Survival of Patient-Specific Unicondylar Knee Replacement
Abstract
1. Introduction
2. Materials and Methods
- Lateral or medial chondromalacia Grade III or more, or symptomatic retropatellar osteoarthritis
- ROM < Flexion/Extension 100–10–0°
- Varus/Valgus deformity (hip–knee–ankle angle) > 15°
- Patients with valgus knees and medial osteoarthritis or patients with a varus knee in lateral osteoarthritis
- Status after osteotomy
- Ligament insufficiency
- Allergy against metal ions (Ni, Co, Cr)
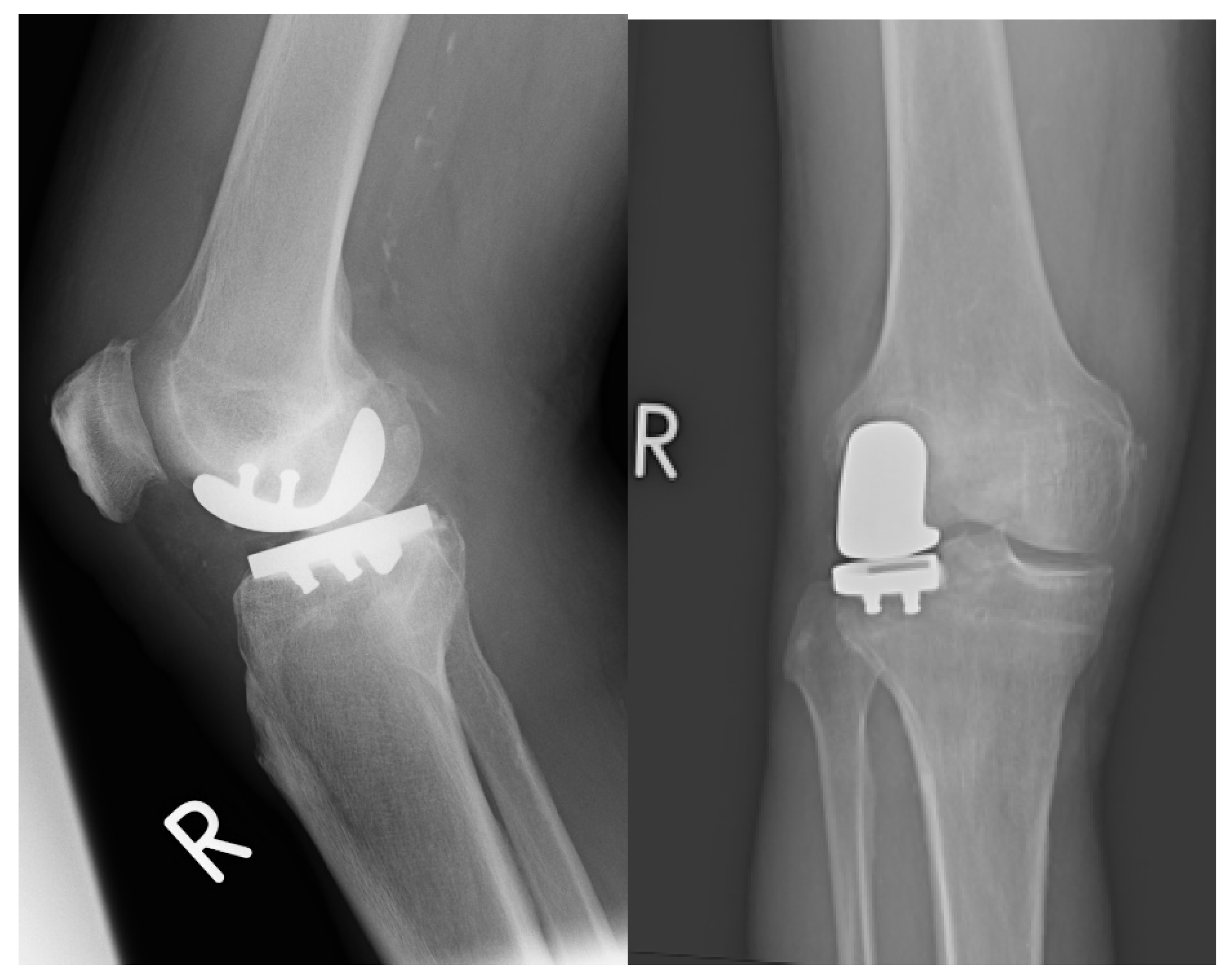
2.1. Prosthesis and Surgical Technique
2.2. Patient Follow-Up and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Preoperative Data
3.2. Follow-Up
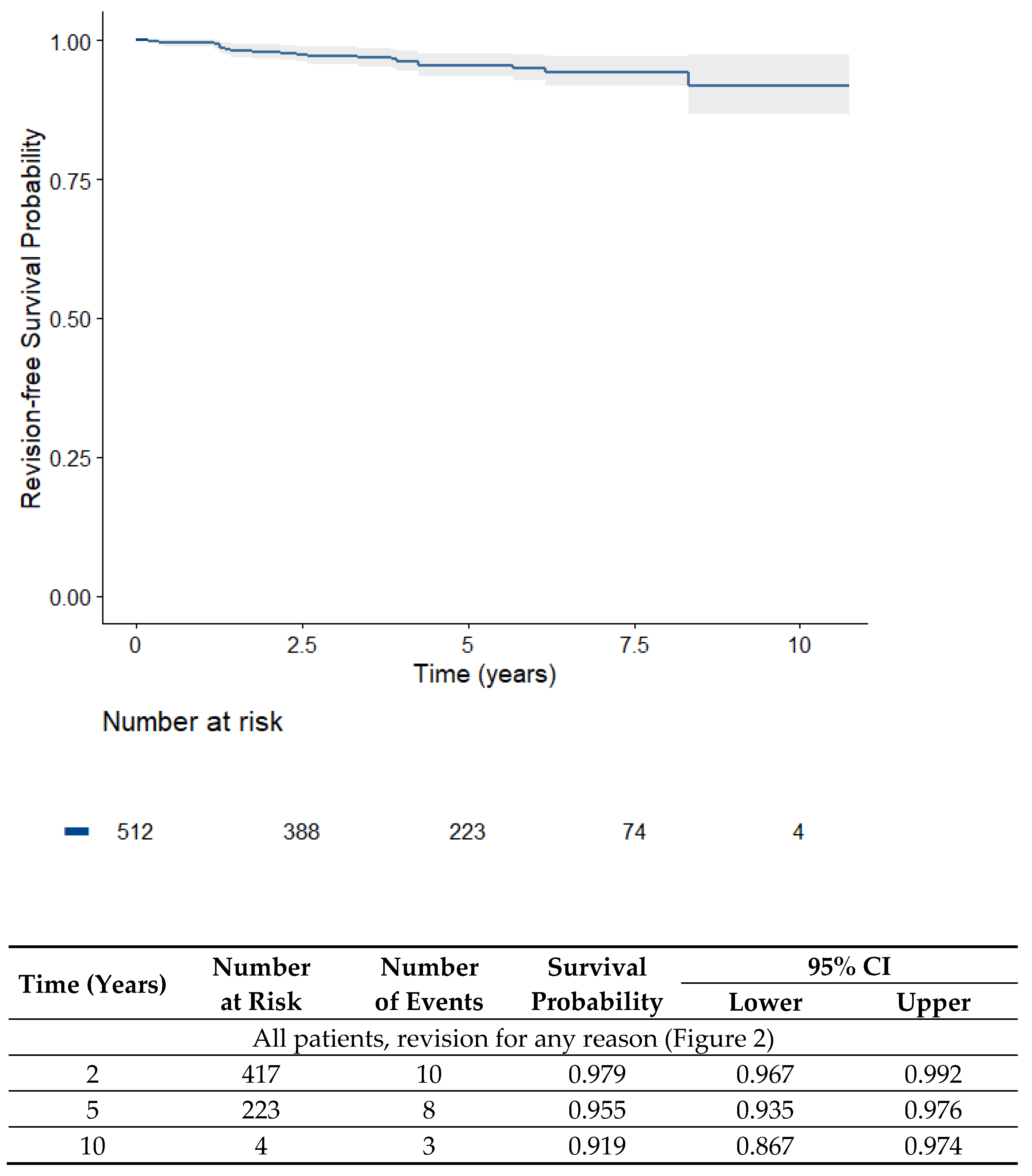
3.3. Survival of the Prosthesis
3.3.1. Overall Survival
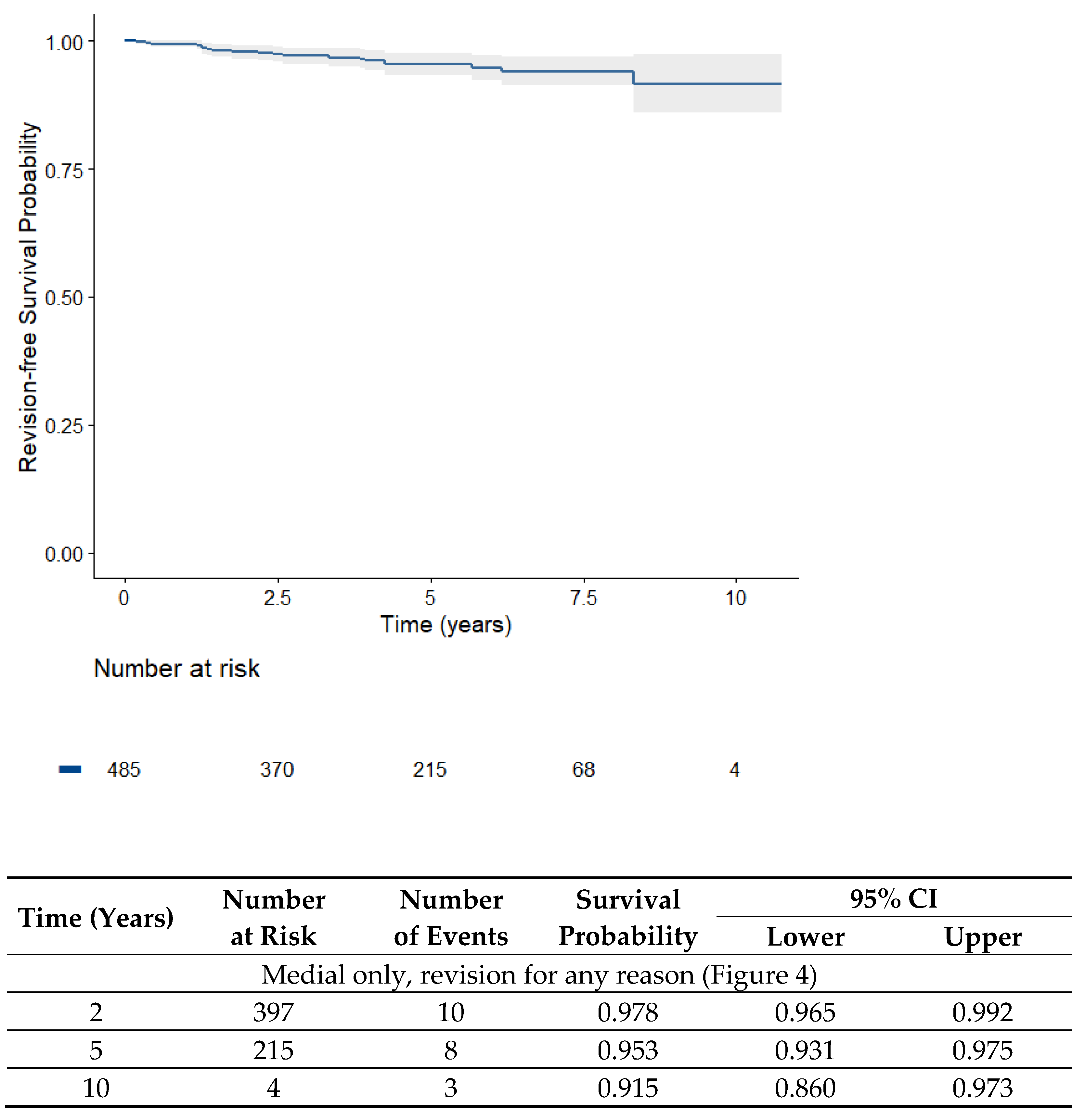
3.3.2. Survival of the Medial UKA
3.3.3. Survival of the Lateral UKA
3.4. Reasons for Revision
| Reason for Revision | |
|---|---|
| Aseptic loosening (six isolated tibial, three combined femoral + tibial) | 9 (1.73%) |
| Infection | 5 (0.97%) |
| Older periprosthetic fracture | 1 (0.2%) |
| Tibial bone marrow edema | 1 (0.2%) |
| Progressive osteoarthritis in the other compartments | 1 (0.2%) |
| Infrapatellar contracture syndrome (revision at external institution) | 1 (0.2%) |
| Not reported (revision at external institution) | 1 (0.2%) |
3.5. Radiological Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heyse, T.J.; El-Zayat, B.F.; De Corte, R.; Chevalier, Y.; Scheys, L.; Innocenti, B.; Fuchs-Winkelmann, S.; Labey, L. UKA closely preserves natural knee kinematics in vitro. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2014, 22, 1902–1910. [Google Scholar] [CrossRef] [PubMed]
- Muller, P.E.; Pellengahr, C.; Witt, M.; Kircher, J.; Refior, H.J.; Jansson, V. Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J. Arthroplast. 2004, 19, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Price, A.J.; Rees, J.L.; Beard, D.J.; Gill, R.H.; Dodd, C.A.; Murray, D.M. Sagittal plane kinematics of a mobile-bearing unicompartmental knee arthroplasty at 10 years: A comparative in vivo fluoroscopic analysis. J. Arthroplast. 2004, 19, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Price, A.J.; Webb, J.; Topf, H.; Dodd, C.A.; Goodfellow, J.W.; Murray, D.W.; Oxford, H.; Knee, G. Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J. Arthroplast. 2001, 16, 970–976. [Google Scholar] [CrossRef]
- Pongcharoen, B.; Liengwattanakol, P.; Boontanapibul, K. Comparison of Functional Recovery Between Unicompartmental and Total Knee Arthroplasty: A Randomized Controlled Trial. J. Bone Jt. Surg. Am. Vol. 2023, 105, 191–201. [Google Scholar] [CrossRef]
- Wu, L.P.; Mayr, H.O.; Zhang, X.; Huang, Y.Q.; Chen, Y.Z.; Li, Y.M. Knee Scores of Patients with Non-Lateral Compartmental Knee Osteoarthritis Undergoing Mobile, Fixed-Bearing Unicompartmental Knee and Total Knee Arthroplasties: A Randomized Controlled Trial. Orthop. Surg. 2022, 14, 73–87. [Google Scholar] [CrossRef]
- Goodfellow, J.W.; O’Connor, J.J.; Murray, D.W. A critique of revision rate as an outcome measure: Re-interpretation of knee joint registry data. J. Bone Jt. Surg. Br. Vol. 2010, 92, 1628–1631. [Google Scholar] [CrossRef]
- EndoprothesenregisterDeutschland. Jahresbericht 2022. 2022. Available online: https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/Jahresbericht2022-Status5_2022-10-25_F.pdf (accessed on 10 January 2023).
- Weber, P.; Schroder, C.; Schmidutz, F.; Kraxenberger, M.; Utzschneider, S.; Jansson, V.; Muller, P.E. Increase of tibial slope reduces backside wear in medial mobile bearing unicompartmental knee arthroplasty. Clin. Biomech. 2013, 28, 904–909. [Google Scholar] [CrossRef]
- Weber, P.; Schroder, C.; Schwiesau, J.; Utzschneider, S.; Steinbruck, A.; Pietschmann, M.F.; Jansson, V.; Muller, P.E. Increase in the tibial slope reduces wear after medial unicompartmental fixed-bearing arthroplasty of the knee. Biomed. Res. Int. 2015, 2015, 736826. [Google Scholar] [CrossRef]
- Weber, P.; Woiczinski, M.; Steinbruck, A.; Schmidutz, F.; Niethammer, T.; Schroder, C.; Jansson, V.; Muller, P.E. Increase in the Tibial Slope in Unicondylar Knee Replacement: Analysis of the Effect on the Kinematics and Ligaments in a Weight-Bearing Finite Element Model. Biomed. Res. Int. 2018, 2018, 8743604. [Google Scholar] [CrossRef]
- Weber, P.; Crispin, A.; Schmidutz, F.; Utzschneider, S.; Pietschmann, M.F.; Jansson, V.; Muller, P.E. Improved accuracy in computer-assisted unicondylar knee arthroplasty: A meta-analysis. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2013, 21, 2453–2461. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Lv, G.; Yin, P.; Dong, S.; Dai, Z.; Li, L.; Liu, G. Effect of tibial component overhang on survivorship in medial mobile-bearing unicompartmental knee arthroplasty. Knee 2022, 37, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, D.P.; Holmberg, R.R.; Quartulli, M.J.; Barnes, C.L. Tibial plateau coverage in UKA: A comparison of patient specific and off-the-shelf implants. J. Arthroplast. 2014, 29, 1694–1698. [Google Scholar] [CrossRef] [PubMed]
- Koeck, F.X.; Beckmann, J.; Luring, C.; Rath, B.; Grifka, J.; Basad, E. Evaluation of implant position and knee alignment after patient-specific unicompartmental knee arthroplasty. Knee 2011, 18, 294–299. [Google Scholar] [CrossRef]
- Hernigou, P.; Deschamps, G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J. Bone Jt. Surg. Am. 2004, 86, 506–511. [Google Scholar] [CrossRef]
- Ollivier, M.; Abdel, M.P.; Parratte, S.; Argenson, J.N. Lateral unicondylar knee arthroplasty (UKA): Contemporary indications, surgical technique, and results. Int. Orthop. 2014, 38, 449–455. [Google Scholar] [CrossRef]
- Bonanzinga, T.; Tanzi, P.; Altomare, D.; Dorotei, A.; Iacono, F.; Marcacci, M. High survivorship rate and good clinical outcomes at mid-term follow-up for lateral UKA: A systematic literature review. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2021, 29, 3262–3271. [Google Scholar] [CrossRef]
- Arnholdt, J.; Holzapfel, B.M.; Sefrin, L.; Rudert, M.; Beckmann, J.; Steinert, A.F. Individualized unicondylar knee replacement: Use of patient-specific implants and instruments. Oper. Orthop. Traumatol. 2017, 29, 31–39. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- National_Joint_Registry_for_England_and_Wales. Report; 2022; p. 371. Available online: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR 19th Annual Report 2022.pdf (accessed on 10 January 2023).
- AustralianOrthopaedicAssociationNationalJointReplacementRegistry. Hip, Knee & Shoulder Arthroplasty 2022 ANNUAL REPORT; Australian Orthopaedic Association National Joint Replacement Registry: 2022. Available online: https://aoanjrr.sahmri.com/documents/10180/732916/AOA+2022+AR+Digital/f63ed890-36d0-c4b3-2e0b-7b63e2071b16 (accessed on 10 January 2023).
- Burger, J.A.; Kleeblad, L.J.; Laas, N.; Pearle, A.D. Mid-term survivorship and patient-reported outcomes of robotic-arm assisted partial knee arthroplasty. Bone Jt. J. 2020, 102, 108–116. [Google Scholar] [CrossRef]
- St Mart, J.P.; de Steiger, R.N.; Cuthbert, A.; Donnelly, W. The three-year survivorship of robotically assisted versus non-robotically assisted unicompartmental knee arthroplasty. Bone Jt. J. 2020, 102, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Pumilia, C.A.; Schroeder, L.; Sarpong, N.O.; Martin, G. Patient Satisfaction, Functional Outcomes, and Implant Survivorship in Patients Undergoing Customized Unicompartmental Knee Arthroplasty. J. Pers. Med. 2021, 11, 753. [Google Scholar] [CrossRef] [PubMed]
- Freigang, V.; Rupp, M.; Pfeifer, C.; Worlicek, M.; Radke, S.; Deckelmann, S.; Alt, V.; Baumann, F. Patient-reported outcome after patient-specific unicondylar knee arthroplasty for unicompartmental knee osteoarthritis. BMC Musculoskelet. Disord. 2020, 21, 773. [Google Scholar] [CrossRef]
- Smith, E.; Lee, D.; Masonis, J.; Melvin, J.S. Lateral Unicompartmental Knee Arthroplasty. JBJS Rev. 2020, 8, e0044. [Google Scholar] [CrossRef]
- Baker, P.N.; Jameson, S.S.; Deehan, D.J.; Gregg, P.J.; Porter, M.; Tucker, K. Mid-term equivalent survival of medial and lateral unicondylar knee replacement: An analysis of data from a National Joint Registry. J. Bone Jt. Surg. Br. Vol. 2012, 94, 1641–1648. [Google Scholar] [CrossRef] [PubMed]
- Demange, M.K.; Von Keudell, A.; Probst, C.; Yoshioka, H.; Gomoll, A.H. Patient-specific implants for lateral unicompartmental knee arthroplasty. Int. Orthop. 2015, 39, 1519–1526. [Google Scholar] [CrossRef]
- Chau, R.; Gulati, A.; Pandit, H.; Beard, D.J.; Price, A.J.; Dodd, C.A.; Gill, H.S.; Murray, D.W. Tibial component overhang following unicompartmental knee replacement--does it matter? Knee 2009, 16, 310–313. [Google Scholar] [CrossRef]
- Saltybaeva, N.; Jafari, M.E.; Hupfer, M.; Kalender, W.A. Estimates of effective dose for CT scans of the lower extremities. Radiology 2014, 273, 153–159. [Google Scholar] [CrossRef]
- FDA. What are the Radiation Risks from CT? Available online: https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/what-are-radiation-risks-ct (accessed on 19 March 2023).
- Amis, E.S., Jr.; Butler, P.F.; Applegate, K.E.; Birnbaum, S.B.; Brateman, L.F.; Hevezi, J.M.; Mettler, F.A.; Morin, R.L.; Pentecost, M.J.; Smith, G.G.; et al. American College of Radiology white paper on radiation dose in medicine. J. Am. Coll. Radiol. 2007, 4, 272–284. [Google Scholar] [CrossRef]
- Knifsund, J.; Niinimaki, T.; Nurmi, H.; Toom, A.; Keemu, H.; Laaksonen, I.; Seppanen, M.; Liukas, A.; Pamilo, K.; Vahlberg, T.; et al. Functional results of total-knee arthroplasty versus medial unicompartmental arthroplasty: Two-year results of a randomised, assessor-blinded multicentre trial. BMJ Open 2021, 11, e046731. [Google Scholar] [CrossRef]


| Variable | Total (n = 537) | Medial UKA (n = 507) | Lateral (n = 30) |
|---|---|---|---|
| Mean age, years (SD) | 66.6 (9.4) | 66.9 (9.9) | 60.9 (9.4) |
| Male sex, n (%) Mean BMI, kg/m2 (SD) | 313 (58.3) 29.2 (4.9) | 299 (59.0) 29.4 (4.9) 1 | 16 (53.3) 26.2 (3.6) |
| Preoperative KL 1 grade, n (%) | |||
| Grade 1 to 2 | 0.2% * | 0.2% | 0 |
| Grade 3 to 4 | 99.8 | 99.8 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weber, P.; Beck, M.; Klug, M.; Klug, A.; Klug, A.; Glowalla, C.; Gollwitzer, H. Survival of Patient-Specific Unicondylar Knee Replacement. J. Pers. Med. 2023, 13, 665. https://doi.org/10.3390/jpm13040665
Weber P, Beck M, Klug M, Klug A, Klug A, Glowalla C, Gollwitzer H. Survival of Patient-Specific Unicondylar Knee Replacement. Journal of Personalized Medicine. 2023; 13(4):665. https://doi.org/10.3390/jpm13040665
Chicago/Turabian StyleWeber, Patrick, Melina Beck, Michael Klug, Andreas Klug, Alexander Klug, Claudio Glowalla, and Hans Gollwitzer. 2023. "Survival of Patient-Specific Unicondylar Knee Replacement" Journal of Personalized Medicine 13, no. 4: 665. https://doi.org/10.3390/jpm13040665
APA StyleWeber, P., Beck, M., Klug, M., Klug, A., Klug, A., Glowalla, C., & Gollwitzer, H. (2023). Survival of Patient-Specific Unicondylar Knee Replacement. Journal of Personalized Medicine, 13(4), 665. https://doi.org/10.3390/jpm13040665







