Accuracy of Positioning and Risk Factors for Malpositioning Custom-Made Femoral Stems in Total Hip Arthroplasty—A Retrospective Multicenter Analysis
Abstract
1. Introduction
2. Materials and Methods
- The center of the femoral head on the affected side.
- Both teardrops.
- Greater and lesser trochanter.
- A line tangent to the inferior border of both teardrops (inter-teardrop line).
- A line parallel to the inter-teardrop line passing through the center of the femoral head on the affected side.
- A line perpendicular to the inter-teardrop line crossing the deepest point of the teardrop (vertical teardrop line).
- A horizontal line connecting the ischial tuberosities.
- A horizontal line connecting the inferior borders of the lesser trochanter on both sides.
- The anatomical axis of the proximal femur.
- The longitudinal axis of the prosthetic neck.
- The longitudinal axis of the implanted stem.
- Horizontal femoral offset (HFO):
- The horizontal femoral offset is defined as the distance from the center of rotation of the femoral head to the anatomical axis of the proximal femur.
- Vertical femoral offset (VFO):
- The vertical femoral offset is defined as the distance from the center of rotation of the femoral head to the lower margin of the lesser trochanter.
- Horizontal center of rotation (HCOR):
- The horizontal center of rotation is defined as the distance from the center of rotation of the femoral head to the vertical teardrop line.
- Vertical center of rotation (VCOR):
- The vertical center of rotation is defined as the distance from the center of rotation of the femoral head to the inter-teardrop line.
- Projected neck-to-shaft angle (CCD):
- The projected neck-to-shaft angle is defined as the projected angle between the anatomical axis of the femur and the axis of the femoral neck.
- Leg length discrepancy (LLD):
- The leg length discrepancy is defined as the difference in the distance between the inferior margin of the lesser trochanter and the inter-teardrop line.
- Stem version:
- The stem version was calculated by the formula presented by Weber et al. [11]:
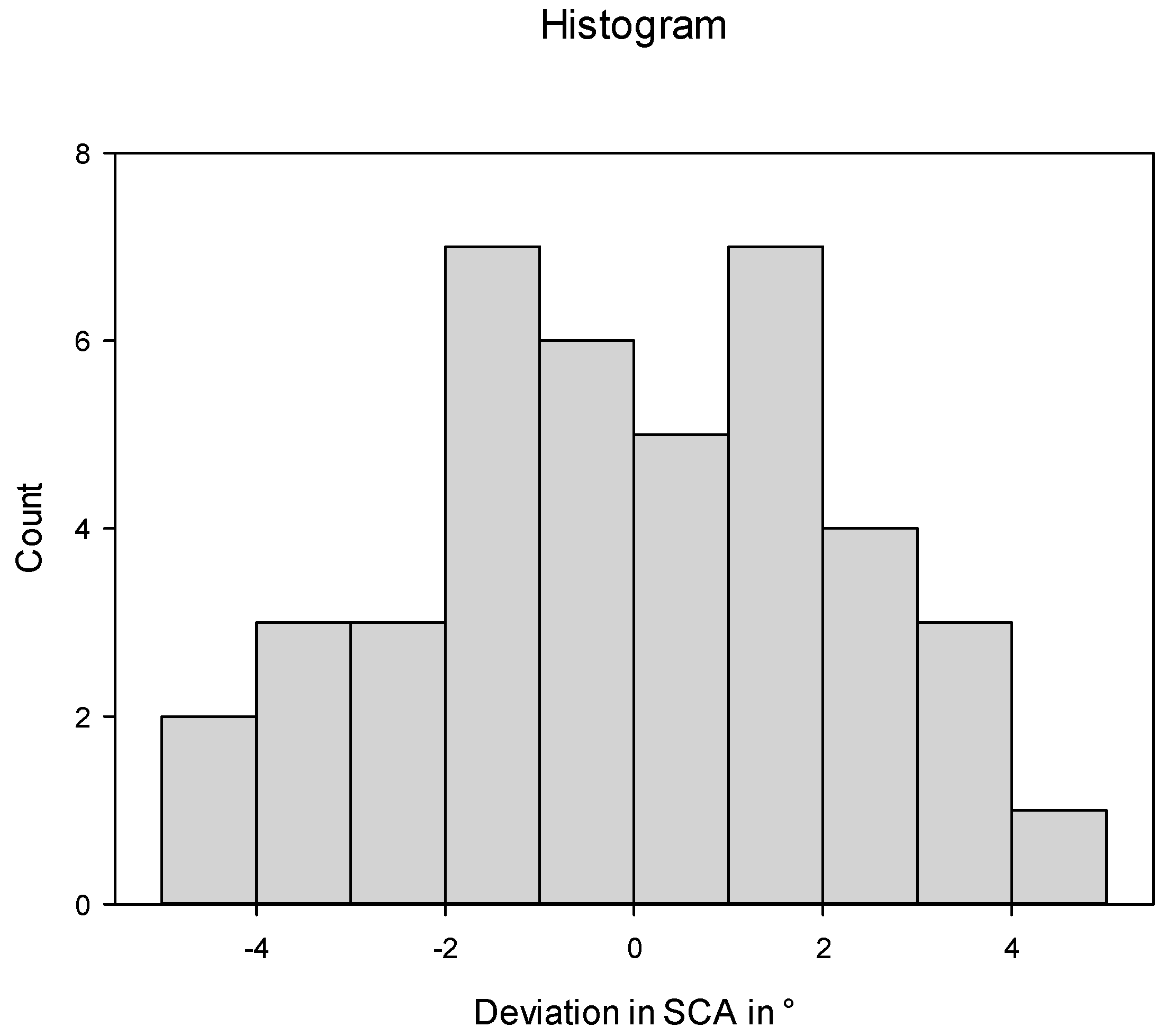
- Stem coronal angle:
- The stem coronal angle is defined as the angle between the longitudinal axis of the implanted stem and the anatomical axis of the proximal femur.
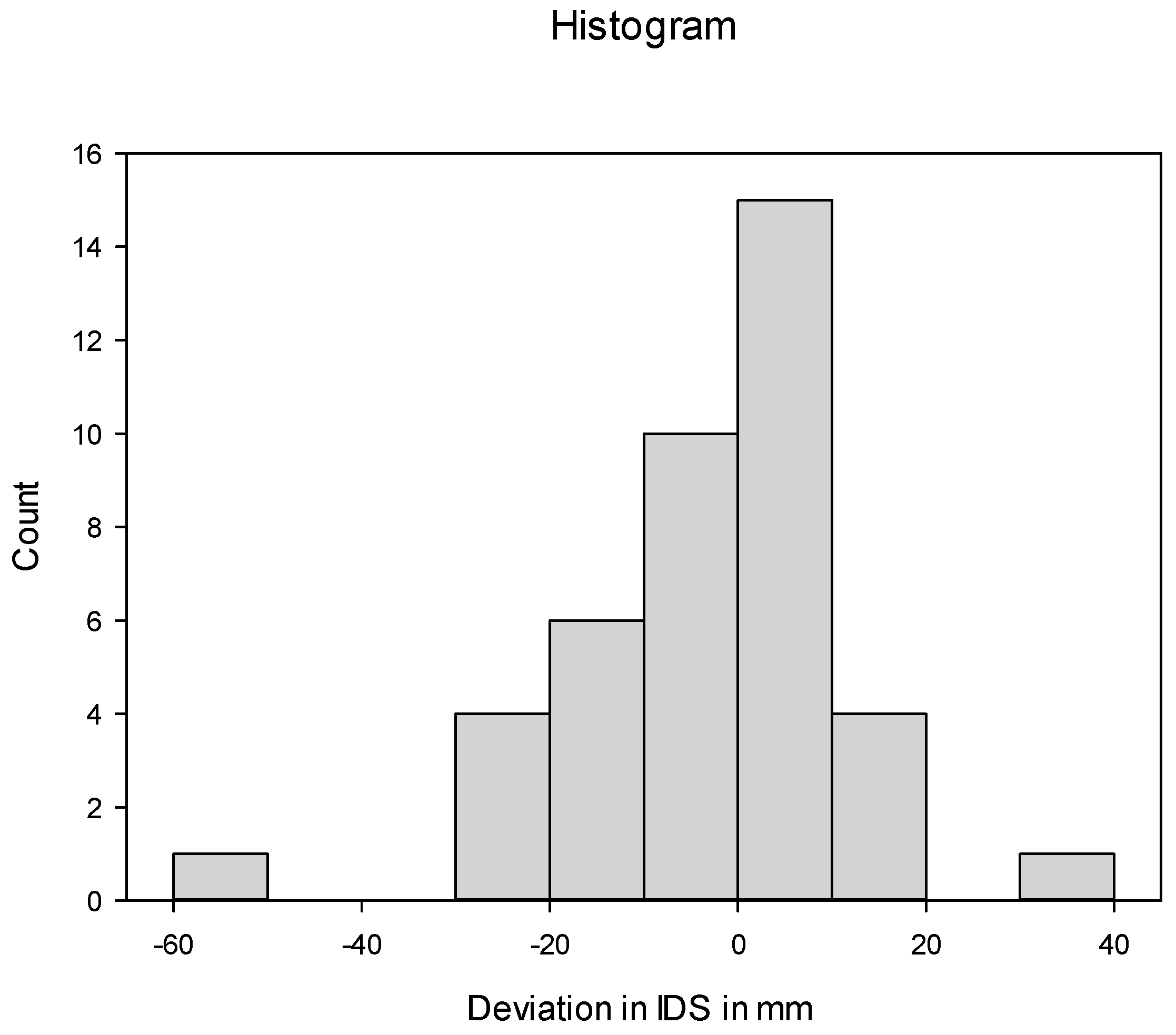
- Implantation depth of the stem:
- The implantation depth of the stem is defined as the distance from the lower margin of the lesser trochanter to the shoulder of the stem.
- Planned stem version;
- Planned stem coronal angle;
- Planned implantation depth of the stem.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.M.; Vollmann, P.; Weißenberger, M.; Rudert, M. Total hip arthroplasty in geriatric patients—A single-center experience. SICOT-J 2022, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- D’Antonio, J.; McCarthy, J.C.; Bargar, W.L.; Borden, L.S.; Cappelo, W.N.; Collis, D.K.; Steinberg, M.E.; Wedge, J.H. Classification of femoral abnormalities in total hip arthroplasty. Clin. Orthop. Relat. Res. 1993, 296, 133–139. [Google Scholar] [CrossRef]
- Mortazavi, S.M.J.; Restrepo, C.; Kim, P.J.W.; Parvizi, J.; Hozack, W.J. Cementless femoral reconstruction in patients with proximal femoral deformity. J. Arthroplast. 2011, 26, 354–359. [Google Scholar] [CrossRef]
- McCarthy, J.C.; Bono, J.V.; O’Donnell, P.J. Custom and modular components in primary total hip replacement. Clin. Orthop. Relat. Res. (1976–2007) 1997, 344, 162–171. [Google Scholar] [CrossRef]
- Berry, D.J. Utility of modular implants in primary total hip arthroplasty. J. Arthroplast. 2014, 29, 657–658. [Google Scholar] [CrossRef] [PubMed]
- Lakstein, D.; Eliaz, N.; Levi, O.; Backstein, D.; Kosashvili, Y.; Safir, O.; Gross, A.E. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. JBJS 2011, 93, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Tsiampas, D.T.; Pakos, E.E.; Georgiadis, G.C.; Xenakis, T.A. Custom-made femoral implants in total hip arthroplasty due to congenital disease of the hip: A review. HIP Int. 2016, 26, 209–214. [Google Scholar] [CrossRef]
- Yanik-Karaca, Z. Erfassung der ctx-individualschaftposition mit ebra-fca: Abgleich präoperativer planung mit postoperativem prothesensitz bei künstlichem hüftgelenksersatz. Ph.D. Thesis, Frankfurt University of Applied Sciences, Frankfurt, Germany, 2008. [Google Scholar]
- Bishi, H.; Smith, J.B.V.; Asopa, V.; Field, R.E.; Wang, C.; Sochart, D.H. Comparison of the accuracy of 2d and 3d templating methods for planning primary total hip replacement: A systematic review and meta-analysis. EFORT Open Rev. 2022, 7, 70–83. [Google Scholar] [CrossRef]
- Dorr, L.D.; Faugere, M.-C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.S.; Dramis, A.; Board, T.N. Leg length discrepancy after total hip arthroplasty: A review of literature. Curr. Rev. Musculoskelet. Med. 2013, 6, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Ranawat, C.S.; Rodriguez, J. Functional leg-length inequality following total hip arthroplasty. J. Arthroplast. 1997, 12, 359–364. [Google Scholar] [CrossRef] [PubMed]
- White, T.O.; Dougall, T.W. Arthroplasty of the hip. J. Bone Jt. Surg. Br. Vol. 2002, 84, 335–338. [Google Scholar] [CrossRef]
- Othman, B.; Chandra, R.; Nestel, D. Age of the leftie: The lived experience of left-handed surgeons. ANZ J. Surg. 2022, 92, 2082–2087. [Google Scholar] [CrossRef]
- Papadatou-Pastou, M.; Ntolka, E.; Schmitz, J.; Martin, M.; Munafò, M.R.; Ocklenburg, S.; Paracchini, S. Human handedness: A meta-analysis. Psychol. Bull. 2020, 146, 481. [Google Scholar] [CrossRef]
- Pennington, N.; Redmond, A.; Stewart, T.; Stone, M. The impact of surgeon handedness in total hip replacement. Ann. R. Coll. Surg. Engl. 2014, 96, 437–441. [Google Scholar] [CrossRef]
- Mehta, S.; Lotke, P.A. Impact of surgeon handedness and laterality on outcomes of total knee arthroplasties: Should right-handed surgeons do only right tkas? Am. J. Orthop.-Belle Mead 2007, 36, 530. [Google Scholar]
- Moloney, D.; Bishay, M.; Ivory, J.; Pozo, J. Failure of the sliding hip screw in the treatment of femoral neck fractures: ‘Left-handed surgeons for left-sided hips’. Injury 1994, 25, SB9–SB13. [Google Scholar] [CrossRef]
- Spaans, A.J.; Hout, J.A.A.M.v.d.; Bolder, S.B.T. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012, 83, 342–346. [Google Scholar] [CrossRef]
- Martin, R.; Clayson, P.E.; Troussel, S.; Fraser, B.P.; Docquier, P.-L. Anterolateral minimally invasive total hip arthroplasty: A prospective randomized controlled study with a follow-up of 1 year. J. Arthroplast. 2011, 26, 1362–1372. [Google Scholar] [CrossRef]
- den Hartog, Y.M.; Mathijssen, N.M.C.; Vehmeijer, S.B.W. The less invasive anterior approach for total hip arthroplasty: A comparison to other approaches and an evaluation of the learning curve—A systematic review. HIP Int. 2016, 26, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Innmann, M.M.; Streit, M.R.; Kolb, J.; Heiland, J.; Parsch, D.; Aldinger, P.R.; Königshausen, M.; Gotterbarm, T.; Merle, C. Influence of surgical approach on component positioning in primary total hip arthroplasty. BMC Musculoskelet. Disord. 2015, 16, 180. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, P.B.; Thompson, M.T.; Esposito, C.I.; Poli, N.; McGree, J.; Donnelly, T.; Donnelly, W. The impact of functional combined anteversion on hip range of motion: A new optimal zone to reduce risk of impingement in total hip arthroplasty. Bone Jt. Open 2021, 2, 834–841. [Google Scholar] [CrossRef]
- Krebs, V.E.; Hameed, D.; Mont, M.A. The evolving influence of spino-pelvic biomechanics and research on hip arthroplasty. J. Arthroplast. 2023, 38, 611–613. [Google Scholar] [CrossRef]
- Dorr, L.D.; Callaghan, J.J. Death of the lewinnek “safe zone”. J. Arthroplast. 2019, 34, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Haversath, M.; Busch, A.; Jäger, M.; Tassemeier, T.; Brandenburger, D.; Serong, S. The ‘critical trochanter angle’: A predictor for stem alignment in total hip arthroplasty. J. Orthop. Surg. Res. 2019, 14, 165. [Google Scholar] [CrossRef] [PubMed]
- Free, M.D.; Barnes, I.; Hutchinson, M.; Harvie, P. Preoperative radiographs to predict component malposition in direct anterior approach total hip arthroplasty. HIP Int. 2023, 33, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Worlicek, M.; Weber, M.; Craiovan, B.; Wörner, M.; Völlner, F.; Springorum, H.R.; Grifka, J.; Renkawitz, T. Native femoral anteversion should not be used as reference in cementless total hip arthroplasty with a straight, tapered stem: A retrospective clinical study. BMC Musculoskelet. Disord. 2016, 17, 399. [Google Scholar] [CrossRef][Green Version]
- Emerson, R.H. Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin. Orthop. Relat. Res. 2012, 470, 477–481. [Google Scholar] [CrossRef]
- Marcovigi, A.; Ciampalini, L.; Perazzini, P.; Caldora, P.; Grandi, G.; Catani, F. Evaluation of native femoral neck version and final stem version variability in patients with osteoarthritis undergoing robotically implanted total hip arthroplasty. J. Arthroplast. 2019, 34, 108–115. [Google Scholar] [CrossRef]
- Belzunce, M.A.; Henckel, J.; Di Laura, A.; Hart, A. Uncemented femoral stem orientation and position in total hip arthroplasty: A ct study. J. Orthop. Res. 2020, 38, 1486–1496. [Google Scholar] [CrossRef] [PubMed]
- Rittmeister, M.; Eisenbeis, K.; Hanusek, S.; Yanik-Karaca, Z.; Starker, M.; Arabmotlagh, M. Bewertung der implantatposition von 107 individuellen ctx-hüftendoprothesenschäften mit ebra-fca. Z. Orthop. Ihre Grenzgeb. 2004, 142, 659–665. [Google Scholar] [CrossRef]
- Jacquet, C.; Flecher, X.; Pioger, C.; Fabre-Aubrespy, M.; Ollivier, M.; Argenson, J.N. Long-term results of custom-made femoral stems. Orthopade 2020, 49, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Pakos, E.E.; Stafilas, K.S.; Tsovilis, A.E.; Vafiadis, J.N.; Kalos, N.K.; Xenakis, T.A. Long term outcomes of total hip arthroplasty with custom made femoral implants in patients with congenital disease of hip. J. Arthroplast. 2015, 30, 2242–2247. [Google Scholar] [CrossRef]
- Liu, Z.; Gao, Y.; Cai, L. Imageless navigation versus traditional method in total hip arthroplasty: A meta-analysis. Int. J. Surg. 2015, 21, 122–127. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, R.; Gong, S.; Han, L.; Gong, T.; Yi, Y.; Feng, Y.; Wang, G.; Xu, W. A comparison of radiological and clinical outcomes between robotic-assisted and conventional total hip arthroplasty: A meta-analysis. Int. J. Med. Robot. Comput. Assist. Surg. 2023, 19, e2463. [Google Scholar] [CrossRef]
- Domb, B.G.; El Bitar, Y.F.; Sadik, A.Y.; Stake, C.E.; Botser, I.B. Comparison of robotic-assisted and conventional acetabular cup placement in tha: A matched-pair controlled study. Clin. Orthop. Relat. Res. 2014, 472, 329–336. [Google Scholar] [CrossRef]
- Koper, M.C.; Reijman, M.; van Es, E.M.; Waarsing, J.H.; Koot, H.W.J.; Keizer, S.B.; Jansen, I.; van Biezen, F.C.; Verhaar, J.A.N.; Bos, P.K. No added value for computer-assisted surgery to improve femoral component positioning and patient reported outcomes in hip resurfacing arthroplasty; a multi-center randomized controlled trial. BMC Musculoskelet. Disord. 2019, 20, 473. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Lechler, P.; Kunow, F.v.; Völlner, F.; Keshmiri, A.; Hapfelmeier, A.; Grifka, J.; Renkawitz, T. The validity of a novel radiological method for measuring femoral stem version on anteroposterior radiographs of the hip after total hip arthroplasty. Bone Jt. J. 2015, 97, 306–311. [Google Scholar] [CrossRef] [PubMed]



| Measured Parameters | Mean | ±SD |
|---|---|---|
| HFO (mm) | 26.4 | ±13.2 |
| VFO (mm) | 68.4 | ±19.9 |
| HCOR (mm) | 32.7 | ±11.0 |
| VCOR (mm) | 24.6 | ±9.3 |
| CCD (°) | 136 | ±22.4 |
| LLD (mm) | 9.4 | ±18.4 |
| Kellgren and Lawrence Score | n | (%) |
| 0 | 5 | (12.2) |
| 1 | 2 | (4.9) |
| 2 | 15 | (36.6) |
| 3 | 8 | (19.5) |
| 4 | 11 | (26.8) |
| Dorr Classification Type | n | (%) |
| A | 15 | (36.6) |
| B | 18 | (43.9) |
| C | 8 | (19.5) |
| Minimally Invasive Anterior and Antero-Lateral Approach (n = 25) | Lateral Approach (n = 16) | p | |||
|---|---|---|---|---|---|
| Stem version deviation in ° (mean ± SD) | 18.0 | ±17.9 | 11.4 | ±10.9 | 0.198 |
| Stem implantation depth deviation in mm (mean ±SD) | −5.3 | ±17.8 | −3.1 | ±10.8 | 0.657 |
| Stem coronal angle deviation in ° (mean ± SD) | 0.1 | ±2.2 | −0.4 | ±2.4 | 0.516 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, P.M.; Heinz, T.; Rak, D.; Arnholdt, J.; Holzapfel, B.M.; Dorsch, S.; Weißenberger, M.; von Eisenhart-Rothe, R.; Jaenisch, M.; Ertl, M.; et al. Accuracy of Positioning and Risk Factors for Malpositioning Custom-Made Femoral Stems in Total Hip Arthroplasty—A Retrospective Multicenter Analysis. J. Pers. Med. 2023, 13, 1285. https://doi.org/10.3390/jpm13091285
Anderson PM, Heinz T, Rak D, Arnholdt J, Holzapfel BM, Dorsch S, Weißenberger M, von Eisenhart-Rothe R, Jaenisch M, Ertl M, et al. Accuracy of Positioning and Risk Factors for Malpositioning Custom-Made Femoral Stems in Total Hip Arthroplasty—A Retrospective Multicenter Analysis. Journal of Personalized Medicine. 2023; 13(9):1285. https://doi.org/10.3390/jpm13091285
Chicago/Turabian StyleAnderson, Philip Mark, Tizian Heinz, Dominik Rak, Jörg Arnholdt, Boris Michael Holzapfel, Silke Dorsch, Manuel Weißenberger, Rüdiger von Eisenhart-Rothe, Max Jaenisch, Max Ertl, and et al. 2023. "Accuracy of Positioning and Risk Factors for Malpositioning Custom-Made Femoral Stems in Total Hip Arthroplasty—A Retrospective Multicenter Analysis" Journal of Personalized Medicine 13, no. 9: 1285. https://doi.org/10.3390/jpm13091285
APA StyleAnderson, P. M., Heinz, T., Rak, D., Arnholdt, J., Holzapfel, B. M., Dorsch, S., Weißenberger, M., von Eisenhart-Rothe, R., Jaenisch, M., Ertl, M., Wagner, M., Windhagen, H., Rudert, M., & Jakuscheit, A. (2023). Accuracy of Positioning and Risk Factors for Malpositioning Custom-Made Femoral Stems in Total Hip Arthroplasty—A Retrospective Multicenter Analysis. Journal of Personalized Medicine, 13(9), 1285. https://doi.org/10.3390/jpm13091285









