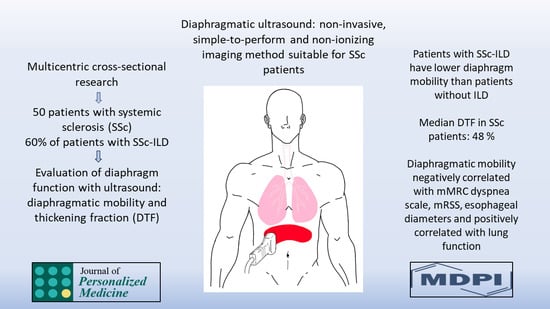
Ultrasonic Evaluation of Diaphragm in Patients with Systemic Sclerosis
Abstract
:1. Introduction
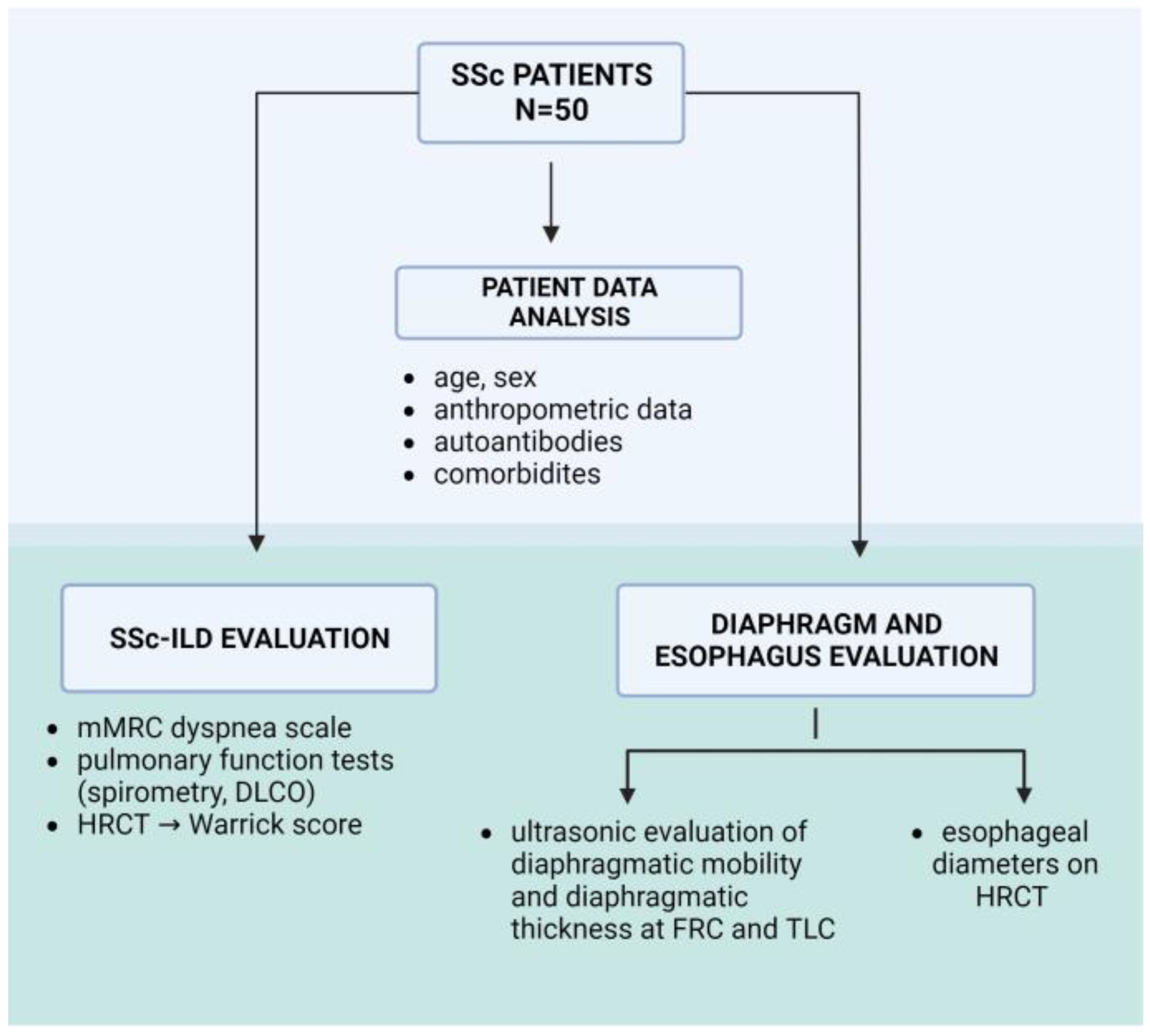
2. Materials and Methods
2.1. Study Design
2.2. Patient Characteristics
2.3. Evaluation of Lung Disease
2.4. Evaluation of the Diaphragm
2.5. Evaluation of the Esophagus
2.6. Sample Size Calculation
2.7. Statistical Methods
3. Results
3.1. Patients and Characteristics
3.2. Results of Ultrasonic Diaphragmatic Assessment
3.3. Correlations of Diaphragmatic Mobility with other Evaluated Clinical Parameters
3.4. Factors Predicting SSc-ILD
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonella, F.; Patuzzo, G.; Lunardi, C. Biomarker Discovery in Systemic Sclerosis: State of the Art. CBF 2015, 5, 47–68. [Google Scholar] [CrossRef]
- Li, B.; Yan, J.; Pu, J.; Tang, J.; Xu, S.; Wang, X. Esophageal Dysfunction in Systemic Sclerosis: An Update. Rheumatol. Ther. 2021, 8, 1535–1549. [Google Scholar] [CrossRef] [PubMed]
- van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A.; Carreira, P.E.; et al. 2013 Classification Criteria for Systemic Sclerosis: An American College of Rheumatology/European League against Rheumatism Collaborative Initiative. Ann. Rheum. Dis. 2013, 72, 1747–1755. [Google Scholar] [CrossRef] [PubMed]
- Wells, A.U.; Margaritopoulos, G.A.; Antoniou, K.M.; Denton, C. Interstitial Lung Disease in Systemic Sclerosis. Semin. Respir. Crit. Care Med. 2014, 35, 213–221. [Google Scholar] [CrossRef]
- Solomon, J.J.; Olson, A.L.; Fischer, A.; Bull, T.; Brown, K.K.; Raghu, G. Scleroderma Lung Disease. Eur. Respir. Rev. 2013, 22, 6–19. [Google Scholar] [CrossRef]
- Perelas, A.; Silver, R.M.; Arrossi, A.V.; Highland, K.B. Systemic Sclerosis-Associated Interstitial Lung Disease. Lancet Respir. Med. 2020, 8, 304–320. [Google Scholar] [CrossRef]
- Bruni, C.; Chung, L.; Hoffmann-Vold, A.M.; Assassi, S.; Gabrielli, A.; Khanna, D.; Bernstein, E.J.; Distler, O. EUSTAR and SCTC collaborators High-Resolution Computed Tomography of the Chest for the Screening, Re-Screening and Follow-up of Systemic Sclerosis-Associated Interstitial Lung Disease: A EUSTAR-SCTC Survey. Clin. Exp. Rheumatol. 2022, 40, 1951–1955. [Google Scholar] [CrossRef]
- Warrick, J.H.; Bhalla, M.; Schabel, S.I.; Silver, R.M. High Resolution Computed Tomography in Early Scleroderma Lung Disease. J. Rheumatol. 1991, 18, 1520–1528. [Google Scholar]
- Savarino, E.; Bazzica, M.; Zentilin, P.; Pohl, D.; Parodi, A.; Cittadini, G.; Negrini, S.; Indiveri, F.; Tutuian, R.; Savarino, V.; et al. Gastroesophageal Reflux and Pulmonary Fibrosis in Scleroderma: A Study Using pH-Impedance Monitoring. Am. J. Respir. Crit. Care Med. 2009, 179, 408–413. [Google Scholar] [CrossRef]
- Diot, E.; Boissinot, E.; Asquier, E.; Guilmot, J.L.; Lemarié, E.; Valat, C.; Diot, P. Relationship between Abnormalities on High-Resolution CT and Pulmonary Function in Systemic Sclerosis. Chest 1998, 114, 1623–1629. [Google Scholar] [CrossRef]
- Salaffi, F.; Di Carlo, M.; Carotti, M.; Fraticelli, P.; Gabrielli, A.; Giovagnoni, A. Relationship between Interstitial Lung Disease and Oesophageal Dilatation on Chest High-Resolution Computed Tomography in Patients with Systemic Sclerosis: A Cross-Sectional Study. Radiol. Med. 2018, 123, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Sexton, W.L.; Farkas, G.A.; Powers, S.K.; Reid, M.B. Diaphragm Structure and Function in Health and Disease. Med. Sci. Sports Exerc. 1997, 29, 738–754. [Google Scholar] [CrossRef] [PubMed]
- de Troyer, A.; Loring, S.H. Action of the Respiratory Muscles. In Comprehensive Physiology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011; pp. 443–461. ISBN 978-0-470-65071-4. [Google Scholar]
- Pickering, M.; Jones, J.F.X. The Diaphragm: Two Physiological Muscles in One. J. Anat. 2002, 201, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Mittal, R.K.; Rochester, D.F.; McCallum, R.W. Electrical and Mechanical Activity in the Human Lower Esophageal Sphincter during Diaphragmatic Contraction. J. Clin. Investig. 1988, 81, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.J.; Bowen, T.S. Respiratory Muscle Weakness in Patients with Heart Failure: Time to Make It a Standard Clinical Marker and a Need for Novel Therapeutic Interventions? J. Card. Fail. 2018, 24, 217–218. [Google Scholar] [CrossRef]
- Ottenheijm, C.A.C.; Heunks, L.M.A.; Sieck, G.C.; Zhan, W.-Z.; Jansen, S.M.; Degens, H.; De Boo, T.; Dekhuijzen, P.N.R. Diaphragm Dysfunction in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2005, 172, 200–205. [Google Scholar] [CrossRef]
- Kelley, R.C.; Ferreira, L.F. Diaphragm Abnormalities in Heart Failure and Aging: Mechanisms and Integration of Cardiovascular and Respiratory Pathophysiology. Heart Fail. Rev. 2017, 22, 191–207. [Google Scholar] [CrossRef]
- Summerhill, E.M.; El-Sameed, Y.A.; Glidden, T.J.; McCool, F.D. Monitoring Recovery from Diaphragm Paralysis with Ultrasound. Chest 2008, 133, 737–743. [Google Scholar] [CrossRef]
- Flores-Franco, R.A.; Castillo-Soltero, J.; Pacheco-Tena, C.F. Diaphragmatic Paralysis in Eosinophilic Granulomatosis with Polyangiitis. Reumatol. Clin. 2018, 14, 61–62. [Google Scholar] [CrossRef]
- Maish, M.S. The Diaphragm. Surg. Clin. North Am. 2010, 90, 955–968. [Google Scholar] [CrossRef]
- Laroche, C.M.; Mier, A.K.; Moxham, J.; Green, M. Diaphragm Strength in Patients with Recent Hemidiaphragm Paralysis. Thorax 1988, 43, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Boussuges, A.; Rives, S.; Finance, J.; Brégeon, F. Assessment of Diaphragmatic Function by Ultrasonography: Current Approach and Perspectives. World J. Clin. Cases 2020, 8, 2408–2424. [Google Scholar] [CrossRef] [PubMed]
- Laursen, C.B.; Clive, A.; Hallifax, R.; Pietersen, P.I.; Asciak, R.; Davidsen, J.R.; Bhatnagar, R.; Bedawi, E.O.; Jacobsen, N.; Coleman, C.; et al. European Respiratory Society Statement on Thoracic Ultrasound. Eur. Respir. J. 2021, 57, 2001519. [Google Scholar] [CrossRef] [PubMed]
- Tuinman, P.R.; Jonkman, A.H.; Dres, M.; Shi, Z.-H.; Goligher, E.C.; Goffi, A.; de Korte, C.; Demoule, A.; Heunks, L. Respiratory Muscle Ultrasonography: Methodology, Basic and Advanced Principles and Clinical Applications in ICU and ED Patients-a Narrative Review. Intensive Care Med. 2020, 46, 594–605. [Google Scholar] [CrossRef]
- Spiesshoefer, J.; Herkenrath, S.; Henke, C.; Langenbruch, L.; Schneppe, M.; Randerath, W.; Young, P.; Brix, T.; Boentert, M. Evaluation of Respiratory Muscle Strength and Diaphragm Ultrasound: Normative Values, Theoretical Considerations, and Practical Recommendations. Respiration 2020, 99, 369–381. [Google Scholar] [CrossRef]
- Ferrari, G.; De Filippi, G.; Elia, F.; Panero, F.; Volpicelli, G.; Aprà, F. Diaphragm Ultrasound as a New Index of Discontinuation from Mechanical Ventilation. Crit. Ultrasound J. 2014, 6, 8. [Google Scholar] [CrossRef]
- Shand, L.; Lunt, M.; Nihtyanova, S.; Hoseini, M.; Silman, A.; Black, C.M.; Denton, C.P. Relationship between Change in Skin Score and Disease Outcome in Diffuse Cutaneous Systemic Sclerosis: Application of a Latent Linear Trajectory Model. Arthritis Rheum. 2007, 56, 2422–2431. [Google Scholar] [CrossRef]
- Richardson, C.; Agrawal, R.; Lee, J.; Almagor, O.; Nelson, R.; Varga, J.; Cuttica, M.J.; Dematte, J.D.A.; Chang, R.W.; Hinchcliff, M.E. Esophageal Dilatation and Interstitial Lung Disease in Systemic Sclerosis: A Cross-Sectional Study. Semin. Arthritis Rheum. 2016, 46, 109–114. [Google Scholar] [CrossRef]
- Khanna, D.; Furst, D.E.; Clements, P.J.; Allanore, Y.; Baron, M.; Czirjak, L.; Distler, O.; Foeldvari, I.; Kuwana, M.; Matucci-Cerinic, M.; et al. Standardization of the Modified Rodnan Skin Score for Use in Clinical Trials of Systemic Sclerosis. J. Scleroderma Relat. Disord. 2017, 2, 11–18. [Google Scholar] [CrossRef]
- Showalter, K.; Merkel, P.A.; Khanna, D.; Gordon, J.K. Assessment of Skin Disease in Scleroderma: Practices and Opinions of Investigators Studying Scleroderma. J. Scleroderma Relat. Disord. 2020, 5, 167–171. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.L.; Brusasco, V.; Burgos, F.; Cooper, B.G.; Jensen, R.; Kendrick, A.; MacIntyre, N.R.; Thompson, B.R.; Wanger, J. 2017 ERS/ATS Standards for Single-Breath Carbon Monoxide Uptake in the Lung. Eur. Respir. J. 2017, 49, 1600016. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lian, X.; Huang, S.; Li, L.; Zhao, Y.; Lai, H.; Lyu, G. A Study of the Diagnostic Value of a Modified Transthoracic Lung Ultrasound Scoring Method in Interstitial Lung Disease. Quant. Imaging Med. Surg. 2023, 13, 946–956. [Google Scholar] [CrossRef] [PubMed]
- Bestall, J.C.; Paul, E.A.; Garrod, R.; Garnham, R.; Jones, P.W.; Wedzicha, J.A. Usefulness of the Medical Research Council (MRC) Dyspnoea Scale as a Measure of Disability in Patients with Chronic Obstructive Pulmonary Disease. Thorax 1999, 54, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Sethi, D.K.; Rhodes, J.; Ferris, R.; Banka, R.; Clarke, A.; Mishra, E.K. Breathlessness Predicts Mortality in Adults: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e39192. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; Wells, C.K. Evaluation of Clinical Methods for Rating Dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Qu, Q.; Deng, P.; Zhao, Y.; Liu, C.; Fu, C.; Jia, J. Assessment of Diaphragm in Hemiplegic Patients after Stroke with Ultrasound and Its Correlation of Extremity Motor and Balance Function. Brain Sci. 2022, 12, 882. [Google Scholar] [CrossRef]
- Kantarci, F.; Mihmanli, I.; Demirel, M.K.; Harmanci, K.; Akman, C.; Aydogan, F.; Mihmanli, A.; Uysal, O. Normal Diaphragmatic Motion and the Effects of Body Composition: Determination with M-Mode Sonography. J. Ultrasound Med. 2004, 23, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Boon, A.J.; Harper, C.J.; Ghahfarokhi, L.S.; Strommen, J.A.; Watson, J.C.; Sorenson, E.J. Two-Dimensional Ultrasound Imaging of the Diaphragm: Quantitative Values in Normal Subjects. Muscle Nerve 2013, 47, 884–889. [Google Scholar] [CrossRef]
- Santana, P.V.; Cardenas, L.Z.; de Albuquerque, A.L.P.; de Carvalho, C.R.R.; Caruso, P. Diaphragmatic Ultrasound: A Review of Its Methodological Aspects and Clinical Uses. J. Bras. Pneumol. 2020, 46, e20200064. [Google Scholar] [CrossRef]
- Vivier, E.; Mekontso Dessap, A.; Dimassi, S.; Vargas, F.; Lyazidi, A.; Thille, A.W.; Brochard, L. Diaphragm Ultrasonography to Estimate the Work of Breathing during Non-Invasive Ventilation. Intensive Care Med. 2012, 38, 796–803. [Google Scholar] [CrossRef]
- Gottesman, E.; McCool, F.D. Ultrasound Evaluation of the Paralyzed Diaphragm. Am. J. Respir. Crit. Care Med. 1997, 155, 1570–1574. [Google Scholar] [CrossRef]
- Boussuges, A.; Gole, Y.; Blanc, P. Diaphragmatic Motion Studied by M-Mode Ultrasonography: Methods, Reproducibility, and Normal Values. Chest 2009, 135, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Santana, P.V.; Prina, E.; Albuquerque, A.L.P.; Carvalho, C.R.R.; Caruso, P. Identifying Decreased Diaphragmatic Mobility and Diaphragm Thickening in Interstitial Lung Disease: The Utility of Ultrasound Imaging. J. Bras. Pneumol. 2016, 42, 88–94. [Google Scholar] [CrossRef] [PubMed]
- McCool, F.D.; Tzelepis, G.E. Dysfunction of the Diaphragm. N. Engl. J. Med. 2012, 366, 932–942. [Google Scholar] [CrossRef] [PubMed]
- Santana, P.V.; Cardenas, L.Z.; de Albuquerque, A.L.P.; de Carvalho, C.R.R.; Caruso, P. Diaphragmatic Ultrasound Findings Correlate with Dyspnea, Exercise Tolerance, Health-Related Quality of Life and Lung Function in Patients with Fibrotic Interstitial Lung Disease. BMC Pulm. Med. 2019, 19, 183. [Google Scholar] [CrossRef] [PubMed]
- Leelarungrayub, J.; Pinkaew, D.; Wonglangka, K.; Eungpinichpong, W.; Klaphajone, J. Short-Term Pulmonary Rehabilitation for a Female Patient with Chronic Scleroderma under a Single-Case Research Design. Clin. Med. Insights Circ. Respir. Pulm. Med. 2016, 10, 11–17. [Google Scholar] [CrossRef]
- Pehlivan, E.; Mutluay, F.; Balcı, A.; Kılıç, L. The Effects of Inspiratory Muscle Training on Exercise Capacity, Dyspnea and Respiratory Functions in Lung Transplantation Candidates: A Randomized Controlled Trial. Clin. Rehabil. 2018, 32, 1328–1339. [Google Scholar] [CrossRef]
- Faverzani, S.; Nocera, F.; Crisafulli, E.; Marvisi, M.; Becciolini, A.; Mosetti, F.; Di Donato, E.; Mozzani, F.; Santilli, D.; Scopelliti, G.; et al. Home-Based Unsupervised Pulmonary Rehabilitation Program Improves the Respiratory Disability in Systemic Sclerosis Patients with Dyspnea: An Observational Prospective Study. Monaldi. Arch. Chest. Dis. 2021, 92, 3. [Google Scholar] [CrossRef]
- Greising, S.M.; Ottenheijm, C.A.C.; O’Halloran, K.D.; Barreiro, E. Diaphragm Plasticity in Aging and Disease: Therapies for Muscle Weakness Go from Strength to Strength. J. Appl. Physiol. 2018, 125, 243–253. [Google Scholar] [CrossRef]
- Rivet, V.; Riviere, S.; Goulabchand, R.; Suzon, B.; Henneton, P.; Partouche, L.; Rullier, P.; Quellec, A.L.; Konate, A.; Schiffmann, A.; et al. High Prevalence of Malnutrition in Systemic Sclerosis: Results from a French Monocentric Cross-Sectional Study. Nutrition 2023, 112171. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM Criteria for the Diagnosis of Malnutrition—A Consensus Report from the Global Clinical Nutrition Community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Siegert, E.; March, C.; Otten, L.; Makowka, A.; Preis, E.; Buttgereit, F.; Riemekasten, G.; Müller-Werdan, U.; Norman, K. Prevalence of Sarcopenia in Systemic Sclerosis: Assessing Body Composition and Functional Disability in Patients with Systemic Sclerosis. Nutrition 2018, 55–56, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Schoser, B.; Fong, E.; Geberhiwot, T.; Hughes, D.; Kissel, J.T.; Madathil, S.C.; Orlikowski, D.; Polkey, M.I.; Roberts, M.; Tiddens, H.A.W.M.; et al. Maximum Inspiratory Pressure as a Clinically Meaningful Trial Endpoint for Neuromuscular Diseases: A Comprehensive Review of the Literature. Orphanet J. Rare Dis. 2017, 12, 52. [Google Scholar] [CrossRef]
- Catalá-Ripoll, J.V.; Monsalve-Naharro, J.Á.; Hernández-Fernández, F. Incidence and Predictive Factors of Diaphragmatic Dysfunction in Acute Stroke. BMC Neurol. 2020, 20, 79. [Google Scholar] [CrossRef]
- Smargiassi, A.; Inchingolo, R.; Tagliaboschi, L.; Di Marco Berardino, A.; Valente, S.; Corbo, G.M. Ultrasonographic Assessment of the Diaphragm in Chronic Obstructive Pulmonary Disease Patients: Relationships with Pulmonary Function and the Influence of Body Composition—A Pilot Study. Respiration 2014, 87, 364–371. [Google Scholar] [CrossRef]
- Satış, H.; Cindil, E.; Salman, R.B.; Yapar, D.; Temel, E.; Demir, N.B.; Babaoğlu, H.; Gündoğdu, O.; Ataş, N.; Şendur, H.; et al. Diaphragmatic Muscle Thickness and Diaphragmatic Function Are Reduced in Patients with Systemic Lupus Erythematosus Compared to Those with Primary Sjögren’s Syndrome. Lupus 2020, 29, 715–720. [Google Scholar] [CrossRef]
- Choudhury, S.; Ramos, M.; Anjum, H.; Ali, M.; Surani, S.; Choudhury, S.; Ramos, M.; Anjum, H.; Ali, M.; Surani, S. Shrinking Lung Syndrome: A Rare Manifestation of Systemic Lupus Erythematosus. Cureus 2020, 12, e8216. [Google Scholar] [CrossRef]
- Saragadam, S.D.; Mukkera, S. Atypical Presentation of Mixed Connective Tissue Disorder Involving Bilateral Diaphragm. Cureus 2022, 14, e22154. [Google Scholar] [CrossRef]
- van Doorn, J.L.M.; Wijntjes, J.; Saris, C.G.J.; Ottenheijm, C.A.C.; van Alfen, N.; Doorduin, J. Association of Diaphragm Thickness and Echogenicity with Age, Sex, and Body Mass Index in Healthy Subjects. Muscle Nerve 2022, 66, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Takekoshi, D.; Arami, S.; Sheppard, T.J.; Cole-Saffold, P.; Michel, J.C.; Kondos, G.T.; Schraufnagel, D.E. Computed Tomography of the Esophagus in Scleroderma and Lung Disease. Tohoku J. Exp. Med. 2015, 237, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Heathcote, K.L.; Cockcroft, D.W.; Fladeland, D.A.; Fenton, M.E. Normal Expiratory Flow Rate and Lung Volumes in Patients with Combined Emphysema and Interstitial Lung Disease: A Case Series and Literature Review. Can. Respir. J. 2011, 18, e73–e76. [Google Scholar] [CrossRef]
- Balbir-Gurman, A.; Braun-Moscovici, Y. Scleroderma Overlap Syndrome. Isr. Med. Assoc. J. 2011, 13, 14–20. [Google Scholar]
- Wielosz, E.; Majdan, M.; Dryglewska, M.; Targońska-Stępniak, B. Overlap Syndromes in Systemic Sclerosis. Postepy. Dermatol. Alergol. 2018, 35, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Fairchild, R.; Chung, M.; Yang, D.; Sharpless, L.; Li, S.; Chung, L. Development and Assessment of Novel Lung Ultrasound Interpretation Criteria for the Detection of Interstitial Lung Disease in Systemic Sclerosis. Arthritis Care Res. 2021, 73, 1338–1342. [Google Scholar] [CrossRef]
- Radić, M.; Đogaš, H.; Gelemanović, A.; Jurić Petričević, S.; Škopljanac, I.; Radić, J. Pulmonary Ultrasonography in Systemic Sclerosis-Induced Interstitial Lung Disease—A Systematic Review and Meta-Analysis. Diagnostics 2023, 13, 1429. [Google Scholar] [CrossRef]
| Characteristics of Patients with Systemic Sclerosis | All Patients (N 50) | Patients with Interstitial Lung Disease (N 30) | Patients without Interstitial Lung Disease (N 20) | p Value |
|---|---|---|---|---|
| Age | 63 (54–70) | 64 (54–72) | 60 (46–65) | 0.17 * |
| Gender: Male | 5 (10) | 4 (13) | 1 (5) | 0.64 † |
| Female | 45 (90) | 26 (87) | 19 (95) | |
| Duration of disease, years | 9 (5–17) | 13 (7–22) | 6 (5–10) | 0.01 * |
| BMI | 25.5 (23.2–29.1) | 24.3 (23.1–26.4) | 28.27 (23.2–31.0) | 0.10 * |
| Weight (kg) | 68.5 (60–82.5) | 65.5 (56.8–72.3) | 78 (65–94.25) | 0.05 * |
| Height (cm) | 165 (158–170) | 162 (158–170.3) | 166 (165–170) | 0.09 * |
| Anti-Scl-70 antibodies | 18 (36) | 14 (47) | 4 (20) | 0.07 † |
| Anticentromere antibodies | 16 (32) | 6 (20) | 10 (50) | 0.03 † |
| mRSS | 6.5 (2–13) | 9.5 (1.75–13) | 4 (2–13) | 0.38 * |
| Gastroesophageal symptoms | 41 (82) | 28 (93) | 13 (65) | 0.02 * |
| Pulmonary hypertension | 10 (20) | 9 (30) | 1 (5) | 0.04 † |
| FEV1/FVC | 0.79 (0.8–0.8) | 0.79 (0.8–0.8) | 0.76 (0.7–0.8) | 0.12 * |
| FEV1 (%) | 91 (81.8–101.8) | 87 (77.3–99.5) | 97.5 (87–104.8) | 0.03 * |
| FVC (%) | 98.5 (84–109.3) | 91 (78–105.8) | 102 (96.3–109.8) | 0.03 * |
| MMEF (%) | 70 (48–92) | 64 (45–83) | 84 (68.3–105.8) | 0.02 * |
| DLCO (%) | 69.5 (58.5–85.3) | 64.5 (47.5–70.5) | 81.5 (73–98.8) | <0.001 * |
| KCO (%) | 80.5 (67.3–90.8) | 76 (63–82) | 87.5 (72.5–97.3) | 0.01 * |
| VA (%) | 90 (79–101) | 84 (72.5–95) | 97.5 (90–105) | 0.002 * |
| Ground-glass opacities | 28 (56) | 26 (87) | 2 (10) | <0.001 † |
| Irregular pleura | 25 (50) | 22 (73) | 3 (15) | <0.001 † |
| Septal/subpleural lines | 37 (74) | 29 (97) | 8 (40) | <0.001 † |
| Honeycombing | 5 (10) | 5 (17) | 0 | 0.08 † |
| Subpleural cysts | 7 (14) | 7 (23) | 0 | 0.03 † |
| Esophageal diameter at location 1 (mm) | 8 (6–14) | 12 (7.5–16) | 7 (6–8) | <0.001 * |
| Esophageal diameter at location 2 (mm) | 12 (7.5–18.5) | 17 (9.5–22.5) | 8 (7–10.75) | <0.001 * |
| Esophageal diameter at location 3 (mm) | 16 (10.5–21) | 20 (13–25.5) | 11 (9–16) | 0.001 * |
| All Patients (N 50) | Patients with Interstitial Lung Disease (N 30) | Patients without Interstitial Lung Disease (N 20) | p Value | |
|---|---|---|---|---|
| Diaphragm mobility in deep breathing (cm) | ||||
| 5.35 (3.75–6.88) | 5.05 (2.43–6.71) | 5.85 (4.5–7.03) | 0.004 | |
| Diaphragm mobility in quiet breathing (cm) | 1.59 (1.18–2.13) | 1.8 (1.50–2.50) | 1.45 (1–1.92) | 0.21 |
| Diaphragm thickness at FRC (mm) | ||||
| Right side | 0.20 (0.20–0.30) | 0.24 (0.20–0.30) | 0.20 (0.17–0.30) | 0.20 |
| Left side | 0.24 (0.20–0.30) | 0.30 (0.20–0.30) | 0.21 (0.18–0.30) | 0.20 |
| Diaphragm thickness at TLC (mm) | ||||
| Right side | 0.40 (0.30–0.40) | 0.40 (0.30–0.40) | 0.36 (0.29–0.42) | 0.80 |
| Left side | 0.36 (0.30–0.40) | 0.38 (0.30–0.43) | 0.34 (0.28–0.40) | 0.51 |
| Thickening fraction | ||||
| Right side | 0.48 (0.33–0.67) | 0.50 (0.33–0.67) | 0.48 (0.33–0.84) | 0.32 |
| Left side | 0.44 (0.33–0.65) | 0.40 (0.33–0.50) | 0.43 (0.33–0.80) | 0.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ljilja Posavec, A.; Hrkač, S.; Tečer, J.; Huzjan Korunić, R.; Karanović, B.; Ježić, I.; Škopljanac, I.; Piskač Živković, N.; Mitrović, J. Ultrasonic Evaluation of Diaphragm in Patients with Systemic Sclerosis. J. Pers. Med. 2023, 13, 1441. https://doi.org/10.3390/jpm13101441
Ljilja Posavec A, Hrkač S, Tečer J, Huzjan Korunić R, Karanović B, Ježić I, Škopljanac I, Piskač Živković N, Mitrović J. Ultrasonic Evaluation of Diaphragm in Patients with Systemic Sclerosis. Journal of Personalized Medicine. 2023; 13(10):1441. https://doi.org/10.3390/jpm13101441
Chicago/Turabian StyleLjilja Posavec, Anja, Stela Hrkač, Josip Tečer, Renata Huzjan Korunić, Boris Karanović, Ivana Ježić, Ivan Škopljanac, Nevenka Piskač Živković, and Joško Mitrović. 2023. "Ultrasonic Evaluation of Diaphragm in Patients with Systemic Sclerosis" Journal of Personalized Medicine 13, no. 10: 1441. https://doi.org/10.3390/jpm13101441
APA StyleLjilja Posavec, A., Hrkač, S., Tečer, J., Huzjan Korunić, R., Karanović, B., Ježić, I., Škopljanac, I., Piskač Živković, N., & Mitrović, J. (2023). Ultrasonic Evaluation of Diaphragm in Patients with Systemic Sclerosis. Journal of Personalized Medicine, 13(10), 1441. https://doi.org/10.3390/jpm13101441