Functional Independence of Taiwanese Children with Osteogenesis Imperfecta
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. WeeFIM Questionnaire
2.3. Statistical Analysis
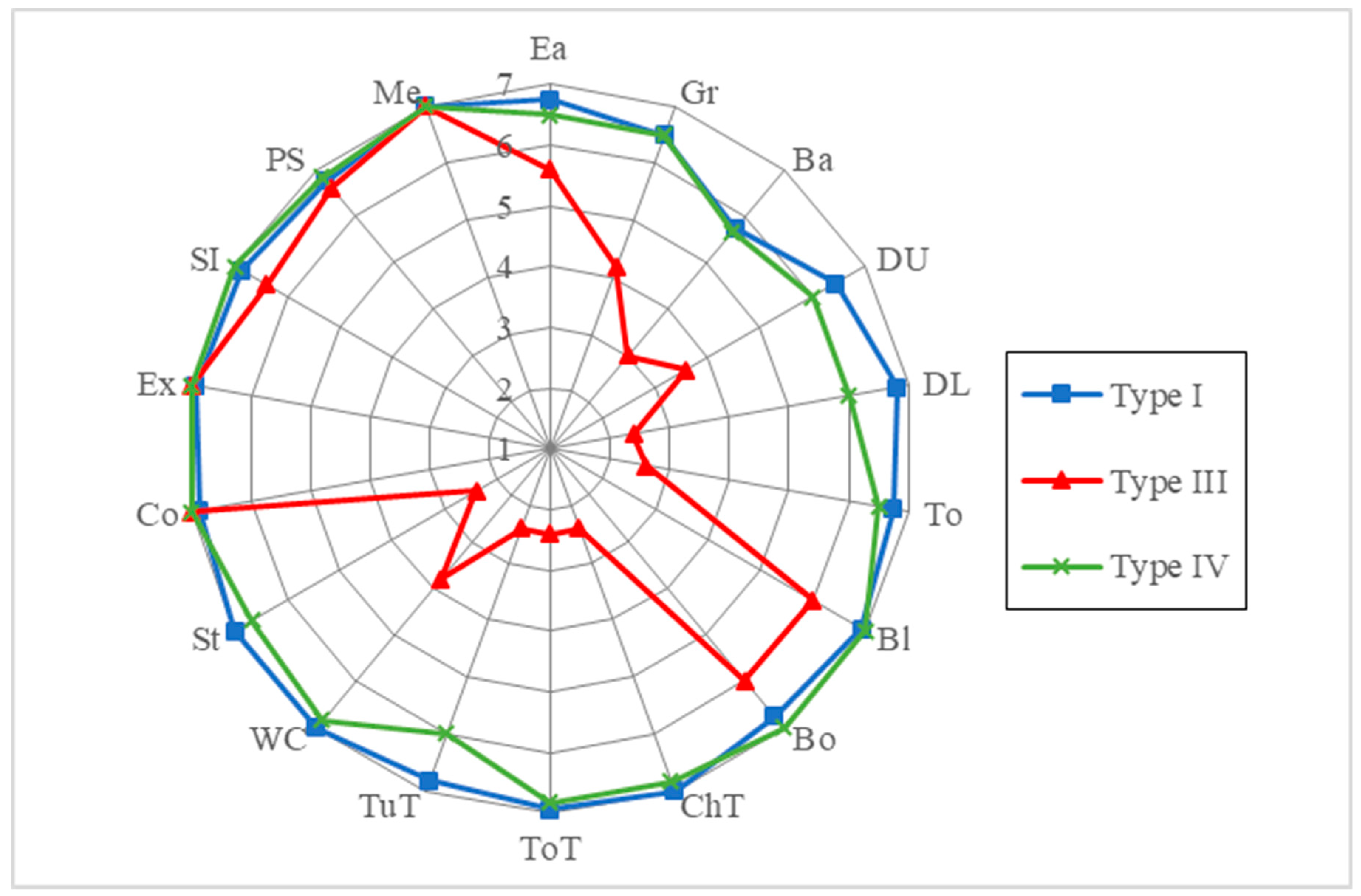
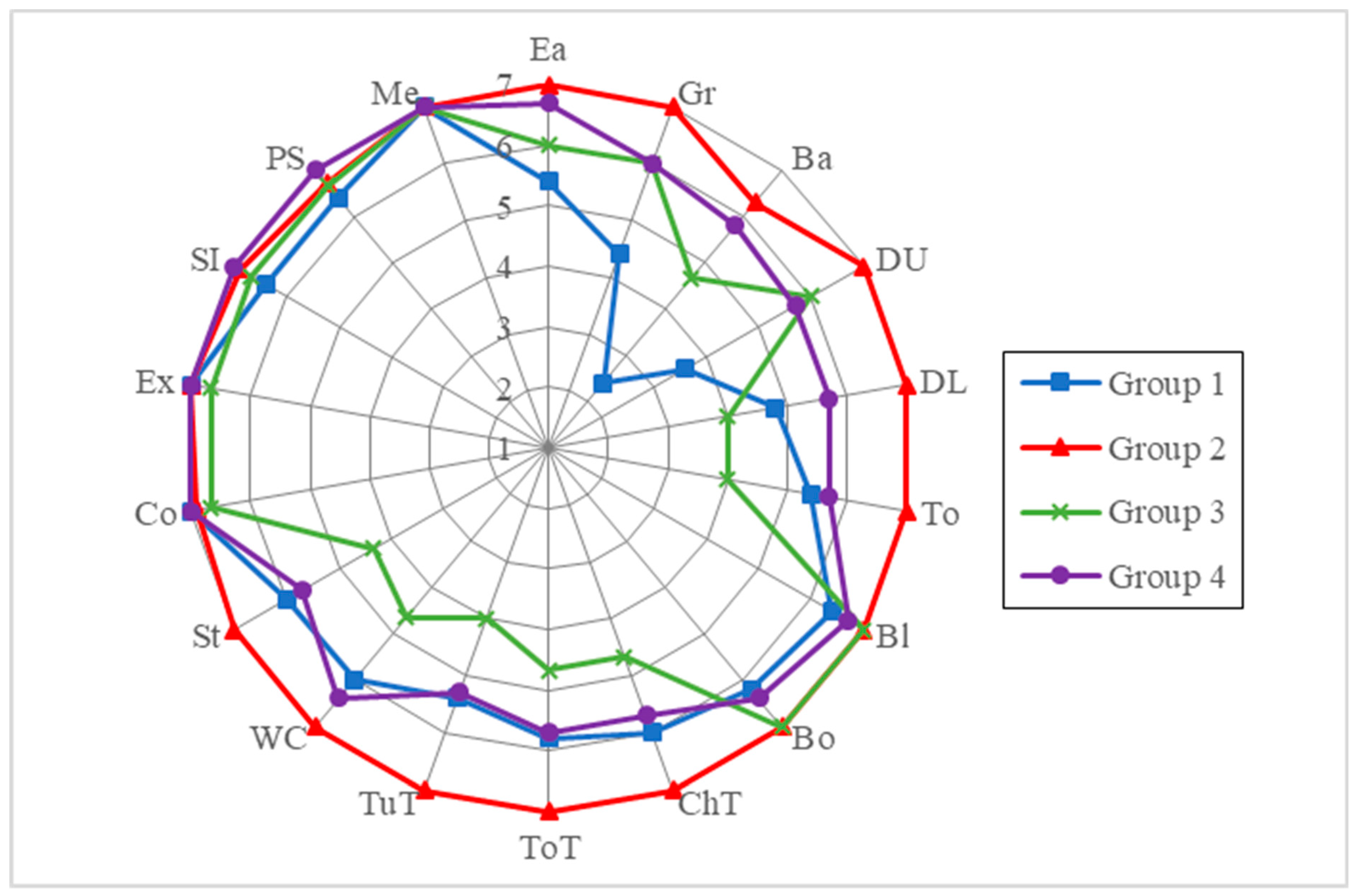
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OI | osteogenesis imperfecta |
| WeeFIM | Functional Independence Measure for Children |
| IQR | interquartile range |
References
- Mortier, G.R.; Cohn, D.H.; Cormier-Daire, V.; Hall, C.; Krakow, D.; Mundlos, S.; Nishimura, G.; Robertson, S.; Sangiorgi, L.; Savarirayan, R.; et al. Nosology and classification of genetic skeletal disorders: 2019 revision. Am. J. Med. Genet. A 2019, 179, 2393–2419. [Google Scholar] [CrossRef] [PubMed]
- Engelbert, R.H.; Beemer, F.A.; van der Graaf, Y.; Helders, P.J. Osteogenesis imperfecta in childhood: Impairment and disability—A follow-up study. Arch. Phys. Med. Rehabil. 1999, 80, 896–903. [Google Scholar] [CrossRef]
- Engelbert, R.H.; Uiterwaal, C.S.; Gerver, W.J.; van der Net, J.J.; Pruijs, H.E.; Helders, P.J. Osteogenesis imperfecta in childhood: Impairment and disability. A prospective study with 4-year follow-up. Arch. Phys. Med. Rehabil. 2004, 85, 772–778. [Google Scholar] [CrossRef]
- Nijhuis, W.; Verhoef, M.; van Bergen, C.; Weinans, H.; Sakkers, R. Fractures in Osteogenesis Imperfecta: Pathogenesis, Treatment, Rehabilitation and Prevention. Children 2022, 9, 268. [Google Scholar] [CrossRef]
- Marom, R.; Rabenhorst, B.M.; Morello, R. Osteogenesis imperfecta: An update on clinical features and therapies. Eur. J. Endocrinol. 2020, 183, R95–R106. [Google Scholar] [CrossRef] [PubMed]
- Montpetit, K.; Palomo, T.; Glorieux, F.H.; Fassier, F.; Rauch, F. Multidisciplinary Treatment of Severe Osteogenesis Imperfecta: Functional Outcomes at Skeletal Maturity. Arch. Phys. Med. Rehabil. 2015, 96, 1834–1839. [Google Scholar] [CrossRef] [PubMed]
- Arshad, F.; Bishop, N. Osteogenesis imperfecta in children. Bone 2021, 148, 115914. [Google Scholar] [CrossRef]
- Sousa, T.; Bompadre, V.; White, K.K. Musculoskeletal functional outcomes in children with osteogenesis imperfecta: Associations with disease severity and pamidronate therapy. J. Pediatr. Orthop. 2014, 34, 118–122. [Google Scholar] [CrossRef]
- Garganta, M.D.; Jaser, S.S.; Lazow, M.A.; Schoenecker, J.G.; Cobry, E.; Hays, S.R.; Simmons, J.H. Cyclic bisphosphonate therapy reduces pain and improves physical functioning in children with osteogenesis imperfecta. BMC Musculoskelet. Disord. 2018, 19, 344. [Google Scholar] [CrossRef]
- Dwan, K.; Phillipi, C.A.; Steiner, R.D.; Basel, D. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst. Rev. 2016, 10, CD005088. [Google Scholar] [CrossRef]
- Seikaly, M.G.; Kopanati, S.; Salhab, N.; Waber, P.; Patterson, D.; Browne, R.; A Herring, J. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J. Pediatr. Orthop. 2005, 25, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Veilleux, L.N.; Trejo, P.; Rauch, F. Muscle abnormalities in osteogenesis imperfecta. J. Musculoskelet. Neuronal Interact. 2017, 17, 1–7. [Google Scholar] [PubMed]
- Ottenbacher, K.J.; Msall, M.E.; Lyon, N. Measuring developmental and functional status in children with disabilities. Pediatr. Phys. Ther. 2000, 12, 198–199. [Google Scholar] [CrossRef]
- Wong, V.; Wong, S.; Chan, K.; Wong, W. Functional Independence Measure (WeeFIM) for Chinese children: Hong Kong Cohort. Pediatrics 2002, 109, E36. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.S.; Wong, V.C. Functional Independence Measure for Children: A comparison of Chinese and Japanese children. Neurorehabilit. Neural Repair. 2007, 21, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.; Salem, Y.; Liu, H.H.; Zhou, X.; Chen, S.; Chen, N.; Yang, X.; Lialng, J.; Sun, K. A home-based exercise program for children with congenital heart disease following interventional cardiac catheterization: Study protocol for a randomized controlled trial. Trials 2017, 18, 38. [Google Scholar] [CrossRef]
- Wong, V.; Chung, B.; Hui, S.; Fong, A.; Lau, C.; Law, B.; Lo, K.; Shum, T.; Wong, R. Cerebral palsy: Correlation of risk factors and functional performance using the Functional Independence Measure for Children (WeeFIM). J. Child Neurol. 2004, 19, 887–893. [Google Scholar] [CrossRef]
- Lee, C.L.; Lin, H.Y.; Chuang, C.K.; Chiu, H.C.; Tu, R.Y.; Huang, Y.H.; Hwu, W.-L.; Tsai, F.-J.; Chiu, P.-C.; Niu, D.-M.; et al. Functional independence of Taiwanese patients with mucopolysaccharidoses. Mol. Genet. Genom. Med. 2019, 7, e790. [Google Scholar] [CrossRef]
- Lee, C.L.; Lin, H.Y.; Tsai, L.P.; Chiu, H.C.; Tu, R.Y.; Huang, Y.H.; Chien, Y.-H.; Lee, N.-C.; Niu, D.-M.; Chao, M.-C.; et al. Functional independence of Taiwanese children with Prader-Willi syndrome. Am. J. Med. Genet. A 2018, 176, 1309–1314. [Google Scholar] [CrossRef]
- Lin, H.Y.; Chuang, C.K.; Chen, Y.J.; Tu, R.Y.; Chen, M.R.; Niu, D.M.; Lin, S.-P. Functional independence of Taiwanese children with Down syndrome. Dev. Med. Child Neurol. 2016, 58, 502–507. [Google Scholar] [CrossRef]
- Sperle, P.A.; Ottenbacher, K.J.; Braun, S.L.; Lane, S.J.; Nochajski, S. Equivalence reliability of the functional independence measure for children (WeeFIM) administration methods. Am. J. Occup. Ther. 1997, 51, 35–41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lin, H.Y.; Lin, S.P.; Lin, H.Y.; Hsu, C.H.; Chang, J.H.; Kao, H.A.; Hung, H.-Y.; Peng, C.-C.; Lee, H.-C.; Chen, M.-R.; et al. Functional independence of Taiwanese children with VACTERL association. Am. J. Med. Genet. A 2012, 158A, 3101–3105. [Google Scholar] [CrossRef] [PubMed]
- Engelbert, R.H.H.; Custers, J.W.H.; van der Net, J.; van der Graaf, Y.; Beemer, F.A.; Helders, P.J.M. Functional Outcome in Osteogenesis Imperfecta: Disability Profiles Using the PEDI. Pediatr. Phys. Therapy 1997, 9, 18–22. [Google Scholar] [CrossRef]
- Vanz, A.P.; van de Sande Lee, J.; Pinheiro, B.; Zambrano, M.; Brizola, E.; da Rocha, N.S.; Schwartz, I.V.D.; Pires, M.M.D.S.; Félix, T.M. Health-related quality of life of children and adolescents with osteogenesis imperfecta: A cross-sectional study using PedsQL. BMC Pediatr. 2018, 18, 95. [Google Scholar] [CrossRef] [PubMed]
- Constantino, C.S.; Krzak, J.J.; Fial, A.V.; Kruger, K.M.; Rammer, J.R.; Radmanovic, K.; Smith, P.A.; Harris, G.F. Effect of Bisphosphonates on Function and Mobility Among Children With Osteogenesis Imperfecta: A Systematic Review. JBMR Plus. 2019, 3, e10216. [Google Scholar] [CrossRef]
- Engelbert, R.H.; Uiterwaal, C.S.; Gulmans, V.A.; Pruijs, H.; Helders, P.J. Osteogenesis imperfecta in childhood: Prognosis for walking. J. Pediatr. 2000, 137, 397–402. [Google Scholar] [CrossRef]
- Amako, M.; Fassier, F.; Hamdy, R.C.; Aarabi, M.; Montpetit, K.; Glorieux, F.H. Functional analysis of upper limb deformities in osteogenesis imperfecta. J. Pediatr. Orthop. 2004, 24, 689–694. [Google Scholar] [CrossRef]
- Palomo, T.; Glorieux, F.H.; Schoenau, E.; Rauch, F. Body Composition in Children and Adolescents with Osteogenesis Imperfecta. J. Pediatr. 2016, 169, 232–237. [Google Scholar] [CrossRef]
- Veilleux, L.N.; Pouliot-Laforte, A.; Lemay, M.; Cheung, M.S.; Glorieux, F.H.; Rauch, F. The functional muscle-bone unit in patients with osteogenesis imperfecta type I. Bone 2015, 79, 52–57. [Google Scholar] [CrossRef]
- Gremminger, V.L.; Phillips, C.L. Impact of Intrinsic Muscle Weakness on Muscle-Bone Crosstalk in Osteogenesis Imperfecta. Int. J. Mol. Sci. 2021, 22, 4963. [Google Scholar] [CrossRef]
- Pavone, V.; Mattina, T.; Pavone, P.; Falsaperla, R.; Testa, G. Early Motor Delay: An Outstanding, Initial Sign of Osteogenesis Imperfecta Type 1. J. Orthop. Case Rep. 2017, 7, 63–66. [Google Scholar] [PubMed]
- Brizola, E.; Staub, A.L.; Felix, T.M. Muscle strength, joint range of motion, and gait in children and adolescents with osteogenesis imperfecta. Pediatr. Phys. Ther. 2014, 26, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Veilleux, L.N.; Lemay, M.; Pouliot-Laforte, A.; Cheung, M.S.; Glorieux, F.H.; Rauch, F. Muscle anatomy and dynamic muscle function in osteogenesis imperfecta type I. J. Clin. Endocrinol. Metab. 2014, 99, E356–E362. [Google Scholar] [CrossRef] [PubMed]
- Veilleux, L.N.; Darsaklis, V.B.; Montpetit, K.; Glorieux, F.H.; Rauch, F. Muscle Function in Osteogenesis Imperfecta Type IV. Calcif. Tissue Int. 2017, 101, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Badhyal, S.; Dhole, S.R.; Gopinathan, N.R.; Dhillon, M.S.; Dhiman, V.; Jayal, A.D.; Prasad, J. Kinetic and Kinematic Analysis of Gait in Type IV Osteogenesis Imperfecta Patients: A Comparative Study. Indian J. Orthop. 2019, 53, 560–566. [Google Scholar] [CrossRef]
- Caudill, A.; Flanagan, A.; Hassani, S.; Graf, A.; Bajorunaite, R.; Harris, G.; Smith, P. Ankle strength and functional limitations in children and adolescents with type I osteogenesis imperfecta. Pediatr. Phys. Ther. 2010, 22, 288–295. [Google Scholar] [CrossRef]
- Zack, P.; Franck, L.; Devile, C.; Clark, C. Fracture and non-fracture pain in children with osteogenesis imperfecta. Acta Paediatr. 2005, 94, 1238–1242. [Google Scholar] [CrossRef]
- Dahan-Oliel, N.; Oliel, S.; Tsimicalis, A.; Montpetit, K.; Rauch, F.; Dogba, M.J. Quality of life in osteogenesis imperfecta: A mixed-methods systematic review. Am. J. Med. Genet. A 2016, 170A, 62–76. [Google Scholar] [CrossRef]
- Germain-Lee, E.L.; Brennen, F.S.; Stern, D.; Kantipuly, A.; Melvin, P.; Terkowitz, M.S.; Shapiro, J.R. Cross-sectional and longitudinal growth patterns in osteogenesis imperfecta: Implications for clinical care. Pediatr. Res. 2016, 79, 489–495. [Google Scholar] [CrossRef]
- Aglan, M.S.; Zaki, M.E.; Hosny, L.; El-Houssini, R.; Oteify, G.; Temtamy, S.A. Anthropometric measurements in Egyptian patients with osteogenesis imperfecta. Am. J. Med. Genet. A 2012, 158A, 2714–2718. [Google Scholar] [CrossRef]
- Barber, L.A.; Abbott, C.; Nakhate, V.; Do, A.N.D.; Blissett, A.R.; Marini, J.C. Longitudinal growth curves for children with classical osteogenesis imperfecta (types III and IV) caused by structural pathogenic variants in type I collagen. Genet. Med. 2019, 21, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Graff, K.; Syczewska, M. Developmental charts for children with osteogenesis imperfecta, type I (body height, body weight and BMI). Eur. J. Pediatr. 2017, 176, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Tam, A.; Shapiro, J.R.; Steiner, R.D.; Smith, P.A.; Bober, M.B.; Hart, T.; Cuthbertson, D.; Krischer, J.; Mullins, M.; et al. Growth characteristics in individuals with osteogenesis imperfecta in North America: Results from a multicenter study. Genet. Med. 2019, 21, 275–283. [Google Scholar] [CrossRef]
- Lund, A.M.; Muller, J.; Skovby, F. Anthropometry of patients with osteogenesis imperfecta. Arch. Dis. Child. 1999, 80, 524–528. [Google Scholar] [CrossRef]
- Grafe, I.; Yang, T.; Alexander, S.; Homan, E.P.; Lietman, C.; Jiang, M.M.; Bertin, T.; Munivez, E.; Chen, Y.; Dawson, B.; et al. Excessive transforming growth factor-beta signaling is a common mechanism in osteogenesis imperfecta. Nat. Med. 2014, 20, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.L.; Hsieh, C.L.; Sheu, C.F.; Hu, F.C.; Tseng, M.H. Reliability and validity of a Chinese version of the Pediatric Evaluation of Disability Inventory in children with cerebral palsy. J. Rehabil. Med. 2009, 41, 273–278. [Google Scholar] [CrossRef]
- Msall, M.E.; DiGaudio, K.; Duffy, L.C.; LaForest, S.; Braun, S.; Granger, C.V. WeeFIM. Normative sample of an instrument for tracking functional independence in children. Clin. Pediatr. (Phila) 1994, 33, 431–438. [Google Scholar] [CrossRef] [PubMed]

| Levels |
| Independent |
| 7. Complete independence (timely, safe) |
| 6. Modified independence (assistive device/not safe or timely) |
| Modified dependence |
| 5. Supervision |
| 4. Minimal assistance (subject > 75%) |
| 3. Moderate assistance (subject = 50–74%) |
| Complete dependence |
| 2. Maximal assistance (subject = 25–49%) |
| 1. Total assistance (subject = 0–24%) |
| Items |
| Self-care |
| 1. Eating (Ea) |
| 2. Grooming (Gr) |
| 3. Bathing (Ba) |
| 4. Dressing-upper (DU) |
| 5. Dressing-lower (DL) |
| 6. Toileting (To) |
| 7. Bladder (Bl) |
| 8. Bowel (Bo) |
| Mobility |
| 9. Bed/Chair/Wheelchair transfer (ChT) |
| 10. Toilet transfer (ToT) |
| 11. Tub/Shower transfer (TuT) |
| 12. Walk/Wheelchair (WC) |
| 13. Stairs (St) |
| Cognition |
| 14. Comprehension (Co) |
| 15. Expression (Ex) |
| 16. Social interaction (SI) |
| 17. Problem-solving (PS) |
| 18. Memory (Me) |
| Group 1 | Group 2 | Group 3 | Group 4 | Total | |
|---|---|---|---|---|---|
| Age (years) | 2.0–5.9 | 6.0–10.9 | 11–15.9 | 16–21 | 2–21 |
| n | 5 | 10 | 3 | 9 | 27 |
| Self-care score | p = 0.28 | ||||
| Range | 24–53 | 52–56 | 38–56 | 13–56 | 13–56 |
| Median score | 37 | 56 | 40 | 56 | 56 |
| Mean quotient (%) a | 89.64 | 99.29 | 79.76 | 86.7 | 91.14 |
| Interquartile range | 11 | 0 | 9 | 2 | 13.5 |
| Mobility score | p = 0.206 | ||||
| Range | 10–35 | 35 | 5–35 | 5–35 | 5–35 |
| Median score | 34 | 35 | 27 | 35 | 35 |
| Mean quotient (%) a | 84.17 | 100 | 63.8 | 82.22 | 87.12 |
| Interquartile range | 3 | 0 | 15 | 3 | 2 |
| Cognition score | p = 0.09 | ||||
| Range | 30–35 | 33–35 | 31–35 | 35 | 30–35 |
| Median score | 35 | 35 | 35 | 35 | 35 |
| Mean quotient (%) a | 100 | 98.57 | 96.19 | 100 | 99.05 |
| Interquartile range | 1 | 1 | 2 | 0 | 0.5 |
| Total score | p = 0.211 | ||||
| Range | 64–123 | 120–126 | 80–122 | 53–126 | 53–126 |
| Median score | 105 | 125.5 | 100 | 126 | 124 |
| Mean quotient (%) a | 93.06 | 99.29 | 79.89 | 89.15 | 92.6 |
| Interquartile range | 8 | 1 | 21 | 3 | 17.5 |
| Type I | Type III | Type IV | Total | |
|---|---|---|---|---|
| Mean age (years) | 11.2 | 15.3 | 11.1 | 11.9 |
| n | 16 | 5 | 6 | 27 |
| Self-care score | p < 0.001 | |||
| Range | 34–56 | 13–56 | 38–56 | 13–56 |
| Mean score | 52.69 | 33.4 | 51.17 | 48.78 |
| Median score | 56 | 26 | 56 | 56 |
| Mean quotient (%) a | 98.98 | 63.07 | 93.6 | 91.14 |
| Standard deviation | 6.87 | 14.59 | 7.8 | 11.3 |
| Interquartile range | 3 | 16 | 8.25 | 13.5 |
| Mobility score | p < 0.001 | |||
| Range | 32–35 | 5–35 | 27–35 | 5–35 |
| Mean score | 34.75 | 13.4 | 33.17 | 30.44 |
| Median score | 35 | 10 | 35 | 35 |
| Mean quotient (%) a | 99.46 | 38.45 | 94.76 | 87.12 |
| Standard deviation | 0.78 | 12.34 | 3.25 | 9.74 |
| Interquartile range | 0 | 5 | 2.25 | 2 |
| Cognition score | p = 0.486 | |||
| Range | 31–35 | 30–35 | 34–35 | 30–35 |
| Mean score | 34.44 | 34 | 34.83 | 34.44 |
| Median score | 35 | 35 | 35 | 35 |
| Mean quotient (%) a | 98.57 | 100 | 99.52 | 99.05 |
| Standard deviation | 1.09 | 2.24 | 0.41 | 1.25 |
| Interquartile range | 1 | 0 | 0 | 0.5 |
| Total score | p < 0.001 | |||
| Range | 104–126 | 53–126 | 100–126 | 53–126 |
| Mean score | 121.88 | 80.8 | 119.17 | 113.7 |
| Median score | 124.5 | 68 | 125.5 | 124 |
| Mean quotient (%) a | 99.16 | 67.03 | 96.43 | 92.6 |
| Standard deviation | 7.01 | 26.25 | 10.89 | 20.33 |
| Interquartile range | 3.25 | 16 | 10.75 | 17.5 |
| Number of Patients | 6 | |||
|---|---|---|---|---|
| Mean Age of First Evaluation (Months) | 113.8 | |||
| Age Range (Months) | 53–252 | |||
| Mean-Pre | Mean-Post | Coefficient | p Value | |
| Self-care score | 41.2 | 50 | 0.84 | 0.053 |
| Mobility score | 28 | 30 | 1 | 0.1 |
| Cognition score | 32.5 | 35 | 0.42 | 0.41 |
| Total score | 102 | 115 | 0.9 | 0.052 |
| Body height | 103 | 113 | 0.9 | 0.044 * |
| Requiring Help (1–4 Points) | Requiring Supervision (5 Points) | Requiring no Help (6–7 Points) | ||||
|---|---|---|---|---|---|---|
| Task | n | % | n | % | n | % |
| Eating | 4 | 14.8 | 0 | 0.0 | 23 | 85.2 |
| Grooming | 6 | 22.2 | 0 | 0.0 | 21 | 77.8 |
| Bathing | 11 | 40.7 | 0 | 0.0 | 16 | 59.3 |
| Dressing-upper | 7 | 25.9 | 0 | 0.0 | 20 | 74.1 |
| Dressing-lower | 7 | 25.9 | 0 | 0.0 | 20 | 74.1 |
| Toileting | 6 | 22.2 | 0 | 0.0 | 21 | 77.8 |
| Bladder | 1 | 3.7 | 1 | 3.7 | 25 | 92.6 |
| Bowel | 1 | 3.7 | 2 | 7.4 | 24 | 88.9 |
| Chair transfer | 4 | 14.8 | 0 | 0.0 | 23 | 85.2 |
| Toilet transfer | 4 | 14.8 | 0 | 0.0 | 23 | 85.2 |
| Tub transfer | 7 | 25.9 | 0 | 0.0 | 20 | 74.1 |
| Walking | 3 | 11.1 | 0 | 0.0 | 24 | 88.9 |
| Stairs | 4 | 14.8 | 1 | 3.7 | 22 | 81.5 |
| Comprehension | 0 | 0.0 | 0 | 0.0 | 27 | 100.0 |
| Expression | 0 | 0.0 | 0 | 0.0 | 27 | 100.0 |
| Social interaction | 1 | 3.7 | 0 | 0.0 | 26 | 96.3 |
| Problem-solving | 0 | 0.0 | 1 | 3.7 | 26 | 96.3 |
| Memory | 0 | 0.0 | 0 | 0.0 | 27 | 100.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Syu, Y.-M.; Lee, C.-L.; Chuang, C.-K.; Chiu, H.-C.; Chang, Y.-H.; Lin, H.-Y.; Lin, S.-P. Functional Independence of Taiwanese Children with Osteogenesis Imperfecta. J. Pers. Med. 2022, 12, 1205. https://doi.org/10.3390/jpm12081205
Syu Y-M, Lee C-L, Chuang C-K, Chiu H-C, Chang Y-H, Lin H-Y, Lin S-P. Functional Independence of Taiwanese Children with Osteogenesis Imperfecta. Journal of Personalized Medicine. 2022; 12(8):1205. https://doi.org/10.3390/jpm12081205
Chicago/Turabian StyleSyu, Yu-Min, Chung-Lin Lee, Chih-Kuang Chuang, Huei-Ching Chiu, Ya-Hui Chang, Hsiang-Yu Lin, and Shuan-Pei Lin. 2022. "Functional Independence of Taiwanese Children with Osteogenesis Imperfecta" Journal of Personalized Medicine 12, no. 8: 1205. https://doi.org/10.3390/jpm12081205
APA StyleSyu, Y.-M., Lee, C.-L., Chuang, C.-K., Chiu, H.-C., Chang, Y.-H., Lin, H.-Y., & Lin, S.-P. (2022). Functional Independence of Taiwanese Children with Osteogenesis Imperfecta. Journal of Personalized Medicine, 12(8), 1205. https://doi.org/10.3390/jpm12081205








