Is Augmented Reality Technology Effective in Locating the Apex of Teeth Undergoing Apicoectomy Procedures?
Abstract
1. Background
2. Methods
2.1. Study Design
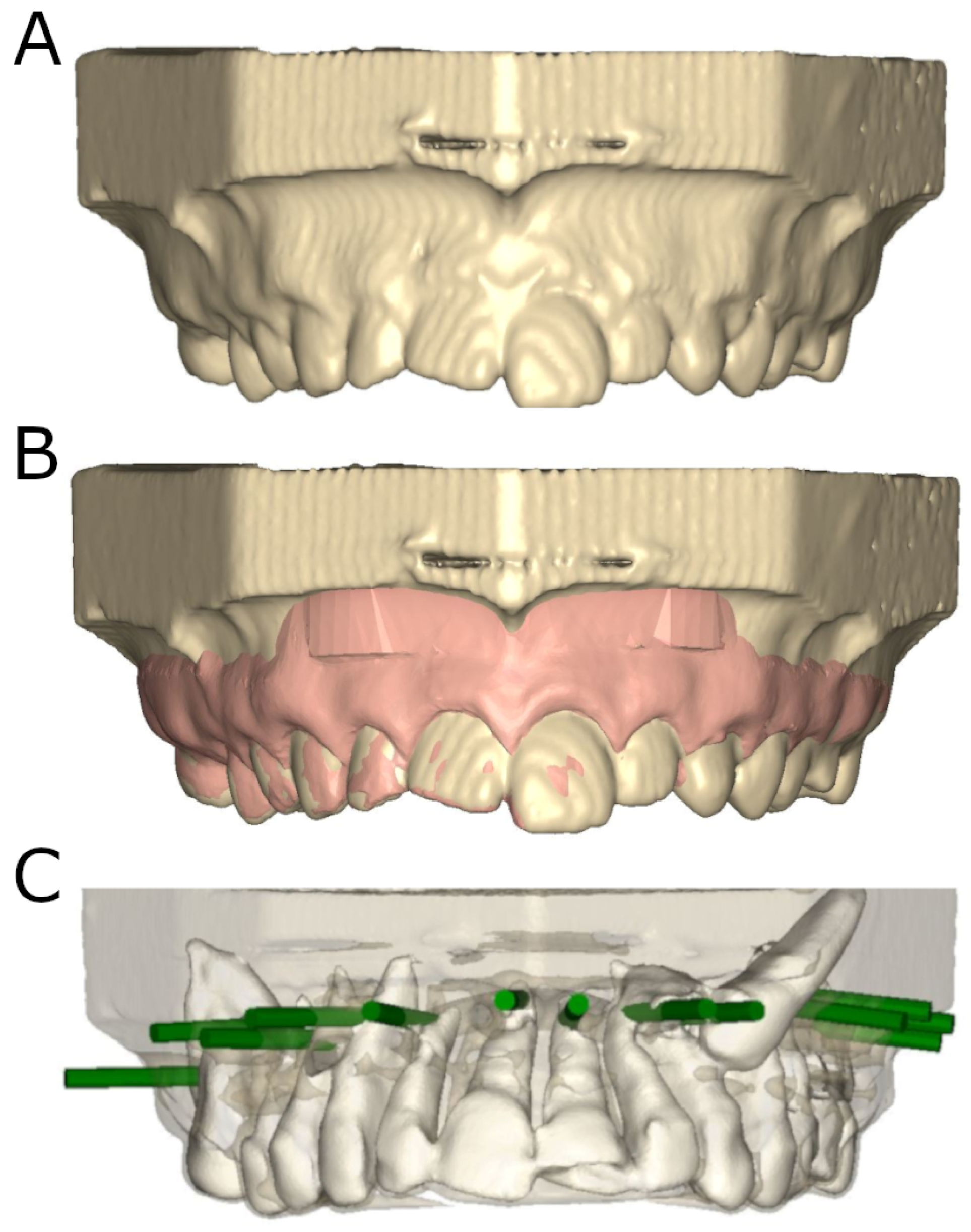
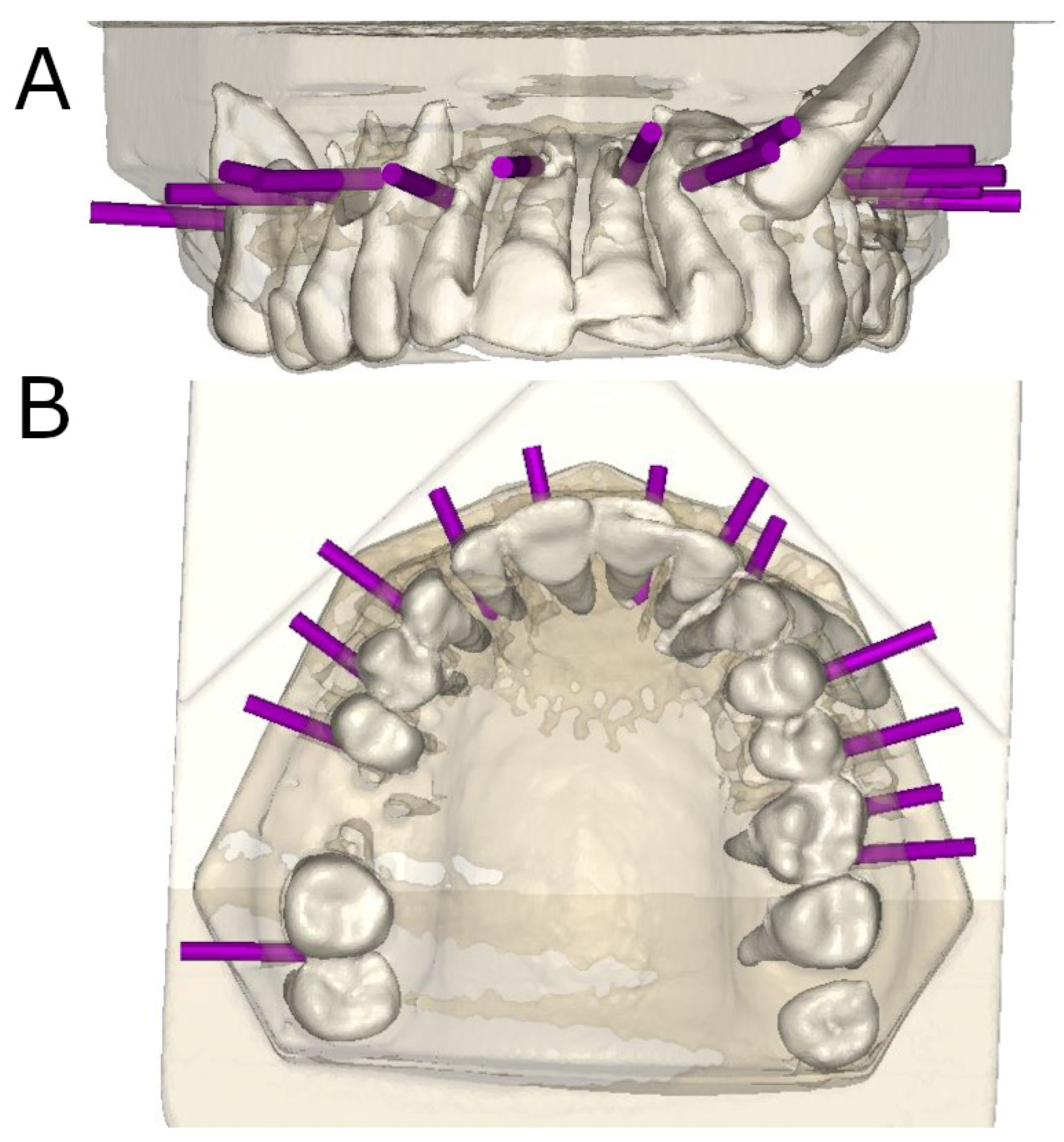
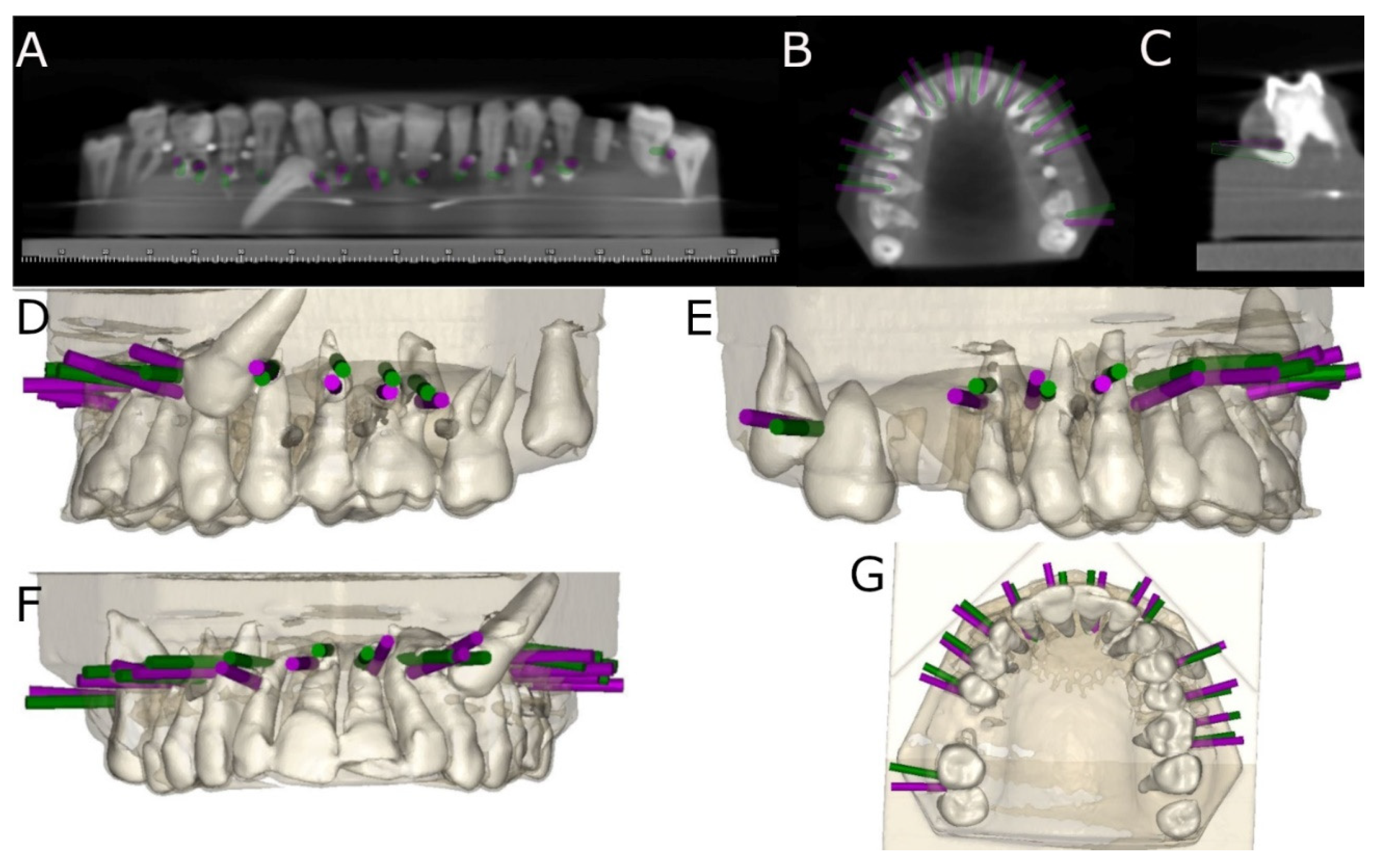
2.2. Experimental Procedure
2.3. Measurement Procedure
2.4. Statistical Tests
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Javier, F.C.; Pascual Sevillano, M.Á. La Producción Científica Sobre Realidad Aumentada, Un Análisis De La Situación Educativa Desde La Perspectiva SCOPUS. Edmetic 2016, 6, 39–61. [Google Scholar]
- Morimoto, T.; Kobayashi, T.; Hirata, H.; Otani, K.; Sugimoto, M.; Tsukamoto, M.; Yoshihara, T.; Ueno, M.; Mawatari, M. XR (Extended Reality: Virtual Reality, Augmented Reality, Mixed Reality) Technology in Spine Medicine: Status Quo and Quo Vadis. J. Clin. Med. 2022, 11, 470. [Google Scholar] [CrossRef]
- Eckert, M.; Volmerg, J.S.; Friedrich, C.M. Augmented Reality in Medicine: Systematic and Bibliographic Review. JMIR Mhealth Uhealth 2019, 7, e10967. [Google Scholar] [CrossRef] [PubMed]
- Munzer, B.W.; Khan, M.M.; Shipman, B.; Mahajan, P. Augmented Reality in Emergency Medicine: A Scoping Review. J. Med. Internet Res. 2019, 21, e12368. [Google Scholar] [CrossRef] [PubMed]
- Meola, A.; Cutolo, F.; Carbone, M.; Cagnazzo, F.; Ferrari, M.; Ferrari, V. Augmented reality in neurosurgery: A systematic review. Neurosurg. Rev. 2017, 40, 537–548. [Google Scholar] [CrossRef]
- Chicchi Giglioli, I.A.; Pallavicini, F.; Pedroli, E.; Serino, S.; Riva, G. Augmented Reality: A Brand New Challenge for the Assessment and Treatment of Psychological Disorders. Comput. Math. Methods Med. 2015, 2015, 862942. [Google Scholar] [CrossRef] [PubMed]
- Berryman, D.R. Augmented reality: A review. Med. Ref. Serv. Q. 2012, 31, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Cabrilo, I.; Bijlenga, P.; Schaller, K. Augmented reality in the surgery of cerebral arteriovenous malformations: Technique assessment and considerations. Acta Neurochir. 2014, 156, 1769–1774. [Google Scholar] [CrossRef]
- Cabrilo, I.; Bijlenga, P.; Schaller, K. Augmented reality in the surgery of cerebral aneurysms: A technical report. Neurosurgery 2014, 10 (Suppl. S2), 252–260; discussion 260–261. [Google Scholar] [CrossRef]
- Cabrilo, I.; Sarrafzadeh, A.; Bijlenga, P.; Landis, B.N.; Schaller, K. Augmented reality-assisted skull base surgery. Neurochirurgie 2014, 60, 304–306. [Google Scholar] [CrossRef]
- Cabrilo, I.; Schaller, K.; Bijlenga, P. Augmented reality-assisted bypass surgery: Embracing minimal invasiveness. World Neurosurg. 2015, 83, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Li, F.; Wang, M.; Song, Z. Easy-to-use augmented reality neuronavigation using a wireless tablet PC. Ster. Funct. Neurosurg. 2014, 92, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lopez, F.; Maina, M.F.; Arango, F.; Saigí-Rubió, F. Use of a Low-Cost PorTable 3D Virtual Reality Simulator for Psychomotor Skill Training in Minimally Invasive Surgery: Task Metrics and Score Validity. JMIR Serious Games 2020, 8, e19723. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Onda, S.; Yanaga, K.; Suzuki, N.; Hattori, A. Clinical application of navigation surgery using augmented reality in the abdominal field. Surg. Today 2015, 45, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Rocco, N.; Velotti, N.; Pontillo, M.; Vitiello, A.; Berardi, G.; Accurso, A.; Masone, S.; Musella, M. New techniques versus standard mapping for sentinel lymph node biopsy in breast cancer: A systematic review and meta-analysis. Updat. Surg. 2023, 75, 1699–1710. [Google Scholar] [CrossRef] [PubMed]
- Szabó, E.V.; Huszta, B.; Polyák, M.; Ruksakiet, K.; Bernáth, R.; Ghidán, Á.; Csáki, Á.; Kostadinova, M.; Dinya, E.; Vág, J.; et al. Antimicrobial efficacy of sodium hypochlorite and hyper-pure chlorine dioxide in the depth of dentin tubules in vitro. BMC Oral. Health 2023, 23, 930. [Google Scholar] [CrossRef]
- Selvakumar, G.; Raveendran, A.; Swathika, B.; Ganesan, S.; Kumar, P.; Sanyal, G.C. Evaluation of the Anti-microbial Efficacy of a Novel Endodontic Irrigant Against Enterococcus faecalis: An In Vitro Study. Cureus 2023, 15, e46410. [Google Scholar] [CrossRef]
- de Chevigny, C.; Dao, T.T.; Basrani, B.R.; Marquis, V.; Farzaneh, M.; Abitbol, S.; Friedman, S. Treatment outcome in endodontics: The Toronto study--phases 3 and 4: Orthograde retreatment. J. Endod. 2008, 34, 131–137. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Muñoz, A.P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An in Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef]
- Nagendrababu, V.; Murray, P.E.; Ordinola-Zapata, R.; Peters, O.A.; Rôças, I.N.; Siqueira, J.F., Jr.; Priya, E.; Jayaraman, J.J.; Pulikkotil, S.; Camilleri, J.; et al. PRILE 2021 guidelines for reporting laboratory studies in Endodontology: A consensus-based development. Int. Endod. J. 2021, 54, 1482–1490. [Google Scholar] [CrossRef]
- Nagendrababu, V.; Murray, P.E.; Ordinola-Zapata, R.; Peters, O.A.; Rôças, I.N.; Siqueira, J.F., Jr.; Priya, E.; Jayaraman, J.; Pulikkotil, S.J.; Suresh, N.; et al. PRILE 2021 guidelines for reporting laboratory studies in Endodontology: Explanation and elaboration. Int. Endod. J. 2021, 54, 1491–1515. [Google Scholar] [CrossRef] [PubMed]
- Cáceres Madroño, E.; Rodríguez Torres, P.; Oussama, S.; Zubizarreta-Macho, Á.; Bufalá Pérez, M.; Mena-Álvarez, J.; Riad Deglow, E.; Hernández Montero, S. A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study. J. Pers. Med. 2021, 11, 1034. [Google Scholar] [CrossRef]
- Reidsma, D.; Katayose, H.; Nijholt, A. Advances in computer entertainment. In Proceedings of the10th International Conference, ACE 2013, Bekel, The Netherlands, 12–15 November 2013; Springer: Berlin, The Netherlands, 2013. [Google Scholar]
- Mahmud, N.; Cohen, J.; Tsourides, K.; Berzin, T.M. Computer vision and augmented reality in gastrointestinal endoscopy. Gastroenterol. Rep. 2015, 3, 179–184. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sicilia, A.; Botticelli, D. Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAOConsensus Conference 2012. Clin. Oral. Implant. Res. 2012, 23, 157–161. [Google Scholar] [CrossRef]
- Kohli, M.R.; Berenji, H.; Setzer, F.C.; Lee, S.M.; Karabucak, B. Outcome of Endodontic Surgery: A Meta-analysis of the Literature—Part 3: Comparison of Endodontic Microsurgical Techniques with 2 Different Root-end Filling Materials. J. Endod. 2018, 44, 923–931. [Google Scholar] [CrossRef]
- Setzer, F.C.; Kohli, M.R.; Shah, S.B.; Karabucak, B.; Kim, S. Outcome of endodontic surgery: A meta-analysis of the literature—Part 2: Comparison of endodontic microsurgical techniques with and without the use of higher magnification. J. Endod. 2012, 38, 1–10. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402.e6. [Google Scholar] [CrossRef] [PubMed]
- Zubizarreta-Macho, Á.; Castillo-Amature, C.; Montiel-Company, J.M.; Mena-Álvarez, J. Efficacy of Computer-Aided Static Navigation Technique on the Accuracy of Endodontic Microsurgery. A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 313. [Google Scholar] [CrossRef]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assited implant surgery in single tooth space: A randomized controlled trial. Clin. Oral. Implant. Res. 2019, 30, 505–514. [Google Scholar] [CrossRef]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral. Maxillofac. Implant 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Guzmán, A.M.; Deglow, E.R.; Zubizarreta-Macho, Á.; Agustín-Panadero, R.; Montero, S.H. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Navigation for Dental Implants Placement: An In Vitro Study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef]
- Block, M.; Emery, R.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral. Maxillofac. Implant 2017, 32, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Chong, B.S.; Dhesi, M.; Makdissi, J. Computer-aided dynamic navigation: A novel method for guided endodontics. Quintessence Int. 2019, 50, 196–202. [Google Scholar]
- Jain, S.D.; Carrico, C.K.; Bermanis, I. 3-Dimensional Accuracy of Dynamic Navigation Technology in Locating Calcified Canals. J. Endod. 2020, 46, 839–845. [Google Scholar] [CrossRef]
- Abate, A.; Cavagnetto, D.; Rusconi, F.M.E.; Cressoni, P.; Esposito, L. Safety and Effects of the Rapid Maxillary Expander on Temporomandibular Joint in Subjects Affected by Juvenile Idiopathic Arthritis: A Retrospective Study. Children 2021, 8, 33. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Valle Castaño, S.; Montiel-Company, J.M.; Mena-Álvarez, J. Effect of Computer-Aided Navigation Techniques on the Accuracy of Endodontic Access Cavities: A Systematic Review and Meta-Analysis. Biology 2021, 10, 212. [Google Scholar] [CrossRef] [PubMed]
- Sutter, E.; Lotz, M.; Rechenberg, D.-K.; Stadlinger, B.; Rücker, M.; Valdec, S. Guided apicoectomy using a CAD/CAM drilling template. Int. J. Comput. Dent. 2019, 22, 363–369. [Google Scholar]
- Antal, M.; Nagy, E.; Sanyó, L.; Braunitzer, G. Digitally planned root end surgery with static guide and custom trephine burs: A case report. Int. J. Med. Robot. Comput. Assist. Surg. 2020, 16, e2115. [Google Scholar] [CrossRef]
- Eszter, N.; Mark, F.; Mark, A. Guided modern endodontic microsurgery by use of a trephine bur. Orv. Hetil. 2020, 161, 1260–1265. [Google Scholar]
- Giacomino, C.M.; Ray, J.J.; Wealleans, J.A. Targeted Endodontic Microsurgery: A Novel Approach to Anatomically Challenging Scenarios Using 3-dimensional–printed Guides and Trephine Burs—A Report of 3 Cases. J. Endod. 2018, 44, 671–677. [Google Scholar] [CrossRef]


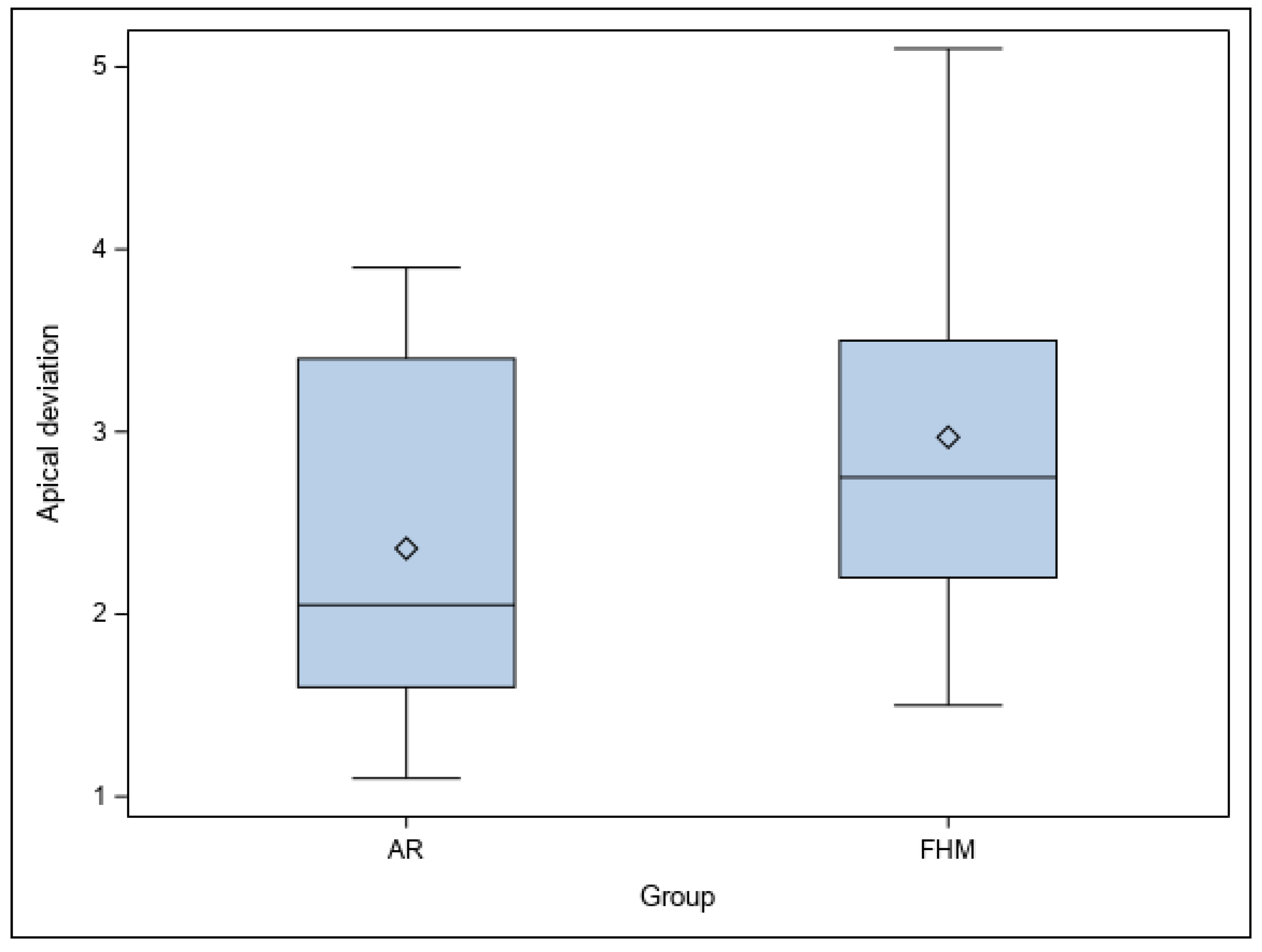
| Location | Group | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Coronal | AR | 30 | 2.71 a | 0.79 | 1.70 | 4.40 |
| FHM | 30 | 3.43 a | 1.21 | 1.70 | 5.10 | |
| Apical | AR | 30 | 2.36 a | 0.96 | 1.10 | 3.90 |
| FHM | 30 | 2.97 a | 1.26 | 1.50 | 5.10 | |
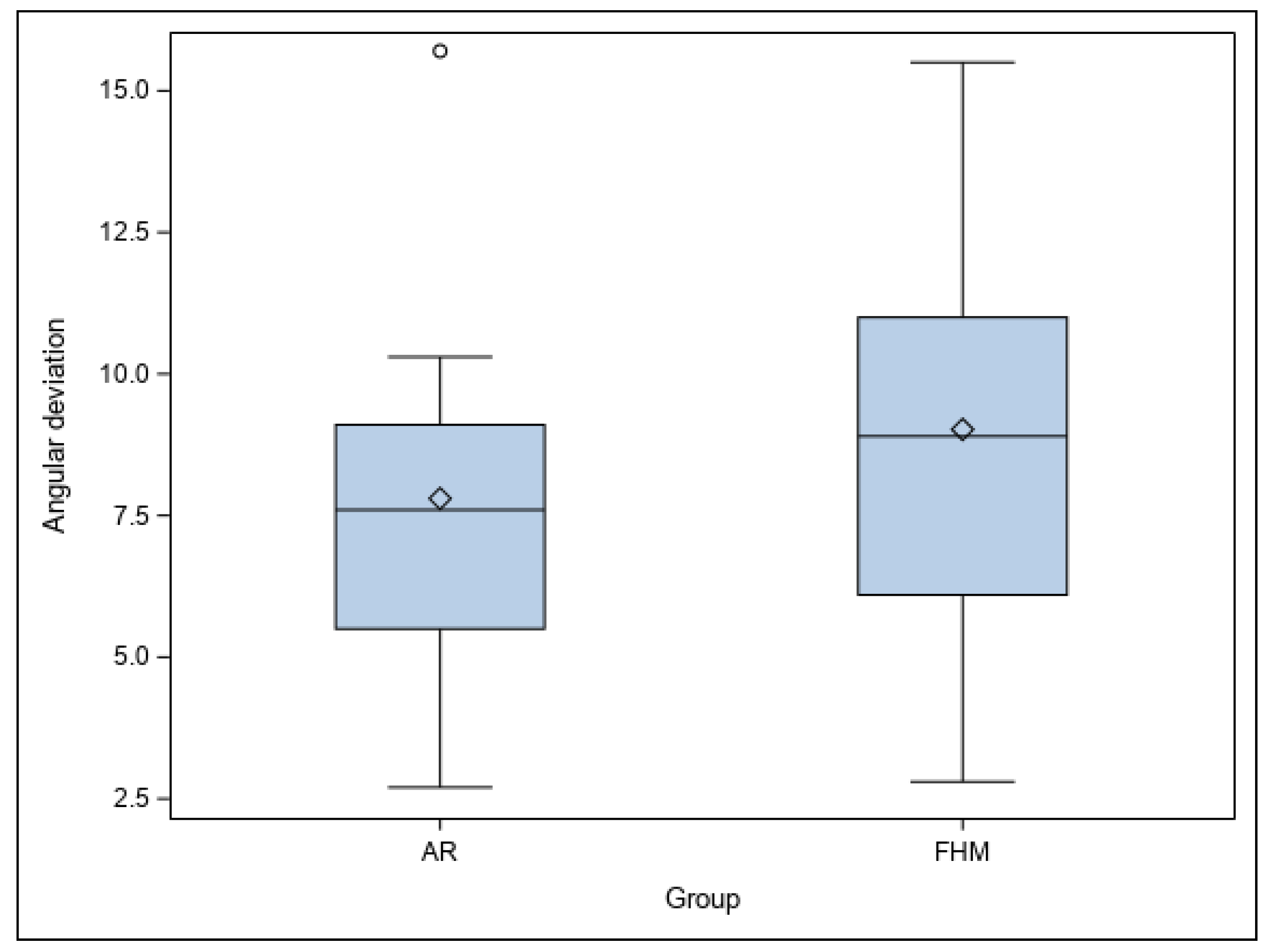
| Angular | AR | 30 | 7.80 a | 3.57 | 2.70 | 15.70 |
| FHM | 30 | 9.02 a | 4.07 | 2.80 | 15.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tamayo-Estebaranz, N.; Viñas, M.J.; Arrieta-Blanco, P.; Zubizarreta-Macho, Á.; Aragoneses-Lamas, J.M. Is Augmented Reality Technology Effective in Locating the Apex of Teeth Undergoing Apicoectomy Procedures? J. Pers. Med. 2024, 14, 73. https://doi.org/10.3390/jpm14010073
Tamayo-Estebaranz N, Viñas MJ, Arrieta-Blanco P, Zubizarreta-Macho Á, Aragoneses-Lamas JM. Is Augmented Reality Technology Effective in Locating the Apex of Teeth Undergoing Apicoectomy Procedures? Journal of Personalized Medicine. 2024; 14(1):73. https://doi.org/10.3390/jpm14010073
Chicago/Turabian StyleTamayo-Estebaranz, Nuria, María José Viñas, Patricia Arrieta-Blanco, Álvaro Zubizarreta-Macho, and Juan Manuel Aragoneses-Lamas. 2024. "Is Augmented Reality Technology Effective in Locating the Apex of Teeth Undergoing Apicoectomy Procedures?" Journal of Personalized Medicine 14, no. 1: 73. https://doi.org/10.3390/jpm14010073
APA StyleTamayo-Estebaranz, N., Viñas, M. J., Arrieta-Blanco, P., Zubizarreta-Macho, Á., & Aragoneses-Lamas, J. M. (2024). Is Augmented Reality Technology Effective in Locating the Apex of Teeth Undergoing Apicoectomy Procedures? Journal of Personalized Medicine, 14(1), 73. https://doi.org/10.3390/jpm14010073











