Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review
Abstract
1. Introduction
2. Materials and Methods
3. Discussion
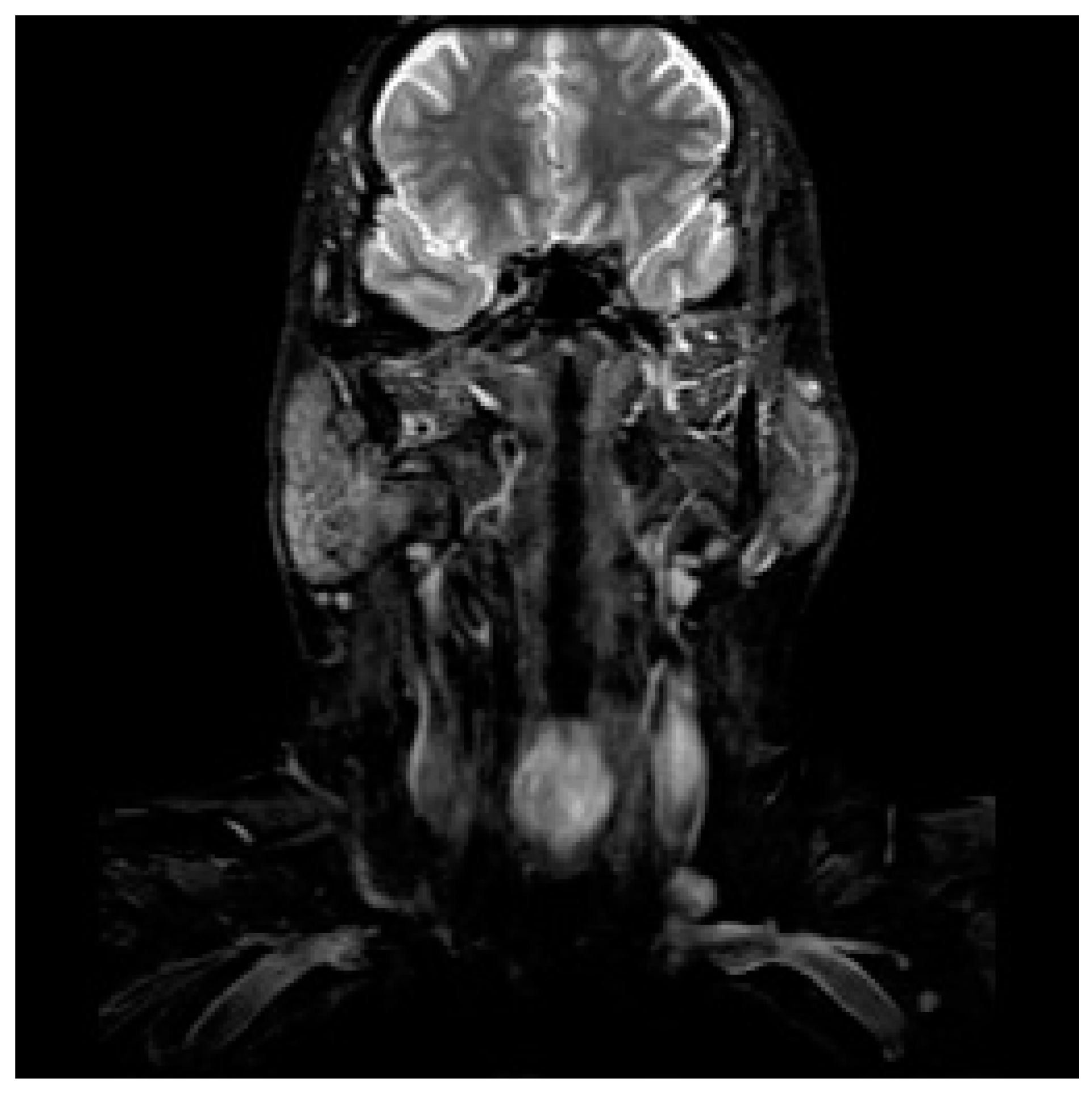
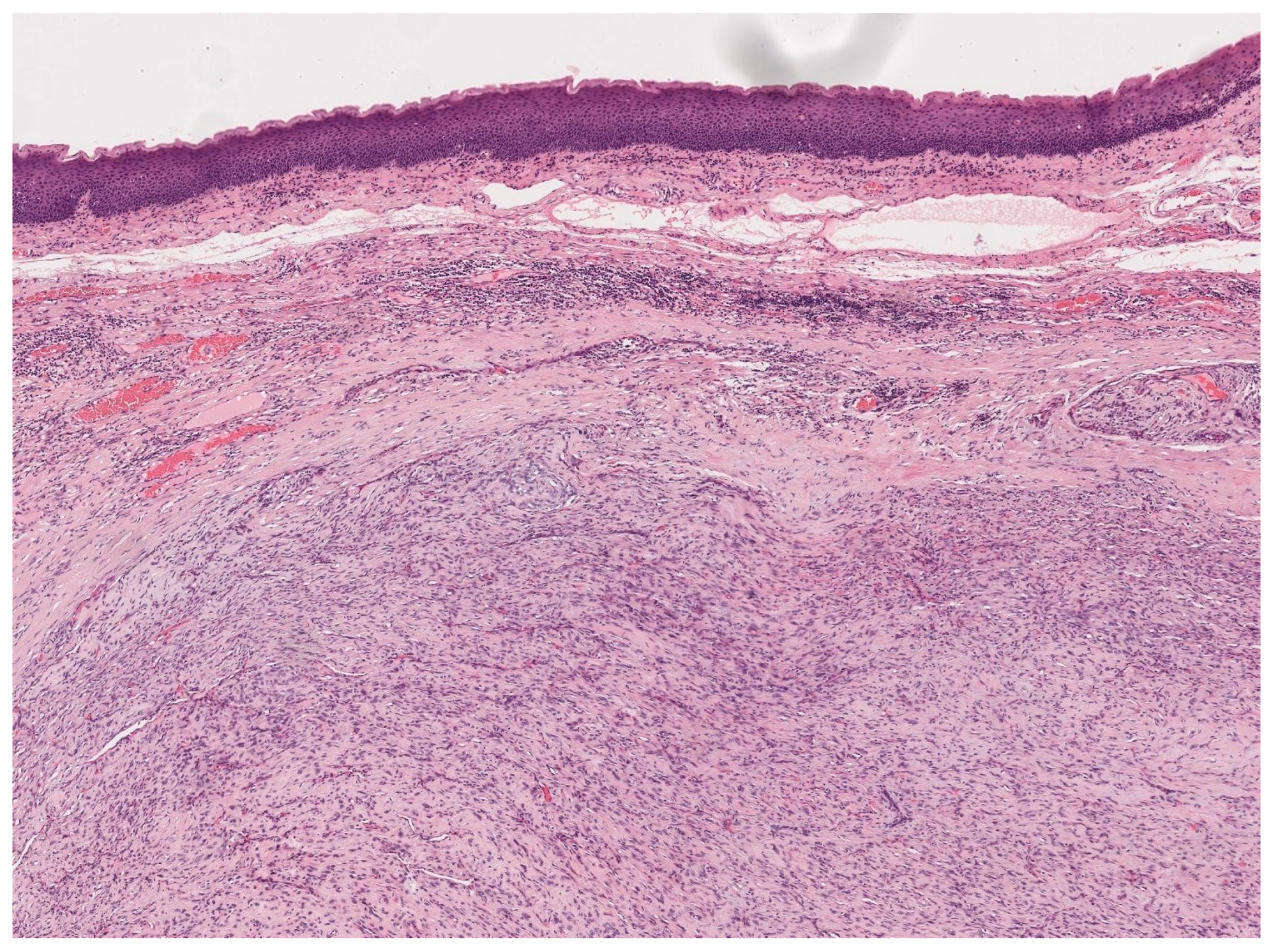
3.1. Diagnostic Workup
3.2. Neuroendocrine Tumors
3.3. Spindle-Cell Carcinoma
3.4. Minor Salivary Gland Tumors
3.5. Soft Tissue Sarcomas
3.6. Bone/Cartilage Sarcomas
3.7. Lymphoepithelial Carcinoma
3.8. Malignant Melanoma
3.9. Primary Lymphoma of the Larynx
3.10. Perspectives in Non-Squamous Cell Carcinomas
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koroulakis, A.; Agarwal, M. Laryngeal Cancer. In StatPearls [Internet]; [Updated 10 August 2020]; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK526076/ (accessed on 12 December 2022).
- American Cancer Society. Cancer Facts & Figures 2017; American Cancer Society: Atlanta, GA, USA, 2017; Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-andfigures/2017/cancer-facts-and-figures-2017.pdf (accessed on 13 December 2020).
- American Cancer Society. Cancer Facts & Figures 2018; American Cancer Society: Atlanta, GA, USA, 2018; Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statis-tics/annual-cancer-factsandfigures/2018/cancer-facts-and-figures-2018.pdf (accessed on 13 December 2020).
- Shah, J.P.; Karnell, L.H.; Hoffman, H.T.; Ariyan, S.; Brown, G.S.; Fee, W.E.; Glass, A.G.; Goepfert, H.; Ossoff, R.H.; Fremgen, A. Patterns of care for cancer of the larynx in the United States. Arch. Otolaryngol. Head Neck Surg. 1997, 123, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.; Mody, M.D.; Saba, N.F. Systemic therapy in non-conventional cancers of the larynx. Oral Oncol. 2018, 82, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Marioni, G.; Marchese-Ragona, R.; Cartei, G.; Marchese, F.; Staffieri, A. Current opinion in diagnosis and treatment of laryngeal carcinoma. Cancer Treat. Rev. 2006, 32, 504–515. [Google Scholar] [CrossRef]
- Hoffman, H.T.; Porter, K.; Karnell, L.H.; Cooper, J.S.; Weber, R.S.; Langer, C.J.; Ang, K.-K.; Gay, G.; Stewart, A.; Robinson, R.A.; et al. Laryngeal Cancer in the United States: Changes in Demographics, Patterns of Care, and Survival. Laryngoscope 2006, 116, 1–13. [Google Scholar] [CrossRef]
- Karatzanis, A.D.; Psychogios, G.; Waldfahrer, F.; Kapsreiter, M.; Zenk, J.; Velegrakis, G.A.; Iro, H. Management of locally advanced laryngeal cancer. J. Otolaryngol.-Head Neck Surg. 2014, 43, 4. [Google Scholar] [CrossRef]
- Cheraghlou, S.; Kuo, P.; Judson, B.L. Treatment delay and facility case volume are associated with survival in early-stage glottic cancer. Laryngoscope 2017, 127, 616–622. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Head and Neck Cancers (Version 2.2018). Available online: http://oncolife.com.ua/doc/nccn/Head_and_Neck_Cancers.pdf (accessed on 10 December 2020).
- Moher, D.; Liberati, M.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Torabi, S.J.; Cheraghlou, S.; Kasle, D.A.; Savoca, E.L.; Judson, B.L. Nonsquamous cell laryngeal cancers: Incidence, demographics, care patterns, and effect of surgery. Laryngoscope 2019, 129, 2496–2505. [Google Scholar] [CrossRef]
- Lin, H.W.; Bhattacharyya, N. Staging and Survival Analysis for Nonsquamous Cell Carcinomas of the Larynx. Laryngoscope 2008, 118, 1003–1013. [Google Scholar] [CrossRef]
- Ferlito, A.; Barnes, L.; Rinaldo, A.; Gnepp, D.R.; Milroy, C.M. A review of neuroendocrine neoplasms of the larynx: Update on diagnosis and treatment. J. Laryngol. Otol. 1998, 112, 827–834. [Google Scholar] [CrossRef]
- Ferlito, A.; Silver, C.E.; Bradford, C.R.; Rinaldo, A. Neuroendocrine neoplasms of the larynx: An overview. Head Neck 2009, 31, 1634–1646. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Zhao, R.; Chen, X.; Liu, Y.; Tian, L.; Liu, M. Establishment of a non-squamous cell carcinoma of the larynx nomogram prognostic model and prognosis analysis. Auris Nasus Larynx 2022, 49, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Iandelli, A.; Missale, F.; Laborai, A.; Filauro, M.; Marchi, F.; Del Bon, F.; Perotti, P.; Parrinello, G.; Piazza, C.; Peretti, G. Surgical management and oncological outcome of non squamous cell carcinoma of the larynx: A bicentric study. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 299–310. [Google Scholar] [CrossRef]
- Rotsides, J.M.; Patel, E.; Oliver, J.R.; Moses, L.E.; Jacobson, A.S.; Hu, K.S.; Vaezi, A.; Tam, M.; Givi, B. Non-Squamous Cell Malignancies of the Larynx. Laryngoscope 2022, 132, 1771–1777. [Google Scholar] [CrossRef] [PubMed]
- Doğan, S.; Vural, A.; Kahriman, G.; İmamoğlu, H.; Abdülrezzak, U.; Öztürk, M. Non-squamous cell carcinoma diseases of the larynx: Clinical and imaging findings. Braz. J. Otorhinolaryngol. 2020, 86, 468–482. [Google Scholar] [CrossRef]
- Banko, B.; Đukić, V.; Milovanovic, J.; Kovač, J.; Artiko, V.; Maksimović, R. Diagnostic significance of magnetic resonance imaging in preoperative evaluation of patients with laryngeal tumors. Eur. Arch. Oto-Rhino-Laryngol. 2011, 268, 1617–1623. [Google Scholar] [CrossRef]
- Torabi, S.; Benchetrit, L.; Spock, T.; Judson, B. Clinically node-negative head and neck mucosal melanoma: An analysis of current treatment guidelines & outcomes. Oral Oncol. 2019, 92, 67–76. [Google Scholar] [CrossRef]
- Strojan, P.; Hernandez-Prera, J.C.; Beitler, J.J.; Eisbruch, A.; Saba, N.F.; Mendenhall, W.M.; Nieto, C.S.; Smee, R.; Rinaldo, A.; Ferlito, A. Small cell and large cell neuroendocrine carcinoma of the larynx: A comparative analysis. Cancer Treat. Rev. 2019, 78, 42–51. [Google Scholar] [CrossRef]
- Oren, N.; Vaysberg, A.; Ginat, D.T. Updated WHO nomenclature of head and neck lesions and associated imaging findings. Insights Imaging 2019, 10, 72. [Google Scholar] [CrossRef]
- Ferlito, A.; Rinaldo, A. Primary and secondary small cell neuroendocrine carcinoma of the larynx: A review. Head Neck 2008, 30, 518–524. [Google Scholar] [CrossRef]
- Moisa, I.; Silver, C. Treatment of Neuroendocrine Neoplasms of the Larynx. ORL 1991, 53, 259–264. [Google Scholar] [CrossRef]
- Bapat, U.; MacKinnon, N.A.; Spencer, M.G. Carcinoid tumours of the larynx. Eur. Arch. Oto-Rhino-Laryngol. 2005, 262, 194–197. [Google Scholar] [CrossRef]
- Ferlito, A.; Devaney, K.O.; Rinaldo, A. Neuroendocrine neoplasms of the larynx: Advances in identification, understanding, and management. Oral Oncol. 2006, 42, 770–788. [Google Scholar] [CrossRef]
- Goldman, N.C.; Katibah, G.M.; Medina, J. Carcinoid tumors of the larynx. ORL 1985, 64, 130–134. [Google Scholar]
- Gnepp, D. Small Cell Neuroendocrine Carcinoma of the Larynx. A critical review of the literature. ORL 1991, 53, 210–219. [Google Scholar] [CrossRef]
- Baugh, R.F.; Wolf, G.T.; Krause, C.J.; Beals, T.F.; Forastiere, A. Small Cell Carcinoma of the Larynx: Results of Therapy. Laryngoscope 1986, 96, 1283–1290. [Google Scholar] [CrossRef]
- Pointer, K.B.; Ko, H.C.; Brower, J.V.; Witek, M.E.; Kimple, R.J.; Lloyd, R.V.; Harari, P.M.; Baschnagel, A.M. Small cell carcinoma of the head and neck: An analysis of the National Cancer Database. Oral Oncol. 2017, 69, 92–98. [Google Scholar] [CrossRef]
- Barnes, L. Neuroendocrine tumours. In Pathology and Genetics Head and Neck Tumours. World Health Organization Classification of Tumours; Barnes, L., Eveson, J.W., Reichart, P., Sidransky, D., Eds.; IARC Press: Lyon, France, 2005; pp. 135–139. [Google Scholar]
- Grignon, D.J.; Ro, J.Y.; Ayala, A.G.; Chong, C. Carcinoma of prostate metastasizingto vocal cord. Urology 1990, 36, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Danikas, D.; Theodorou, S.J.; Matthews, W.E.; Rienzo, A.A. Unusually Aggressive Rectal Carcinoid Metastasizing to Larynx, Pancreas, Adrenal Glands, and Brain. Am. Surg. 2000, 66, 1179–1180. [Google Scholar] [CrossRef]
- López, F.; Williams, M.D.; Cardesa, A.; Hunt, J.L.; Strojan, P.; Rinaldo, A.; Nixon, I.J.; Rodrigo, J.P.; Saba, N.F.; Mendenhall, W.M.; et al. How phenotype guides management of non-conventional squamous cell carcinomas of the larynx? Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 2709–2726. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Purgina, B.; Seethala, R.R. Spindle Cell Carcinoma of the Larynx with Rhabdomyoblastic Heterologous Element: A Rare Form of Divergent Differentiation. Head Neck Pathol. 2013, 7, 263–267. [Google Scholar] [CrossRef]
- Thompson, L.D.; Wieneke, J.A.; Miettinen, M.; Heffner, D.K. Spindle cell (sarcomatoid) carcinomas of the larynx: A clinicopathologic study of 187 cases. Am. J. Surg. Pathol. 2002, 26, 153–170. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.M.; Choudhry, H.S.; Desai, A.D.; Shah, V.P.; Patel, P.; Eloy, J.A.; Roden, D.F.; Fang, C.H. Prognostic significance of head and neck spindle cell carcinoma. Head Neck 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Deng, W.; Li, C.; Lau, H.; Tao, L.; Wang, S.; Zhou, L.; Zhang, M. Clinical outcome and comparison between squamous and non-squamous cell carcinoma of the larynx. Acta Otolaryngol. 2020, 140, 195–201. [Google Scholar] [CrossRef]
- López, F.; Williams, M.D.; Skálová, A.; Hellquist, H.; Suárez, C.; Nixon, I.J.; Rodrigo, J.P.; Cardesa, A.; Strojan, P.; Quer, M.; et al. How Phenotype Guides Management of the Most Common Malignant Salivary Neoplasms of the Larynx? Adv. Ther. 2017, 34, 813–825. [Google Scholar] [CrossRef]
- Ereno, C.; I Lopez, J.; Bilbao, F.J. The biphasic pattern of laryngeal and hypopharyngeal adenosquamous carcinoma is retained in lymph node metastases. Histopathology 2005, 46, 715–716. [Google Scholar] [CrossRef] [PubMed]
- Keelawat, S.; Liu, C.Z.; Roehm, P.C.; Barnes, L. Adenosquamous carcinoma of the upper aerodigestive tract: A clinicopathologic study of 12 cases and review of the literature. Am. J. Otolaryngol. 2002, 23, 160–168. [Google Scholar] [CrossRef]
- Cumberworth, V.L.; Narula, A.; MacLennan, K.A.; Bradley, P.J. Mucoepidermoid carcinoma of the larynx. J. Laryngol. Otol. 1989, 103, 420–423. [Google Scholar] [CrossRef]
- Nance, M.A.; Seethala, R.R.; Wang, Y.; Chiosea, S.I.; Myers, E.N.; Johnson, J.T.; Lai, S.Y. Treatment and survival outcomes based on histologic grading in patients with head and neck mucoepidermoid. Cancer 2008, 113, 2082–2089. [Google Scholar] [CrossRef]
- Trosman, S.; Chute, D.; Wood, B.; Lamarre, E. Unknown primary mucoepidermoid carcinoma: Diagnosis and treatment. Head Neck 2015, 37, E22–E25. [Google Scholar] [CrossRef]
- Gomes, V.; Costarelli, L.; Cimino, G.; Magaldi, L.; Bisceglia, M. Mucoepidermoid carcinoma of the larynx. Eur. Arch. Otorhinolaryngol. 1990, 248, 31–34. [Google Scholar] [CrossRef]
- Ferlito, A.; Recher, G.; Bottin, R. Mucoepidermoid Carcinoma of the Larynx. A clinicopathological study of 11 cases with review of the literature. ORL 1981, 43, 280–299. [Google Scholar] [CrossRef]
- Alavi, S.; Calcaterra, T.C.; Namazie, A.; Blackwell, K.E. Glandular Carcinoma of the Larynx: The Ucla Experience. Ann. Otol. Rhinol. Laryngol. 1999, 108, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Luna-Ortiz, K.; Cano-Valdez, A.M.; Chacón, A.P.; Gómez, A.H. Horizontal partial laryngectomy in mucoepidermoid carcinoma of the larynx after failure of laser surgery followed by radiotherapy: A case report. Cases J. 2009, 2, 8421. [Google Scholar] [CrossRef]
- Ferlito, A.; Rinaldo, A.; Devaney, K.O.; Carbone, A. Management of the clinically negative cervical lymph nodes in patients with non-conventional squamous carcinoma of the larynx. J. Laryngol. Arch Otorhinolaryngol. 1999, 113, 619–623. [Google Scholar] [CrossRef]
- Walvekar, R.R.; Filho, P.A.A.; Seethala, R.R.; Gooding, W.E.; Heron, D.E.; Johnson, J.T.; Ferris, R.L. Clinicopathologic features as stronger prognostic factors than histology or grade in risk stratification of primary parotid malignancies. Head Neck 2011, 33, 225–231. [Google Scholar] [CrossRef]
- Rapidis, A.D.; Givalos, N.; Gakiopoulou, H.; Stavrianos, S.D.; Faratzis, G.; Lagogiannis, G.A.; Katsilieris, I.; Patsouris, E. Mucoepidermoid carcinoma of the salivary glands.: Review of the literature and clinicopathological analysis of 18 patients. Oral Oncol. 2007, 43, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Pires, F.R.; de Almeida, O.P.; de Araújo, V.C.; Kowalski, L.P. Prognostic Factors in Head and Neck Mucoepidermoid Carcinoma. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Karatayli-Ozgursoy, S.; Bishop, J.; Hillel, A.; Akst, L.; Best, S. Non-epithelial tumors of the larynx: A single institution review. Am. J. Otolaryngol. 2016, 37, 279–285. [Google Scholar] [CrossRef]
- Fernández-Aceñero, M.J.; Larach, F.; Ortega-Fernández, C. Non-epithelial lesions of the larynx: Review of the 10-year experience in a tertiary Spanish hospital. Acta Oto-Laryngol. 2009, 129, 108–112. [Google Scholar] [CrossRef]
- Friedman, A.D.; A Burns, J.; Lutch, M.J.; Zeitels, S.M. Submucosal neoplasms of the laryngeal introitus. J. Laryngol. Otol. 2012, 126, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Wenig, B.M.; Weiss, S.W.; Gnepp, D.R. Laryngeal and Hypopharyngeal Liposarcoma a Clinicopathologic Study of 10 Cases with a Comparison to Soft-Tissue Counterparts. Am. J. Surg. Pathol. 1990, 14, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Makeieff, M.; Pelliccia, P.; Poizat, F.; Arnaud, S.; Rat, F.; Cupissol, D.; Guerrier, B.; Costes, V. Laryngeal dedifferentiated liposarcoma. Eur. Arch. Otorhinolaryngol. 2010, 267, 991–994. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Sun, J.; Wei, S.; Wang, D.; Brandwein, M. Well-Differentiated Laryngeal/Hypopharyngeal Liposarcoma in the MDM2 Era Report of Three Cases and Literature Review. Head Neck Pathol. 2017, 11, 146–151. [Google Scholar] [CrossRef]
- Tamaki, A.; Wasman, J.; Weidenbecher, M. Laryngeal alveolar soft part sarcoma: A case report of a rare malignancy in an atypical location. Am. J. Otolaryngol. 2017, 38, 260–262. [Google Scholar] [CrossRef]
- Cowan, M.L.; Thompson, L.; Leon, M.E.; Bishop, J.A. Low-Grade Fibromyxoid Sarcoma of the Head and Neck: A Clinicopathologic Series and Review of the Literature. Head Neck Pathol. 2016, 10, 161–166. [Google Scholar] [CrossRef]
- Dikbas, O.; Altundag, K.; Abali, H.; Turker, A.; Engin, H.; Sungur, A.; Baltali, E. Embryonal Rhabdomyosarcoma of the Larynx. Otolaryngol. Head Neck Surg. 2005, 133, 160–162. [Google Scholar] [CrossRef]
- Jain, A.; Singh, S.N.; Singhal, P.; Sharma, M.P. A rare case of subglottic embryonal rhabdomyosarcoma: Managed with the aim of organ preservation. J. Laryngol. Otol. 2015, 129, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Kukwa, W.; Wojtowicz, P.; Jagielska, B.; Sobczyk, G.; Kukwa, A.; Czarnecka, A.M. Laryngeal embryonal rhabdomyosarcoma in an adult—A case presentation in the eyes of geneticists and clinicians. BMC Cancer 2011, 11, 166. [Google Scholar] [CrossRef]
- Russell, J.O.; Revenaugh, P.C.; Budd, G.T.; Greskovich, J.; Scharpf, J. Failed organ preservation strategy for adult laryngeal embryonal rhabdomyosarcoma. Am. J. Otolaryngol. 2015, 36, 277–279. [Google Scholar] [CrossRef]
- Sivanandan, R.; Kong, C.S.; Kaplan, M.J.; Fee, W.E.; Thu-Le, Q.; Goffinet, D.R. Laryngeal Embryonal Rhabdomyosarcoma: A case of cervical metastases 13 years after treatment and a 25-year review of existing literature. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 1217–1222. [Google Scholar] [CrossRef]
- Pantanowitz, L.; Dezube, B.J. Kaposi sarcoma in unusual locations. BMC Cancer 2008, 8, 190. [Google Scholar] [CrossRef] [PubMed]
- Jeong, C.Y.; Kim, C.S. Undifferentiated pleomorphic sarcoma of the vocal fold. Ear Nose Throat J. 2016, 95, E12–E14. [Google Scholar] [PubMed]
- Kim, J.P.; Kim, J.Y.; Ko, G.H.; Woo, S.H. A rare case of malignant fibrous histiocytoma (pleomorphic undifferentiated sarcoma NOS) of the vocal fold. Ear Nose Throat J. 2015, 94, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Cambruzzi, E.; Cruz, R.P.; Gava, V.G.; Pêgas, K.L. Undifferentiated high-grade pleomorphic sarcoma of the larynx treated with partial laringectomy. Braz. J. Otorhinolaryngol. 2016, 86, 14–16. [Google Scholar] [CrossRef]
- Shein, G.; Sandhu, G.; Potter, A.; Loo, C.; Jacobson, I.; Anazodo, A. Laryngeal Synovial Sarcoma: A Systematic Review of the Last 40 Years of Reported Cases. Ear Nose Throat J. 2021, 100, NP93–NP104. [Google Scholar] [CrossRef]
- Gatti, W.M.; Strom, C.G.; Orfei, E. Synovial sarcoma of laryngopharynx. Arch. Otolaryngol. Head Neck Surg. 1975, 101, 633–636. [Google Scholar] [CrossRef]
- Miller, L.H.; Santaella Latimer, L.; Miller, T. Synovial sarcoma of the larynx. Trans. Sect. Ophthalmol. Am. Acad. Ophthalmol. Otolaryngol. 1975, 80, 448–451. [Google Scholar]
- Mochloulis, G.; Irving, R.M.; Grant, H.R.; Miller, R.F. Laryngeal Kaposi’s sarcoma in patients with AIDS. J. Laryngol. Otol. 1996, 110, 1034–1037. [Google Scholar] [CrossRef]
- Ablanedo-Terrazas, Y.; La Barrera, C.A.-D.; Ormsby, C.E.; Ruiz-Cruz, M.; Reyes-Terán, G. Intralesional bevacizumab in patients with Human immunodeficiency virus-associated Kaposi’s sarcoma in the upper airway. Laryngoscope 2015, 125, E132–E137. [Google Scholar] [CrossRef]
- Thompson, L.D.R.; Gannon, F.H. Chondrosarcoma of the Larynx: A clinicopathologic study of 111 cases with a review of the literature. Am. J. Surg. Pathol. 2002, 26, 836–851. [Google Scholar] [CrossRef]
- Tiwari, R.; Mahieu, H.; Snow, G. Long-term results of organ preservation in chondrosarcoma of the cricoid. Eur. Arch. Oto-Rhino-Laryngol. 1999, 256, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Mosalleum, E.; Afrogheh, A.; Stofberg, S.; Bezuidenhout, A.F.; Schneider, J.; Hille, J. A Review of Primary Osteosarcoma of the Larynx and Case Report. Head Neck Pathol. 2015, 9, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, F.M.; Godoy, L.M.R.; Daboin, K.P.; Casiraghi, O.; Garcia, A.M.; Luna, M.A. Laryngeal osteosarcoma: A clinicopathologic analysis of four cases and comparison with a carcinosarcoma. Ann. Diagn. Pathol. 2002, 6, 1–9. [Google Scholar] [CrossRef]
- Mäkitie, A.A.; Devaney, K.O.; Baujat, B.; Almangush, A.; Ferlito, A. Characteristics of Laryngeal Osteosarcoma: A Critical Review. Oncol. Ther. 2020, 8, 33–44. [Google Scholar] [CrossRef]
- Miettinen, M. Keratin subsets in spindle cell sarcomas. Keratins are widespread but synovial sarcoma contains a distinctive keratin polypeptide pattern and desmoplakins. Am. J. Pathol. 1991, 138, 505–513. [Google Scholar] [PubMed]
- Dray, T.; Vargas, H.; Weidnerg, N.; Sofferman, R.A. Lymphoepitheliomas of the laryngohypopharynx. Am. J. Otolaryngol. 1998, 19, 263–266. [Google Scholar] [CrossRef]
- Macmillan, C.; Kapadia, S.B.; Finkelstein, S.D.; Nalesnik, M.A.; Barnes, L. Lymphoepithelial carcinoma of the larynx and hypopharynx: Study of eight cases with relationship to Epstein-Barr virus and p53 gene alterations, and review of the literature. Hum. Pathol. 1996, 27, 1172–1179. [Google Scholar] [CrossRef]
- Weiss, L.M.; Movahed, L.A.; Butler, A.E.; Swanson, S.A.; Frierson, H.F.; Cooper, P.H.; Colby, T.V.; Mills, S.E. Analysis of Lymphoepithelioma and Lymphoepithelioma-like Carcinomas for Epstein-Barr Viral Genomes by in situ Hybridization. Am. J. Surg. Pathol. 1989, 13, 625–631. [Google Scholar] [CrossRef]
- Frank, D.K.; Cheron, F.; DiCostanzo, D.; Cho, H.; Sclafani, A. Nonnasopharyngeal Lymphoepitheliomas (Undifferentiated Carcinomas) of the Upper Aerodigestive Tract. Ann. Otol. Rhinol. Laryngol. 1995, 104, 305–310. [Google Scholar] [CrossRef]
- Andryk, J.; Freije, J.E.; Schultz, C.J.; Campbell, B.H.; Komorowski, R.A. Lymphoepithelioma of the larynx. Am. J. Otolaryngol. 1996, 17, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.P.; Vargas, H.I.; Kleiner, D.E.; Merino, M.J. The role of prognostic markers (MiB-1, RB, and bcl-2) in the diagnosis bf parathyroid tumors. Mod. Pathol. 1997, 10, 12–17. [Google Scholar]
- Busuttil, A. Dendritic Pigmented Cells Within Human Laryngeal Mucosa. Arch. Otolaryngol. Neck Surg. 1976, 102, 43–44. [Google Scholar] [CrossRef] [PubMed]
- Reuter, V.E.; Woodruff, J.M. Melanoma of the larynx. Laryngoscope 1986, 94, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.L.; Lawson, W.; Zak, F.G.; Roffman, J.D. The presence of melanocytes in the human larynx. Laryngoscope 1972, 82, 824–835. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.T.; Robbins, K.T.; Weitzner, S. Upper Aerodigestive Tract Metastases in Disseminated Malignant Melanoma. Arch. Otolaryngol. Head Neck Surg. 1986, 112, 659–663. [Google Scholar] [CrossRef]
- Wenig, B.M. Laryngeal mucosal malignant melanoma. A clinicopathologic, immunohistochemical, and ultrastructural study of four patients and review of the literature. Cancer 1995, 75, 1568–1577. [Google Scholar] [CrossRef]
- Mifsud, M.; Padhya, T.A. Metastatic melanoma to the upper aerodigestive tract: A systematic review of the literature. Laryngoscope 2014, 124, 1143–1149. [Google Scholar] [CrossRef]
- Browne, J.D. Management of nonepidermoid cancer of the larynx. Otolaryngol. Clin. N. Am. 2002, 30, 215–229. [Google Scholar] [CrossRef]
- Ferlito, A.; Rinaldo, A.; Devaney, K.O.; Devaney, S.L.; Milroy, C.M. Impact of phenotype on treatment and prognosis of laryngeal malignancies. J. Laryngol. Otol. 2002, 112, 710–714. [Google Scholar] [CrossRef]
- Cavalot, A.L.; Preti, G.; Vione, N.; Nazionale, G.; Palonta, F.; Fadda, G.L. Isolated primary non-Hodgkin’s malignant lymphoma of the larynx. J. Laryngol. Otol. 2001, 115, 324–326. [Google Scholar] [CrossRef]
- Horny, H.-P.; Ferlito, A.; Carbone, A. Laryngeal Lymphoma Derived from Mucosa-Associated Lymphoid Tissue. Ann. Otol. Rhinol. Laryngol. 1996, 105, 577–583. [Google Scholar] [CrossRef]
- Nayak, J.V.; Cook, J.R.; Molina, J.T.; Branch, M.P.; Iv, B.F.B.; Ferris, R.L.; Myers, E.N. Primary Lymphoma of the Larynx: New Diagnostic and Therapeutic Approaches. ORL 2003, 65, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Zinzani, P.L.; Magagnoli, M.; Galieni, P.; Martelli, M.; Poletti, V.; Zaja, F.; Molica, S.; Zaccaria, A.; Cantonetti, A.M.; Gentilini, P.; et al. Nongastrointestinal Low-Grade Mucosa-Associated Lymphoid Tissue Lymphoma: Analysis of 75 Patients. J. Clin. Oncol. 1999, 17, 1254. [Google Scholar] [CrossRef] [PubMed]
- De Bree, R.; Mahieu, H.F.; Ossenkoppele, G.J.; Van Der Valk, P. Malignant lymphoma of mucosa-associated lymphoid tissue in the larynx. Eur. Arch. Oto-Rhino-Laryngol. 1998, 255, 368–370. [Google Scholar] [CrossRef] [PubMed]

| Main Histology Group | Subtypes or Most Common Disease |
|---|---|
| Neuroendocrine Tumors (Epithelial and Neural) |
|
| Spindle-Cell Carcinoma | |
| Minor Salivary Gland Tumors |
|
| Soft Tissue Sarcomas |
|
| Bone/Cartilage Sarcomas |
|
| Lymphoepithelial Carcinoma | |
| Malignant Melanoma |
|
| Primary Lymphoma of the larynx |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiesa-Estomba, C.M.; Barillari, M.R.; Mayo-Yáñez, M.; Maniaci, A.; Fakhry, N.; Cammaroto, G.; Ayad, T.; Lechien, J.R. Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review. J. Pers. Med. 2023, 13, 1084. https://doi.org/10.3390/jpm13071084
Chiesa-Estomba CM, Barillari MR, Mayo-Yáñez M, Maniaci A, Fakhry N, Cammaroto G, Ayad T, Lechien JR. Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review. Journal of Personalized Medicine. 2023; 13(7):1084. https://doi.org/10.3390/jpm13071084
Chicago/Turabian StyleChiesa-Estomba, Carlos M., Maria Rosaria Barillari, Miguel Mayo-Yáñez, Antonino Maniaci, Nicolas Fakhry, Giovanni Cammaroto, Tareck Ayad, and Jerome R. Lechien. 2023. "Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review" Journal of Personalized Medicine 13, no. 7: 1084. https://doi.org/10.3390/jpm13071084
APA StyleChiesa-Estomba, C. M., Barillari, M. R., Mayo-Yáñez, M., Maniaci, A., Fakhry, N., Cammaroto, G., Ayad, T., & Lechien, J. R. (2023). Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review. Journal of Personalized Medicine, 13(7), 1084. https://doi.org/10.3390/jpm13071084










