Radiation Dose to Critical Cardiac Structures from Three-Dimensional Conformal Radiation Therapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) Techniques for Left-Sided Breast Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Planning Computed Tomorgaphy
2.3. Treatment Planning
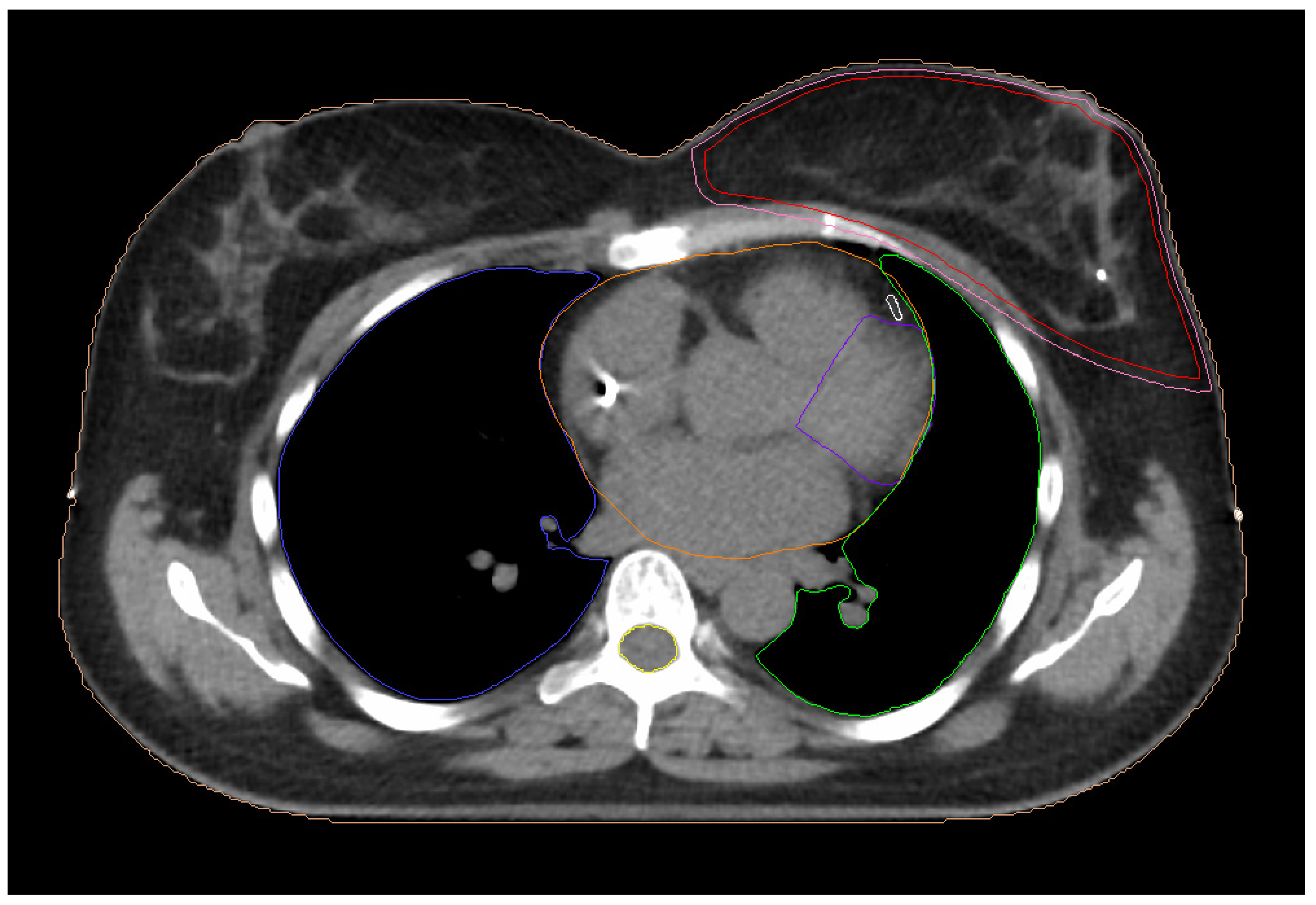
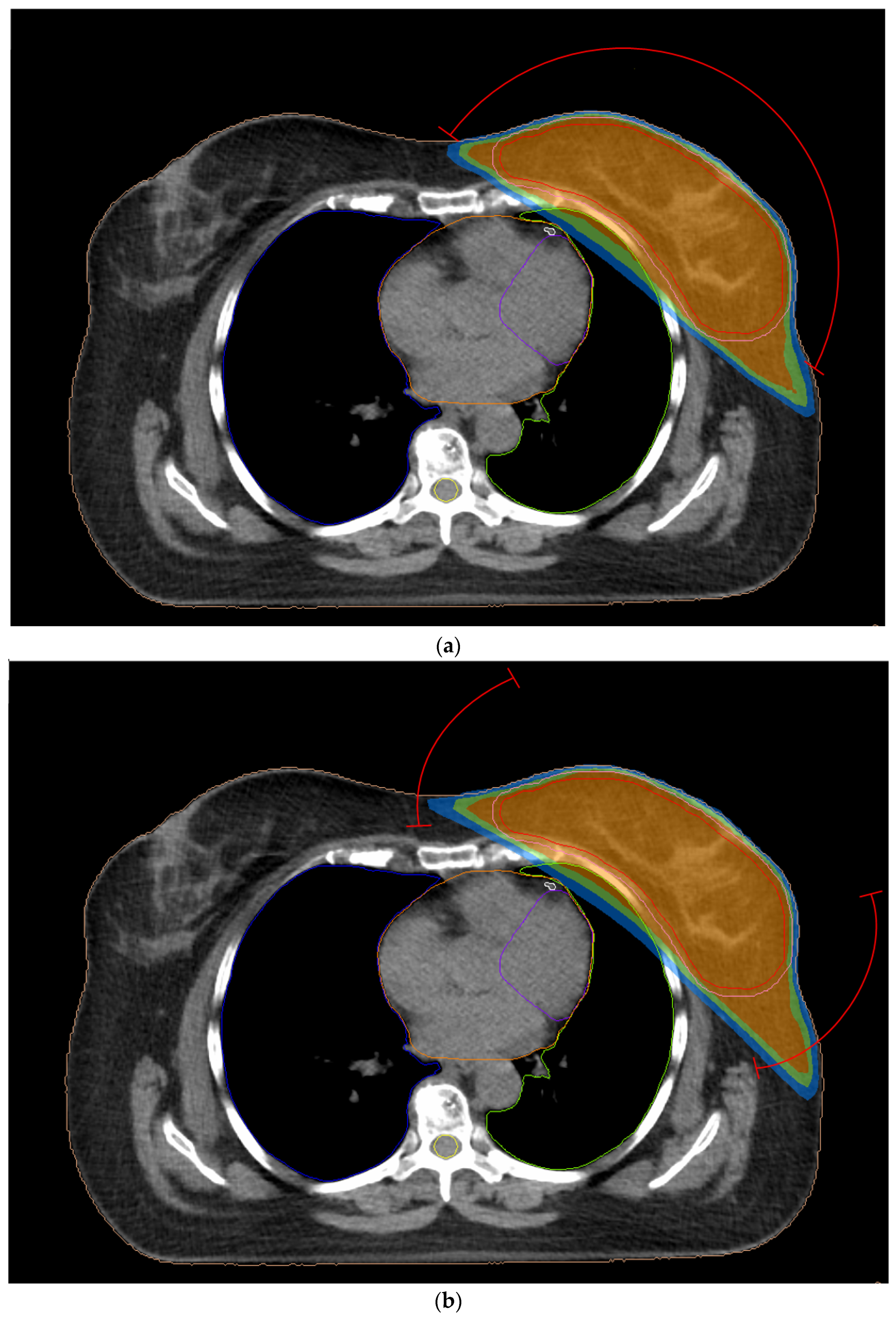
2.3.1. 3D-CRT Technique
2.3.2. Two-Field IMRT Technique (2F-IMRT)
2.3.3. Seven-Field IMRT Technique (7F-IMRT)
2.3.4. Two Partial-Arc VMAT Technique (VMAT1)
2.3.5. Four Partial-Arc VMAT Technique (VMAT2)
2.4. Statistical Analysis
3. Results
3.1. Treatment Evaluation
3.2. Exposure of Cardiac Structures
3.2.1. Left Anterior Descending Artery (LAD)
3.2.2. Left Ventricle (LV)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Howlader, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. (Eds.) SEER Cancer Statistics Review, 1975–2018; National Cancer Institute: Bethesda, MD, USA, 2023. Available online: https://seer.cancer.gov/csr/1975_2018/ (accessed on 15 October 2023).
- Duffy, S.W.; Tabár, L.; Yen, A.M.; Dean, P.B.; Smith, R.A.; Jonsson, H.; Törnberg, S.; Chen, S.L.; Chiu, S.Y.; Fann, J.C.; et al. Mammography Screening Reduces Rates of Advanced and Fatal Breast Cancers: Results in 549,091 Women. Cancer 2020, 126, 2971–2979. [Google Scholar] [CrossRef] [PubMed]
- Kerr, A.J.; Dodwell, D.; McGale, P.; Holt, F.; Duane, F.; Mannu, G.; Darby, S.C.; Taylor, C.W. Adjuvant and Neoadjuvant Breast Cancer Treatments: A Systematic Review of Their Effects on Mortality. Cancer Treat. Rev. 2022, 105, 102375. [Google Scholar] [CrossRef] [PubMed]
- Bellon, J.R.; Wong, J.S.; MacDonald, S.M.; Ho, A.Y. (Eds.) Radiation Therapy Techniques and Treatment Planning for Breast Cancer; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group. Effect of Radiotherapy after Breast-Conserving Surgery on 10-Year Recurrence and 15-Year Breast Cancer Death: Meta-Analysis of Individual Patient Data for 10 801 Women in 17 Randomised Trials. Lancet 2011, 378, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative Group. Effects of Radiotherapy and of Differences in the Extent of Surgery for Early Breast Cancer on Local Recurrence and 15-Year Survival: An Overview of the Randomised Trials. Lancet 2005, 366, 2087–2106. [Google Scholar] [CrossRef] [PubMed]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Nie, X.; Ji, C.; Lin, X.; Liu, L.; Chen, X.; Yao, H.; Wu, S. Long-Term Cardiovascular Risk After Radiotherapy in Women With Breast Cancer. J. Am. Heart Assoc. 2017, 6, e005633. [Google Scholar] [CrossRef] [PubMed]
- Wennstig, A.-K.; Wadsten, C.; Garmo, H.; Fredriksson, I.; Blomqvist, C.; Holmberg, L.; Nilsson, G.; Sund, M. Long-Term Risk of Ischemic Heart Disease after Adjuvant Radiotherapy in Breast Cancer: Results from a Large Population-Based Cohort. Breast Cancer Res. 2020, 22, 10. [Google Scholar] [CrossRef]
- Correa, C.R.; Litt, H.I.; Hwang, W.-T.; Ferrari, V.A.; Solin, L.J.; Harris, E.E. Coronary Artery Findings After Left-Sided Compared With Right-Sided Radiation Treatment for Early-Stage Breast Cancer. J. Clin. Oncol. 2007, 25, 3031–3037. [Google Scholar] [CrossRef]
- Sardar, P.; Kundu, A.; Chatterjee, S.; Nohria, A.; Nairooz, R.; Bangalore, S.; Mukherjee, D.; Aronow, W.S.; Lavie, C.J. Long-term Cardiovascular Mortality after Radiotherapy for Breast Cancer: A Systematic Review and Meta-analysis. Clin. Cardiol. 2017, 40, 73–81. [Google Scholar] [CrossRef]
- Bouillon, K.; Haddy, N.; Delaloge, S.; Garbay, J.-R.; Garsi, J.-P.; Brindel, P.; Mousannif, A.; Lê, M.G.; Labbe, M.; Arriagada, R.; et al. Long-Term Cardiovascular Mortality after Radiotherapy for Breast Cancer. J. Am. Coll. Cardiol. 2011, 57, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, G.; Holmberg, L.; Garmo, H.; Duvernoy, O.; Sjögren, I.; Lagerqvist, B.; Blomqvist, C. Distribution of Coronary Artery Stenosis After Radiation for Breast Cancer. J. Clin. Oncol. 2012, 30, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Wennstig, A.-K.; Garmo, H.; Isacsson, U.; Gagliardi, G.; Rintelä, N.; Lagerqvist, B.; Holmberg, L.; Blomqvist, C.; Sund, M.; Nilsson, G. The Relationship between Radiation Doses to Coronary Arteries and Location of Coronary Stenosis Requiring Intervention in Breast Cancer Survivors. Radiat. Oncol. 2019, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Camilleri, J.; Derreumaux, S.; Walker, V.; Lairez, O.; Lapeyre, M.; Bruguière, E.; Pathak, A.; Bernier, M.-O.; Laurier, D.; et al. Is Mean Heart Dose a Relevant Surrogate Parameter of Left Ventricle and Coronary Arteries Exposure during Breast Cancer Radiotherapy: A Dosimetric Evaluation Based on Individually-Determined Radiation Dose (BACCARAT Study). Radiat. Oncol. 2019, 14, 29. [Google Scholar] [CrossRef] [PubMed]
- Kaidar-Person, O.; Zagar, T.M.; Oldan, J.D.; Matney, J.; Jones, E.L.; Das, S.; Jensen, B.C.; Zellars, R.C.; Wong, T.Z.; Marks, L.B. Early Cardiac Perfusion Defects after Left-Sided Radiation Therapy for Breast Cancer: Is There a Volume Response? Breast Cancer Res. Treat. 2017, 164, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Walker, V.; Lairez, O.; Fondard, O.; Pathak, A.; Pinel, B.; Chevelle, C.; Franck, D.; Jimenez, G.; Camilleri, J.; Panh, L.; et al. Early Detection of Subclinical Left Ventricular Dysfunction after Breast Cancer Radiation Therapy Using Speckle-Tracking Echocardiography: Association between Cardiac Exposure and Longitudinal Strain Reduction (BACCARAT Study). Radiat. Oncol. 2019, 14, 204. [Google Scholar] [CrossRef]
- Fourati, N.; Charfeddine, S.; Chaffai, I.; Dhouib, F.; Farhat, L.; Boukhris, M.; Abid, L.; Kammoun, S.; Mnejja, W.; Daoud, J. Subclinical Left Ventricle Impairment Following Breast Cancer Radiotherapy: Is There an Association between Segmental Doses and Segmental Strain Dysfunction? Int. J. Cardiol. 2021, 345, 130–136. [Google Scholar] [CrossRef]
- Song, J.; Tang, T.; Caudrelier, J.-M.; Bélec, J.; Chan, J.; Lacasse, P.; Aldosary, G.; Nair, V. Dose-Sparing Effect of Deep Inspiration Breath Hold Technique on Coronary Artery and Left Ventricle Segments in Treatment of Breast Cancer. Radiother. Oncol. 2021, 154, 101–109. [Google Scholar] [CrossRef]
- Eber, J.; Schmitt, M.; Dehaynin, N.; Le Fèvre, C.; Antoni, D.; Noël, G. Evaluation of Cardiac Substructures Exposure of DIBH-3DCRT, FB-HT, and FB-3DCRT in Hypofractionated Radiotherapy for Left-Sided Breast Cancer after Breast-Conserving Surgery: An In Silico Planning Study. Cancers 2023, 15, 3406. [Google Scholar] [CrossRef]
- Chang, J.S.; Chang, J.H.; Kim, N.; Kim, Y.B.; Shin, K.H.; Kim, K. Intensity Modulated Radiotherapy and Volumetric Modulated Arc Therapy in the Treatment of Breast Cancer: An Updated Review. J. Breast Cancer 2022, 25, 349. [Google Scholar] [CrossRef]
- Kuzba-Kryszak, T.; Nowakowski, S.; Winiecki, J.; Makarewicz, R. Comparative Analysis of the Absorbed Dose in the Heart and Anterior Descending Branch of the Left Coronary Artery (LAD) in Patients with Left-Sided Breast Cancer Who Received Radiotherapy Using 3D-CRT, IMRT and VMAT Techniques. J. BUON Off. J. Balk. Union Oncol. 2021, 26, 753–758. [Google Scholar]
- Offersen, B.V.; Boersma, L.J.; Kirkove, C.; Hol, S.; Aznar, M.C.; Biete Sola, A.; Kirova, Y.M.; Pignol, J.-P.; Remouchamps, V.; Verhoeven, K.; et al. ESTRO Consensus Guideline on Target Volume Delineation for Elective Radiation Therapy of Early Stage Breast Cancer. Radiother. Oncol. 2015, 114, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Duane, F.; Aznar, M.C.; Bartlett, F.; Cutter, D.J.; Darby, S.C.; Jagsi, R.; Lorenzen, E.L.; McArdle, O.; McGale, P.; Myerson, S.; et al. A Cardiac Contouring Atlas for Radiotherapy. Radiother. Oncol. 2017, 122, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Biedka, M.; Zmuda, E. Contouring of the left anterior descending coronary artery in patients with breast cancer–The radiation oncologist’s view. Nowotowory. J. Oncol. 2020, 70, 60–64. [Google Scholar]
- Goyal, S.; Buchholz, T.; Haffy, G.B. Breast Cancer: Early Stage. In Principles and Practice of Radiation Oncology, 7th ed.; Halperin, C.E., Wazer, E.D., Perez, A.C., Brady, W.L., Eds.; Wolters Kluwer: Philadelphia, PA, USA, 2019; p. 1332. [Google Scholar]
- Jeulink, M.; Dahele, M.; Meijnen, P.; Slotman, B.J.; Verbakel, W.F.A.R. Is There a Preferred IMRT Technique for Left-breast Irradiation? J. Appl. Clin. Med. Phys. 2015, 16, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Kataria, T.; Goyal, S.; Malik, A.; Kumar, K.; Shyam, S.B.; Deepak, G. Modulated Radiotherapy for Breast Cancer: Locoregional Outcomes. Int. J. Radiol. Radiat. Ther. 2016, 1, 00003. [Google Scholar] [CrossRef]
- Thomsen, M.S.; Berg, M.; Zimmermann, S.; Lutz, C.M.; Makocki, S.; Jensen, I.; Hjelstuen, M.H.B.; Pensold, S.; Hasler, M.P.; Jensen, M.-B.; et al. Dose Constraints for Whole Breast Radiation Therapy Based on the Quality Assessment of Treatment Plans in the Randomised Danish Breast Cancer Group (DBCG) HYPO Trial. Clin. Transl. Radiat. Oncol. 2021, 28, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Piroth, M.D.; Baumann, R.; Budach, W.; Dunst, J.; Feyer, P.; Fietkau, R.; Haase, W.; Harms, W.; Hehr, T.; Krug, D.; et al. Heart Toxicity from Breast Cancer Radiotherapy: Current Findings, Assessment, and Prevention. Strahlenther. Onkol. 2019, 195, 1–12. [Google Scholar] [CrossRef]
- Chen, C.-P.; Chen, T.-H.; Chiou, J.-F.; Chen, Y.-J.; Kuo, C.-C.; Tseng, K.-H.; Chung, M.-Y.; Chen, C.-Y.; Wu, J.-Y.; Lu, L.-S.; et al. Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT. J. Pers. Med. 2022, 12, 1368. [Google Scholar] [CrossRef]
- Ott, O.J.; Stillkrieg, W.; Lambrecht, U.; Schweizer, C.; Lamrani, A.; Sauer, T.-O.; Strnad, V.; Bert, C.; Hack, C.C.; Beckmann, M.W.; et al. External-Beam-Accelerated Partial-Breast Irradiation Reduces Organ-at-Risk Doses Compared to Whole-Breast Irradiation after Breast-Conserving Surgery. Cancers 2023, 15, 3128. [Google Scholar] [CrossRef]
- Ratosa, I.; Jenko, A.; Sljivic, Z.; Pirnat, M.; Oblak, I. Breast Size and Dose to Cardiac Substructures in Adjuvant Three-Dimensional Conformal Radiotherapy Compared to Tangential Intensity Modulated Radiotherapy. Radiol. Oncol. 2020, 54, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Mazonakis, M.; Kachris, S.; Tolia, M.; Damilakis, J. NTCP Calculations of Five Different Irradiation Techniques for the Treatment of Thymoma. Curr. Oncol. 2023, 30, 7740–7752. [Google Scholar] [CrossRef] [PubMed]
- Matsali, E.; Pappas, E.P.; Lyraraki, E.; Lymperopoulou, G.; Mazonakis, M.; Karaiskos, P. Assessment of Radiation-Induced Bladder and Bowel Cancer Risks after Conventionally and Hypo-Fractionated Radiotherapy for the Preoperative Management of Rectal Carcinoma. J. Pers. Med. 2022, 12, 1442. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-H.; Cheng, J.-Y.; Huang, B.-S.; Luo, S.-D.; Lin, W.-C.; Chou, S.-Y.; Juang, P.-J.; Li, S.-H.; Huang, E.-Y.; Wang, Y.-M. Significant Reduction in Vertebral Artery Dose by Intensity Modulated Proton Therapy: A Pilot Study for Nasopharyngeal Carcinoma. J. Pers. Med. 2021, 11, 822. [Google Scholar] [CrossRef] [PubMed]
- Rezaeijo, S.M.; Hashemi, B.; Mofid, B.; Bakhshandeh, M.; Mahdavi, A.; Hashemi, M.S. The Feasibility of a Dose Painting Procedure to Treat Prostate Cancer Based on mpMR Images and Hierarchical Clustering. Radiat. Oncol. 2021, 16, 182. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Mei, X.; Chen, X.; Hu, W.; Hu, S.; Zhang, Y.; Shao, Z.; Guo, X.; Tuan, J.; Yu, X. Estimating Cardiac Substructures Exposure From Diverse Radiotherapy Techniques in Treating Left-Sided Breast Cancer. Medicine 2015, 94, e847. [Google Scholar] [CrossRef]
- Karpf, D.; Sakka, M.; Metzger, M.; Grabenbauer, G.G. Left Breast Irradiation with Tangential Intensity Modulated Radiotherapy (t-IMRT) versus Tangential Volumetric Modulated Arc Therapy (t-VMAT): Trade-Offs between Secondary Cancer Induction Risk and Optimal Target Coverage. Radiat. Oncol. 2019, 14, 156. [Google Scholar] [CrossRef]
- Nikovia, V.; Chinis, E.; Gkantaifi, A.; Marketou, M.; Mazonakis, M.; Charalampakis, N.; Mavroudis, D.; Orfanidou, K.V.; Varveris, A.; Antoniadis, C.; et al. Current Cardioprotective Strategies for the Prevention of Radiation-Induced Cardiotoxicity in Left-Sided Breast Cancer Patients. J. Pers. Med. 2023, 13, 1038. [Google Scholar] [CrossRef]

| Structure | Dosimetric Parameters |
|---|---|
| PTV | D95% |
| Heart | Dav |
| LAD | V40Gy |
| V30Gy | |
| Dav | |
| LV | V23Gy |
| V5Gy | |
| Dav |
| Structure | Parameter | Mean ± Standard Deviation | ||||
|---|---|---|---|---|---|---|
| 3D-CRT | 2F-IMRT | 7F-IMRT | VMAT1 | VMAT2 | ||
| CTV | D95% (%) | 96.56 ± 1.45 | 97.04 ± 1.73 | 99.12 ± 1.00 | 98.86 ± 1.30 | 99.00 ± 1.13 |
| PTV | D95% (%) | 92.11 ± 1.95 | 92.68 ± 1.62 | 96.04 ± 0.98 | 95.46 ± 1.09 | 96.45 ± 1.30 |
| Heart | V40Gy (%) | 1.88 ± 1.31 | 1.65 ± 1.34 | 0.67 ± 0.68 | 0.55 ± 0.56 | 0.52 ± 0.58 |
| V20Gy (%) | 4.65 ± 2.19 | 4.67 ± 2.37 | 3.38 ± 1.72 | 3.28 ± 1.94 | 3.17 ± 1.82 | |
| Dav (Gy) | 3.70 ± 0.98 | 6.43 ± 10.60 | 5.21 ± 1.04 | 5.15 ± 1.08 | 5.99 ± 9.54 | |
| Isp. lung | V20Gy (%) | 11.40 ± 4.76 | 11.22 ± 4.51 | 8.90 ± 3.26 | 9.65 ± 3.36 | 10.00 ± 3.47 |
| Structure | Parameter | Mean ± Standard Deviation | ||||
|---|---|---|---|---|---|---|
| 3D-CRT | 2F-IMRT | 7F-IMRT | VMAT1 | VMAT2 | ||
| LAD | V40Gy (%) | 12.91 ± 11.76 | 10.30 ± 10.74 | 4.98 ± 8.04 | 2.90 ± 5.91 | 3.10 ± 6.08 |
| V30Gy (%) | 18.51 ± 13.00 | 17.48 ± 13.73 | 12.84 ± 11.96 | 10.80 ± 10.84 | 10.88 ± 12.07 | |
| Dav (Gy) | 12.94 ± 5.33 | 14.73 ± 9.40 | 12.92 ± 5.51 | 12.02 ± 4.91 | 11.77 ± 5.05 | |
| LV | V23Gy (%) | 7.43 ± 4.18 | 7.26 ± 4.50 | 4.53 ± 3.27 | 4.47 ± 3.36 | 4.29 ± 3.40 |
| V5Gy (%) | 18.24 ± 6.26 | 28.77 ± 17.46 | 30.05 ± 14.38 | 29.99 ± 14.75 | 25.80 ± 14.05 | |
| Dav (Gy) | 5.69 ± 1.92 | 6.40 ± 1.75 | 5.93 ± 1.77 | 5.89 ± 1.80 | 5.37 ± 1.76 | |
| Techniques Comparison | p-Value | |||||
|---|---|---|---|---|---|---|
| LAD | LV | |||||
| V40Gy | V30Gy | Dav | V23Gy | V5Gy | Dav | |
| 3D-CRT vs. 2F-IMRT | 0.007 * | 0.101 | 0.316 | 0.546 | <0.001 * | 0.007 * |
| 3D-CRT vs. 7F-IMRT | <0.001 * | <0.001 * | 0.967 | <0.001 * | <0.001 * | 0.277 |
| 3D-CRT vs. VMAT1 | <0.001 * | <0.001 * | 0.125 | <0.001 * | <0.001 * | 0.412 |
| 3D-CRT vs. VMAT2 | <0.001 * | <0.001 * | 0.016 * | <0.001 * | 0.002 * | 0.110 |
| 2F-IMRT vs. 7F-IMRT | <0.001 * | <0.001 * | 0.484 | <0.001 * | 0.162 | 0.144 |
| 2F-IMRT vs. VMAT1 | <0.001 * | <0.001 * | 0.039 * | <0.001 * | 0.144 | 0.124 |
| 2F-IMRT vs. VMAT2 | <0.001 * | <0.001 * | 0.008 * | <0.001 * | 0.533 | 0.002 * |
| 7F-IMRT vs. VMAT1 | 0.039 * | 0.071 | 0.014 * | 0.436 | 0.966 | 0.809 |
| 7F-IMRT vs. VMAT2 | 0.019 * | 0.198 | 0.008 * | 0.263 | 0.104 | 0.002 * |
| VMAT1 vs. VMAT2 | 0.767 | 0.629 | 0.545 | 0.487 | 0.098 | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konstantinou, E.; Varveris, A.; Solomou, G.; Antoniadis, C.; Tolia, M.; Mazonakis, M. Radiation Dose to Critical Cardiac Structures from Three-Dimensional Conformal Radiation Therapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) Techniques for Left-Sided Breast Cancer. J. Pers. Med. 2024, 14, 63. https://doi.org/10.3390/jpm14010063
Konstantinou E, Varveris A, Solomou G, Antoniadis C, Tolia M, Mazonakis M. Radiation Dose to Critical Cardiac Structures from Three-Dimensional Conformal Radiation Therapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) Techniques for Left-Sided Breast Cancer. Journal of Personalized Medicine. 2024; 14(1):63. https://doi.org/10.3390/jpm14010063
Chicago/Turabian StyleKonstantinou, Evgenia, Antonis Varveris, Georgia Solomou, Chrysostomos Antoniadis, Maria Tolia, and Michalis Mazonakis. 2024. "Radiation Dose to Critical Cardiac Structures from Three-Dimensional Conformal Radiation Therapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) Techniques for Left-Sided Breast Cancer" Journal of Personalized Medicine 14, no. 1: 63. https://doi.org/10.3390/jpm14010063
APA StyleKonstantinou, E., Varveris, A., Solomou, G., Antoniadis, C., Tolia, M., & Mazonakis, M. (2024). Radiation Dose to Critical Cardiac Structures from Three-Dimensional Conformal Radiation Therapy (3D-CRT), Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) Techniques for Left-Sided Breast Cancer. Journal of Personalized Medicine, 14(1), 63. https://doi.org/10.3390/jpm14010063







