobnail (1/7), tall-cell (1/7) | 5/7 | 2/7 | 2/3 | TTmy (4/7), STTmy (2/7), lymphadenectomy (6/7) | 1/1 | EBRT (1/1) | NA | BRAF (1/1) |
| Bichoo, 2019 [50] | 142 | 1/2.1 | 50.9 (mean) | PDTC (27/142), PTC with PDA (27/142), FTC with PDA (88/142) | 51/142 | 75/142 | 43/142 | TTmy (136/142), near total (1/142), HTmy (1/142), debulking (4/142), lymphadenectomy (53/142), resection of metastasis (20/142) | 110/142 | EBRT (30/142), Sorafenib (3/142) | 64% (G1), 85% (G2), 62% (G3) DOD. From those alive: 66% (G1), 50% (G2), 39% (G3) AWD | NA |
| Brijmohan, 2023 [51] | 1 | 1/0 | 68 | PDTC (insular, solid, trabecular), PTC | 1/1 | Liver, bones, scalp | 1/1 | TTmy (+ND) | 1/1 | NA | NA | NA |
| Ching, 2018 [52] | 1 | 0/1 | 44 | PDTC (insular, trabecular) | 0 | 0 | 0 | Rt Tmy (first), TTmy | NA | NA | AND | NA |
| Choi, 2021 [53] | 1 | 0/1 | 61 | PDTC (insular, solid, trabecular) | 0 | 0 | 0 | TTmy | 1 | NA | AND | TERT promoter point mutation |
| Choi, 2020 [54] | 21 | 7/14 | 15–78 | PDTC (insular, trabecular), FC (15/21), PTC (5/21), | 21/21 | 4/21 (lung, bones) | 0 | TTmy (8/21), CTmy (10/21) | 19/21 | 0 | AND (16/21) AWD (5/21) | NA |
| Colombo, 2022 [55] | 1 | 1/0 | 35 | PDTC, FTC | 1 | Lung, liver, adrenal | 1 | TTmy, thoracic surgery | 1 | Sorafenib | DOD | PTEN, p53 |
| Corean, 2019 [56] | 1 | 0/1 | 29 | CMVPTC, PDTC | 0 | 0 | 0 | TTmy | 0 | NA | AND | APC |
| Das, 2021 [57] | 1 | 1/0 | 58 | Poorly differentiated follicular carcinoma with rhabdoid phenotype | 1/1 | Lung | NA | Tracheostomy only | NA | Cisplatin, endoxan, doxorubicin | AWD | NA |
| de la Fouchardière, 2018 [58] | 104 | 40/64 | 12–91 | Insular (93/104), solid (11/104), trabecular (17/104), PTC (59/102), FTC (29/102), Hurthle (14/102) | 40/100 | 17/98 | 11/98 | TTmy (101/104), ND (36/104) | 99/104 (1–6 cycles) | EBRT (9/104), TKIs (21/104) | AND (36/104), AWD (33/104), DOD (35/104) | TERT promoter (24/63), BRAF (3/38), RAS (10/38) |
| Dettmer, 2023 [59] | 1 | 0/1 | 44 | CMTC, PDTC | 0 | 0 | 0 | Rt Tmy (first), TTmy | 1 | 0 | AND | APC, TERT promoter, PIC3CA |
| Dierks, 2021 [60] | 2 | NA | 49/63 | PDTC | 2/2 | 2/2 (bone, lung, liver, kidney) | 2/2 | TTmy (2/2), ND(1/2) | 1/2 (2 cycles) | EBRT (1/2), cisplatin/doxorubicin and carboplatin/paclitaxel (1/2), lenvatinib + pembrolizumab (2/2) | DOD (2/2) | TERT promoter and PTEN (2/2) |
| Elshafie, 2023 [61] | 1 | 0/1 | 60 | PDTC | NA | Bones, lung | 1/1 | TTmy (+centra/left lateral ND) | 1 | EBRT | AWD | NA |
| Farahmandfar, 2020 [62] | 1 | 1/0 | 70 | PTC, PDTC | NA | Parotid, lung, pericardium | 1/1 | TTmy (+CND) | 1 | EBRT, chemo (NA) | DOD | NA |
| Feffer, 2017 [63] | 1 | 0/1 | 55 | PDTC (insular) | NA | Sphenoid bone | 0 | 0 | 0 | EBRT | AWD | NA |
| Gay, 2019 [64] | 1 | 0/1 | 81 | PDTC with focal squamous differentiation | 1/1 | 0 | 0 | TTmy | 1 | EBRT, lenvatinib | AND | NA |
| Gazeu, 2020 [65] | 1 | 0/1 | 43 | PDTC (solid), oncocytic, follicular component | 0 | 0 | 0 | Rt Tmy (first), TTmy | 1 | 0 | AND | 0 |
| Gill, 2023 [66] | 1 | 0/1 | 46 | PDTC | 0 | SVC tumor thrombus | 1 | TTmy | 3 | EBRT | AWD | NA |
| Goto, 2018 [67] | 1 | 0/1 | 75 | PDTC, PTC | NA | Lung | NA | TTmy, ND | 1 | Lenvatinib, sorafenib | AWD | NA |
| Grawe, 2021 [68] | 47 | 21/26 | 57 ± 19 | PDTC | 9/47 | 18/47 | 14/47 | TTmy | 1 (0–3) | Lenvatinib/sorafenib (2/47), EBRT | AND (18/47), AWD (15/47), DOD (14/47) | NA |
| Gubbiotti, 2023 [69] | 65 | 29/36 | 21–85 | PDTC, PTC (52/65), FTC(13/65) | 31/65 | 19/65 (lung, bones, brain) | 11/65 | TTmy (53/65), lobectomy first (11/12) | 42/65 | Chemo (6/65), EBRT (4/65) | DOD (11/65) | HRAS (2/8), NRAS (2/8), BRAF (1/8), TERT promoter (1/8), p53 (2/8), PAX8: PPARy rearrangement (2/8), NSD3:: NUTM1 fusion(1/8) |
| Gülbahar Ateş, 2024 [70] | 1 | 0/1 | 66 | PDTC (solid, insular, trabecular) | 1/1 | Lung, bones, tumor thrombus | 0 | Neck surgery | 0 | EBRT | AWD | NA |
| Hu, 2022 [71] | 1 | 0/1 | 35 | PTC, PDTC | NA | Breast, neck | 1/1 | Endoscopic Tmy (first), TTmy (+bilateral CND), local tumor excision, modified radical ND, partial mastectomy | 0 | Adjuvant therapy (?) | AND | 0 |
| Ieni, 2021 [72] | 1 | 1/0 | 69 | FTC, PDTC | 0 | Kidney | 0 | Partial nephrectomy, TTmy | 0 | 0 | AND | NA |
| Iravani, 2019 [73] | 3 | 0/3 | 45–61 | FTC, PDTC | 3/3 | 3/3 (lung, neck, muscle, bone) | 1/3 | TTmy (3/3), lymphadenectomy (1/3) | 3/3 | Sunitinib, sorafenib (1/3), trametinib (3/3), lenvatinib(2/3) | AWD (3/3) | NRAS (3/3) |
| Isaev, 2022 [74] | 91 | 35/56 | 16–93 | PDTC | 63/91 | 38/91 | 37/91 | TTmy (55/91), extended TTmy (25/91), lobectomy (9/91), subtotal (2/91), ND (59/91) | 67/85 | EBRT (7/85), systemic therapy (11/89) | AWD (40/91), DOD (27/91) | NA |
| Kalshetty, 2018 [75] | 3 | 2/1 | 32–51 | PDTC (3/3), PTC (1/3), focal cribriform (1/3) | 2/3 | 3/3(bone, pleura, neck, lung) | 1/3 | TTmy (3/3), lymphadenectomy (2/3), tumor resection | 2/3 | EBRT (2/3), sorafenib (1/3) | DOD (1/3), AWD(2/3) | NA |
| Kersting, 2021 [76] | 1 | 1/0 | 38 | PDTC | 0 | Lung | 1/1 | NA, metastasectomy | NA | TKIs | AWD | NA |
| Khetrapal, 2018 [77] | 1 | 0/1 | 42 | PDTC | 1/1 | NA | 1/1 | TTmy, CND | NA | NA | NA | NA |
| Kim, 2023 [78] | 1 | 1/0 | 34 | PDTC (solid), SCC | 1/1 | Lung (SCC) | NA | TTmy, ND, lobectomy | NA | Paclitaxel, cisplatin, and etoposide | DOD | ATRX (c.6793G>T), TP53 (c.377A>G) MYCL (c.332G>T) |
| im, 2023 [79] | 1 | 0/1 | 67 | PDTC (neck) | 0 | 0 | 0 | lobectomy + CND (for benign lesion), neck excision | NA | NA | AWD | NA |
| Kunte, 2022 [80] | 23 | 14/9 | 39–89 | PDTC (23/23), PTC(7/23), FTC(7/23) | 18/13 | 7/23 | 8/23 | TTmy (19/23), lymphadenectomy (8/19) | 13/23 | EBRT (2/19), TKIs (sorafenib, lenvatinib, sorafenib, and pazopanib)(6/23) | DOD (12/23) | NRAS, TERT promoter (1/2) |
| Kut, 2020 [81] | 1 | 1/0 | 60 | FTC, PDTC (insular) | 1/1 | Lung | 1/1 | TTmy, lymphadenectomy, neck surgery | 1 | EBRT, TKIs (lenvatinib, pazopanib), pembrolizumab | AWD | TERT promoter |
| Laforga and Cortés, 2019 [82] | 1 | 1/0 | 76 | OV–PDTC | NA | Lung, spleen, bones, liver | 1/1 | TTmy, bilateral ND | 1 | NA | DOD | NA |
| Leboulleux, 2019 [83] | 1 | 0/1 | 59 | PDTC | 1/1 | Lung, bone | 1/1 | 0 | 0 | Dabrafenib and trametinib | AWD | BRAF-K601E mutation |
| Lee, 2021 [84] | 1 | 1/0 | 76 | PDTC | 1/1 | Lung | 1/1 | 0 | 0 | Carboplatin, EBRT, pembrolizumab, lenvatinib, rametinib, dabrafenib | AWD | BRAF T599_V600insT, CDKN2A/B loss, loss of MTAP exons 2–8 and TERT promoter mutation |
| Lukovic, 2021 [85] | 45 | 24/21 | 35.5–83.6 | OV–PDTC | 6/45 | 16/45 | 3/16 | TTmy (21/45), staged Tmy (24/45) | 39/45 | EBRT (4/45), VEGF | NA | NA |
| Molinaro, 2019 [86] | 1 | 0/1 | 65 | PTC, PDTC with squamous cells | 1/1 | 0 | 0 | TTmy | 1 | Lenvatinib | DOD | BRAF V600E |
| Morvan, 2022 [87] | 1 | 0/1 | 58 | PDTC | 1/1 | Bone, IJV tumor thrombus | 0 | TTmy + removal infiltrated portion IJV, ND | 1 | 0 | AND | NA |
| Nagaoka, 2023 [88] | 1 | 1/0 | 70 | PDTC | 1/1 | Bones | 0 | TTmy | 1 | 0 | AWD | NA |
| O’Donohue, 2022 [89] | 1 | 1/0 | 79 | PDTC | 0 | Liver (port hepatis), bones | 0 | TTmy | 0 | Lenvatinib | DOD | |
| Oh, 2024 [90] | 1 | 0/1 | 50 | PDTC | 1/1 | Lung, liver, bones | 1/1 | TTmy | 1 | EBRT, lenvatinib, nivolumab and ipilimumab, cabozantinib, temsirolimus, nivolumab + relatinib | DOD | PTEN L194fs and TP53 F270S |
| Panchangam, 2022 [91] | 61 | 1/1.3–1.6 | 16–81 | PDTC, PTC with PDA | 59–73% | 19–41% | 50–55% | TTmy (52/61), near Tmy (5/61), debulking (4/61) | 29–65% | EBRT (7/61), chemo(1/61) | NA | NA |
| Peng, 2022 [92] | 2 | 0/2 | 72–73 | PDTC, poorly differentiated squamous cell carcinoma | 2/2 | 1/2(lung) | 1/2 | TTmy + ND(Hx PTC) | 3(Hx PTC) | Anlotinib (1/2), dabrafenib, and trametinib (2/2) | DOC (1/2), AWD (1/2) | BRAFV660E (1/2), TERT promoter (1/2) |
| Pinto, 2019 [93] | 1 | 0/1 | 71 | PDTC with a focal papillary and follicular pattern | NA | Lung, bones | 0 | TTmy | 0 | 0 | DOD | NA |
| Prete, 2024 [94] | 2 | 2/0 | 68–69 | PDTC | 1/2 | Lung, IJV + SVC tumor thrombus | 1/2 | TTmy (1/2), thrombectomy (1/2), lymphadenectomy(2/2) | 0 | Lenvatinib (1/2) | DOC (1/2), AWD(1/2) | NA |
| Purbhoo, 2023 [95] | 1 | 0/1 | 51 | PDTC (solid, insular) | 0 | Bone, lung, pituitary gland | 0 | TTmy + CND | NA | NA | AWD | NA |
| Raffaelli, 2023 [96] | 1 | 0/1 | 72 | PDTC | 1/1 | 0 | 1/1 | TTmy + central/ lateral ND | NA | NA | AND | NA |
| Roque, 2023 [97] | 8 | 3/5 | 34–67 | PDTC | NA | 7/8 | NA | Surgery (6/8), metastasis excision (2/8) | 6/8 | EBRT (4/8), paclitaxel and carboplatin (1/8), other TKIS(3/8), lenvatinib(8/8) | AWD (5/8), DOD(3/8) | NA |
| Temperley, 2023 [98] | 1 | 1/0 | 69 | PDTC | 1/1 | 1/1(liver, bones, hilar LN) | 0 | 0 | 0 | Lenvatinib, cabozantinib, EBRT | DOD | NA |
| Sato, 2017 [99] | 1 | 0/1 | 64 | PTC, PDTC | 1/1 | 0 | 0 | total Rt thyroid lobectomy isthmectomy, resection + CND | 1 | NA | AND | NA |
| Schopper, 2017 [100] | 1 | 1/0 | 49 | Conventional PTC, follicular variant of papillary carcinoma, columnar cell carcinoma, clear cell papillary carcinoma, PDCT | 1/1 | 0 | 1/1 | TTmy + L ND | NA | NA | NA | KRAS, BRAF (PDTC) |
| Shakeri, 2020 [101] | 1 | 0/1 | 58 | PDTC | NA | Lung, brain | 1/1 | TTmy + ND | 1/1 | NA | NA | NA |
| Sonavane, 2023 [102] | 1 | 1/0 | 39 | PDTC | 1/1 | Brain, bones, lung | 1/1 | TTmy + CND | 3 | EBRT | AWD | NA |
| Suehiro, 2021 [103] | 6 | 1/5 | 21–67 | PDTC (6/6), PTC (2/6), squamous differentiation (1/6), signet ring differentiation (1/6) | NA | Axillary lymph nodes | NA | TTmy (5/6), CTmy (1/6), ND (6/6), axillary node dissection (6/6) | NA | NA | AWD (2/3), AND (1/3) | NA |
| Sugawar, 2023 [104] | 1 | 0/1 | 36 | PDTC (trabecular) | NA | NA | NA | left lobectomy (first), TTmy | 1 | 0 | AND | NA |
| Sukrithan, 2023 [105] | 1 | 1/0 | 70 s | PDTC | NA | 1/1 | NA | TTmy | 1 | EBRT, lenvatinib | AWD | NA |
| Suman and Basu, 2018 [106] | 1 | 0/1 | 77 | PDTC, FTC (bones) | 0 | Bones | 0 | TTmy + Rt CND | 2 | 0 | AND | NA |
| Thiagarajan, 2020 [107] | 35 | 11/24 | 22–77 | PDTC (solid (10/35), insular (11/35), trabecular (1/35), mixed (6/35)) | 12/35 | 18/35 | 9/35 | completion Tmy (7/35), TTmy (27/35), thyroid bed exploration (1/35), ND(21/53) | 35/35 | EBRT (16/35) | AND (23/35), AWD (10/35), DOD (2/35) | NA |
| Thompson, 2023 [108] | 24 | 11/13 | 58(mean) | PDTC (24/24), PTC (13/24), metastatic SCC to thyroid gland (1/24) | 9/24 | 5/24 | 6/24 | Surgery (lobectomy, Tmy, and/or CTmy) (24/24) | 18/24 | EBRT (5/24), chemo (1/24) | AND (15/24), AWD (3/24), DOD (5/24), DOC(1/24) | NRAS (3/13) TERT+ NRAS (1/13), TERT + NRAS + KAT6B (1/13) NRAS + MUTYH (1/13); NRAS + PALB2 (1/13) PTENdeletion (1/13), WHSC1L1::NUTM1 (1/13), PAX8::PPARγ (1/13) |
| Toyoshima, 2021 [109] | 1 | 0/1 | 63 | Oncocytic carcinoma, PTC (classic and hobnail component), PDTC | 0 | Lung, liver | 1/1 | TTmy, bilateral LN dissection | 1 | EBRT, sorafenib | DOD | NA |
| Tsuji, 2018 [110] | 1 | 0/1 | 26 | CMV–PTC (thyroid), CMV–PTC, PDTC (lung) | NA | Lung | 0 | TTmy, cervical lymph ND, Rt partial lobectomy | 1 | Sorafenib | AWD | NA |
| Uchida, 2019 [111] | 1 | 0/1 | 73 | PDTC | NA | Lung, pleura | 1/1 | 0 | 1/1 | Lenvatinib | DOD | NA |
| Wan, 2023 [112] | 94 | 34/55 | 8–85 | PDTC (94/94), PTC only (20/94), FTC only (17/94), other (34/94) | 83/94 | 23/94 | 78/94 | Tmy (73/95), ND(29/94) | 23/94 | EBRT (26/94), chemo (22/94) | Median OS (m) (min–max) 33(1–170) | NA |
| Xu, 2023 [113] | 210 | 101/109 | 5–87 | PDTC, oncocytic component (79/210) | 132/210 | NA | 39/210 | lobectomy/HTmy (38/210), TTmy/STmy (172/210) | 157/200 | EBRT (90/199), TKIs (67/209), chemo (37/199) | NA | BRAF (6/87), NRAS (35/87), HRAS (4/87), KRAS (3/87), RET (1/87), PPARG (1/60), ALK (1/87), TERT (43/87), PTEN (15/87), TP53 (15/87), EIF1AX (11/87), NF 1(6/87), RBM10 (5/87), ATM (4/87), DNMT3A (4/87), STK11 (4/87), ARID1A (4/87) |
| Xue, 2017 [114] | 5 | 2/3 | 43–76 | PDTC | 5/5 | 2/5 (lung) | 5/5 | unilateral Tmy (1/5) | NA | IMRT (5/5), gemcitabine (1/5), cisplatin (1/5) paclitaxel and cisplatin (4/5) | AWD (2/5), DOD (3/5) | NA |
| Yasuoka, 2017 [115] | 1 | 0/1 | 35 | PDTC (solid, trabecular, microfollicular) | 1/1 | 0 | 0 | L HTmy (+ND), completion Tmy (+CND) | 1 | EBRT | AND | NRASgene |
| Yin, 2023 [116] | 206 | 98/108 | 57.9 ± 15.9 | Insular | 158/200 (T3 + T4) | 53/202 | 66/192 | 193/204 | 155/206 | Chemo (22/206) | 90.3% (1year-OS), 82.0% (2year-OS), 62.2% (5 year-OS), and 42.5%(10 year-OS) | NA |
| Yu, 2017 [117] | 18 | 5/13 | 40–75 | PDTC insular (8/18), trabecular (7/18), solid (3/18) | 8/18 | 5/18 (lung (3/5), bone (2/5)) | 5/18 | TTmy (+neck dissection) (5/18), TTmy only (5/18), subtotal + completion Tmy (2/18), lobectomy completion (1/18), tumor debulking (4/18) | 8/18 | 0 | AND (6/18), AWD (9/18), DOD (3/18) | NA |
| Yuang, 2023 [118] | 1 | 1/0 | 66 | PDTC (solid/trabecular), FTC | NA | 0 | 0 | Rt lobectomy + isthmectomy | 0 | 0 | AND | NA |
| Zhang, 2023 [119] | 2 | 1/1 | <60 (1/2), >60 (1/2) | PDTC, poorly differentiated squamous cell carcinoma | 1/2 | 1/2 (lung, bone, brain) | 2/2 | 0 | EBRT (1/2) | nab-paclitaxel + carboplatin (2/2), toripalimab (2/2) | AWD (1/2), DOD (1/2) | NA |
| PRESENT CASE | 1 | 1/0 | 45 | PDTC, hobnail, tall-cell | 1/1 | 1/1 (brain, bone, sinus) | 1/1 | TTmy (+neck dissection, completion ND) | 2 | Lenvatinib, sorafenib, trametinib/dabrafenib | DOD | BRAF |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Violetis, O.; Konstantakou, P.; Spyroglou, A.; Xydakis, A.; Kekis, P.B.; Tseleni, S.; Kolomodi, D.; Konstadoulakis, M.; Mastorakos, G.; Theochari, M.; et al. The Long Journey towards Personalized Targeted Therapy in Poorly Differentiated Thyroid Carcinoma (PDTC): A Case Report and Systematic Review. J. Pers. Med. 2024, 14, 654. https://doi.org/10.3390/jpm14060654
Violetis O, Konstantakou P, Spyroglou A, Xydakis A, Kekis PB, Tseleni S, Kolomodi D, Konstadoulakis M, Mastorakos G, Theochari M, et al. The Long Journey towards Personalized Targeted Therapy in Poorly Differentiated Thyroid Carcinoma (PDTC): A Case Report and Systematic Review. Journal of Personalized Medicine. 2024; 14(6):654. https://doi.org/10.3390/jpm14060654
Chicago/Turabian StyleVioletis, Odysseas, Panagiota Konstantakou, Ariadni Spyroglou, Antonios Xydakis, Panagiotis B. Kekis, Sofia Tseleni, Denise Kolomodi, Manousos Konstadoulakis, George Mastorakos, Maria Theochari, and et al. 2024. "The Long Journey towards Personalized Targeted Therapy in Poorly Differentiated Thyroid Carcinoma (PDTC): A Case Report and Systematic Review" Journal of Personalized Medicine 14, no. 6: 654. https://doi.org/10.3390/jpm14060654
APA StyleVioletis, O., Konstantakou, P., Spyroglou, A., Xydakis, A., Kekis, P. B., Tseleni, S., Kolomodi, D., Konstadoulakis, M., Mastorakos, G., Theochari, M., Aller, J., & Alexandraki, K. I. (2024). The Long Journey towards Personalized Targeted Therapy in Poorly Differentiated Thyroid Carcinoma (PDTC): A Case Report and Systematic Review. Journal of Personalized Medicine, 14(6), 654. https://doi.org/10.3390/jpm14060654







