Internal and External Validation of Machine Learning Models for Predicting Acute Kidney Injury Following Non-Cardiac Surgery Using Open Datasets
Abstract
1. Introduction
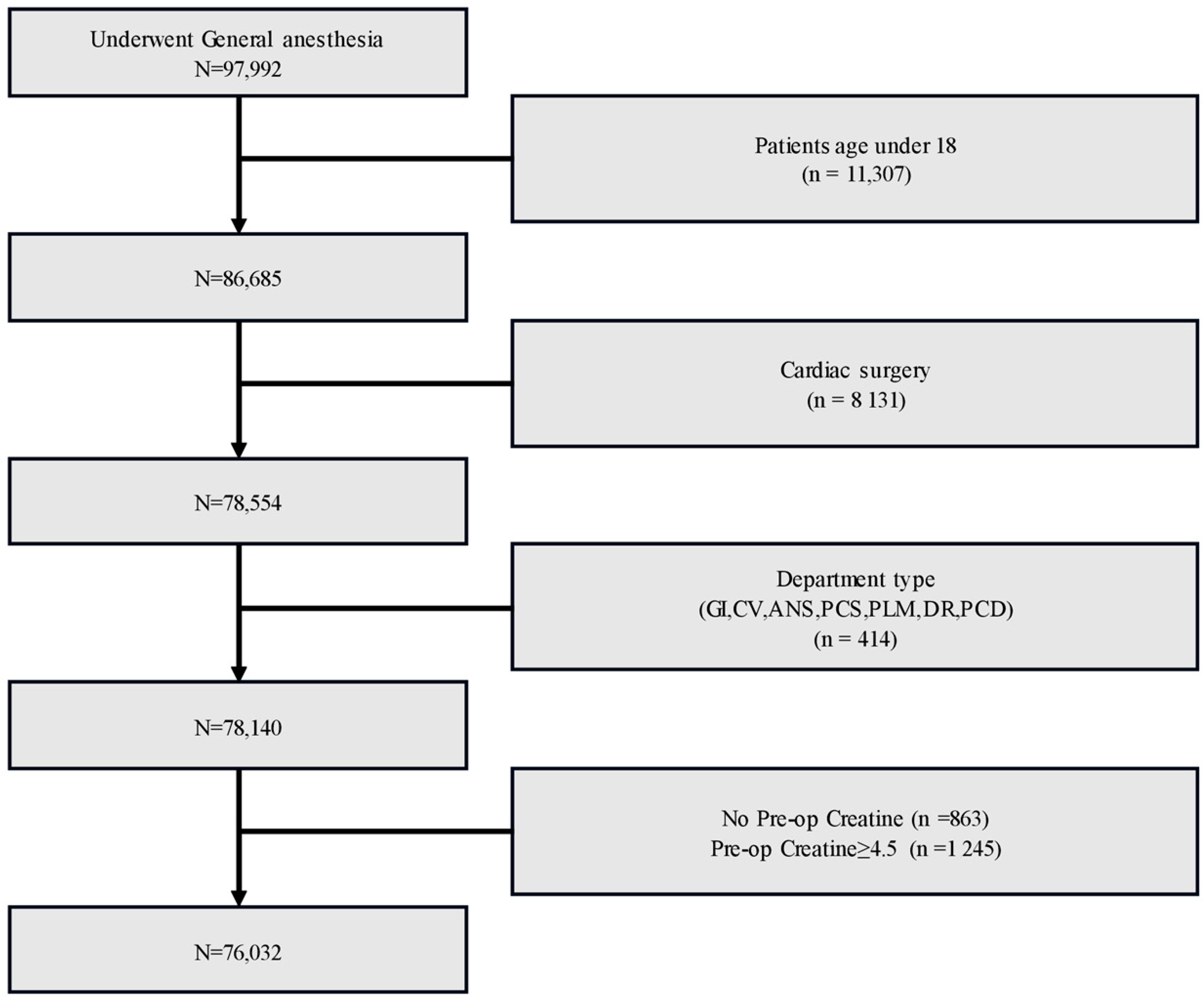
2. Materials and Methods
2.1. Ethical Statement and Study Data
2.2. Variables for Modeling and Preprocessing Data
2.3. Open Dataset for External Validation
2.4. Primary Outcome
2.5. Modeling and Model Evaluation
2.6. Statistical Analysis and Modeling Tools
3. Results
3.1. Study Data Characteristics
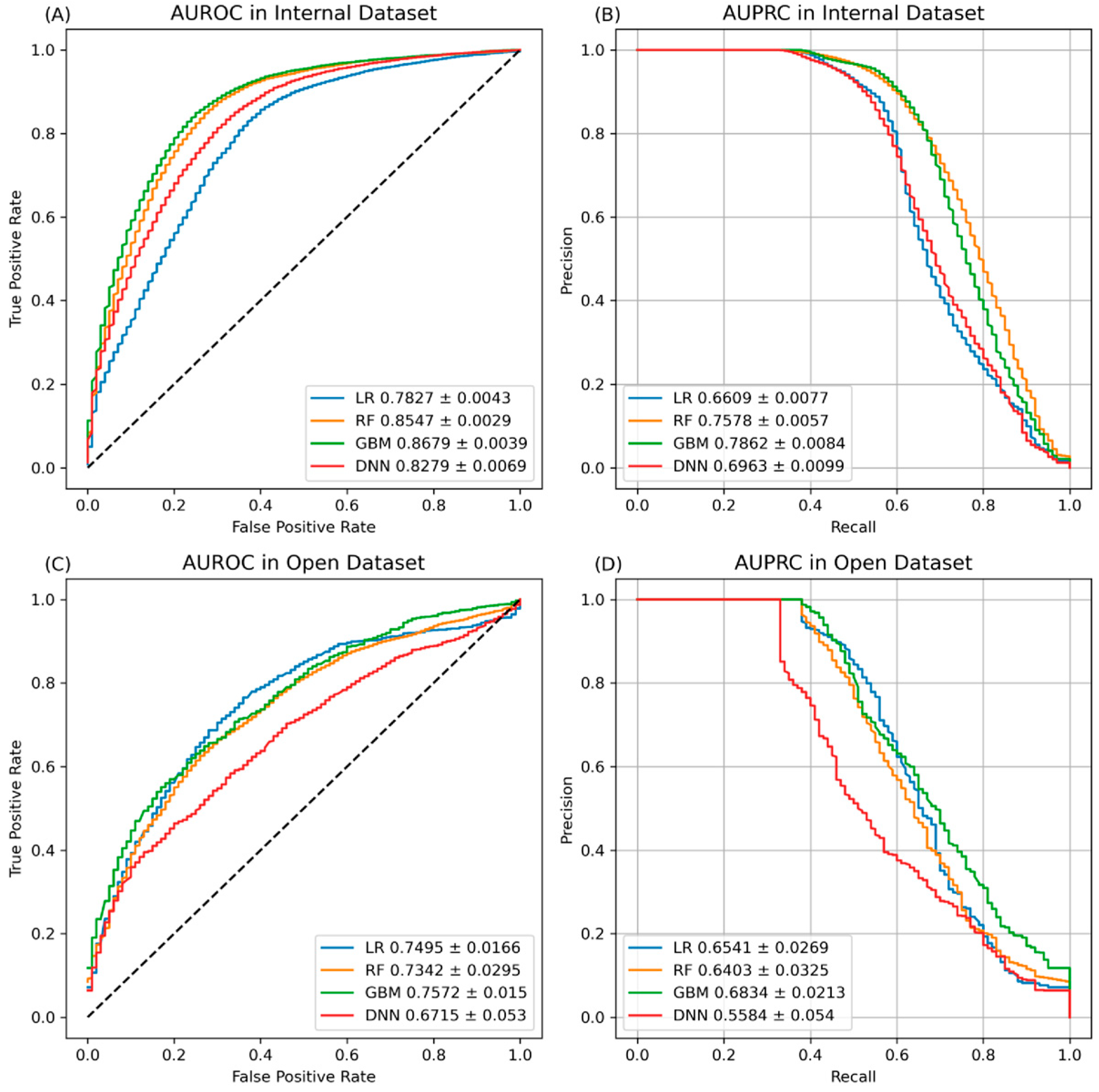
3.2. Predictive Performance Results of Internal and External Validations
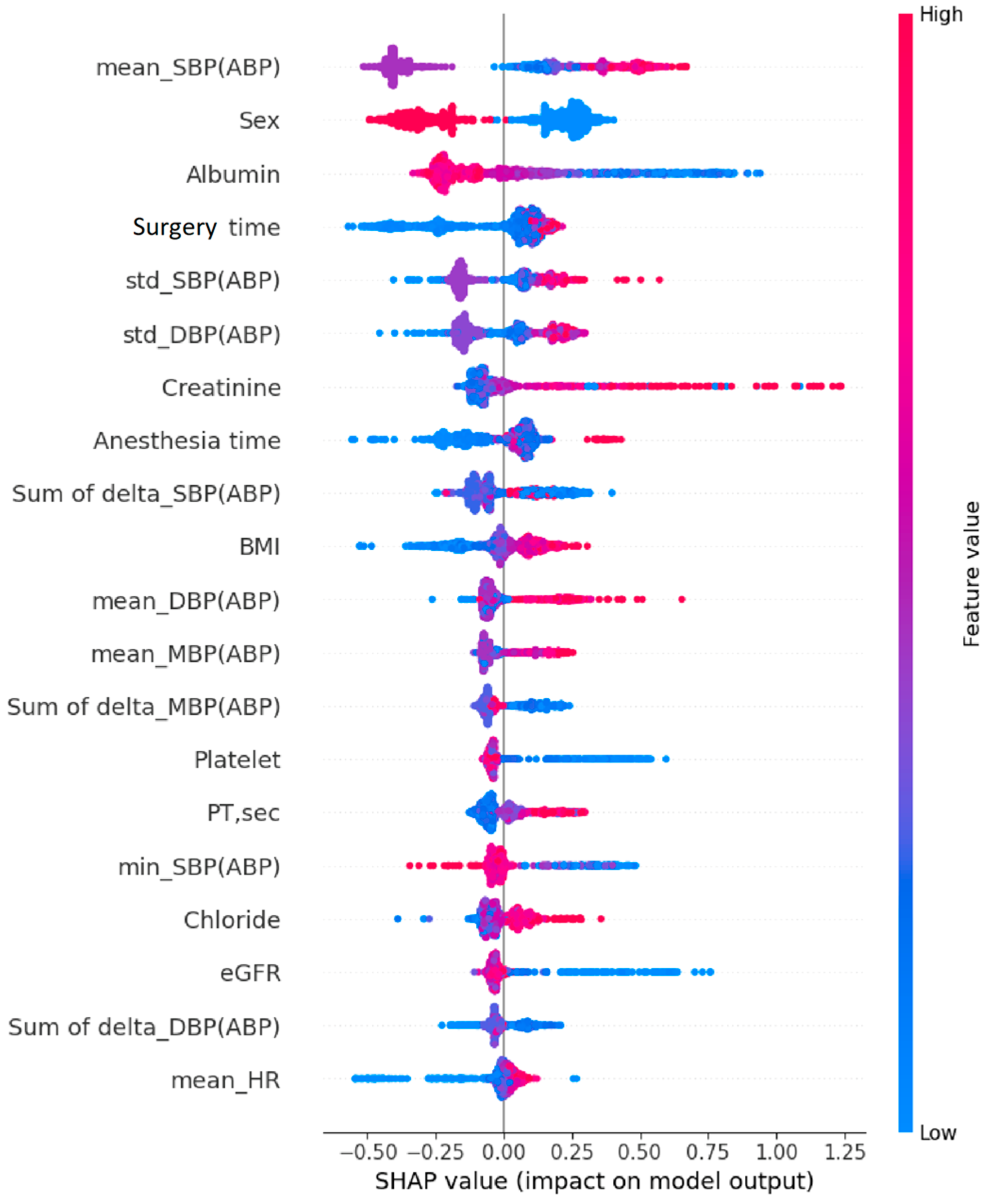
3.3. Feature Importance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoste, E.A.J.; Kellum, J.A.; Selby, N.M.; Zarbock, A.; Palevsky, P.M.; Bagshaw, S.M.; Goldstein, S.L.; Cerda, J.; Chawla, L.S. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol. 2018, 14, 607–625. [Google Scholar] [CrossRef]
- Thakar, C.V. Perioperative acute kidney injury. Adv. Chronic Kidney Dis. 2013, 20, 67–75. [Google Scholar] [CrossRef]
- Chertow, G.M.; Burdick, E.; Honour, M.; Bonventre, J.V.; Bates, D.W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 2005, 16, 3365–3370. [Google Scholar] [CrossRef]
- Hobson, C.; Ozrazgat-Baslanti, T.; Kuxhausen, A.; Thottakkara, P.; Efron, P.A.; Moore, F.A.; Moldawer, L.L.; Segal, M.S.; Bihorac, A. Cost and Mortality Associated with Postoperative Acute Kidney Injury. Ann. Surg. 2015, 261, 1207–1214. [Google Scholar] [CrossRef]
- Biteker, M.; Dayan, A.; Tekkesin, A.I.; Can, M.M.; Tayci, I.; Ilhan, E.; Sahin, G. Incidence, risk factors, and outcomes of perioperative acute kidney injury in noncardiac and nonvascular surgery. Am. J. Surg. 2014, 207, 53–59. [Google Scholar] [CrossRef]
- Cho, E.; Kim, S.C.; Kim, M.G.; Jo, S.K.; Cho, W.Y.; Kim, H.K. The incidence and risk factors of acute kidney injury after hepatobiliary surgery: A prospective observational study. BMC Nephrol. 2014, 15, 169. [Google Scholar] [CrossRef]
- Saran, R.; Robinson, B.; Abbott, K.C.; Agodoa, L.Y.C.; Bhave, N.; Bragg-Gresham, J.; Balkrishnan, R.; Dietrich, X.; Eckard, A.; Eggers, P.W.; et al. US Renal Data System 2017 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2018, 71, A7. [Google Scholar] [CrossRef]
- Karway, G.K.; Koyner, J.L.; Caskey, J.; Spicer, A.B.; Carey, K.A.; Gilbert, E.R.; Dligach, D.; Mayampurath, A.; Afshar, M.; Churpek, M.M. Development and external validation of multimodal postoperative acute kidney injury risk machine learning models. JAMIA Open 2023, 6, ooad109. [Google Scholar] [CrossRef]
- Lei, V.J.; Luong, T.; Shan, E.; Chen, X.; Neuman, M.D.; Eneanya, N.D.; Polsky, D.E.; Volpp, K.G.; Fleisher, L.A.; Holmes, J.H.; et al. Risk Stratification for Postoperative Acute Kidney Injury in Major Noncardiac Surgery Using Preoperative and Intraoperative Data. JAMA Netw. Open 2019, 2, e1916921. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Murugiah, K.; Mahajan, S.; Li, S.X.; Dhruva, S.S.; Haimovich, J.S.; Wang, Y.; Schulz, W.L.; Testani, J.M.; Wilson, F.P.; et al. Enhancing the prediction of acute kidney injury risk after percutaneous coronary intervention using machine learning techniques: A retrospective cohort study. PLoS Med. 2018, 15, e1002703. [Google Scholar] [CrossRef] [PubMed]
- Koyner, J.L.; Carey, K.A.; Edelson, D.P.; Churpek, M.M. The Development of a Machine Learning Inpatient Acute Kidney Injury Prediction Model. Crit. Care Med. 2018, 46, 1070–1077. [Google Scholar] [CrossRef]
- Wu, L.; Hu, Y.; Liu, X.; Zhang, X.; Chen, W.; Yu, A.S.L.; Kellum, J.A.; Waitman, L.R.; Liu, M. Feature Ranking in Predictive Models for Hospital-Acquired Acute Kidney Injury. Sci. Rep. 2018, 8, 17298. [Google Scholar] [CrossRef] [PubMed]
- Salmasi, V.; Maheshwari, K.; Yang, D.; Mascha, E.J.; Singh, A.; Sessler, D.I.; Kurz, A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology 2017, 126, 47–65. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.; Stapelfeldt, W.H.; Khanna, A.K.; Smischney, N.J.; Boero, I.J.; Chen, Q.; Stevens, M.; Shaw, A.D. Intraoperative Hypotension Is Associated with Adverse Clinical Outcomes after Noncardiac Surgery. Anesth. Analg. 2021, 132, 1654–1665. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Park, Y.; Yoon, S.B.; Yang, S.M.; Park, D.; Jung, C.W. VitalDB, a high-fidelity multi-parameter vital signs database in surgical patients. Sci. Data 2022, 9, 279. [Google Scholar] [CrossRef] [PubMed]
- Chertow, G.M.; Levy, E.M.; Hammermeister, K.E.; Grover, F.; Daley, J. Independent association between acute renal failure and mortality following cardiac surgery. Am. J. Med. 1998, 104, 343–348. [Google Scholar] [CrossRef]
- Lok, C.E.; Austin, P.C.; Wang, H.; Tu, J.V. Impact of renal insufficiency on short- and long-term outcomes after cardiac surgery. Am. Heart J. 2004, 148, 430–438. [Google Scholar] [CrossRef]
- Machado, M.N.; Nakazone, M.A.; Maia, L.N. Prognostic value of acute kidney injury after cardiac surgery according to kidney disease: Improving global outcomes definition and staging (KDIGO) criteria. PLoS ONE 2014, 9, e98028. [Google Scholar] [CrossRef] [PubMed]
- Bihorac, A.; Yavas, S.; Subbiah, S.; Hobson, C.E.; Schold, J.D.; Gabrielli, A.; Layon, A.J.; Segal, M.S. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann. Surg. 2009, 249, 851–858. [Google Scholar] [CrossRef]
- Grams, M.E.; Sang, Y.; Coresh, J.; Ballew, S.; Matsushita, K.; Molnar, M.Z.; Szabo, Z.; Kalantar-Zadeh, K.; Kovesdy, C.P. Acute Kidney Injury after Major Surgery: A Retrospective Analysis of Veterans Health Administration Data. Am. J. Kidney Dis. 2016, 67, 872–880. [Google Scholar] [CrossRef]
- Park, J.T. Postoperative acute kidney injury. Korean J. Anesthesiol. 2017, 70, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Ji, Y.; Huang, M.; Feng, Z. Machine learning for acute kidney injury: Changing the traditional disease prediction mode. Front. Med. 2023, 10, 1050255. [Google Scholar] [CrossRef]
- Tomasev, N.; Glorot, X.; Rae, J.W.; Zielinski, M.; Askham, H.; Saraiva, A.; Mottram, A.; Meyer, C.; Ravuri, S.; Protsyuk, I.; et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 2019, 572, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Simonov, M.; Ugwuowo, U.; Moreira, E.; Yamamoto, Y.; Biswas, A.; Martin, M.; Testani, J.; Wilson, F.P. A simple real-time model for predicting acute kidney injury in hospitalized patients in the US: A descriptive modeling study. PLoS Med. 2019, 16, e1002861. [Google Scholar] [CrossRef] [PubMed]
- Koyner, J.L.; Adhikari, R.; Edelson, D.P.; Churpek, M.M. Development of a Multicenter Ward-Based AKI Prediction Model. Clin. J. Am. Soc. Nephrol. 2016, 11, 1935–1943. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, L.E.; Sarnowski, A.; Roderick, P.J.; Dimitrov, B.D.; Venn, R.M.; Forni, L.G. Systematic review of prognostic prediction models for acute kidney injury (AKI) in general hospital populations. BMJ Open 2017, 7, e016591. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, L.E.; Roderick, P.J.; Venn, R.M.; Yao, G.L.; Dimitrov, B.D.; Forni, L.G. Correction: The ICE-AKI study: Impact analysis of a Clinical prediction rule and Electronic AKI alert in general medical patients. PLoS ONE 2018, 13, e0203183. [Google Scholar] [CrossRef] [PubMed]
- Moons, K.G.; Altman, D.G.; Reitsma, J.B.; Ioannidis, J.P.; Macaskill, P.; Steyerberg, E.W.; Vickers, A.J.; Ransohoff, D.F.; Collins, G.S. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): Explanation and elaboration. Ann. Intern. Med. 2015, 162, W1–W73. [Google Scholar] [CrossRef]
- Debray, T.P.; Vergouwe, Y.; Koffijberg, H.; Nieboer, D.; Steyerberg, E.W.; Moons, K.G. A new framework to enhance the interpretation of external validation studies of clinical prediction models. J. Clin. Epidemiol. 2015, 68, 279–289. [Google Scholar] [CrossRef]
| Internal Dataset | Open Database | |||
|---|---|---|---|---|
| Total (n = 76,032) | AKI (n = 2314) | Non-AKI (n = 73,718) | Total (n = 5512) | |
| Demographic data | ||||
| Age, years | 55.3 ± 15.2 | 59.0 ± 13.4 | 55.2 ± 15.3 | 58.2 ± 14.0 |
| Sex (female) | 34,491 (45.4) | 1647 (71.2) | 32,844 (44.6) | 2766 (50.2) |
| BMI (kg/m2) | 24.2 ± 3.7 | 24.7 ± 3.8 | 24.2 ± 3.7 | 23.4 ± 3.6 |
| ASA | ||||
| 1 | 7826 (10.3) | 149 (6.4) | 7677 (10.4) | 1612 (29.2) |
| 2 | 60,450 (79.5) | 1439 (62.2) | 59,011 (80.1) | 3337 (60.5) |
| 3 | 7092 (9.3) | 595 (25.7) | 6497 (8.8) | 516 (9.4) |
| ≥4 | 661 (0.8) | 130 (5.6) | 531 (0.7) | 47 (8.5) |
| Surgery department | ||||
| GS | 32,092 (42.2) | 1347 (58.2) | 30,745 (41.7) | 4272 (77.5) |
| URO | 7828 (10.3) | 677 (29.3) | 7151 (9.7) | 116 (2.1) |
| OBY | 7785 (10.2) | 46 (1.9) | 7739 (10.5) | 197 (3.6) |
| OS | 7237 (9.5) | 78 (3.4) | 7159 (9.7) | - |
| ENT | 5699 (7.5) | 32 (1.4) | 5667 (7.7) | - |
| NS | 5149 (6.8) | 20 (0.9) | 5129 (7.0) | - |
| CS | 4409 (5.8) | 93 (4.0) | 4316 (5.9) | 927 (16.8) |
| PS | 2691 (3.5) | 15 (0.6) | 2676 (3.6) | - |
| OPH | 2254 (3.0) | 1 (0.0) | 2253 (3.1) | - |
| DNT | 878 (1.2) | 5 (0.2) | 873 (1.2) | - |
| DER | 10 (0.0) | 0 (0.0) | 10 (0.0) | - |
| Preoperative laboratory results | ||||
| White blood cell, 103/μL | 6.5 ± 2.6 | 6.6 ± 3.3 | 6.5 ± 2.5 | 6.2 ± 2.4 |
| Hemoglobin, g/dL | 12.9 ± 1.8 | 12.3 ± 2.3 | 12.9 ± 1.8 | 12.9 ± 1.9 |
| Sodium, mmol/L | 140.2 ± 2.6 | 139.8 ± 3.5 | 140.3 ± 2.5 | 140.1 ± 2.8 |
| Platelet, 103/μL | 241.8 ± 75.9 | 208.0 ± 99.6 | 242.9 ± 74.8 | 242.87 ± 83.4 |
| Potassium, mmol/L | 4.2 ± 0.4 | 4.2 ± 0.5 | 4.3 ± 0.4 | 4.2 ± 0.4 |
| Chloride, mmol/L | 103.7 ± 2.9 | 103.5 ± 3.9 | 103.7 ± 2.9 | 103.3 ± 4.0 |
| Total bilirubin, mg/dL | 0.6 ± 1.6 | 1.4 ± 3.9 | 0.6 ± 1.4 | 0.7 ± 1.7 |
| BUN, mg/dL | 15.3 ± 6.5 | 17.7 ± 10.1 | 15.2 ± 6.4 | 14.8 ± 6.9 |
| Creatinine, mg/dL | 0.8 ± 0.3 | 1.0 ± 0.6 | 0.8 ± 0.3 | 0.8 ± 0.3 |
| Albumin, g/dL | 3.8 ± 0.5 | 3.5 ± 0.6 | 3.8 ± 0.5 | 4.1 ± 0.5 |
| AST, IU/L | 24.8 ± 49.2 | 40.0 ± 186.1 | 24.3 ± 37.6 | 31.1 ± 140.0 |
| ALT, IU/L | 22.4 ± 40.8 | 32.3 ± 148.2 | 22.1 ± 32.1 | 29.1 ± 95.2 |
| Hematocrit, % | 38.9 ± 5.0 | 36.8 ± 6.6 | 38.9 ± 4.9 | 37.4 ± 6.1 |
| eGFR, mL/min/1.73 m2 | 92.5 ± 19.9 | 85.0 ± 26.6 | 92.7 ± 19.5 | 86.7 ± 26.4 |
| Glucose, mg/dL | 115.2 ± 40.4 | 122.9 ± 49.0 | 114.9 ± 40.1 | 115.8 ± 41.7 |
| PT, INR | 1.0 ± 0.2 | 1.1 ± 0.4 | 1.0 ± 0.2 | 1.0 ± 0.2 |
| aPTT, s | 27.6 ± 4.4 | 29.5 ± 8.5 | 27.6 ± 4.2 | 32.9 ± 8.6 |
| CRP, mg/dL | 1.2 ± 3.4 | 1.9 ± 4.5 | 1.1 ± 3.3 | 1.2 ± 3.6 |
| Intraoperative data | ||||
| EBL, mL | 112.9 ± 232.4 | 145.0 ± 649.4 | 23.3 ± 1360.1 | 365.86 ± 1176.3 |
| Anesthesia time, min | 171.5 ± 128.5 | 301.9 ± 233.4 | 167.4 ± 121.6 | 203.9 ± 114.0 |
| Surgery time, min | 126.0 ± 114.3 | 241.8 ± 210.7 | 122.4 ± 108.0 | 140.10 ± 100.3 |
| Clinical Outcome | Internal Dataset | Open Database | ||
|---|---|---|---|---|
| Total (n = 76,032) | AKI (n = 2314) | Non-AKI (n = 73,718) | Total (n = 5512) | |
| Acute kidney injury, n (%) | 2314 (3.1) | - | - | 78 (1.4) |
| Length of hospital stay (days) | 9.0 ± 38.3 | 21.9 ± 34.5 | 8.6 ± 38.3 | 10.3 ± 13.7 |
| Length of hospital stay ≥ 7 days, n (%) | 29,280 (38.5) | 1651 (71.3) | 27,629 (37.5) | 3153 (57.2) |
| In-hospital death, n (%) | 1595 (2.1) | 144 (6.2) | 1201 (1.6) | 47 (0.9) |
| 30-day mortality, n (%) | 270 (0.4) | 54 (2.3) | 216 (0.3) | 28 (0.5) |
| Postoperative ICU care, n (%) | 7217 (9.5) | 704 (30.4) | 6513 (9.8) | 1008 (18.3) |
| Length of ICU stay (days) | 0.7 ± 6.7 | 3.8 ± 13.9 | 0.6 ± 6.4 | 0.49 ± 3.3 |
| Features | Model | AUROC | AUPRC | F1-Score |
|---|---|---|---|---|
| Demographic data | LR | 0.6942 ± 0.0038 | 0.5714 ± 0.0070 | 0.3981 ± 0.0048 |
| RF | 0.6549 ± 0.0048 | 0.5165 ± 0.0057 | 0.4931 ± 0.0053 | |
| GBM | 0.7137 ± 0.0038 | 0.5906 ± 0.0077 | 0.4573 ± 0.0074 | |
| DNN | 0.6794 ± 0.0092 | 0.5060 ± 0.0140 | 0.2919 ± 0.042 | |
| Preoperative data | LR | 0.6795 ± 0.0043 | 0.5942 ± 0.0080 | 0.4184 ± 0.0059 |
| RF | 0.7224 ± 0.0043 | 0.6375 ± 0.0061 | 0.5023 ± 0.0052 | |
| GBM | 0.7280 ± 0.0040 | 0.6468 ± 0.0066 | 0.5072 ± 0.0047 | |
| DNN | 0.6281 ± 0.0161 | 0.5218 ± 0.0145 | 0.3707 ± 0.0290 | |
| Intraoperative data | LR | 0.7449 ± 0.0039 | 0.6267 ± 0.0066 | 0.4963 ± 0.0042 |
| RF | 0.7221 ± 0.0034 | 0.5983 ± 0.0067 | 0.4595 ± 0.0051 | |
| GBM | 0.8161 ± 0.0037 | 0.7146 ± 0.0082 | 0.6562 ± 0.0069 | |
| DNN | 0.8105 ± 0.0070 | 0.6749 ± 0.0102 | 0.6539 ± 0.0109 | |
| All features | LR | 0.7827 ± 0.0043 | 0.6609 ± 0.0077 | 0.5449 ± 0.0056 |
| RF | 0.8547 ± 0.0029 | 0.7578 ± 0.0057 | 0.7101 ± 0.0058 | |
| GBM | 0.8679 ± 0.0039 | 0.7862 ± 0.0084 | 0.7226 ± 0.0062 | |
| DNN | 0.8279 ± 0.0069 | 0.6963 ± 0.00099 | 0.6355 ± 0.0277 |
| Features | Model | AUROC | AUPRC | F1-Score |
|---|---|---|---|---|
| Demographic data | LR | 0.6815 ± 0.0123 | 0.5491 ± 0.0214 | 0.4028 ± 0.0063 |
| RF | 0.6031 ± 0.0122 | 0.4442 ± 0.0161 | 0.4176 ± 0.0179 | |
| GBM | 0.6995 ± 0.0102 | 0.5900 ± 0.0177 | 0.5042 ± 0.0153 | |
| DNN | 0.6600 ± 0.0108 | 0.5079 ± 0.0172 | 0.3171 ± 0.0360 | |
| Preoperative data | LR | 0.6808 ± 0.0114 | 0.6443 ± 0.0125 | 0.4211 ± 0.0153 |
| RF | 0.6031 ± 0.0122 | 0.4442 ± 0.0161 | 0.4176 ± 0.0179 | |
| GBM | 0.7693 ± 0.0128 | 0.6958 ± 0.0.185 | 0.5118 ± 0.0139 | |
| DNN | 0.6839 ± 0.00223 | 0.5978 ± 0.0239 | 0.4641 ± 0.0386 | |
| Intraoperative data | LR | 0.7674 ± 0.0101 | 0.4027 ± 0.0212 | 0.0292 ± 0.0009 |
| RF | 0.6499 ± 0.0295 | 0.4748 ± 0.0262 | 0.4877 ± 0.0273 | |
| GBM | 0.7054 ± 0.0168 | 0.5836 ± 0.0266 | 0.5985 ± 0.0116 | |
| DNN | 0.5770 ± 0.3780 | 0.489 ± 0.0420 | 0.4804 ± 0.0196 | |
| All features | LR | 0.7495 ± 0.0166 | 0.6541 ± 0.0269 | 0.6268 ± 0.0189 |
| RF | 0.7342 ± 0.0295 | 0.6403 ± 0.0325 | 0.6098 ± 0.0228 | |
| GBM | 0.7572 ± 0.0150 | 0.6834 ± 0.0213 | 0.6129 ± 0.0205 | |
| DNN | 0.6715 ± 0.0530 | 0.5584 ± 0.0540 | 0.5292 ± 0.0303 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-W.; Jang, J.; Seo, W.-Y.; Lee, D.; Kim, S.-H. Internal and External Validation of Machine Learning Models for Predicting Acute Kidney Injury Following Non-Cardiac Surgery Using Open Datasets. J. Pers. Med. 2024, 14, 587. https://doi.org/10.3390/jpm14060587
Lee S-W, Jang J, Seo W-Y, Lee D, Kim S-H. Internal and External Validation of Machine Learning Models for Predicting Acute Kidney Injury Following Non-Cardiac Surgery Using Open Datasets. Journal of Personalized Medicine. 2024; 14(6):587. https://doi.org/10.3390/jpm14060587
Chicago/Turabian StyleLee, Sang-Wook, Jaewon Jang, Woo-Young Seo, Donghee Lee, and Sung-Hoon Kim. 2024. "Internal and External Validation of Machine Learning Models for Predicting Acute Kidney Injury Following Non-Cardiac Surgery Using Open Datasets" Journal of Personalized Medicine 14, no. 6: 587. https://doi.org/10.3390/jpm14060587
APA StyleLee, S.-W., Jang, J., Seo, W.-Y., Lee, D., & Kim, S.-H. (2024). Internal and External Validation of Machine Learning Models for Predicting Acute Kidney Injury Following Non-Cardiac Surgery Using Open Datasets. Journal of Personalized Medicine, 14(6), 587. https://doi.org/10.3390/jpm14060587





