Usefulness of Preoperative Determination of Serum MR-ProAdrenomedullin Levels to Predict the Need for Postoperative Organ Support in Abdominal Oncological Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurement of MR-ProADM
2.3. Study Variables
2.4. Statistic Analysis
3. Results
3.1. Descriptive Data
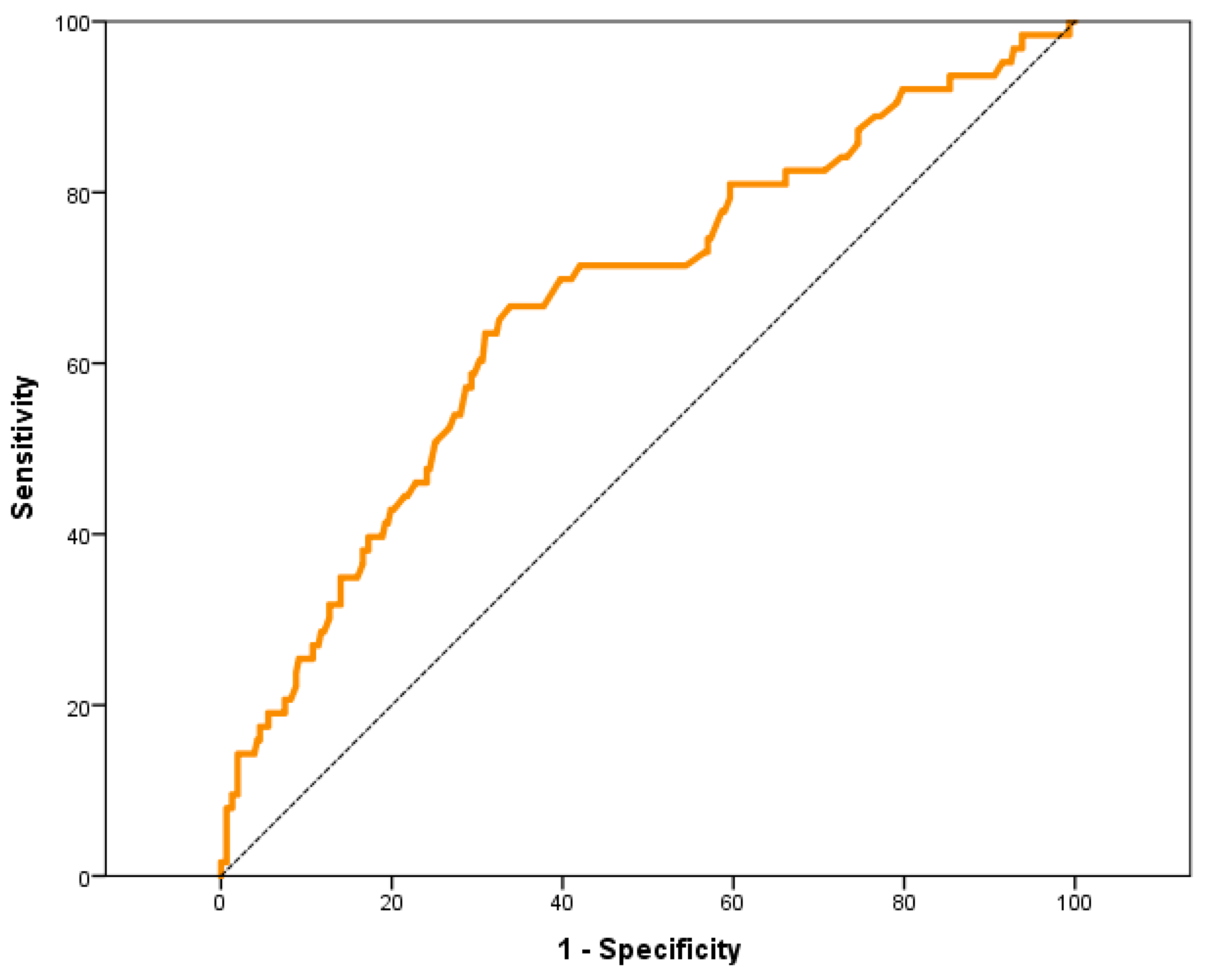
3.2. Outcome Data (Primary Outcome)
3.3. Outcome Data (Secondary Outcome)
4. Discussion
- ○
- A preoperative value of 0.87 nmol/L in the pilot study of our group to predict the need for POS [35];
- ○
- A preoperative value of 0.85 nmol/L in the study by Golubović et al. to predict postoperative mortality in abdominal surgery [36];
- ○
- A preoperative value of 0.77 ± 0.37 nmol/L in the study of Egyed et al. [37];
- ○
- A preoperative value of 1.3 nmol/L in the study referring to the prognostic capacity of mortality after TAVI [38];
- ○
- A postoperative value of 3.2 nmol/L in the study for the prediction of mortality in the postoperative period of cardiac surgery [39].
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pearse, R.M.; Moreno, R.P.; Bauer, P.; Pelosi, P.; Metnitz, P.; Spies, C.; Vallet, B.; Vincent, J.-L.; Hoeft, A.; Rhodes, A. Mortality after surgery in Europe: A 7 day cohort study. Lancet 2012, 380, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Bartels, K.; Karhausen, J.; Clambey, E.T.; Grenz, A.; Eltzschig, H.K. Perioperative organ injury. Anesthesiology 2013, 119, 1474–1489. [Google Scholar] [CrossRef] [PubMed]
- Dale, C.D.; McLoone, P.; Sloan, B.; Kinsella, J.; Morrison, D.; Puxty, K.; Quasim, T. Critical care provision after colorectal cancer surgery. BMC Anesthesiol. 2016, 16, 94. [Google Scholar] [CrossRef] [PubMed]
- Halvorsen, S.; Mehilli, J.; Cassese, S.; Hall, T.S.; Abdelhamid, M.; Barbato, E.; Zacharowski, K. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur. Heart J. 2022, 43, 3826–3924. [Google Scholar] [CrossRef]
- Planas, A.; Ramasco, F. Search for biomarkers to identify surgical patients at high cardiovascular and perioperative mortality risk. Rev. Esp. De Anestesiol. Y Reanim. 2017, 64, 547–549. [Google Scholar] [CrossRef]
- Jankovic, R.J.; Dinic, V.; Markovic, D. Pre and postoperative risk management: The role of scores and biomarkers. Curr. Opin. Anaesthesiol. 2020, 33, 475–480. [Google Scholar] [CrossRef]
- Jankovic, R.J.; Markovic, D.Z.; Sokolovic, D.T.; Zdravkovic, I.; Sorbello, M. Clinical indices and biomarkers for perioperative cardiac risk stratification: An update. Minerva Anestesiol. 2017, 83, 392–401. [Google Scholar] [CrossRef]
- Duceppe, E.; Parlow, J.; MacDonald, P.; Lyons, K.; McMullen, M.; Srinathan, S.; Graham, M.; Tandon, V.; Styles, K.; Bessissow, A.; et al. Canadian Cardiovascular Society Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Noncardiac Surgery. Can. J. Cardiol. 2017, 33, 17–32. [Google Scholar] [CrossRef]
- Álvarez Zurro, C.; Planas Roca, A.; Alday Muñoz, E.; Vega Piris, L.; Ramasco Rueda, F.; Méndez Hernández, R. High levels of preoperative and postoperative N terminal B-type natriuretic propeptide influence mortality and cardiovascular complications after noncardiac surgery. Eur. J. Anaesthesiol. 2016, 33, 444–449. [Google Scholar] [CrossRef]
- Kitamura, K.; Kangawa, K.; Eto, T. Adrenomedullin and PAMP: Discovery, structures, and cardiovascular functions. Microsc. Res. Tech. 2002, 57, 3–13. [Google Scholar] [CrossRef]
- Funke-Kaiser, A.; Havulinna, A.S.; Zeller, T.; Appelbaum, S.; Jousilahti, P.; Vartiainen, E.; Salomaa, V. Predictive value of midregional pro-adrenomedullin compared to natriuretic peptides for incident cardiovascular disease and heart failure in the population-based FINRISK 1997 cohort. Ann. Med. 2014, 46, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Eggers, K.M.; Venge, P.; Lindahl, B.; Lind, L. Associations of mid-regional pro-adrenomedullin levels to cardiovascular and metabolic abnormalities, and mortality in an elderly population from the community. Int. J. Cardiol. 2013, 168, 3537–3542. [Google Scholar] [CrossRef] [PubMed]
- Curbelo, J.; Bueno, S.L.; Galván-Román, J.M.; Ortega-Gómez, M.; Rajas, O.; Fernández-Jiménez, G.; Aspa, J. Inflammation biomarkers in blood as mortality predictors in community-acquired pneumonia admitted patients: Importance of comparison with neutrophil count percentage or neutrophil-lymphocyte ratio. PLoS ONE 2017, 12, e0173947. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela-Sánchez, F.; Valenzuela-Méndez, B.; Rodríguez-Gutiérrez, J.F.; Estella-García, Á.; González-García, M.Á. New role of biomarkers: Mid-regional pro-adrenomedullin, the biomarker of organ failure. Ann. Transl. Med. 2016, 4, 329. [Google Scholar] [CrossRef]
- Kristensen, S.D.; Knuuti, J.; Saraste, A.; Anker, S.; Bøtker, H.E.; De Hert, S.; Archbold, A. 2014 ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: Cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesth. Eur. Heart J. 2014, 35, 2383–2431. [Google Scholar]
- Morgenthaler, N.G.; Struck, J.; Alonso, C.; Bergmann, A. Measurement of midregional proadrenomedullin in plasma with an immunoluminometric assay. Clin. Chem. 2005, 51, 1823–1829. [Google Scholar] [CrossRef]
- Davis, C.; Tait, G.; Carroll, J.; Wijeysundera, D.N.; Beattie, W.S. The Revised Cardiac Risk Index in the new millennium: A single-centre prospective cohort re-evaluation of the original variables in 9519 consecutive elective surgical patients. Can. J. Anesth. 2013, 60, 855–863. [Google Scholar] [CrossRef]
- Copeland, G.P.; Jones, D.; Walters, M. POSSUM: A scoring system for surgical audit. Br. J. Surg. 1991, 78, 355–360. [Google Scholar] [CrossRef]
- Gawande, A.A.; Kwaan, M.R.; Regenbogen, S.E.; Lipsitz, S.A.; Zinner, M.J. An Apgar Score for Surgery. J. Am. Coll. Surg. 2007, 204, 201–208. [Google Scholar] [CrossRef]
- Krintus, M.; Kozinski, M.; Braga, F.; Kubica, J.; Sypniewska, G.; Panteghini, M. Plasma midregional proadrenomedullin (MR-proADM) concentrations and their biological determinants in a reference population. Clin. Chem. Lab. Med. 2018, 56, 1161–1168. [Google Scholar] [CrossRef]
- Holm, J.; Cederholm, I.; Alehagen, U.; Lindahl, T.L.; Szabó, Z. Biomarker dynamics in cardiac surgery: A prospective observational study on MR-proADM, MR-proANP, hs-CRP and sP-selectin plasma levels in the perioperative period. Biomarkers 2020, 25, 296–304. [Google Scholar] [CrossRef]
- Nishikimi, T.; Nakagawa, Y. Adrenomedullin as a Biomarker of Heart Failure. Heart Fail. Clin. 2018, 14, 49–55. [Google Scholar] [CrossRef]
- Pavo, N.; Raderer, M.; Hülsmann, M.; Neuhold, S.; Adlbrecht, C.; Strunk, G.; Goliasch, G.; Gisslinger, H.; Steger, G.G.; Hejna, M.; et al. Cardiovascular biomarkers in patients with cancer and their association with all-cause mortality. Heart 2015, 101, 1874–1880. [Google Scholar] [CrossRef] [PubMed]
- Al Shuaibi, M.; Bahu, R.R.; Chaftari, A.-M.; Al Wohoush, I.; Shomali, W.; Jiang, Y.; Debiane, L.; Raad, S.; Jabbour, J.; Al Akhrass, F.; et al. Pro-adrenomedullin as a novel biomarker for predicting infections and response to antimicrobials in febrile patients with hematologic malignancies. Clin. Infect. Dis. 2013, 56, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Lobo, S.M.; Rezende, E.; Knibel, M.F.; Silva, N.B.; Páramo, J.A.; Nácul, F.E.; Mendes, C.L.; Assunção, M.; Costa, R.C.; Grion, C.C.; et al. Early determinants of death due to multiple organ failure after noncardiac surgery in high-risk patients. Anesth. Analg. 2011, 112, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Christ-Crain, M.; Morgenthaler, N.G.; Struck, J.; Harbarth, S.; Bergmann, A.; Müller, B. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: An observational study. Crit. Care 2005, 9, 816–824. [Google Scholar] [CrossRef]
- Valenzuela-Sánchez, F.; Valenzuela-Méndez, B.; de Bohollo Austria, R.; Rodríguez-Gutiérrez, J.F.; Estella-García, Á.; Fernández-Ruiz, L.; González-García, M.; Rello, J. Plasma levels of mid-regional pro-adrenomedullin in sepsis are associated with risk of death. Minerva Anestesiol. 2019, 85, 366–375. [Google Scholar] [CrossRef]
- Suberviola, B.; Castellanos-Ortega, A.; Ruiz Ruiz, A.; Lopez-Hoyos, M.; Santibañez, M. Hospital mortality prognostication in sepsis using the new biomarkers suPAR and proADM in a single determination on ICU admission. Intensive Care Med. 2013, 39, 1945–1952. [Google Scholar] [CrossRef]
- Li, Q.; Wang, B.S.; Yang, L.; Peng, C.; Ma, L.B.; Chai, C. Assessment of adrenomedullin and proadrenomedullin as predictors of mortality in septic patients: A systematic review and meta-analysis. Med. Intensiv. 2018, 42, 416–424. [Google Scholar] [CrossRef]
- Rodseth, R.N.; Biccard, B.M.; Le Manach, Y.; Sessler, D.I.; Lurati Buse, G.A.; Thabane, L.; Devereaux, P.J. The prognostic value of pre-operative and post-operative B-type natriuretic peptides in patients undergoing noncardiac surgery: B-type natriuretic peptide and N-terminal fragment of pro-B-type natriuretic peptide: A systematic review and individual patien. J. Am. Coll. Cardiol. 2014, 63, 170–180. [Google Scholar] [CrossRef]
- Andrés, C.; Andaluz-Ojeda, D.; Cicuendez, R.; Nogales, L.; Martín, S.; Martin-Fernandez, M.; Bermejo-Martin, J.F. MR- proADM to detect specific types of organ failure in infection. Eur. J. Clin. Investig. 2020, 50, e13246. [Google Scholar] [CrossRef]
- Bernal-Morell, E.; García-Villalba, E.; Vera, M.D.C.; Medina, B.; Martinez, M.; Callejo, V.; Valero, S.; Cinesi, C.; Piñera, P.; Alcaraz, A.; et al. Usefulness of midregional pro-adrenomedullin as a marker of organ damage and predictor of mortality in patients with sepsis. J. Infect. 2018, 76, 249–257. [Google Scholar] [CrossRef]
- Andaluz-Ojeda, D.; Nguyen, H.B.; Meunier-Beillard, N.; Cicuéndez, R.; Quenot, J.-P.; Calvo, D.; Dargent, A.; Zarca, E.; Andrés, C.; Nogales, L.; et al. Superior accuracy of mid-regional proadrenomedullin for mortality prediction in sepsis with varying levels of illness severity. Ann. Intensive Care 2017, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Vigué, B.; Leblanc, P.-E.; Moati, F.; Pussard, E.; Foufa, H.; Rodrigues, A.; Figueiredo, S.; Harrois, A.; Mazoit, J.-X.; Rafi, H.; et al. Mid-regional pro-adrenomedullin (MR-proADM), a marker of positive fluid balance in critically ill patients: Results of the ENVOL study. Crit. Care 2016, 20, 363. [Google Scholar] [CrossRef] [PubMed]
- Ramasco Rueda, F.; Planas Roca, A.; Figuerola Tejerina, A.; Méndez Hernández, R.; Gilsanz Rodriguez, F. Pre-Operative pro-adrenomedullin as a predictor of postoperative requirement of organ support in patients scheduled for major abdominal surgery. A prospective observational pilot study. Rev. Esp. Anestesiol. Reanim. 2020, 67, 8–14. [Google Scholar] [CrossRef]
- Golubović, M.; Janković, R.; Sokolović, D.; Cosić, V.; Maravić-Stojkovic, V.; Kostić, T.; Lađević, N. Preoperative Midregional Pro-Adrenomedullin and High-Sensitivity Troponin T Predict Perioperative Cardiovascular Events in Noncardiac Surgery. Med. Princ. Pract. 2018, 27, 278–284. [Google Scholar] [CrossRef]
- Egyed, E.; Defosse, J.; Schröder, S.; Rosenzweig, S.; Hering, R.; Brockt, S.; Sakka, S.G. Mid-regional proadrenomedullin (MR-proADM) in the assessment of postoperative risk for complications-a pilot study. Biomark. Gene 2017, 1, 1–8. [Google Scholar]
- Csordas, A.; Nietlispach, F.; Schuetz, P.; Huber, A.; Müller, B.; Maisano, F.; Lüscher, T.F. Midregional proadrenomedullin improves risk stratification beyond surgical risk scores in patients undergoing transcatheter aortic valve replacement. PLoS ONE 2015, 10, e0143761. [Google Scholar] [CrossRef] [PubMed]
- Schoe, A.; Schippers, E.F.; Struck, J.; Ebmeyer, S.; Klautz, R.J.M.; De Jonge, E.; van Dissel, J.T. Postoperative pro-adrenomedullin levels predict mortality in thoracic surgery patients: Comparison with acute physiology and chronic health evaluation IV score. Crit. Care Med. 2015, 43, 373–381. [Google Scholar] [CrossRef] [PubMed]
- García de Guadiana-Romualdo, L.; Martínez Martínez, M.; Rodríguez Mulero, M.D.; Esteban-Torrella, P.; Hernández Olivo, M.; Alcaraz García, M.J.; Bernal-Morell, E. Circulating MR-proADM levels, as an indicator of endothelial dysfunction, for early risk stratification of mid-term mortality in COVID-19 patients. Int. J. Infect. Dis. 2021, 111, 211–218. [Google Scholar] [CrossRef]
- Haag, E.; Gregoriano, C.; Molitor, A.; Kloter, M.; Kutz, A.; Mueller, B.; Schuetz, P. Does mid-regional pro-adrenomedullin (MR-proADM) improve the sequential organ failure assessment-score (SOFA score) for mortality-prediction in patients with acute infections? Results of a prospective observational study. Clin. Chem. Lab. Med. 2021, 59, 1165–1176. [Google Scholar] [CrossRef] [PubMed]
- Bellia, C.; Agnello, L.; Sasso, B.L.; Bivona, G.; Raineri, M.S.; Giarratano, A.; Ciaccio, M. Mid-regional pro-adrenomedullin predicts poor outcome in non-selected patients admitted to an intensive care unit. Clin. Chem. Lab. Med. 2019, 57, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Elke, G.; the SepNet Critical Care Trials Group; Bloos, F.; Wilson, D.C.; Brunkhorst, F.M.; Briegel, J.; Reinhart, K.; Loeffler, M.; Kluge, S.; Nierhaus, A.; et al. The use of mid-regional proadrenomedullin to identify disease severity and treatment response to sepsis—A secondary analysis of a large randomised controlled trial. Crit. Care 2018, 22, 79. [Google Scholar] [CrossRef]
- Nierhaus, A.; Bloos, F.; Wilson, D.C.; Elke, G.; Meybohm, P. Predicting the requirement for renal replacement therapy in intensive care patients with sepsis. Crit. Care 2018, 22, 201. [Google Scholar] [CrossRef] [PubMed]
| Surgery Group | Frequency (n) | Average Duration (Minutes) |
|---|---|---|
| Colorectal | 227 | 211.4 ± 78 |
| Pancreatohepatobiliary | 69 | 313.0 ± 139 |
| Esophagogastroduodenal | 29 | 261.7 ± 134 |
| Cystectomy | 30 | 267.4 ± 80 |
| Open Nephrectomy | 15 | 154.1 ± 44 |
| Postoperative Organic Support | Frequency (n) | Percentage (%) |
|---|---|---|
| Vasoconstrictors only | 31 | 8.4% |
| Mechanical ventilation only | 10 | 2.7% |
| Renal replacement therapy only | 0 | 0% |
| Vasoconstrictors + Mechanical ventilation | 16 | 4.3% |
| Vasoconstrictors + Renal replacement therapy | 1 | 0.3% |
| Mechanical ventilation + Renal replacement therapy | 1 | 0.3% |
| Vasoconstrictors + Mechanical ventilation + Renal replacement therapy | 4 | 1.1% |
| Diagnostic Characteristics of MR-ProADM ≥ 0.70 nmol/L | Statistical Value | IC 95% | |
|---|---|---|---|
| Lower Limit | Upper Limit | ||
| Sensitivity | 69.84% | 56.82% | 80.43% |
| Specificity | 59.93% | 54.20% | 65.42% |
| Positive Predictive Value | 26.35% | 19.98% | 33.82% |
| Negative Predictive Value | 90.64% | 85.56% | 94.12% |
| Positive Likelihood Ratio | 1.74 | 1.41 | 2.16 |
| Negative Likelihood Ratio | 0.50 | 0.34 | 0.74 |
| Probability of Correct Diagnosis | 62% | 56.4% | 66.56% |
| OR | IC 95% | p | |
|---|---|---|---|
| Age ≥ 65 years | 1.7 | 1.00–2.76 | <0.05 |
| Sex | 0.6 | 0.38–1.09 | ns |
| Type of surgery | 5.5 | 2.20–5.65 | <0.05 |
| ASA ≥ 3 | 1.5 | 0.94–2.31 | ns |
| RCRI ≥ 2 | 1.5 | 0.92–2.41 | ns |
| POSSUM ≥ 28 | 4.3 | 2.40–7.87 | <0.05 |
| SAS ≤ 4 | 3.9 | 2.56–5.95 | <0.05 |
| MR-ProADM ≥ 0.70 nmol/L | 2.8 | 1.71–4.63 | <0.05 |
| OR | IC 95% | p | |
|---|---|---|---|
| Age ≥ 65 years | 1.0 | 0.49–2.07 | ns |
| Sex | 0.7 | 0.35–1.40 | ns |
| Type of surgery | 1.2 | 0.98–1.58 | ns |
| ASA ≥ 3 | 0.8 | 0.41–1.65 | ns |
| RCRI ≥ 2 | 0.9 | 0.42–1.84 | ns |
| POSSUM ≥ 28 | 4.4 | 2.09–9.16 | <0.05 |
| SAS ≤ 4 | 5.3 | 2.30–12.4 | <0.05 |
| MR-ProADM ≥ 0.70 nmol/L | 2.6 | 1.33–5.09 | <0.05 |
| OR | IC 95% | p | |
|---|---|---|---|
| Age ≥ 65 years | 1.7 | 1.42–1.96 | <0.05 |
| Sex | 0.9 | 0.71–1.15 | ns |
| Type of surgery | 1.0 | 0.79–1.27 | ns |
| ASA ≥ 3 | 1.9 | 1.48–2.34 | <0.05 |
| RCRI ≥ 2 | 1.8 | 1.46–2.20 | <0.05 |
| POSSUM ≥ 28 | 1.9 | 1.50–2.45 | <0.05 |
| SAS ≤ 4 | 1.3 | 0.92–1.77 | ns |
| OR | IC 95% | p | |
|---|---|---|---|
| Age ≥ 65 years | 3.0 | 1.85–4.99 | <0.05 |
| Sex | 1.2 | 0.71–1.93 | ns |
| Type of surgery | 1.2 | 0.95–1.42 | ns |
| ASA ≥ 3 | 1.9 | 1.11–3.09 | <0.05 |
| RCRI ≥ 2 | 1.6 | 0.88–2.98 | ns |
| POSSUM ≥ 28 | 2.0 | 1.26–3.30 | <0.05 |
| SAS ≤ 4 | 1.3 | 0.59–2.96 | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramasco Rueda, F.; Planas Roca, A.; Méndez Hernández, R.; Figuerola Tejerina, A.; Tamayo Gómez, E.; Garcia Bernedo, C.; Maseda Garrido, E.; Pascual Gómez, N.F.; de la Varga-Martínez, O. Usefulness of Preoperative Determination of Serum MR-ProAdrenomedullin Levels to Predict the Need for Postoperative Organ Support in Abdominal Oncological Surgery. J. Pers. Med. 2023, 13, 1151. https://doi.org/10.3390/jpm13071151
Ramasco Rueda F, Planas Roca A, Méndez Hernández R, Figuerola Tejerina A, Tamayo Gómez E, Garcia Bernedo C, Maseda Garrido E, Pascual Gómez NF, de la Varga-Martínez O. Usefulness of Preoperative Determination of Serum MR-ProAdrenomedullin Levels to Predict the Need for Postoperative Organ Support in Abdominal Oncological Surgery. Journal of Personalized Medicine. 2023; 13(7):1151. https://doi.org/10.3390/jpm13071151
Chicago/Turabian StyleRamasco Rueda, Fernando, Antonio Planas Roca, Rosa Méndez Hernández, Angels Figuerola Tejerina, Eduardo Tamayo Gómez, Carlos Garcia Bernedo, Emilio Maseda Garrido, Natalia F. Pascual Gómez, and Olga de la Varga-Martínez. 2023. "Usefulness of Preoperative Determination of Serum MR-ProAdrenomedullin Levels to Predict the Need for Postoperative Organ Support in Abdominal Oncological Surgery" Journal of Personalized Medicine 13, no. 7: 1151. https://doi.org/10.3390/jpm13071151
APA StyleRamasco Rueda, F., Planas Roca, A., Méndez Hernández, R., Figuerola Tejerina, A., Tamayo Gómez, E., Garcia Bernedo, C., Maseda Garrido, E., Pascual Gómez, N. F., & de la Varga-Martínez, O. (2023). Usefulness of Preoperative Determination of Serum MR-ProAdrenomedullin Levels to Predict the Need for Postoperative Organ Support in Abdominal Oncological Surgery. Journal of Personalized Medicine, 13(7), 1151. https://doi.org/10.3390/jpm13071151








