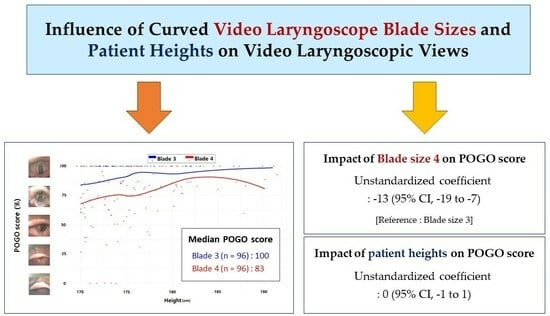
Influence of Curved Video Laryngoscope Blade Sizes and Patient Heights on Video Laryngoscopic Views: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
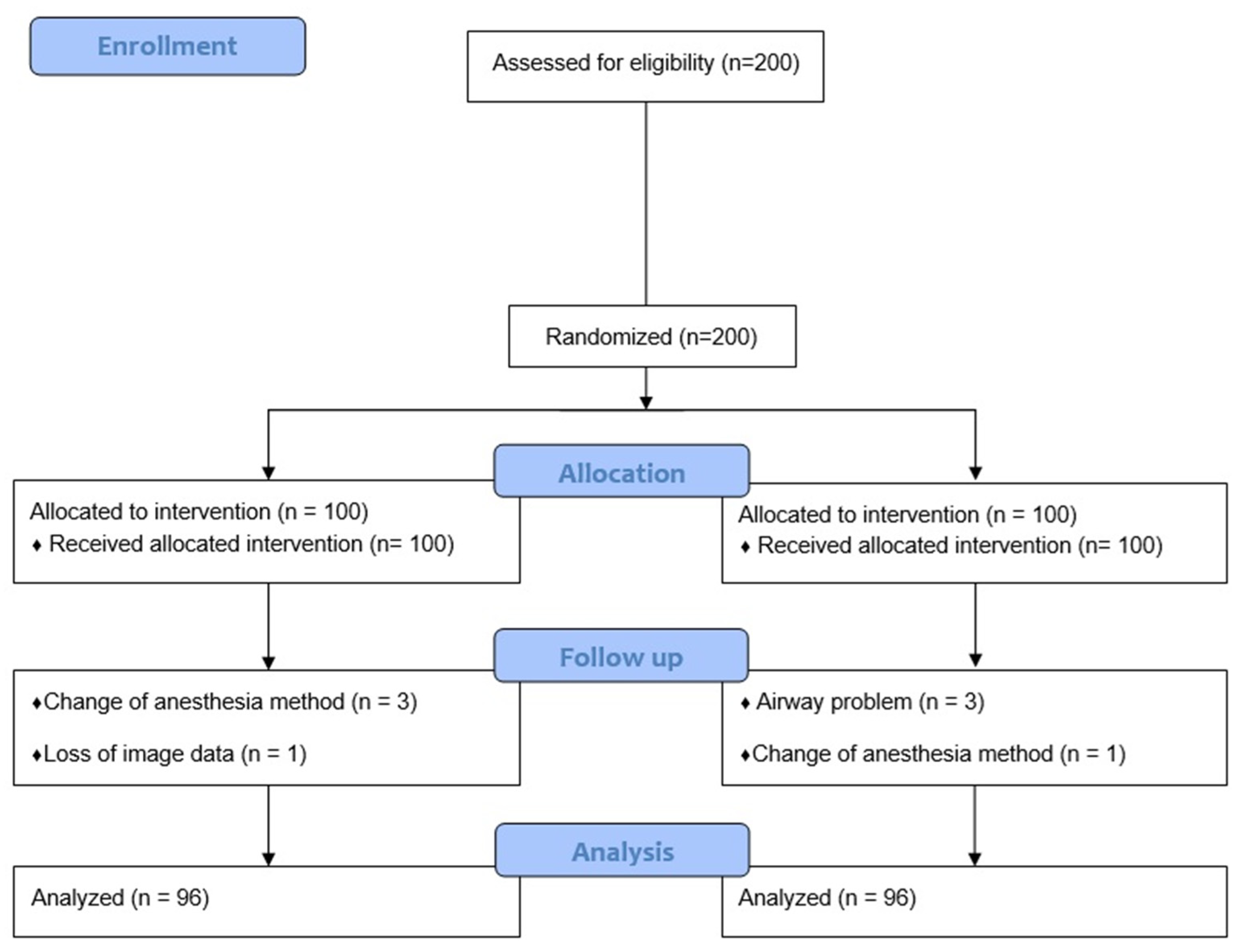
2.2. Participants, Study Design, and Randomization
2.3. Primary and Secondary Outcomes
2.4. Preoperative Measurement
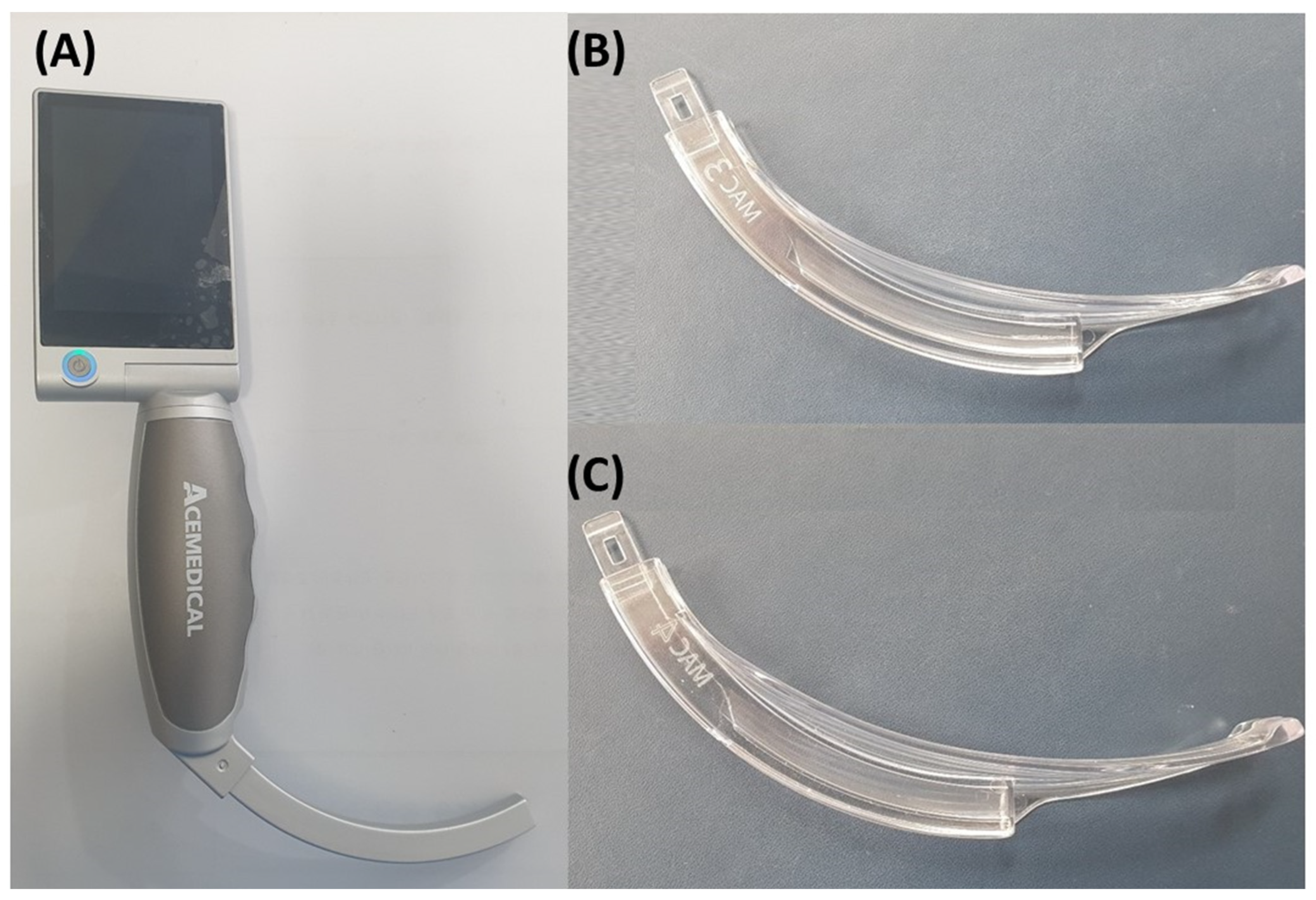
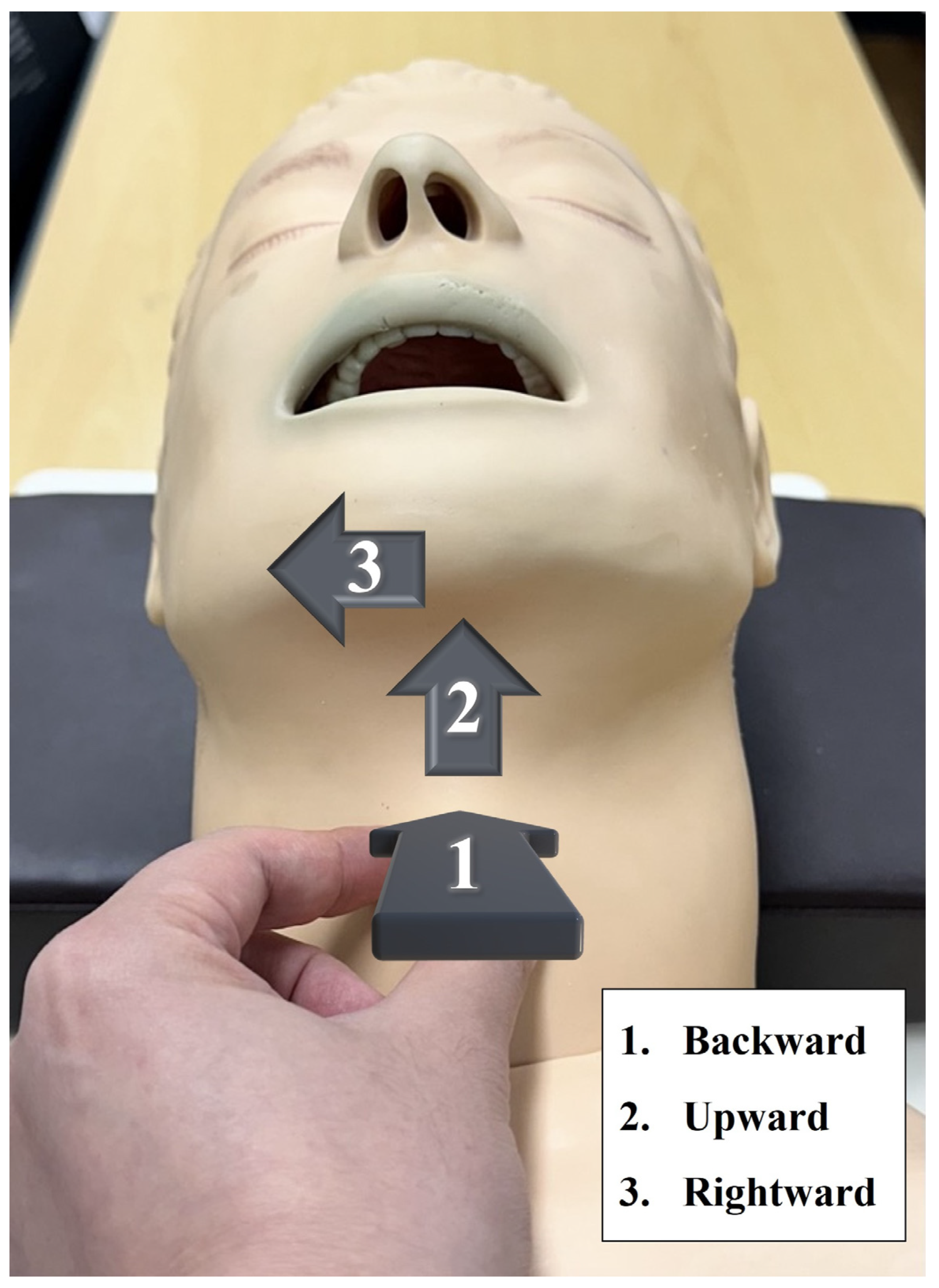
2.5. Intubation
2.6. Statistical Analysis
3. Results
3.1. Percentage of Glottic Opening Scores According to Blade Size
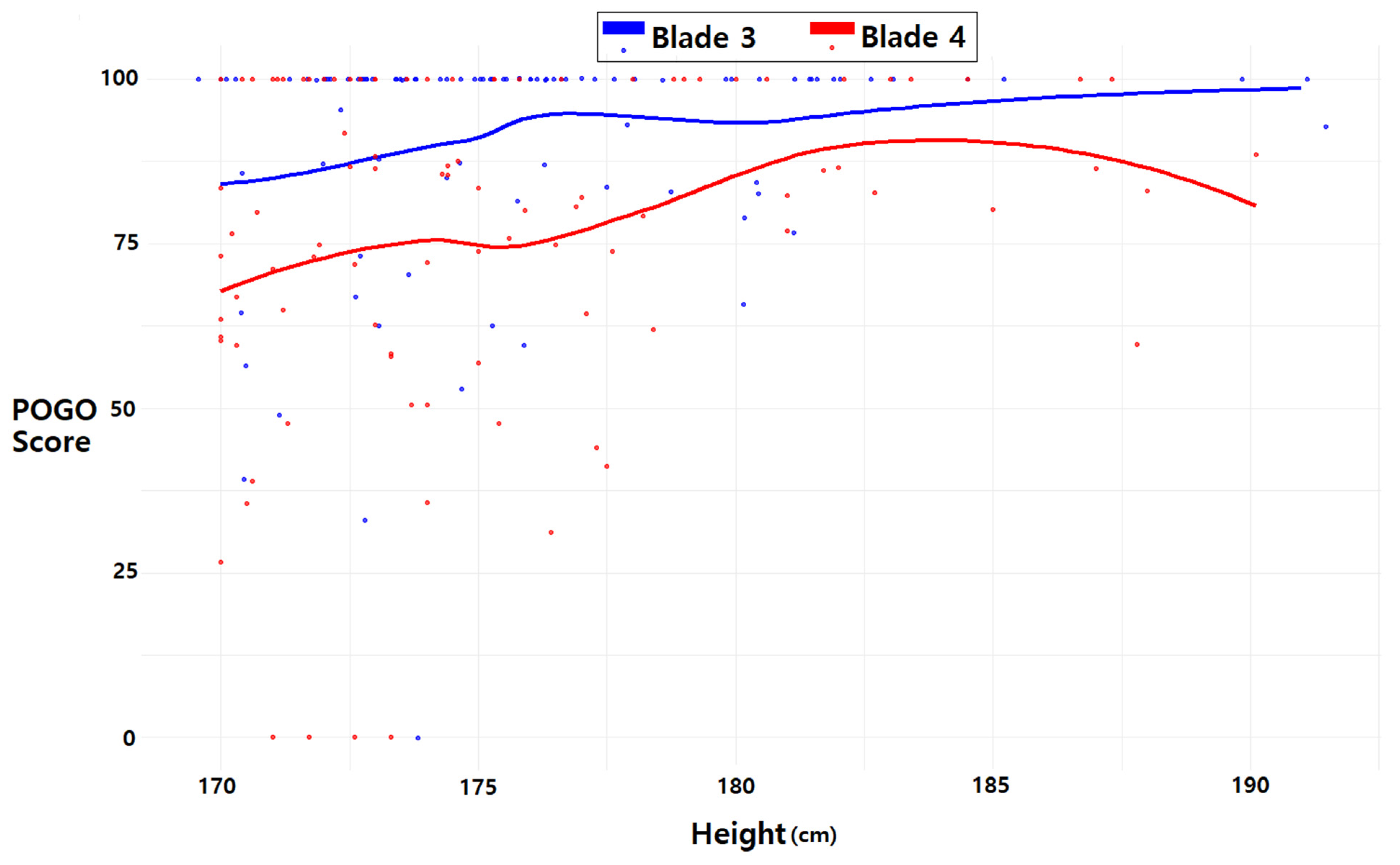
3.2. Percentage of Glottic Opening Score and Patient Height
3.3. Association of Percentage of Glottic Opening Score with Blade Size and Patient Height by Multiple Linear Regression Analysis
3.4. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perkins, E.J.; Begley, J.L.; Brewster, F.M.; Hanegbi, N.D.; Ilancheran, A.A.; Brewster, D.J. The use of video laryngoscopy outside the operating room: A systematic review. PLoS ONE 2022, 17, e0276420. [Google Scholar] [CrossRef]
- Sakles, J.C.; Mosier, J.; Hadeed, G.; Hudson, M.; Valenzuela, T.; Latifi, R. Telemedicine and telepresence for prehospital and remote hospital tracheal intubation using a GlideScope™ videolaryngoscope: A model for tele-intubation. Telemed. e-Health 2011, 17, 185–188. [Google Scholar] [CrossRef]
- de Carvalho, C.C.; da Silva, D.M.; Lemos, V.M.; Dos Santos, T.G.B.; Agra, I.C.; Pinto, G.M.; Ramos, I.B.; Costa, Y.S.C.; Santos Neto, J.M. Videolaryngoscopy vs. direct Macintosh laryngoscopy in tracheal intubation in adults: A ranking systematic review and network meta-analysis. Anaesthesia 2022, 77, 326–338. [Google Scholar] [CrossRef]
- Saul, S.A.; Ward, P.A.; McNarry, A.F. Airway management: The current role of videolaryngoscopy. J. Pers. Med. 2023, 13, 1327. [Google Scholar] [CrossRef]
- Tippmann, S.; Schäfer, J.; Winter, J.; Mühler, A.-K.; Schmitz, K.; Schönfeld, M.; Eichinger, M.; Mildenberger, E.; Kidszun, A. Video versus direct laryngoscopy to improve the success rate of nasotracheal intubations in the neonatal intensive care setting: A randomised controlled trial. BMJ Paediatr. Open 2023, 7, e001958. [Google Scholar]
- Hagberg, C.A. Benumof and Hagberg’s Airway Management E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Lavery, G.G.; Jamison, C.A. Chapter 2—Airway Management in the Critically Ill Adult. In Critical Care Medicine, 3rd ed.; Parrillo, J.E., Dellinger, R.P., Eds.; Mosby: Philadelphia, PA, USA, 2008; pp. 17–37. [Google Scholar]
- Martindale, T.A.; Berkow, L. Manual of Emergency Airway Management, 3rd Edition. Anesthesiology 2009, 111, 683. [Google Scholar] [CrossRef]
- Berkow, L.C.; Morey, T.E.; Urdaneta, F. The Technology of Video Laryngoscopy. Anesth. Analg. 2018, 126, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- De Jong, A.; Molinari, N.; Conseil, M.; Coisel, Y.; Pouzeratte, Y.; Belafia, F.; Jung, B.; Chanques, G.; Jaber, S. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: A systematic review and meta-analysis. Intensive Care Med. 2014, 40, 629–639. [Google Scholar] [CrossRef]
- Pieters, B.M.; Theunissen, M.; van Zundert, A.A. Macintosh Blade Videolaryngoscopy Combined with Rigid Bonfils Intubation Endoscope Offers a Suitable Alternative for Patients with Difficult Airways. Anesth. Analg. 2018, 126, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Grensemann, J.; Simon, M.; Kluge, S. Airway management in intensive care and emergency medicine: What is new? Med. Klin.-Intensivmed. Notfallmedizin 2019, 114, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Soltani, A.E.; Maleki, A.; Espahbodi, E.; Goudarzi, M.; Ariana, P.; Takzare, A. Comparison of the laryngoscopic view using Macintosh and Miller blades in children less than four years old. J. Med. Life 2020, 13, 431. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.W.; Kim, Y.M.; Cho, Y.; Lee, S.J. Effect of the curved blade size on the outcomes of tracheal intubation performed by incoming interns: A randomized controlled manikin study. Medicine 2018, 97, e11984. [Google Scholar] [CrossRef]
- Godet, T.; De Jong, A.; Garin, C.; Guérin, R.; Rieu, B.; Borao, L.; Pereira, B.; Molinari, N.; Bazin, J.-E.; Jabaudon, M.; et al. Impact of Macintosh blade size on endotracheal intubation success in intensive care units: A retrospective multicenter observational MacSize-ICU study. Intensive Care Med. 2022, 48, 1176–1184. [Google Scholar] [CrossRef]
- Landefeld, K.R.; Koike, S.; Ran, R.; Semler, M.W.; Barnes, C.; Stempek, S.B.; Janz, D.R.; Rice, T.W.; Russell, D.W.; Self, W.H.; et al. Effect of Laryngoscope Blade Size on First Pass Success of Tracheal Intubation in Critically Ill Adults. Crit. Care Explor. 2023, 5, e0855. [Google Scholar] [CrossRef]
- Kim, H.; Chang, J.-E.; Han, S.-H.; Lee, J.-M.; Yoon, S.; Hwang, J.-Y. Effect of the Macintosh curved blade size on direct laryngoscopic view in edentulous patients. Am. J. Emerg. Med. 2018, 36, 120–123. [Google Scholar] [CrossRef]
- Karl Storz-Endoskope. Available online: https://www.karlstorz.com/us/en/search.htm?cat=1000105428 (accessed on 13 April 2023).
- Glidescope Titanium. Available online: https://anestesiar.org/WP/uploads/2015/03/glidescope-titanium-un-solo-uso.pdf (accessed on 13 December 2023).
- BD-DP Disposable EMS Video Laryngoscope. Available online: https://besdatatech.com/bd-dp-disposable-video-laryngoscope/ (accessed on 13 December 2023).
- Levitan, R.M.; Ochroch, E.A.; Rush, S.; Shofer, F.S.; Hollander, J.E. Assessment of Airway Visualization: Validation of the Percentage of Glottic Opening (POGO) Scale. Acad. Emerg. Med. 1998, 5, 919–923. [Google Scholar] [CrossRef]
- Oh, J.Y.; Lee, J.H.; Kim, Y.Y.; Baek, S.M.; Jung, D.W.; Park, J.H. A comparative study of glottis visualization according to the method of lifting the epiglottis in video laryngoscopy: Indirect and direct lifting methods. Anesth. Pain. Med. 2021, 16, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.L.; Rosen, I. Utility of the modified Mallampati grade and Friedman tongue position in the assessment of obstructive sleep apnea. J. Clin. Sleep. Med. 2020, 16, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, C.C.d.; Santos Neto, J.M.; Orange, F.A.d. Predictive performance of thyromental height for difficult laryngoscopies in adults: A systematic review and meta-analysis. Braz. J. Anesthesiol. 2023, 73, 491–499. [Google Scholar] [CrossRef]
- Kaniyil, S.; Anandan, K.; Thomas, S. Ratio of height to thyromental distance as a predictor of difficult laryngoscopy: A prospective observational study. J. Anaesthesiol. Clin. Pharmacol. 2018, 34, 485. [Google Scholar] [PubMed]
- Kopanaki, E.; Piagkou, M.; Demesticha, T.; Anastassiou, E.; Skandalakis, P. Sternomental distance ratio as a predictor of difficult laryngoscopy: A prospective, double-blind pilot study. Anesth. Essays Res. 2020, 14, 49. [Google Scholar] [CrossRef] [PubMed]
- Crawley, S.; Dalton, A. Predicting the difficult airway. BJA Educ. 2014, 15, 253–257. [Google Scholar] [CrossRef]
- Riad, W.; Ansari, T.; Shetty, N. Does neck circumference help to predict difficult intubation in obstetric patients? A prospective observational study. Saudi J. Anaesth. 2018, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.J.; Kang, J.M.; Kim, D.O. Laryngeal exposure during laryngoscopy is better in the 25° back-up position than in the supine position. BJA Br. J. Anaesth. 2007, 99, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Arulkumaran, N.; Lowe, J.; Ions, R.; Mendoza, M.; Bennett, V.; Dunser, M. Videolaryngoscopy versus direct laryngoscopy for emergency orotracheal intubation outside the operating room: A systematic review and meta-analysis. Br. J. Anaesth. 2018, 120, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Baek, M.S.; Han, M.; Huh, J.W.; Lim, C.-M.; Koh, Y.; Hong, S.-B. Video laryngoscopy versus direct laryngoscopy for first-attempt tracheal intubation in the general ward. Ann. Intensive Care 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Meitzen, S.E.; Benumof, J.L. Video Laryngoscopy: Positives, Negatives, and Defining the Difficult Intubation. Anesth. Analg. 2019, 128, 399–401. [Google Scholar] [CrossRef] [PubMed]
- Rombey, T.; Schieren, M.; Pieper, D. Video versus direct laryngoscopy for inpatient emergency intubation in adults: A systematic review and meta-analysis of randomized controlled trials. Dtsch. Ärzteblatt Int. 2018, 115, 437. [Google Scholar]
- Chen, D.Y.; Devsam, B.; Sett, A.; Perkins, E.J.; Johnson, M.D.; Tingay, D.G. Factors that determine first intubation attempt success in high-risk neonates. Pediatr. Res. 2023, 1–7. [Google Scholar] [CrossRef]
- Higgs, A.; McGrath, B.; Goddard, C.; Rangasami, J.; Suntharalingam, G.; Gale, R.; Cook, T.; Society, D.A. Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 2018, 120, 323–352. [Google Scholar] [CrossRef]
- Lomasney, C.; Thornton, M. Unexpected benefit of videolaryngoscopy. Br. J. Anaesth. 2014, 113, 1059–1060. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Noppens, R.R.; Möbus, S.; Heid, F.; Schmidtmann, I.; Werner, C.; Piepho, T. Evaluation of the McGrath Series 5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia 2010, 65, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Al Ramadhani, S.; Mohamed, L.A.; Rocke, D.A.; Gouws, E. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. Br. J. Anaesth. 1996, 77, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, M.; Pandey, M. Short Thyromental Distance: A Predictor of Difficult Intubation or an Indicator for Small Blade Selection? Anesthesiology 2006, 104, 1131–1136. [Google Scholar] [CrossRef]
- Pedoto, A. How to choose the double-lumen tube size and side: The eternal debate. Anesth. Clin. 2012, 30, 671–681. [Google Scholar] [CrossRef]
- Hadhoud, Y.; Baraka, M.A.; Saleh, M.; Refaat, A.M. A comparative evaluation of the sniffing, the simple head extension and the head hyperextension positions for laryngoscopic view and intubation difficulty in adults undergoing direct laryngoscopy. Eur. Arch. Oto-Rhino-Laryngol. 2023, 281, 1401–1407. [Google Scholar] [CrossRef]
- Jungbauer, A.; Schumann, M.; Brunkhorst, V.; Börgers, A.; Groeben, H. Expected difficult tracheal intubation: A prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br. J. Anaesth. 2009, 102, 546–550. [Google Scholar] [CrossRef]
- Alvarado, A.C.; Panakos, P. Endotracheal tube intubation techniques. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Johnson, K.N.; Botros, D.B.; Groban, L.; Bryan, Y.F. Anatomic and physiopathologic changes affecting the airway of the elderly patient: Implications for geriatric-focused airway management. Clin. Interv. Aging 2015, 10, 1925–1934. [Google Scholar] [CrossRef]
- Li, T.; Jafari, D.; Meyer, C.; Voroba, A.; Haddad, G.; Abecassis, S.; Bank, M.; Dym, A.; Naqvi, A.; Gujral, R.; et al. Video laryngoscopy is associated with improved first-pass intubation success compared with direct laryngoscopy in emergency department trauma patients. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12373. [Google Scholar] [CrossRef]
- Avva, U.; Lata, J.M.; Kiel, J. Airway Management. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2017. [Google Scholar]
- Mort, T.C. Emergency tracheal intubation: Complications associated with repeated laryngoscopic attempts. Anesth. Analg. 2004, 99, 607–613. [Google Scholar] [CrossRef]
- Wozniak, M.; Arnell, K.; Brown, M.; Gonzales, S.; Lazarus, D.; Rich, W.; Katheria, A. The 30-second rule: The effects of prolonged intubation attempts on oxygen saturation and heart rate in preterm infants in the delivery room. Minerva Pediatr. 2018, 70, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Keenan, B.T.; Wiemken, A.; Staley, B.; Chi, L.; Pack, A.I.; Gislason, T.; Schwab, R.J. 0438 Upper Airway Anatomical Differences between Chinese and Caucasian Patients with Obstructive Sleep Apnea. Sleep 2019, 42, A177. [Google Scholar] [CrossRef]
- Dominelli, P.B.; Ripoll, J.G.; Cross, T.J.; Baker, S.E.; Wiggins, C.C.; Welch, B.T.; Joyner, M.J. Sex differences in large conducting airway anatomy. J. Appl. Physiol. 2018, 125, 960–965. [Google Scholar] [CrossRef]
- Hunter, E.J.; Tanner, K.; Smith, M.E. Gender differences affecting vocal health of women in vocally demanding careers. Logop. Phoniatr. Vocology 2011, 36, 128–136. [Google Scholar] [CrossRef]
- Riede, T.; Stein, A.; Baab, K.L.; Hoxworth, J.M. Post-pubertal developmental trajectories of laryngeal shape and size in humans. Sci. Rep. 2023, 13, 7673. [Google Scholar] [CrossRef]
- Hwang, S.M. A good laryngeal view does not guarantee perfectly successful tracheal intubation. Korean J. Anesthesiol. 2016, 69, 111–112. [Google Scholar] [CrossRef] [PubMed]
- Thierry, S.; Jaulin, F.; Starck, C.; Ariès, P.; Schmitz, J.; Kerkhoff, S.; Bernard, C.I.; Komorowski, M.; Warnecke, T.; Hinkelbein, J. Evaluation of free-floating tracheal intubation in weightlessness via ice-pick position with a direct laryngoscopy and classic approach with indirect videolaryngoscopy. npj Microgravity 2023, 9, 73. [Google Scholar] [CrossRef] [PubMed]

| Blade 3 (n = 96) | Blade 4 (n = 96) | p Value | |
|---|---|---|---|
| Age, years (mean [SD]) | 44.1 (16.0) | 47.3 (16.7) | 0.173 |
| Male (number [%]) | 92 (95.8) | 91 (94.8) | 0.733 |
| Patients with Mallampati class > 2, (number [%]) | 13 (13.5) | 13 (13.5) | >0.999 |
| Thyromental height, cm (mean [SD]) | 5 (1.0) | 5.1 (1.0) | 0.301 |
| Thyromental distance, cm (mean [SD]) | 9.6 (1.3) | 9.9 (1.3) | 0.183 |
| Sternomental distance, cm (mean [SD]) | 17.1 (2.0) | 16.9 (1.8) | 0.487 |
| Mouth opening, cm (mean [SD]) | 5.7 (0.8) | 5.7 (0.7) | 0.816 |
| Neck circumference, cm (mean [SD]) | 40.4 (3.2) | 40.4 (2.7) | 0.951 |
| Height, cm (mean [SD]) | 175.9 (4.5) | 175.5 (5.0) | 0.505 |
| Weight, kg (mean [SD]) | 81.5 (16.4) | 80.7 (12.9) | 0.710 |
| Variables | Full Variables Model | Backward Elimination Model | ||
|---|---|---|---|---|
| Unstandardized Coefficient (95% Confidence Interval) | p Value | Unstandardized Coefficient (95% Confidence Interval) | p Value | |
| Blade size 4 (reference: blade size 3) | −13 (−19–−7) | <0.001 | −13 (−19–−7) | <0.001 |
| Height (cm) | 0 (−1–1) | 0.819 | Eliminated | |
| Age (year) | 0 (−1–−0.28) | <0.001 | 0 (−1–0) | <0.001 |
| Female | 6 (−9–21) | 0.433 | Eliminated | |
| Mallampati class | −1 (−4–3) | 0.684 | Eliminated | |
| Thyromental height (cm) | 0 (−3–4) | 0.791 | Eliminated | |
| Thyromental distance (cm) | 3 (−0–5) | 0.06 | 3 (0–6) | 0.003 |
| Sternomental distance (cm) | 1 (−1–3) | 0.149 | 1 (0–3) | 0.146 |
| Mouth opening (cm) | 2 (−2–6) | 0.252 | Eliminated | |
| Neck circumference (cm) | 0 (−2–1) | 0.625 | −1 (−2–0) | 0.108 |
| Weight (kg) | 0 (0–0) | 0.649 | Eliminated | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-H.; Cheon, B.-R.; Kim, H.; Hwang, S.-M.; Lee, J.-J.; Kwon, Y.-S. Influence of Curved Video Laryngoscope Blade Sizes and Patient Heights on Video Laryngoscopic Views: A Randomized Controlled Trial. J. Pers. Med. 2024, 14, 209. https://doi.org/10.3390/jpm14020209
Kim J-H, Cheon B-R, Kim H, Hwang S-M, Lee J-J, Kwon Y-S. Influence of Curved Video Laryngoscope Blade Sizes and Patient Heights on Video Laryngoscopic Views: A Randomized Controlled Trial. Journal of Personalized Medicine. 2024; 14(2):209. https://doi.org/10.3390/jpm14020209
Chicago/Turabian StyleKim, Jong-Ho, Bo-Reum Cheon, Hyesook Kim, Sung-Mi Hwang, Jae-Jun Lee, and Young-Suk Kwon. 2024. "Influence of Curved Video Laryngoscope Blade Sizes and Patient Heights on Video Laryngoscopic Views: A Randomized Controlled Trial" Journal of Personalized Medicine 14, no. 2: 209. https://doi.org/10.3390/jpm14020209
APA StyleKim, J.-H., Cheon, B.-R., Kim, H., Hwang, S.-M., Lee, J.-J., & Kwon, Y.-S. (2024). Influence of Curved Video Laryngoscope Blade Sizes and Patient Heights on Video Laryngoscopic Views: A Randomized Controlled Trial. Journal of Personalized Medicine, 14(2), 209. https://doi.org/10.3390/jpm14020209