Resistant and Relapsing Collapsing Glomerulopathy Successfully Treated with Rituximab—A Case Report
Abstract
1. Introduction
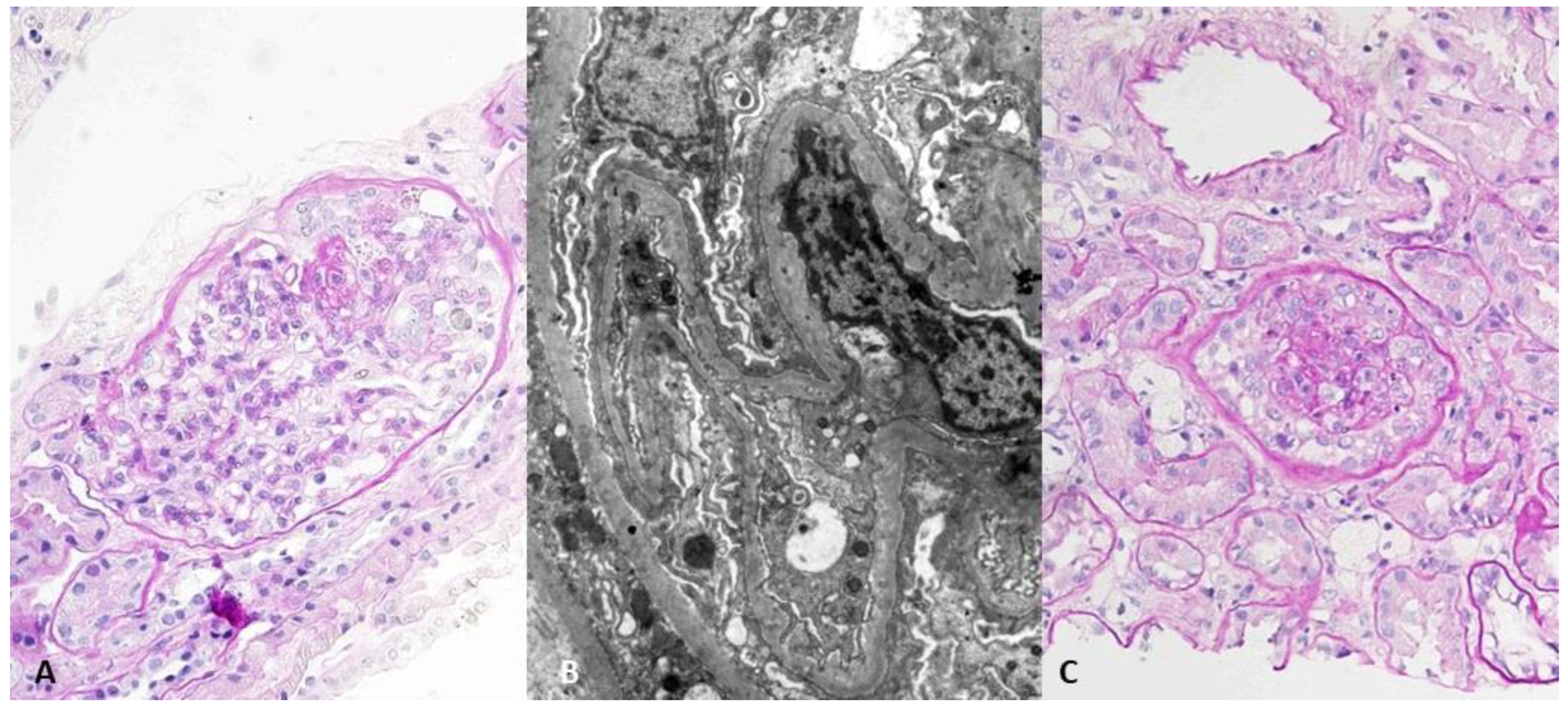
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albaqumi, M.; Barisoni, L. Current views on collapsing glomerulopathy. J. Am. Soc. Nephrol. 2008, 19, 1276–1281. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.B.; Franceschini, N.; Hogan, S.L.; Ten Holder, S.; Jennette, C.E.; Falk, R.J.; Jennette, J.C. Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants. Kidney Int. 2006, 69, 920–926. [Google Scholar] [PubMed]
- Cossey, L.N.; Larsen, C.P.; Liapis, H. Collapsing glomerulopathy: A 30-year perspective and single, large center experience. Clin. Kidney J. 2017, 10, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Laurin, L.P.; Gasim, A.M.; Derebail, V.K.; McGregor, J.G.; Kidd, J.M.; Hogan, S.L.; Poulton, C.J.; Detwiler, R.K.; Jennette, J.C.; Falk, R.J.; et al. Renal Survival in Patients with Collapsing Compared with Not Otherwise Specified FSGS. Clin. J. Am. Soc. Nephrol. 2016, 11, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.A.; Daquioag, E.; Margolin, E.G.; Pollak, V.E. Nephrotic syndrome, progressive irreversible renal failure, and glomerular “collapse”: A new clinicopathologic entity? Am. J. Kidney Dis. 1986, 7, 20–28. [Google Scholar] [CrossRef]
- Raja, R.; Nada, R.; Yadav, A.K.; Kumar, A.; Goyal, A.; Kumar, V.; Rathi, M.; Kohli, H.S.; Gupta, K.L.; Sakhuje, V.; et al. A prospective study of collapsing focal segmental glomerulosclerosis. Ren. Fail. 2016, 38, 894–898. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bitzan, M.; Ouahed, J.D.; Krishnamoorthy, P.; Bernard, C. Rituximab in treatment of collapsing C1q glomerulopathy: Clinical and histopathological evolution. Pediatr. Nephrol. 2008, 23, 1355–1361. [Google Scholar] [CrossRef] [PubMed]
- Kaito, H.; Kamei, K.; Kikuchi, E.; Ogura, M.; Matsuoka, K.; Nagata, M.; Iijima, K.; Ito, S. Successful treatment of collapsing focal segmental glomerulosclerosis with a combination of rituximab, steroids and cyclosporin. Pediatr. Nephrol. 2010, 25, 957–959. [Google Scholar] [CrossRef] [PubMed]
- Radmachandran, R.; Rajakumar, V.; Duseja, R.; Sakjuha, V.; Jha, V. Successful treatment of adult-onset collapsing focal segmental glomerulosclerosis with rituximab. Clin. Kidney J. 2013, 6, 500–502. [Google Scholar] [CrossRef] [PubMed]
- Davda, G.; Chopra, B.; Hussain, S.; Nashar, K.; Ko, T.; Jasnosz, K.; Sureshkumar, K. Successful treatment of post-transplant collapsing glomerulopathy with a rituximab-based regimen. Am. J. Kidney Dis. 2015, 65, A30. [Google Scholar]
- Girimaji, N.; Bharati, J.; Nada, R.; Rathi, M.; Kohli, H.S.; Ramachandran, R. Rituximab in treatment of collapsing FSGS—A case series. Nephrology 2021, 26, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Gauckler, P.; Shin, J.I.; Alberici, F.; Audard, V.; Bruchfeld, A.; Busch, M.; Cheung, C.K.; Crnogorac, M.; Delbarba, E.; Eller, K.; et al. Rutuximab in adult minimal change disease and focal segmental glomerulosclerosis—What is known and what is still unknown? Autoimmun. Rev. 2020, 19, 102671. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Disease Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 2021, 100, S1–S276. [Google Scholar]
- Colucci, M.; Carsetti, R.; Cascioli, S.; Casiraghi, F.; Perna, A.; Rava, L.; Ruggiero, B.; Emma, F.; Vivarelli, M. B Cell Reconstitution after Rituximab Treatment in Idiopathic Nephrotic Syndrome. J. Am. Soc. Nephrol. 2016, 27, 1811–1822. [Google Scholar] [PubMed]
- Lin, L.; Wang, W.; Wu, Y.; Xie, J.; Li, X.; Pan, X.; Zhang, W.; Xu, J.; Cai, Y.; Ren, H.; et al. Consolidation Treatment and Long-Term prognosis of Rituximab in Minimal Change Disease and Focal Segmental Glomerular Sclerosis. Drug Des. Devel. Ther. 2021, 15, 1945–1953. [Google Scholar] [PubMed]

| Laboratory Parameter | February 2010 (Time of Diagnosis) | November 2012 (CYC 1 Initiation) | November 2014 (First RTX 2 Application) | August 2018 (First Relapse after RTX) | December 2021 (Last Visit) |
|---|---|---|---|---|---|
| Hemoglobin (g/L) | 124 | 117 | 127 | 126 | 132 |
| Leukocytes (×106/L) | 9.2 | 5.8 | 7.7 | 5.7 | 9.2 |
| Serum creatinine (μmol/L) | 56 | 78 | 308 | 99 | 111 |
| eGFR CKD-EPI 3 (ml/min/1.73 m2) | 97 | 70 | 13 | 50 | 43 |
| Serum albumin (g/L) | 23 | 24 | 19 | 30 | 42 |
| Urea (mmol/L) | 5.2 | 6.4 | 35.2 | 10.4 | n/a |
| Total cholesterol (mmol/L) | 10 | 9.8 | 10.9 | 9.7 | 5.75 |
| LDL (mmol/L) | 5.77 | 6.4 | n/a | 6.89 | 3.26 |
| Triglycerides (mmol/L) | 1.62 | 2.4 | 4.47 | 1.79 | 0.99 |
| IgG (g/L) | n/a | 2.58 | n/a | n/a | n/a |
| C3 (g/L, ref. 0.9–1.8) | n/a | 1.35 | n/a | n/a | n/a |
| C4 (g/L, ref. 0.1–0.4) | n/a | 0.39 | n/a | n/a | n/a |
| Complete immunology | Negative | Negative | Negative | Negative | n/a |
| Viral hepatitis and HIV 4 serology | Negative | Negative | Negative | Negative | n/a |
| 24 h proteinuria (g/day) | 5.08 | 7.54 | 16.7 | 4.2 | 0.16 |
| Urine sediment, erythrocytes (per HPF 5) | 8 | 8–10 | 14 | 6 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zagorec, N.; Klarić, D.; Klarić, M.; Horvatić, I.; Šenjug, P.; Horaček, M.; Nikić, J.; Galešić Ljubanović, D.; Galešić, K. Resistant and Relapsing Collapsing Glomerulopathy Successfully Treated with Rituximab—A Case Report. J. Pers. Med. 2022, 12, 1415. https://doi.org/10.3390/jpm12091415
Zagorec N, Klarić D, Klarić M, Horvatić I, Šenjug P, Horaček M, Nikić J, Galešić Ljubanović D, Galešić K. Resistant and Relapsing Collapsing Glomerulopathy Successfully Treated with Rituximab—A Case Report. Journal of Personalized Medicine. 2022; 12(9):1415. https://doi.org/10.3390/jpm12091415
Chicago/Turabian StyleZagorec, Nikola, Dragan Klarić, Marta Klarić, Ivica Horvatić, Petar Šenjug, Matija Horaček, Jagoda Nikić, Danica Galešić Ljubanović, and Krešimir Galešić. 2022. "Resistant and Relapsing Collapsing Glomerulopathy Successfully Treated with Rituximab—A Case Report" Journal of Personalized Medicine 12, no. 9: 1415. https://doi.org/10.3390/jpm12091415
APA StyleZagorec, N., Klarić, D., Klarić, M., Horvatić, I., Šenjug, P., Horaček, M., Nikić, J., Galešić Ljubanović, D., & Galešić, K. (2022). Resistant and Relapsing Collapsing Glomerulopathy Successfully Treated with Rituximab—A Case Report. Journal of Personalized Medicine, 12(9), 1415. https://doi.org/10.3390/jpm12091415






