Could Mid- to Late-Onset Glaucoma Be Associated with an Increased Risk of Incident Dementia? A Nationwide Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Database
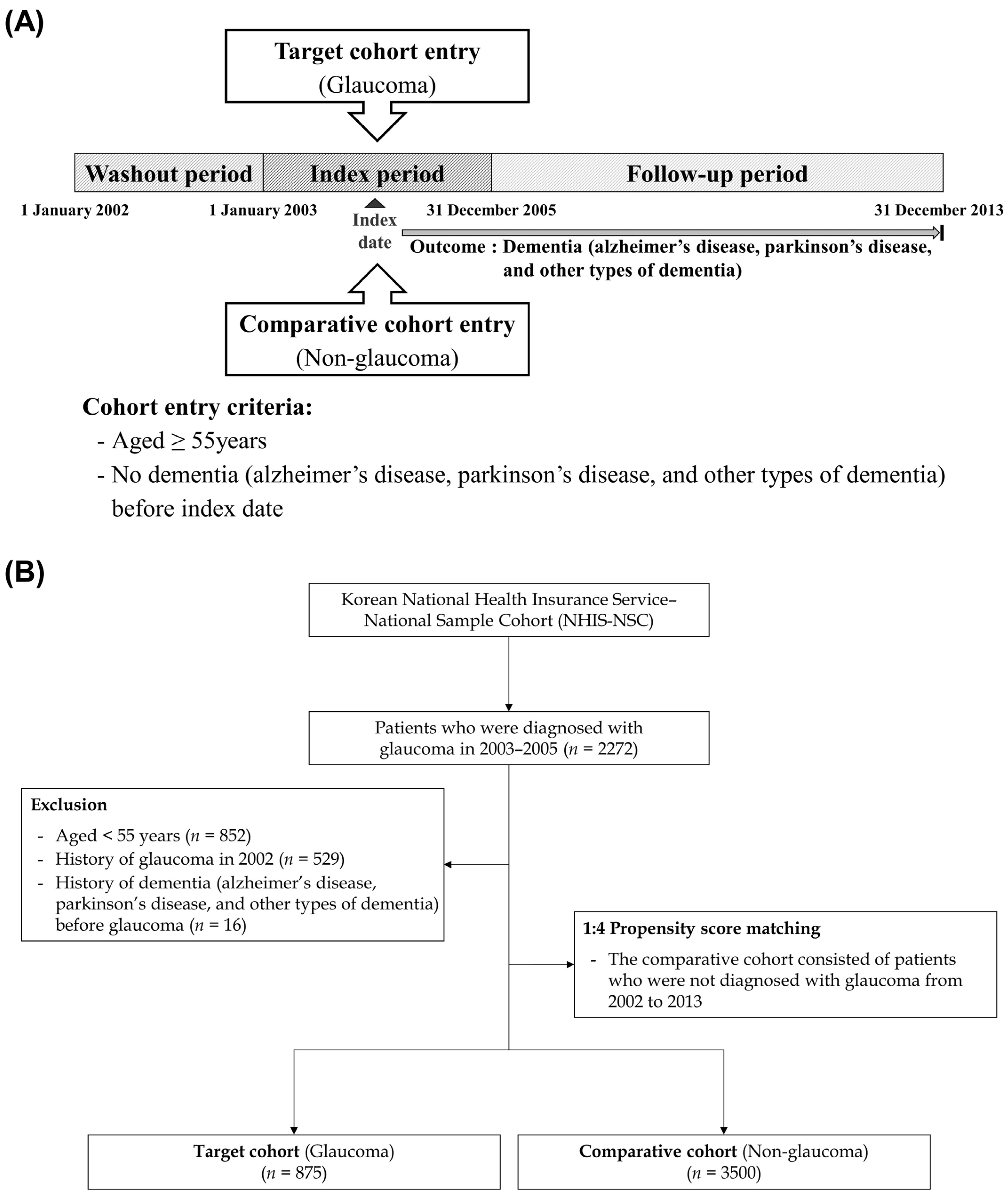
2.2. Study Design
2.3. Statistical Analysis
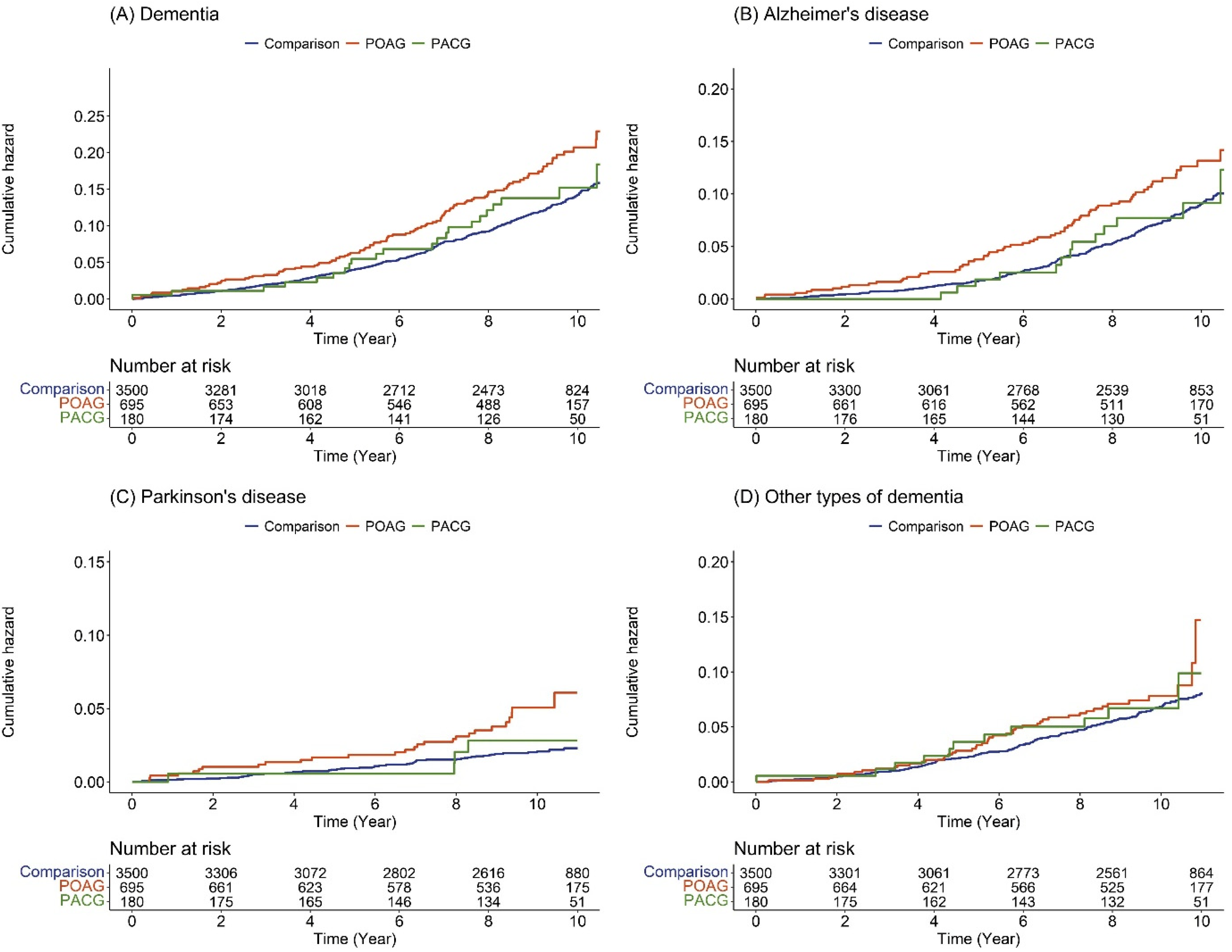
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Quigley, H.A. Glaucoma. Lancet 2011, 377, 1367–1377. [Google Scholar] [CrossRef]
- Cedrone, C.; Mancino, R.; Cerulli, A.; Cesareo, M.; Nucci, C. Epidemiology of primary glaucoma: Prevalence, incidence, and blinding effects. Prog. Brain Res. 2008, 173, 3–14. [Google Scholar] [CrossRef]
- Jiang, T.; Sun, Q.; Chen, S. Oxidative stress: A major pathogenesis and potential therapeutic target of antioxidative agents in Parkinson’s disease and Alzheimer’s disease. Prog. Neurobiol. 2016, 147, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Villemagne, V.L.; Burnham, S.; Bourgeat, P.; Brown, B.; Ellis, K.A.; Salvado, O.; Szoeke, C.; Macaulay, S.L.; Martins, R.; Maruff, P.; et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: A prospective cohort study. Lancet Neurol. 2013, 12, 357–367. [Google Scholar] [CrossRef]
- Lin, I.-C.; Wang, Y.-H.; Wang, T.-J.; Wang, I.-J.; Shen, Y.-D.; Chi, N.-F.; Chien, L.-N. Glaucoma, Alzheimer’s Disease, and Parkinson’s Disease: An 8-Year Population-Based Follow-Up Study. PLoS ONE 2014, 9, e108938. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.-D.; Ho, J.-D.; Chen, C.-H.; Lin, H.-C.; Tsai, M.-C.; Sheu, J.-J. Dementia is associated with open-angle glaucoma: A population-based study. Eye 2015, 29, 1340–1346. [Google Scholar] [CrossRef]
- Moon, J.Y.; Kim, H.J.; Park, Y.H.; Park, T.K.; Park, E.-C.; Kim, C.Y.; Lee, S.H. Association between Open-Angle Glaucoma and the Risks of Alzheimer’s and Parkinson’s Diseases in South Korea: A 10-year Nationwide Cohort Study. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Ou, Y.; Grossman, D.S.; Lee, P.; Sloan, F.A. Glaucoma, Alzheimer Disease and Other Dementia: A Longitudinal Analysis. Ophthalmic Epidemiol. 2012, 19, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Kessing, L.V.; Lopez, A.G.; Andersen, P.K.; Kessing, S.V. No Increased Risk of Developing Alzheimer Disease in Patients with Glaucoma. Eur. J. Gastroenterol. Hepatol. 2007, 16, 47–51. [Google Scholar] [CrossRef]
- Boland, M.V.; Quigley, H.A. Risk Factors and Open-angle Glaucoma: Classification and Application. Eur. J. Gastroenterol. Hepatol. 2007, 16, 406–418. [Google Scholar] [CrossRef]
- Berdahl, J.P.; Fautsch, M.P.; Stinnett, S.S.; Allingham, R.R. Intracranial Pressure in Primary Open Angle Glaucoma, Normal Tension Glaucoma, and Ocular Hypertension: A Case–Control Study. Investig. Ophthalmol. Vis. Sci. 2008, 49, 5412–5418. [Google Scholar] [CrossRef]
- Fleischman, D.; Berdahl, J.; Stinnett, S.S.; Fautsch, M.P.; Allingham, R.R. Cerebrospinal fluid pressure trends in diseases associated with primary open-angle glaucoma. Acta Ophthalmol. 2015, 93, e234–e236. [Google Scholar] [CrossRef]
- Yoneda, S.; Hara, H.; Hirata, A.; Fukushima, M.; Inomata, Y.; Tanihara, H. Vitreous fluid levels of β-amyloid(1–42) and tau in patients with retinal diseases. Jpn. J. Ophthalmol. 2005, 49, 106–108. [Google Scholar] [CrossRef]
- Gupta, N.; Fong, J.; Ang, L.C.; Yücel, Y.H. Retinal tau pathology in human glaucomas. Can. J. Ophthalmol. 2008, 43, 53–60. [Google Scholar] [CrossRef]
- Chiasseu, M.; Vargas, J.L.C.; Destroismaisons, L.; Velde, C.V.; Leclerc, N.; Di Polo, A. Tau Accumulation, Altered Phosphorylation, and Missorting Promote Neurodegeneration in Glaucoma. J. Neurosci. 2016, 36, 5785–5798. [Google Scholar] [CrossRef]
- Aref, A.A.; Jain, S.K.A. Senile dementia and glaucoma: Evidence for a common link. J. Ophthalmic Vis. Res. 2015, 10, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Costa, V.P.; Harris, A.; Anderson, D.; Stodtmeister, R.; Cremasco, F.; Kergoat, H.; Lovasik, J.; Stalmans, I.; Zeitz, O.; Lanzl, I.; et al. Ocular perfusion pressure in glaucoma. Acta Ophthalmol. 2014, 92, e252–e266. [Google Scholar] [CrossRef] [PubMed]
- Chow, N.; Bell, R.D.; Deane, R.; Streb, J.W.; Chen, J.; Brooks, A.; Van Nostrand, W.; Miano, J.M.; Zlokovic, B.V. Serum response factor and myocardin mediate arterial hypercontractility and cerebral blood flow dysregulation in Alzheimer’s phenotype. Proc. Natl. Acad. Sci. USA 2007, 104, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.; E Matthews, F.; E Barnes, D.; Yaffe, K.; Brayne, C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 2014, 13, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.H.; Yu, H.; Ha, S.-S.; Son, G.M.; Park, K.J.; Lee, J.J.; Kim, D.-K. Association between Late-Onset Ménière’s Disease and the Risk of Incident All-Cause Dementia. J. Pers. Med. 2021, 12, 19. [Google Scholar] [CrossRef]
- Kwon, Y.-S.; Lee, J.-J.; Lee, S.-H.; Kim, C.; Yu, H.; Sohn, J.-H.; Kim, D.-K. Risk of Dementia in Patients Who Underwent Surgery under Neuraxial Anesthesia: A Nationwide Cohort Study. J. Pers. Med. 2021, 11, 1386. [Google Scholar] [CrossRef] [PubMed]
- Aptel, F.; Chiquet, C.; Tamisier, R.; Sapene, M.; Martin, F.; Stach, B.; Grillet, Y.; Levy, P.; Pépin, J.-L. Association between glaucoma and sleep apnea in a large French multicenter prospective cohort. Sleep Med. 2014, 15, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Bayer, A.U.; Keller, O.N.; Ferrari, F.; Maag, K.-P. Association of glaucoma with neurodegenerative diseases with apoptotic cell death: Alzheimer’s disease and Parkinson’s disease. Am. J. Ophthalmol. 2002, 133, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Yenice, O.; Onal, S.; Midi, I.; Ozcan, E.; Temel, A.; I-Gunal, D. Visual field analysis in patients with Parkinson’s disease. Park. Relat. Disord. 2008, 14, 193–198. [Google Scholar] [CrossRef]
- Altintas, O.; Işeri, P.; Özkan, B.; Çağlar, Y. Correlation between retinal morphological and functional findings and clinical severity in Parkinson’s disease. Doc. Ophthalmol. 2008, 116, 137–146. [Google Scholar] [CrossRef]
- Moschos, M.M.; Tagaris, G.; Markopoulos, L.; Margetis, L.; Tsapakis, S.; Kanakis, M.; Koutsandrea, C. Morphologic Changes and Functional Retinal Impairment in Patients with Parkinson Disease without Visual Loss. Eur. J. Ophthalmol. 2010, 21, 24–29. [Google Scholar] [CrossRef]
- Lowe, R.F. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br. J. Ophthalmol. 1970, 54, 161–169. [Google Scholar] [CrossRef]
- Sihota, R.; Ghate, D.; Mohan, S.; Gupta, V.; Pandey, R.M.; Dada, T. Study of biometric parameters in family members of primary angle closure glaucoma patients. Eye 2008, 22, 521–527. [Google Scholar] [CrossRef]
- Lee, S.; Cha, J.; Kim, J.-Y.; Son, G.M.; Kim, D.-K. Detection of unknown ototoxic adverse drug reactions: An electronic healthcare record-based longitudinal nationwide cohort analysis. Sci. Rep. 2021, 11, 14045. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.-H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Leuk. Res. 2016, 46, dyv319. [Google Scholar] [CrossRef]
- You, S.C.; Lee, S.; Cho, S.-Y.; Park, H.; Jung, S.; Cho, J.; Yoon, D.; Park, R.W. Conversion of National Health Insurance Service-National Sample Cohort (NHIS-NSC) Database into Observational Medical Outcomes Partnership-Common Data Model (OMOP-CDM). Stud. Health Technol. Inform. 2017, 245, 467–470. [Google Scholar] [CrossRef] [PubMed]
| Variables | Comparison (n = 3500) | Glaucoma (n = 875) | p-Value |
|---|---|---|---|
| Sex | 1.000 | ||
| Male | 1572 (44.9%) | 393 (44.9%) | |
| Female | 1928 (55.1%) | 482 (55.1%) | |
| Ages (years) | 1.000 | ||
| 55–64 | 1424 (40.7%) | 356 (40.7%) | |
| ≥65 | 2076 (59.3%) | 519 (59.3%) | |
| Residence | 1.000 | ||
| Seoul | 724 (20.7%) | 181 (20.7%) | |
| Second area | 820 (23.4%) | 205 (23.4%) | |
| Third area | 1956 (55.9%) | 489 (55.9%) | |
| Household income | 1.000 | ||
| Low (0–30%) | 704 (20.1%) | 176 (20.1%) | |
| Middle (30–70%) | 1172 (33.5%) | 293 (33.5%) | |
| High (70–100%) | 1624 (46.4%) | 406 (46.4%) | |
| CCI | 1.000 | ||
| 0 | 1660 (47.4%) | 415 (47.4%) | |
| 1 | 900 (25.7%) | 225 (25.7%) | |
| ≥2 | 940 (26.9%) | 235 (26.9%) |
| Variables | N | Case | Person Year | Incidence |
|---|---|---|---|---|
| Dementia | ||||
| Comparison | 3500 | 393 | 28,935.3 | 13.58 |
| Glaucoma | 875 | 131 | 7014.7 | 18.67 |
| Alzheimer’s disease | ||||
| Comparison | 3500 | 251 | 29,411.2 | 8.53 |
| Glaucoma | 875 | 85 | 7175.5 | 11.85 |
| Parkinson’s disease | ||||
| Comparison | 3500 | 61 | 29,776.4 | 2.05 |
| Glaucoma | 875 | 31 | 7294.7 | 4.25 |
| Other types of dementia | ||||
| Comparison | 3500 | 194 | 29,504.8 | 6.58 |
| Glaucoma | 875 | 57 | 7231.1 | 7.88 |
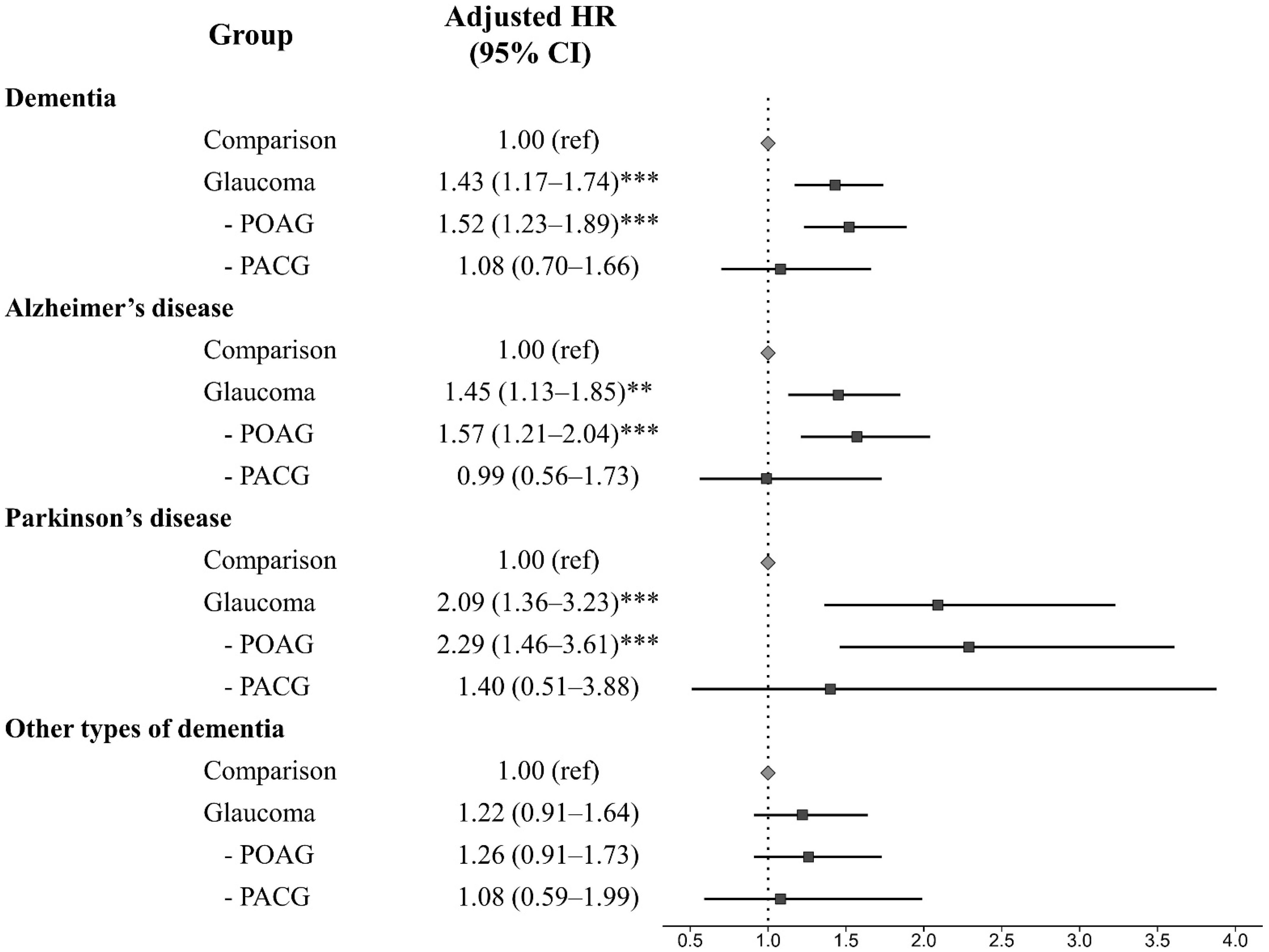
| Variables | N | Case | Unadjusted HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|
| Comparison | 3500 | 393 | 1.00 (ref) | 1.00 (ref) |
| Glaucoma | 875 | 131 | 1.44 (1.18–1.75) *** | 1.43 (1.17–1.74) *** |
| POAG | 695 | 109 | 1.52 (1.23–1.88) *** | 1.52 (1.23–1.89) *** |
| PACG | 180 | 22 | 1.13 (0.74–1.74) | 1.08 (0.70–1.66) |
| Time (Year) | Dementia | Alzheimer’s Disease | Parkinson’s Disease | Other Types of Dementia | ||||
|---|---|---|---|---|---|---|---|---|
| No. of Event | Adjusted HR (95% CI) | No. of Event | Adjusted HR (95% CI) | No. of Event | Adjusted HR (95% CI) | No. of Event | Adjusted HR (95% CI) | |
| 1 | 7 | 2.03 (0.84–4.90) | 4 | 4.07 (1.09–15.19) * | 3 | 2.88 (0.69–12.07) | 1 | 0.64 (0.08–5.11) |
| 2 | 16 | 2.16 (1.20–3.89) * | 8 | 2.69 (1.14–6.36) * | 7 | 4.29 (1.55–11.84) ** | 4 | 1.26 (0.42–3.76) |
| 3 | 22 | 1.69 (1.04–2.75) * | 11 | 2.25 (1.10–4.57) * | 7 | 1.99 (0.83–4.81) | 8 | 1.36 (0.62–2.99) |
| 4 | 29 | 1.55 (1.02–2.36) * | 17 | 2.20 (1.25–3.90) ** | 9 | 2.01 (0.92–4.37) | 11 | 1.22 (0.63–2.37) |
| 5 | 40 | 1.58 (1.11–2.25) * | 24 | 2.19 (1.36–3.55) ** | 11 | 2.03 (1.00–4.09) * | 18 | 1.31 (0.78–2.20) |
| 6 | 54 | 1.63 (1.20–2.21) ** | 33 | 2.05 (1.37–3.08) *** | 12 | 1.73 (0.90–3.35) | 26 | 1.52 (0.98–2.36) |
| 7 | 68 | 1.50 (1.14–1.97) ** | 41 | 1.70 (1.19–2.42) ** | 15 | 1.74 (0.96–3.14) | 32 | 1.36 (0.92–2.01) |
| 8 | 84 | 1.59 (1.24–2.03) *** | 53 | 1.74 (1.27–2.38) *** | 19 | 2.00 (1.17–3.42) * | 37 | 1.33 (0.92–1.91) |
| 9 | 94 | 1.48 (1.18–1.86) *** | 62 | 1.60 (1.20–2.12) ** | 22 | 1.95 (1.19–3.20) ** | 41 | 1.25 (0.89–1.76) |
| 10 | 103 | 1.49 (1.19–1.85) *** | 67 | 1.52 (1.16–2.00) ** | 26 | 2.25 (1.42–3.57) *** | 43 | 1.20 (0.86–1.68) |
| 11 | 109 | 1.52 (1.23–1.89) *** | 72 | 1.57 (1.21–2.04) *** | 27 | 2.29 (1.46–3.61) *** | 46 | 1.26 (0.91–1.73) |
| Sex | Male | Female | ||
|---|---|---|---|---|
| Comparison | POAG | Comparison | POAG | |
| Alzheimer’s disease | ||||
| Unadjusted HR (95% CI) | 1.00 (ref) | 1.31 (0.92–1.85) | 1.00 (ref) | 2.18 (1.45–3.27) *** |
| Adjusted HR (95% CI) | 1.00 (ref) | 1.27 (0.90–1.81) | 1.00 (ref) | 2.16 (1.43–3.24) *** |
| Parkinson’s disease | ||||
| Unadjusted HR (95% CI) | 1.00 (ref) | 3.01 (1.70–5.36) *** | 1.00 (ref) | 1.57 (0.74–3.33) |
| Adjusted HR (95% CI) | 1.00 (ref) | 2.94 (1.65–5.23) *** | 1.00 (ref) | 1.57 (0.74–3.33) |
| CCI | 0 | 1 | ≥2 | |||
|---|---|---|---|---|---|---|
| Comparison | POAG | Comparison | POAG | Comparison | POAG | |
| Alzheimer’s disease | ||||||
| Unadjusted HR (95% CI) | 1.00 (ref) | 1.51 (0.88–2.60) | 1.00 (ref) | 1.87 (1.12–3.10) * | 1.00 (ref) | 1.49 (1.03–2.17) * |
| Adjusted HR (95% CI) | 1.00 (ref) | 1.52 (0.88–2.61) | 1.00 (ref) | 1.84 (1.11–3.05) * | 1.00 (ref) | 1.47 (1.01–2.14) * |
| Parkinson’s disease | ||||||
| Unadjusted HR (95% CI) | 1.00 (ref) | 1.43 (0.57–3.57) | 1.00 (ref) | 1.78 (0.70–4.48) | 1.00 (ref) | 3.52 (1.84–6.77) *** |
| Adjusted HR (95% CI) | 1.00 (ref) | 1.41 (0.57–3.53) | 1.00 (ref) | 1.75 (0.69–4.43) | 1.00 (ref) | 3.48 (1.81–6.69) *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.-K.; Lee, S.Y. Could Mid- to Late-Onset Glaucoma Be Associated with an Increased Risk of Incident Dementia? A Nationwide Retrospective Cohort Study. J. Pers. Med. 2023, 13, 214. https://doi.org/10.3390/jpm13020214
Kim D-K, Lee SY. Could Mid- to Late-Onset Glaucoma Be Associated with an Increased Risk of Incident Dementia? A Nationwide Retrospective Cohort Study. Journal of Personalized Medicine. 2023; 13(2):214. https://doi.org/10.3390/jpm13020214
Chicago/Turabian StyleKim, Dong-Kyu, and So Yeon Lee. 2023. "Could Mid- to Late-Onset Glaucoma Be Associated with an Increased Risk of Incident Dementia? A Nationwide Retrospective Cohort Study" Journal of Personalized Medicine 13, no. 2: 214. https://doi.org/10.3390/jpm13020214
APA StyleKim, D.-K., & Lee, S. Y. (2023). Could Mid- to Late-Onset Glaucoma Be Associated with an Increased Risk of Incident Dementia? A Nationwide Retrospective Cohort Study. Journal of Personalized Medicine, 13(2), 214. https://doi.org/10.3390/jpm13020214







