Evaluation of the Association between Low-Density Lipoprotein (LDL) and All-Cause Mortality in Geriatric Patients with Hip Fractures: A Prospective Cohort Study of 339 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Hospital Treatment
2.4. Follow-Up
2.5. Endpoint Events
2.6. Variables
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Univariate Analysis of Association between Variates and Mortality
3.3. Multivariate Analysis between LDL and Mortality
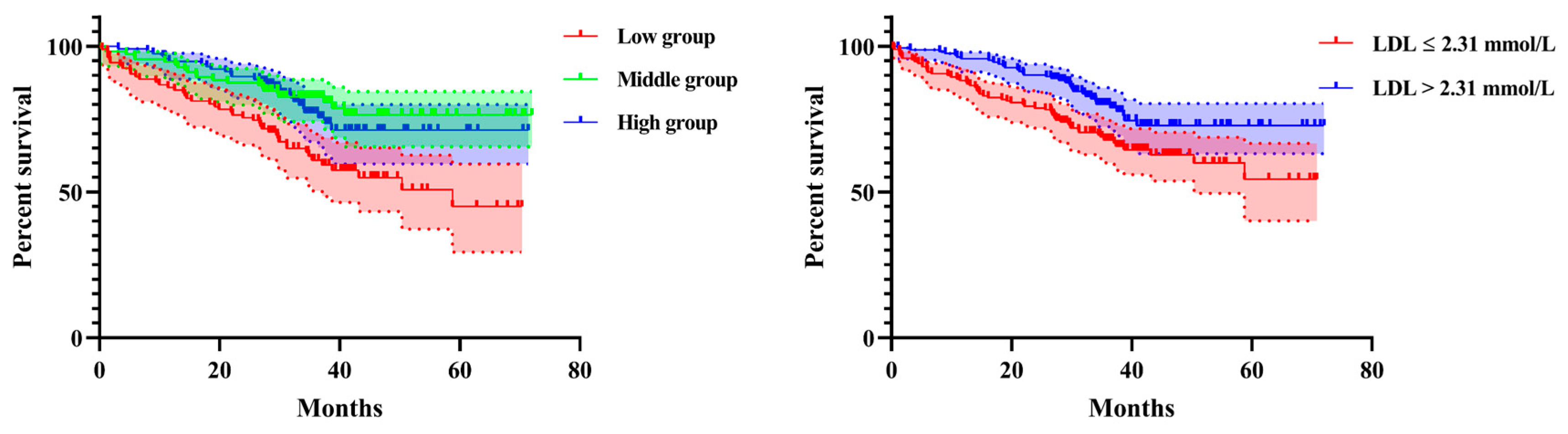
3.4. Curve Fitting and Analysis of Threshold Effect
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| aCCI | age-adjusted Charlson comorbidity index |
| CHD | coronary heart disease |
| CI | confidence interval |
| COPD | chronic obstructive pulmonary disease |
| HR | Hazard ratio |
References
- Watts, N.B.; Bilezikian, J.P.; Usiskin, K.; Edwards, R.; Desai, M.; Law, G.; Meininger, G. Effects of Canagliflozin on Fracture Risk in Patients with Type 2 Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2016, 101, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Borgström, F.; Karlsson, L.; Ortsäter, G.; Norton, N.; Halbout, P.; Cooper, C.; Lorentzon, M.; McCloskey, E.V.; Harvey, N.C.; Javaid, M.K.; et al. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 2020, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.M.; Russell, L.; Khan, S.N. Osteoporosis. Clin. Orthop. Relat. Res. 2000, 372, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.V. Association of BMD and FRAX Score with Risk of Fracture in Older Adults with Type 2 Diabetes. JAMA 2011, 305, 2184–2192. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, E.V.; Oden, A.; Harvey, N.C.; Leslie, W.D.; Hans, D.; Johansson, H.; Barkmann, R.; Boutroy, S.; Brown, J.; Chapurlat, R.; et al. A meta-analysis oftrabecular bone score in fracture risk prediction and its relationship to FRAX. J. Bone Miner. Res. 2016, 31, 940–948. [Google Scholar] [CrossRef]
- Middleton, R.G.; Shabani, F.; Uzoigwe, C.E.; Moqsith, M.; Venkatesan, M. FRAX and the assessment of the risk of developing a fragility fracture. J. Bone Jt. Surg. Br. Vol. 2012, 94-B, 1313–1320. [Google Scholar] [CrossRef]
- Viégas, M.; Costa, C.; Lopes, A.; Griz, L.; Medeiro, M.A.; Bandeira, F. Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J. Diabetes Its Complicat. 2011, 25, 216–221. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Warriner, A.H.; Patkar, N.M.; Curtis, J.R.; Delzell, E.; Gary, L.; Kilgore, M.; Saag, K. Which fractures are most attributable to osteoporosis? J. Clin. Epidemiol. 2011, 64, 46–53. [Google Scholar] [CrossRef]
- Kanis, J.A.; Oden, A.; Johnell, O.; Jonsson, B.; de Laet, C.; Dawson, A. The Burden of Osteoporotic Fractures: A Method for Setting Intervention Thresholds. Osteoporos. Int. 2001, 12, 417–427. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J. Epidemiology of osteoporotic fractures. Osteoporos. Int. 2004, 16, S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos. Int. 2004, 15, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Ström, O.; Borgström, F.; Kanis, J.A.; Compston, J.; Cooper, C.; McCloskey, E.V.; Jonsson, B.G. Osteoporosis: Burden, health care provision and opportunities in the EU. Arch. Osteoporos. 2011, 6, 59–155. [Google Scholar] [CrossRef] [PubMed]
- Dennison, E.; Cooper, C. Epidemiology of Osteoporotic Fractures. Horm. Res. Paediatr. 2000, 54, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Borgström, F.; Sobocki, P.; Ström, O.; Jönsson, B. The societal burden of osteoporosis in Sweden. Bone 2007, 40, 1602–1609. [Google Scholar] [CrossRef] [PubMed]
- Barceló, M.; Torres, O.H.; Mascaró, J.; Casademont, J. Hip fracture and mortality: Study of specific causes of death and risk factors. Arch. Osteoporos. 2021, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Elffors, I.; Allander, E.; Kanis, J.A.; Gullberg, B.; Johnell, O.; Dequeker, J.; Dilsen, G.; Gennari, C.; Vaz, A.A.L.; Lyritis, G.; et al. The variable incidence of hip fracture in Southern Europe: The MEDOS study. Osteoporos. Int. 1994, 4, 253–263. [Google Scholar] [CrossRef]
- Chang, W.; Lv, H.; Feng, C.; Yuwen, P.; Wei, N.; Chen, W.; Zhang, Y. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int. J. Surg. 2018, 52, 320–328. [Google Scholar] [CrossRef]
- Bilsel, K.; Erdil, M.; Gulabi, D.; Elmadag, M.; Cengiz, O.; Sen, C. Factors affecting mortality after hip fracture surgery: A retrospective analysis of 578 patients. Eur. J. Orthop. Surg. Traumatol. 2012, 23, 895–900. [Google Scholar] [CrossRef]
- Dwivedi, A.; Änggård, E.E.; Carrier, M.J. Oxidized LDL-Mediated Monocyte Adhesion to Endothelial Cells Does Not Involve NFκB. Biochem. Biophys. Res. Commun. 2001, 284, 239–244. [Google Scholar] [CrossRef]
- Perrin-Cocon, L.; Coutant, F.; Agaugué, S.; Deforges, S.; André, P.; Lotteau, V. Oxidized Low-Density Lipoprotein Promotes Mature Dendritic Cell Transition from Differentiating Monocyte. J. Immunol. 2001, 167, 3785–3791. [Google Scholar] [CrossRef] [PubMed]
- Ghio, M.; Fabbi, P.; Contini, P.; Fedele, M.; Brunelli, C.; Indiveri, F.; Barsotti, A. OxLDL- and HSP-60 antigen-specific CD8+ T lymphocytes are detectable in the peripheral blood of patients suffering from coronary artery disease. Clin. Exp. Med. 2012, 13, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Major, A.S.; Fazio, S.; Linton, M.F. B-Lymphocyte Deficiency Increases Atherosclerosis in LDL Receptor–Null Mice. Arter. Thromb. Vasc. Biol. 2002, 22, 1892–1898. [Google Scholar] [CrossRef] [PubMed]
- Luegmayr, E.; Glantschnig, H.; Wesolowski, G.A.; Gentile, M.A.; Fisher, J.E.; Rodan, G.A.; Reszka, A.A. Osteoclast formation, survival and morphology are highly dependent on exogenous cholesterol/lipoproteins. Cell Death Differ. 2004, 11, S108–S118. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Shen, H.; Su, K.-J.; Zhang, J.-G.; Tian, Q.; Zhao, L.-J.; Qiu, C.; Zhang, Q.; Garrett, T.J.; Liu, J.; et al. Metabolomic profiles associated with bone mineral density in US Caucasian women. Nutr. Metab. 2018, 15, 57. [Google Scholar] [CrossRef]
- El Maghraoui, A.; Rezqi, A.; El Mrahi, S.; Sadni, S.; Ghozlani, I.; Mounach, A. Osteoporosis, vertebral fractures and metabolic syndrome in postmenopausal women. BMC Endocr. Disord. 2014, 14, 93. [Google Scholar] [CrossRef]
- Nielson, C.M.; Srikanth, P.; Orwoll, E.S. Obesity and fracture in men and women: An epidemiologic perspective. J. Bone Miner. Res. 2011, 27, 1–10. [Google Scholar] [CrossRef]
- Barzilay, J.I.; Buzkova, P.; Kuller, L.H.; Cauley, J.A.; Fink, H.A.; Sheets, K.; Robbins, J.A.; Carbone, L.D.; Elam, R.E.; Mukamal, K.J. The Association of Lipids and Lipoproteins with Hip Fracture Risk: The Cardiovascular Health Study. Am. J. Med. 2022, 135, 1101–1108.e1. [Google Scholar] [CrossRef]
- Guijarro, C.; Cosín-Sales, J. Colesterol LDL y aterosclerosis: Evidencias. Clínica E Investig. En Arterioscler. 2021, 33, 25–32. [Google Scholar] [CrossRef]
- Alekos, N.S.; Moorer, M.C.; Riddle, R.C. Dual Effects of Lipid Metabolism on Osteoblast Function. Front. Endocrinol. 2020, 11, 578194. [Google Scholar] [CrossRef]
- Tintut, Y.; Demer, L.L. Effects of bioactive lipids and lipoproteins on bone. Trends Endocrinol. Metab. 2013, 25, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Yu, X. Lipid metabolism disorders and bone dysfunction-interrelated and mutually regulated (Review). Mol. Med. Rep. 2015, 12, 783–794. [Google Scholar] [CrossRef] [PubMed]
- Kan, B.; Zhao, Q.; Wang, L.; Xue, S.; Cai, H.; Yang, S. Association between lipid biomarkers and osteoporosis: A cross-sectional study. BMC Musculoskelet. Disord. 2021, 22, 759. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Liu, J.; Zhao, K.; Gao, L.; Zhao, J. Cholesterol-induced toxicity: An integrated view of the role of cholesterol in multiple diseases. Cell Metab. 2021, 33, 1911–1925. [Google Scholar] [CrossRef]
- Johannesen, C.D.L.; Langsted, A.; Mortensen, M.B.; Nordestgaard, B.G. Association between low density lipoprotein and all cause and cause specific mortality in Denmark: Prospective cohort study. BMJ 2020, 371, m4266. [Google Scholar] [CrossRef]
- Jacobs, D.; Blackburn, H.; Higgins, M.; Reed, D.; Iso, H.; McMillan, G.; Neaton, J.; Nelson, J.; Potter, J.; Rifkind, B. Report of the Conference on Low Blood Cholesterol: Mortality Associations. Circulation 1992, 86, 1046–1060. [Google Scholar] [CrossRef]
- Franzo, P.R.R.R.S. Serum Cholesterol Levels as a Measure of Frailty in Elderly Patients. Exp. Aging Res. 1998, 24, 169–179. [Google Scholar] [CrossRef]
- Zeng, X.; Zhou, X.; Tan, X.-R.; Chen, Y.-Q. Admission LDL-C and long-term mortality in patients with acute aortic dissection: A survival analysis in China. Ann. Transl. Med. 2021, 9, 1345. [Google Scholar] [CrossRef]
- Charach, G.; Rabinovich, A.; Ori, A.; Weksler, D.; Sheps, D.; Charach, L.; Weintraub, M.; George, J. Low Levels of Low-Density Lipoprotein Cholesterol: A Negative Predictor of Survival in Elderly Patients with Advanced Heart Failure. Cardiology 2013, 127, 45–50. [Google Scholar] [CrossRef]
- Greene, S.J.; Vaduganathan, M.; Lupi, L.; Ambrosy, A.P.; Mentz, R.J.; Konstam, M.A.; Nodari, S.; Subacius, H.P.; Fonarow, G.C.; Bonow, R.O.; et al. Prognostic Significance of Serum Total Cholesterol and Triglyceride Levels in Patients Hospitalized for Heart Failure with Reduced Ejection Fraction (from the EVEREST Trial). Am. J. Cardiol. 2013, 111, 574–581. [Google Scholar] [CrossRef]
- Cheng, K.-H.; Chu, C.-S.; Lin, T.-H.; Lee, K.-T.; Sheu, S.-H.; Lai, W.-T. Lipid Paradox in Acute Myocardial Infarction—The Association with 30-Day In-Hospital Mortality. Crit. Care Med. 2015, 43, 1255–1264. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.S.; Bui, Q.T.; Jacobs, J.R.; Begelman, S.M.; Miller, D.P.; French, W.J. Relationship Between Serum Low-Density Lipoprotein Cholesterol and In-hospital Mortality Following Acute Myocardial Infarction (The Lipid Paradox). Am. J. Cardiol. 2015, 115, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Nakahashi, T.; Tada, H.; Sakata, K.; Yakuta, Y.; Tanaka, Y.; Nomura, A.; Gamou, T.; Terai, H.; Horita, Y.; Ikeda, M.; et al. Paradoxical impact of decreased low-density lipoprotein cholesterol level at baseline on the long-term prognosis in patients with acute coronary syndrome. Heart Vessel. 2017, 33, 695–705. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Liu, J.; Chen, S.; Ying, M.; Chen, G.; Liu, L.; Lun, Z.; Li, H.; Huang, H.; Li, Q.; et al. Malnutrition affects cholesterol paradox in coronary artery disease: A 41,229 Chinese cohort study. Lipids Health Dis. 2021, 20, 36. [Google Scholar] [CrossRef]
- Wang, T.Y.; Newby, L.K.; Chen, A.Y.; Ms, J.M.; Roe, M.T.; Sonel, A.F.; Bhatt, D.L.; DeLong, E.R.; Ohman, E.M.; Gibler, W.B.; et al. Hypercholesterolemia Paradox in Relation to Mortality in Acute Coronary Syndrome. Clin. Cardiol. 2009, 32, E22–E28. [Google Scholar] [CrossRef]
- Zheng, J.; Brion, M.; Kemp, J.P.; Warrington, N.M.; Borges, M.; Hemani, G.; Richardson, T.G.; Rasheed, H.; Qiao, Z.; Haycock, P.; et al. The Effect of Plasma Lipids and Lipid-Lowering Interventions on Bone Mineral Density: A Mendelian Randomization Study. J. Bone Miner. Res. 2020, 35, 1224–1235. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Sugimoto, T.; Yano, S.; Yamauchi, M.; Sowa, H.; Chen, Q.; Chihara, K. Plasma Lipids and Osteoporosis in Postmenopausal Women. Endocr. J. 2002, 49, 211–217. [Google Scholar] [CrossRef]
- Iseri, K.; Dai, L.; Chen, Z.; Qureshi, A.R.; Brismar, T.B.; Stenvinkel, P.; Lindholm, B. Bone mineral density and mortality in end-stage renal disease patients. Clin. Kidney J. 2020, 13, 307–321. [Google Scholar] [CrossRef]
- Iseri, K.; Qureshi, A.R.; Dai, L.; Ripsweden, J.; Heimbürger, O.; Barany, P.; Bergström, I.; Stenvinkel, P.; Brismar, T.B.; Lindholm, B. Bone mineral density at different sites and 5 years mortality in end-stage renal disease patients: A cohort study. Bone 2020, 130, 115075. [Google Scholar] [CrossRef]
- Orlic, L.; Mikolasevic, I.; Crncevic-Orlic, Z.; Jakopcic, I.; Josipovic, J.; Pavlovic, D. Forearm bone mass predicts mortality in chronic hemodialysis patients. J. Bone Miner. Metab. 2016, 35, 396–404. [Google Scholar] [CrossRef]
- Disthabanchong, S.; Jongjirasiri, S.; Adirekkiat, S.; Sumethkul, V.; Ingsathit, A.; Domrongkitchaiporn, S.; Phakdeekitcharoen, B.; Kantachuvesiri, S.; Kitiyakara, C. Low Hip Bone Mineral Density Predicts Mortality in Maintenance Hemodialysis Patients: A Five-Year Follow-Up Study. Blood Purif. 2014, 37, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Äijänseppä, S.; Kivinen, P.; Helkala, E.-L.; Kivelä, S.-L.; Tuomilehto, J.; Nissinen, A. Serum cholesterol and depressive symptoms in elderly Finnish men. Int. J. Geriatr. Psychiatry 2002, 17, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Loggers, S.A.; Van Lieshout, E.M.; Joosse, P.; Verhofstad, M.H.; Willems, H.C. Prognosis of nonoperative treatment in elderly patients with a hip fracture: A systematic review and meta-analysis. Injury 2020, 51, 2407–2413. [Google Scholar] [CrossRef]
- Neuman, M.D.; Fleisher, L.A.; Even-Shoshan, O.; Mi, L.; Silber, J.H. Nonoperative Care for Hip Fracture in the Elderly. Med Care 2010, 48, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Cram, P.; Yan, L.; Bohm, E.; Kuzyk, P.; Lix, L.M.; Morin, S.N.; Majumdar, S.R.; Leslie, W.D. Trends in Operative and Nonoperative Hip Fracture Management 1990–2014: A Longitudinal Analysis of Manitoba Administrative Data. J. Am. Geriatr. Soc. 2016, 65, 27–34. [Google Scholar] [CrossRef]
- Fischer, V.; Haffner-Luntzer, M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin. Cell Dev. Biol. 2021, 123, 14–21. [Google Scholar] [CrossRef]
- Artal, M.D.M.; Chacón, O.R.; Martínez-Alonso, M.; Godoy, M.S.; Mas-Atance, J.; Gutiérrez, R.G. Fractura de cadera en el paciente anciano: Factores pronóstico de mortalidad y recuperación funcional al año. Rev. Española De Geriatría Y Gerontol. 2018, 53, 247–254. [Google Scholar] [CrossRef]

| LDL Tertiles | Low | Middle | High | p-Value | p-Value * |
|---|---|---|---|---|---|
| N | 111 | 112 | 116 | ||
| LDL | 1.54 ± 0.33 | 2.29 ± 0.19 | 3.27 ± 0.48 | <0.001 | <0.001 |
| Age (years) | 81.36 ± 6.30 | 79.76 ± 6.45 | 79.01 ± 6.45 | 0.02 | 0.032 |
| Sex | 0.028 | - | |||
| Male | 45 (40.54%) | 39 (34.82%) | 28 (24.14%) | ||
| Female | 66 (59.46%) | 73 (65.18%) | 88 (75.86%) | ||
| Occupation | 0.618 | - | |||
| Retirement | 62 (55.86%) | 61 (54.46%) | 68 (58.62%) | ||
| Farmer | 29 (26.13%) | 23 (20.54%) | 23 (19.83%) | ||
| Other | 20 (18.02%) | 28 (25.00%) | 25 (21.55%) | ||
| History of allergy | 11 (9.91%) | 7 (6.25%) | 9 (7.76%) | 0.598 | - |
| Injury mechanism | 0.427 | 0.379 | |||
| Falling | 106 (95.50%) | 109 (97.32%) | 115 (99.14%) | ||
| Accident | 3 (2.70%) | 1 (0.89%) | 1 (0.86%) | ||
| Other | 2 (1.80%) | 2 (1.79%) | 0 (0.00%) | ||
| Fracture classification | 0.009 | 0.005 | |||
| Intertrochanteric fracture | 87 (78.38%) | 83 (74.11%) | 69 (59.48%) | ||
| Femoral neck fracture | 24 (21.62%) | 25 (22.32%) | 43 (37.07%) | ||
| Subtrochanteric fracture | 0 (0.00%) | 4 (3.57%) | 4 (3.45%) | ||
| Hypertension | 60 (54.05%) | 64 (57.14%) | 72 (62.07%) | 0.466 | - |
| Diabetes | 24 (21.62%) | 19 (16.96%) | 27 (23.28%) | 0.477 | - |
| CHD | 57 (51.35%) | 53 (47.32%) | 56 (48.28%) | 0.82 | - |
| Arrhythmia | 44 (39.64%) | 29 (25.89%) | 25 (21.55%) | 0.008 | - |
| Hemorrhagic stroke | 1 (0.90%) | 3 (2.68%) | 5 (4.31%) | 0.279 | 0.311 |
| Ischemic stroke | 44 (39.64%) | 39 (34.82%) | 37 (31.90%) | 0.47 | - |
| Cancer | 2 (1.80%) | 4 (3.57%) | 3 (2.59%) | 0.712 | 0.777 |
| Multiple injuries | 4 (3.60%) | 9 (8.04%) | 7 (6.03%) | 0.372 | - |
| Dementia | 6 (5.41%) | 7 (6.25%) | 6 (5.17%) | 0.934 | - |
| COPD | 6 (5.41%) | 7 (6.25%) | 5 (4.31%) | 0.807 | - |
| Hepatitis | 2 (1.80%) | 2 (1.79%) | 2 (1.72%) | 0.999 | 1 |
| Gastritis | 1 (0.90%) | 3 (2.68%) | 3 (2.59%) | 0.575 | 0.707 |
| Treatment strategy | 0.002 | - | |||
| Conservation | 14 (12.61%) | 2 (1.79%) | 7 (6.03%) | ||
| ORIF | 73 (65.77%) | 84 (75.00%) | 65 (56.03%) | ||
| HA | 24 (21.62%) | 25 (22.32%) | 43 (37.07%) | ||
| THA | 0 (0.00%) | 1 (0.89%) | 1 (0.86%) | ||
| Time to admission (h) | 128.73 ± 530.08 | 100.21 ± 203.31 | 94.80 ± 263.95 | 0.75 | 0.819 |
| Time to operation (d) | 4.61 ± 2.04 | 4.63 ± 2.24 | 4.79 ± 2.60 | 0.827 | 0.985 |
| Operation time (mins) | 101.02 ± 41.34 | 96.36 ± 32.08 | 100.28 ± 38.61 | 0.621 | 0.975 |
| Blood loss (mL) | 247.66 ± 156.49 | 212.67 ± 114.02 | 241.40 ± 159.01 | 0.183 | 0.441 |
| Infusion (mL) | 1521.08 ± 354.91 | 1587.92 ± 360.94 | 1597.77 ± 383.82 | 0.289 | 0.259 |
| Transfusion (U) | 1.24 ± 1.27 | 1.12 ± 1.22 | 0.87 ± 1.26 | 0.1 | 0.055 |
| Length in hospital (d) | 8.59 ± 3.46 | 8.35 ± 2.63 | 8.45 ± 2.67 | 0.82 | 0.954 |
| Follow-up (months) | 31.02 ± 17.91 | 36.62 ± 15.02 | 34.86 ± 13.09 | 0.023 | 0.039 |
| Mortality | 49 (44.14%) | 22 (19.64%) | 28 (24.14%) | <0.001 | - |
| Exposure | Non-Adjusted Model | Minimally-Adjusted Model | Fully Adjusted Model |
|---|---|---|---|
| LDL | 0.61 (0.46, 0.80) 0.0005 | 0.67 (0.50, 0.88) 0.0048 | 0.69 (0.53, 0.91) 0.0085 |
| LDL tertiles | |||
| Low | Ref | Ref | Ref |
| Middle | 0.38 (0.23, 0.63) 0.0002 | 0.42 (0.25, 0.69) 0.0007 | 0.48 (0.29, 0.81) 0.0058 |
| High | 0.48 (0.30, 0.77) 0.0022 | 0.57 (0.35, 0.91) 0.0192 | 0.61 (0.37, 0.99) 0.0434 |
| p for trend | 0.0012 | 0.01 | 0.0263 |
| Outcome | HR (95%CI), p-Value |
|---|---|
| Fitting model by stand linear regression | 0.69 (0.53, 0.91), 0.0085 |
| Fitting model by two-piecewise linear regression | |
| Inflection point | 2.31 mmol/L |
| <2.31 mmol/L | 0.42 (0.25, 0.69), 0.0006 |
| >2.31 mmol/L | 1.06 (0.70, 1.63), 0.7722 |
| p for log-likelihood ratio test | 0.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, X.; Tian, B.; Zhao, Z.-D.; Zhang, B.-F.; Zhang, M. Evaluation of the Association between Low-Density Lipoprotein (LDL) and All-Cause Mortality in Geriatric Patients with Hip Fractures: A Prospective Cohort Study of 339 Patients. J. Pers. Med. 2023, 13, 345. https://doi.org/10.3390/jpm13020345
Kang X, Tian B, Zhao Z-D, Zhang B-F, Zhang M. Evaluation of the Association between Low-Density Lipoprotein (LDL) and All-Cause Mortality in Geriatric Patients with Hip Fractures: A Prospective Cohort Study of 339 Patients. Journal of Personalized Medicine. 2023; 13(2):345. https://doi.org/10.3390/jpm13020345
Chicago/Turabian StyleKang, Xin, Bin Tian, Zan-Dong Zhao, Bin-Fei Zhang, and Ming Zhang. 2023. "Evaluation of the Association between Low-Density Lipoprotein (LDL) and All-Cause Mortality in Geriatric Patients with Hip Fractures: A Prospective Cohort Study of 339 Patients" Journal of Personalized Medicine 13, no. 2: 345. https://doi.org/10.3390/jpm13020345
APA StyleKang, X., Tian, B., Zhao, Z.-D., Zhang, B.-F., & Zhang, M. (2023). Evaluation of the Association between Low-Density Lipoprotein (LDL) and All-Cause Mortality in Geriatric Patients with Hip Fractures: A Prospective Cohort Study of 339 Patients. Journal of Personalized Medicine, 13(2), 345. https://doi.org/10.3390/jpm13020345







