Enhancing Kidney Transplant Outcomes: The Impact of Living Donor Programs
Abstract
1. Introduction
2. Methods
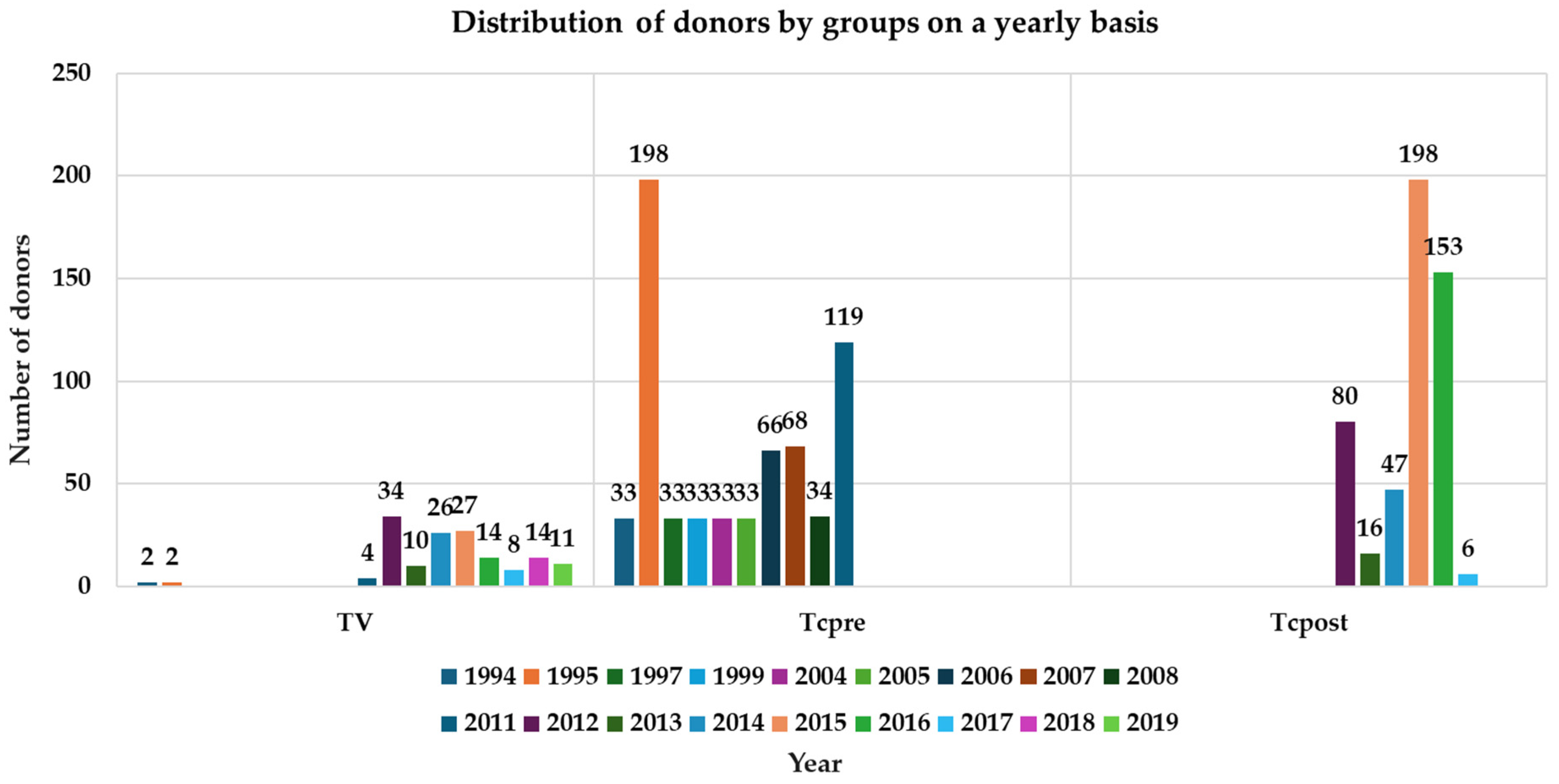
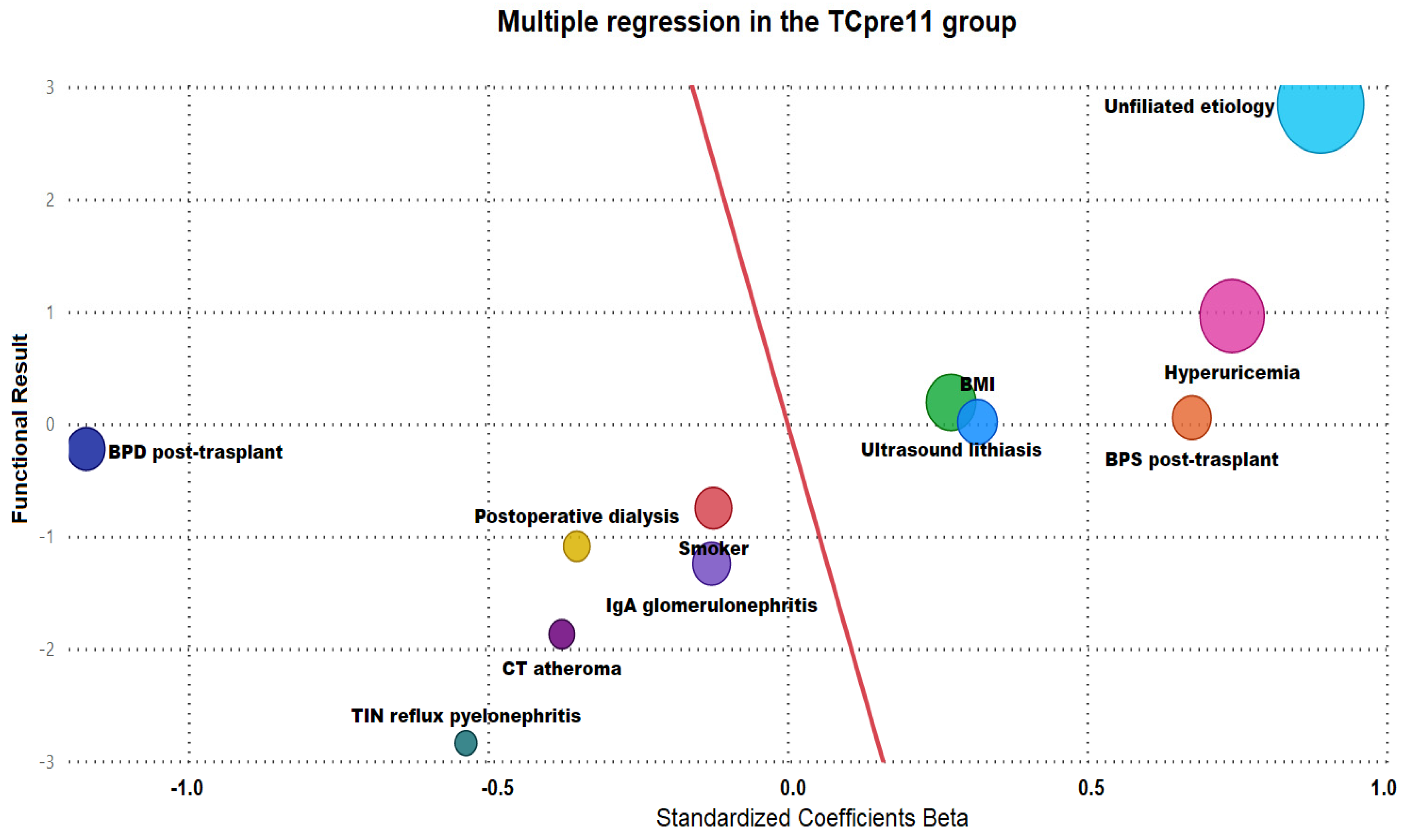
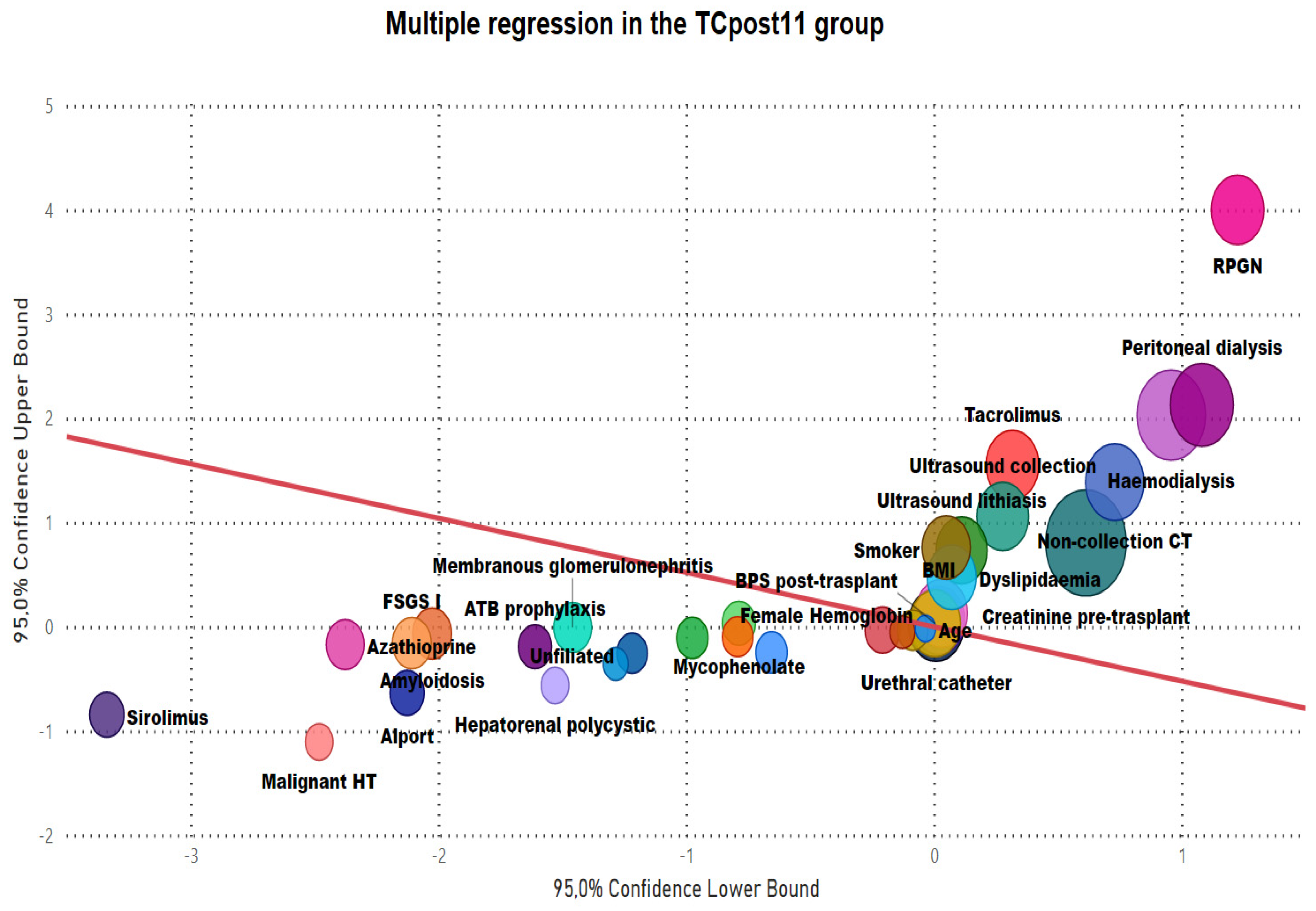
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Otero, A.; De Francisco, A.; Gayoso, P.; García, F.; EPIRCE Study Group. Prevalence of chronic renal disease in Spain: Results of the EPIRCE study. Nephrology 2010, 30, 78–86. [Google Scholar]
- Axelrod, D.A.; Schnitzler, M.A.; Xiao, H.; Irish, W.; Tuttle-Newhall, E.; Chang, S.-H.; Kasiske, B.L.; Alhamad, T.; Lentine, K.L. An economic assessment of contemporary kidney transplant practice. Am. J. Transplant. 2018, 18, 1168–1176. [Google Scholar] [CrossRef]
- Ministry-of-Health, Spanish Government. Kidney Donation and Transplant Activity; National Transplant Organisatio: Madrid, Spain, 2023.
- Aslam, S.; Buggs, J.; Wasserman, J.; Chaves, K.; Rogers, E.; Kumar, A.; Huang, J. Outcomes With Age Combinations in Living Donor Kidney Transplantation. Am. Surg. 2020, 86, 659–664. [Google Scholar] [CrossRef]
- Lorenz, E.C.; Cosio, F.G.; Bernard, S.L.; Bogard, S.D.; Bjerke, B.R.; Geissler, E.N.; Hanna, S.W.; Kremers, W.K.; Cheng, Y.; Stegall, M.D.; et al. The Relationship Between Frailty and Decreased Physical Performance With Death on the Kidney Transplant Waiting List. Prog. Transplant. 2019, 29, 108–114. [Google Scholar] [CrossRef]
- Padilla-Fernández, B.-Y. Renal Transplantation. Surgical Aspects. In Nephrology and Urology, 1st ed.; Lorenzo-Gómez, M.-F., Fraile-Gómez, M.-P., Macías-Núñez, J.-F., Eds.; Editions University of Salamanca: Salamanca, Spain, 2021; pp. 523–533. [Google Scholar]
- Salvatierra-Pérez, C.; Martín-Parada, A. Laparoscopy and robotics in Urology. In Nephrology and Urology; Lorenzo-Gómez, M.-F., Fraile-Gómez, M.-P., Macías-Núñez, J.-F., Eds.; Editions University of Salamanca: Salamanca, Spain, 2021; pp. 543–544. [Google Scholar]
- Ministry of Health, Social Services and Equality. Royal Decree 1723/2012, of December 28, Which Regulates the Activities of Obtaining, Clinical Use and Territorial Coordination of Human Organs Intended for Transplantation and Establishes Quality and Safety Requirements; State Agency Official State Gazette, Spain State Agency: Madrid, Spain, 2012; «BOE» num. 313; pp. 89315–89348.
- University of Salamanca Healthcare Complex. Memoire: Donation and Transplants Coordination; Health Counseling of Castilla y Leon: Valladolid, Spain, 2020. [Google Scholar]
- Regmi, S.; Rattanavich, R.; Villicana, R. Kidney and pancreas transplant candidacy. Curr. Opin. Organ. Transplant. 2021, 26, 62–68. [Google Scholar] [CrossRef]
- Koken, Z.O.; Karahan, S.; Tuncbilek, Z.; Celik, S.S. Nursing Diagnoses and Interventions in Kidney Transplant Recipients: A Retrospective Study. Transplant. Proc. 2019, 51, 2321–2323. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, D.; Donnelly, S.; Miller, J.; Stewart, D.; Albert, S.E. Gender disparity in living renal transplant donation. Am. J. Kidney Dis. 2000, 36, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Veroux, M.; Mattone, E.; Cavallo, M.; Gioco, R.; Corona, D.; Volpicelli, A.; Veroux, P. Obesity and bariatric surgery in kidney transplantation: A clinical review. World J. Diabetes 2021, 12, 1563–1575. [Google Scholar] [CrossRef] [PubMed]
- Pham, P.T.; Danovitch, G.M.; Pham, P.C. Kidney transplantation in the obese transplant candidates: To transplant or not to transplant? Semin. Dial. 2013, 26, 568–577. [Google Scholar] [CrossRef]
- Yin, S.; Wu, L.; Huang, Z.; Fan, Y.; Lin, T.; Song, T. Nonlinear relationship between body mass index and clinical outcomes after kidney transplantation: A dose-response meta-analysis of 50 observational studies. Surgery 2022, 171, 1396–1405. [Google Scholar] [CrossRef]
- Salinas-Casado, J.; Méndez-Rubio, S.; Esteban-Fuertes, M.; Gómez-Rodríguez, A.; Vírseda-Chamorro, M.; Luján-Galán, M.; Rituman, G. Efficacy and safety of D-mannose (2 g), 24 h prolonged release, associated with Proanthocyanidin (PAC), versus isolate PAC, in the management of a series of women with recurrent urinary infections. Arch. Esp. Urol. 2018, 71, 169–177. [Google Scholar] [PubMed]
- Behzad, D.; Hakimeh, A.; Hossein, R.; Khaledi, A. A middle east systematic review and meta-analysis of bacterial urinary tract infection among renal transplant recipients; Causative microorganisms. Microb. Pathog. 2020, 148, 104458. [Google Scholar] [CrossRef] [PubMed]
- Neretljak, I.; Mihovilović, K.; Kovacević-Vojtusek, I.; Vidas, Z.; Jurenec, F.; Knotek, M. Effect of pretransplant dialysis modality on incidence of early posttransplant infections in kidney recipients. Acta Med. Croatica 2011, 65 (Suppl. 3), 58–62. [Google Scholar] [PubMed]
- Kinoshita, Y.; Katano, S.; Nishida, S.; Shimizu, T.; Fujimura, T.; Kume, H.; Iwami, D. Creatinine reduction ratio on postoperative day 2 predicts long-term outcomes after living donor kidney transplantation. Int. J. Urol. 2022, 29, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Hicks, M.; Hing, A.; Gao, L.; Ryan, J.; Macdonald, P.S. Organ preservation. Methods Mol. Biol. 2006, 333, 331–374. [Google Scholar] [PubMed]
- Ming, Y.; Shao, M.; Tian, T.; She, X.; Liu, H.; Ye, S.; Ye, Q. Outcome of kidney transplantation between controlled cardiac death and brain death donors: A meta-analysis. Chin. Med. J. 2014, 127, 2829–2836. [Google Scholar] [PubMed]
- Kayler, L.; Yu, X.; Cortes, C.; Lubetzky, M.; Friedmann, P. Impact of Cold Ischemia Time in Kidney Transplants From Donation After Circulatory Death Donors. Transplant. Direct 2017, 3, e177. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.; Rose, C.; Joffres, Y.; Kadatz, M.; Gill, J. Cold ischemia time up to 16 hours has little impact on living donor kidney transplant outcomes in the era of kidney paired donation. Kidney Int. 2017, 92, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Gorayeb-Polacchini, F.S.; Caldas, H.C.; Fernandes-Charpiot, I.M.M.; Ferreira-Baptista, M.A.S.; Gauch, C.R.; Abbud-Filho, M. Impact of Cold Ischemia Time on Kidney Transplant: A Mate Kidney Analysis. Transplant. Proc. 2020, 52, 1269–1271. [Google Scholar] [CrossRef]
- Fletchinger, T.; Jensen, H.K.; Wells, A.; Giorgakis, E.; Patel, R.B.; Barone, G.W.; Khan, N.; Burdine, M.; Sharma, A.; Bhusal, S.; et al. Impact of Prolonged Cold Ischemia Time on One Year Kidney Transplant Outcomes. Transplant. Proc. 2022, 54, 2170–2173. [Google Scholar] [CrossRef]
- Dube, G.K.; Brennan, C. Outcomes of kidney transplant from deceased donors with acute kidney injury and prolonged cold ischemia time—A retrospective cohort study. Transpl. Int. 2019, 32, 646–657. [Google Scholar] [CrossRef] [PubMed]
- Serrano, O.K.; Vock, D.M.; Chinnakotla, S.; Dunn, T.B.; Kandaswamy, R.; Pruett, T.L.; Feldman, R.; Matas, A.J.; Finger, E.B. The Relationships Between Cold Ischemia Time, Kidney Transplant Length of Stay, and Transplant-related Costs. Transplantation 2019, 103, 401–411. [Google Scholar] [CrossRef]
- Vinson, A.J.; Kiberd, B.A.; Tennankore, K.K. Prolonged Cold Ischemia Time Offsets the Benefit of Human Leukocyte Antigen Matching in Deceased Donor Kidney Transplant. Transplant. Proc. 2020, 52, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Cheng, K.; Huang, J. Effect of Long Cold Ischemia Time of Kidneys from Aged Donors on Prognosis of Kidney Transplantation. Ann. Transplant. 2021, 26, e928735. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Pachón, D.; Calatayud, E.; Buxeda, A.; Pérez-Sáez, M.J.; Arias-Cabrales, C.; Gimeno, J.; Burballa, C.; Mir, M.; Llinàs-Mallol, L.; Outon, S.; et al. Evolución de las causas de pérdida del injerto en trasplante renal durante 40 años (1979–2019). Rev. Nefrol. 2021, 43, 316–327. [Google Scholar] [CrossRef]
- Zomorrodi, A.; Bohluli, A. Double urinary bladder voiding technique post removal of urethral catheter in renal allograft recipients. Saudi J. Kidney Dis. Transpl. 2007, 18, 532–535. [Google Scholar]
- Thompson, E.R.; Hosgood, S.A.; Nicholson, M.L.; Wilson, C.H. Early versus late ureteric stent removal after kidney transplantation. Cochrane Database Syst. Rev. 2018, 1, cd011455. [Google Scholar] [CrossRef] [PubMed]
- Ng, Z.Q.; Tan, J.H.; Larkins, N.; Willis, F.; He, B. Outcomes of Early Simultaneous Removal of Ureteric Stent With Indwelling Urethral Catheter After Kidney Transplant in Pediatric Recipients: A 10-Year Review. Exp. Clin. Transplant. 2021, 19, 118–124. [Google Scholar] [CrossRef]
- Cai, J.-F.; Wang, W.; Hao, W.; Sun, Z.-J.; Su, L.-L.; Li, X.; Zheng, X.; Zhang, X.-D. Meta-analysis of Early Versus Late Ureteric Stent Removal After Kidney Transplantation. Transplant. Proc. 2018, 50, 3411–3415. [Google Scholar] [CrossRef]
- Luján, S.; García-Fadrique, G.; Budía, A.; Broseta, E.; Jiménez-Cruz, F. Should ureteral catheterization be systematically used in kidney transplants? Actas Urol. Esp. 2011, 35, 213–217. [Google Scholar] [CrossRef][Green Version]
- Redondo-Pachon, D. Evaluación del Donante para Trasplante Renal con Criterios Expandidos. Lorenzo, V., López Gómez, J.M., Eds.; Nefrología al Día. ISSN 2659-2606. Available online: https://www.nefrologiaaldia.org/336 (accessed on 12 December 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noya-Mourullo, A.; Martín-Parada, A.; Palacios-Hernández, A.; Eguiluz-Lumbreras, P.; Heredero-Zorzo, Ó.; García-Gómez, F.; Álvarez-Ossorio-Fernández, J.L.; Álvarez-Ossorio-Rodal, A.; Márquez-Sánchez, M.-T.; Flores-Fraile, J.; et al. Enhancing Kidney Transplant Outcomes: The Impact of Living Donor Programs. J. Pers. Med. 2024, 14, 408. https://doi.org/10.3390/jpm14040408
Noya-Mourullo A, Martín-Parada A, Palacios-Hernández A, Eguiluz-Lumbreras P, Heredero-Zorzo Ó, García-Gómez F, Álvarez-Ossorio-Fernández JL, Álvarez-Ossorio-Rodal A, Márquez-Sánchez M-T, Flores-Fraile J, et al. Enhancing Kidney Transplant Outcomes: The Impact of Living Donor Programs. Journal of Personalized Medicine. 2024; 14(4):408. https://doi.org/10.3390/jpm14040408
Chicago/Turabian StyleNoya-Mourullo, Andrea, Alejandro Martín-Parada, Alberto Palacios-Hernández, Pablo Eguiluz-Lumbreras, Óscar Heredero-Zorzo, Francisco García-Gómez, José Luis Álvarez-Ossorio-Fernández, Andrea Álvarez-Ossorio-Rodal, Magaly-Teresa Márquez-Sánchez, Javier Flores-Fraile, and et al. 2024. "Enhancing Kidney Transplant Outcomes: The Impact of Living Donor Programs" Journal of Personalized Medicine 14, no. 4: 408. https://doi.org/10.3390/jpm14040408
APA StyleNoya-Mourullo, A., Martín-Parada, A., Palacios-Hernández, A., Eguiluz-Lumbreras, P., Heredero-Zorzo, Ó., García-Gómez, F., Álvarez-Ossorio-Fernández, J. L., Álvarez-Ossorio-Rodal, A., Márquez-Sánchez, M.-T., Flores-Fraile, J., Fraile-Gómez, P., Padilla-Fernández, B. Y., & Lorenzo-Gómez, M.-F. (2024). Enhancing Kidney Transplant Outcomes: The Impact of Living Donor Programs. Journal of Personalized Medicine, 14(4), 408. https://doi.org/10.3390/jpm14040408







