National Chronic Disease Management Programmes in Irish General Practice-Preparedness and Challenges
Abstract
1. Introduction
2. Methods
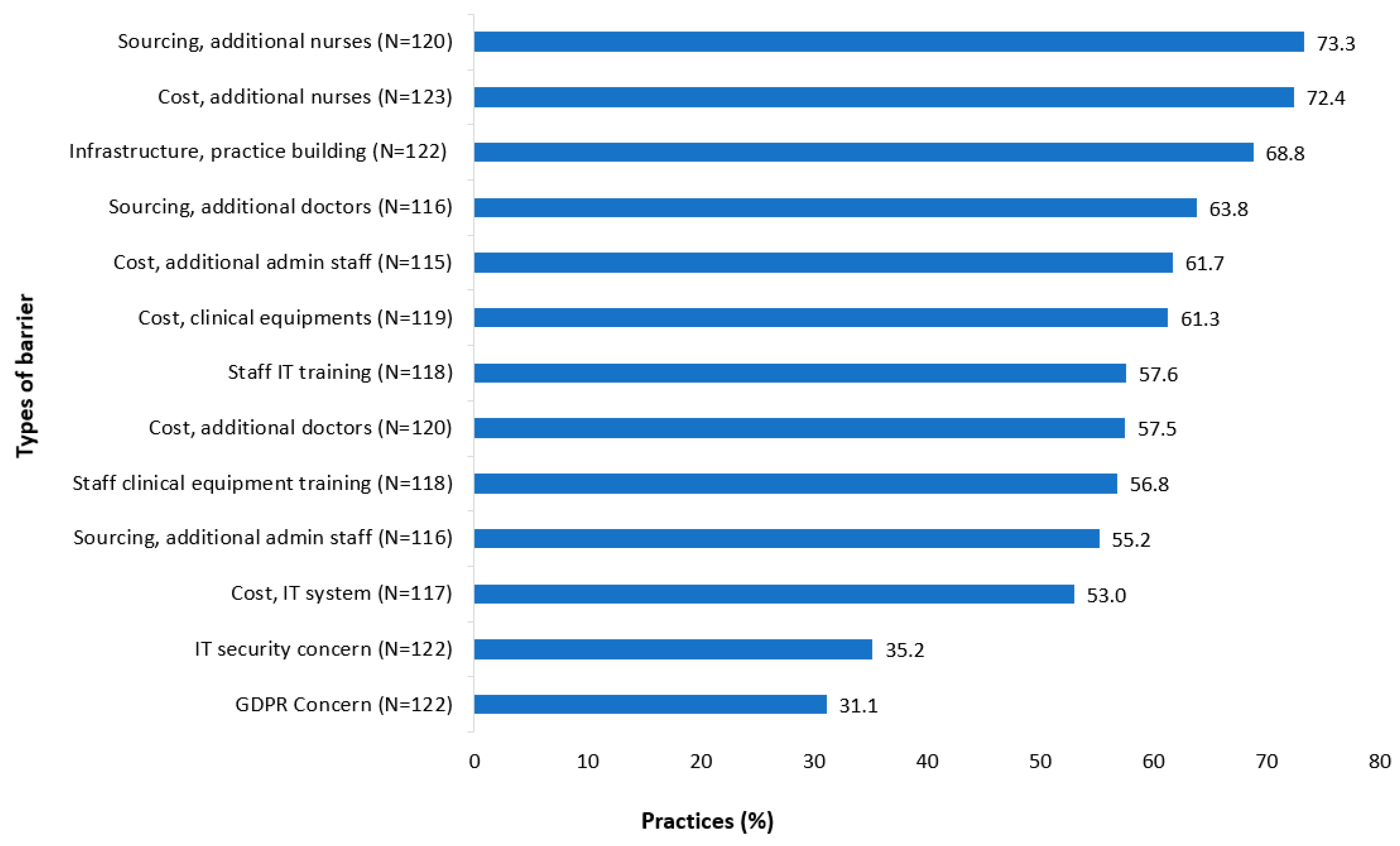
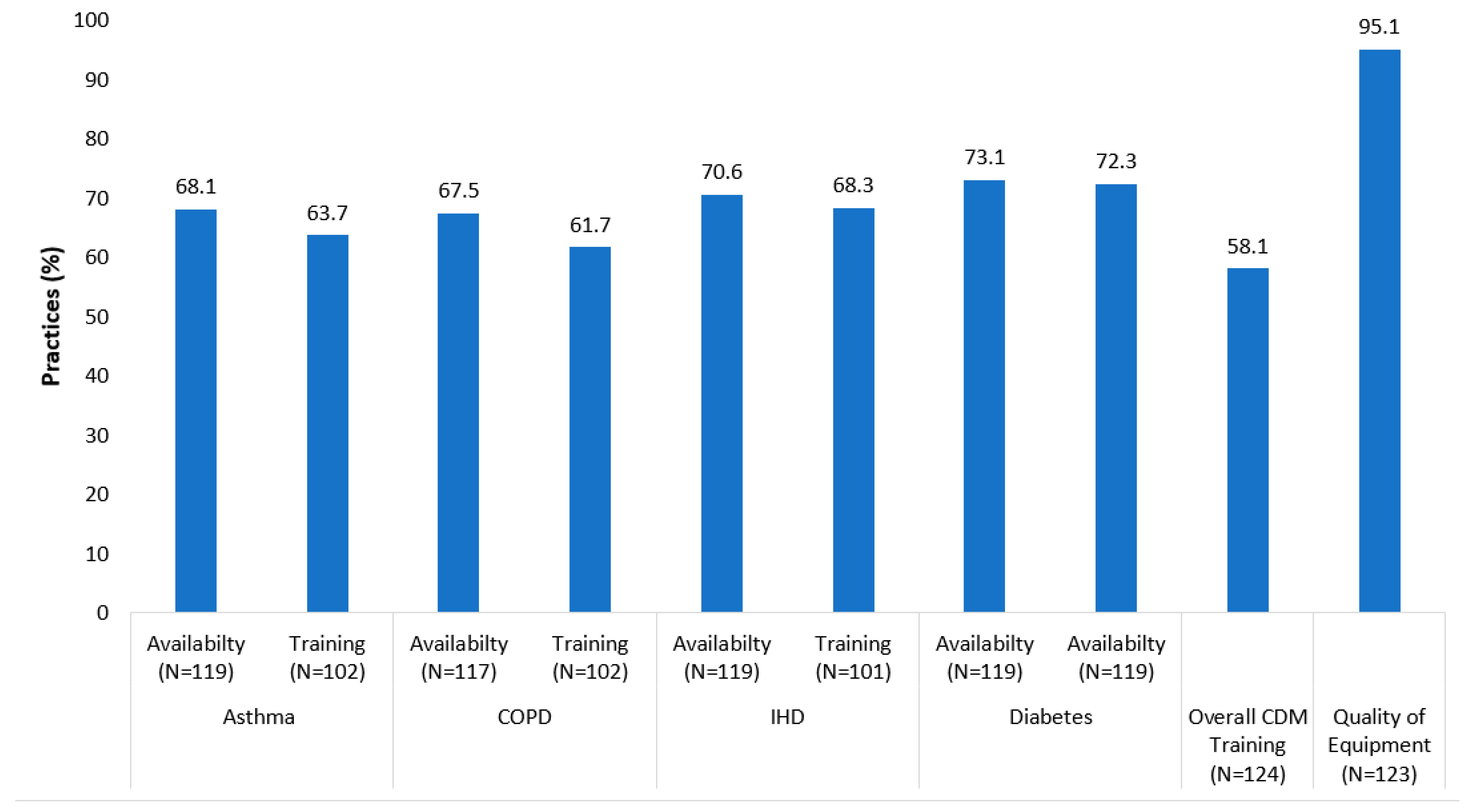
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tandan, M.; Duane, S.; Vellinga, A. Do general practitioners prescribe more antimicrobials when the weekend comes? SpringerPlus 2015, 4, 725. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alyousef, M.; Naughton, C.; Bradley, C.; Savage, E. Primary healthcare reform for chronic conditions in countries with high or very high human development index: A systematic review. Chronic Illn. 2021, 17423953211059143. [Google Scholar] [CrossRef] [PubMed]
- Kruis, A.L.; Boland, M.R.; Assendelft, W.J.; Gussekloo, J.; Tsiachristas, A.; Stijnen, T.; Blom, C.; Sont, J.K.; Rutten-van Mölken, M.P.; Chavannes, N.H. Effectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: Results of cluster randomised trial. BMJ 2014, 349, g5392. [Google Scholar] [CrossRef] [PubMed]
- Markun, S.; Rosemann, T.; Dalla-Lana, K.; Steurer-Stey, C. Care in Chronic Obstructive Lung Disease (CAROL): A randomised trial in general practice. Eur. Respir. J. 2018, 51, 1701873. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Cousins, G.; Clyne, B.; Allwright, S.; O’Dowd, T. Shared care across the interface between primary and specialty care in management of long term conditions. Cochrane Database Syst. Rev. 2017, 2, Cd004910. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.X.; Dong, Y.; Tan, P.C.; Gan, P.; Zhang, D.; Chi, Y.; Chao, F.F.T.; Lu, J.; Teo, B.H.D.; Tan, Y.Q. Development of a Community-Based e-Health Program for Older Adults With Chronic Diseases: Pilot Pre-Post Study. JMIR Aging 2022, 5, e33118. [Google Scholar] [CrossRef] [PubMed]
- Health Service Executive (HSE). Chronic Disease Management Programme. Available online: https://www.hse.ie/eng/about/who/gmscontracts/2019agreement/chronic-disease-management-programme/chronic-disease-management-programme.html (accessed on 18 February 2022).
- Health Service Executive (HSE). National Framework for the Integerated Prevention and Management of Chronic Disease in Ireland 2020–2025; Health Service Executive: Dublin, Ireland, 2020. [Google Scholar]
- Collins, C.; Homeniuk, R. How many general practice consultations occur in Ireland annually? Cross-sectional data from a survey of general practices. BMC Fam. Pract. 2021, 22, 40. [Google Scholar] [CrossRef] [PubMed]
- Health Service Executive (HSE). HSE Wins International UN Award for Tackling Chronic Disease; HSE Press Release October 2021; HSE: Dublin, Ireland, 2021. [Google Scholar]
- Darker, C.; Martin, C.; O’Dowd, T.; O’Kelly, F.; O’Shea, B. Chronic disease management in general practice: Results from a national study. Ir. Med. J. 2012, 105, 102–105. [Google Scholar] [PubMed]
- Løkke, A.; Søndergaard, J.; Hansen, M.K.; Roslind, K.; Lange, P. Management of chronic obstructive pulmonary disease in general practice in Denmark. Dan. Med. J. 2020, 67, A03190163. [Google Scholar] [PubMed]
- Med, I.; O’Halloran, L.; Purcell, A.; Ryan, E.; O’Doherty, J.; Troddyn, L.; Slepanek, M.; O’Driscoll, N.; O’Reilly, O. A Snapshot Of Chronic Obstructive Pulmonary Disease Management in General Practice in Ireland. Ir. J. Med. Sci. 2020, 190, 1055–1061. [Google Scholar] [CrossRef]
- Moth, G.; Vestergaard, M.; Vedsted, P. Chronic care management in Danish general practice--a cross-sectional study of workload and multimorbidity. BMC Fam. Pract. 2012, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- Rudolphy, S. Asthma management in general practice—A chronic disease health priority. Aust. Fam. Physician 2008, 37, 710–714. [Google Scholar] [PubMed]
- Sandelowsky, H.; Weinreich, U.M.; Aarli, B.B.; Sundh, J.; Høines, K.; Stratelis, G.; Løkke, A.; Janson, C.; Jensen, C.; Larsson, K. COPD—Do the right thing. BMC Fam. Pract. 2021, 22, 244. [Google Scholar] [CrossRef] [PubMed]
- Anwar, M.S.; Baker, R.; Walker, N.; Mainous, A.G., 3rd; Bankart, M.J. Chronic disease detection and access: Does access improve detection, or does detection make access more difficult? Br. J. Gen. Pract. 2012, 62, e337–e343. [Google Scholar] [CrossRef] [PubMed]
- Pericin, I.; Larkin, J.; Collins, C. Diagnostic coding of chronic physical conditions in Irish general practice. Ir. J. Med. Sci. 2021, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.; Koehne, K.; Verrall, C.C.; Szabo, N.; Bollen, C.; Parker, S. Building chronic disease management capacity in General Practice: The South Australian GP Plus Practice Nurse Initiative. Collegian 2015, 22, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Young, J.; Eley, D.; Patterson, E.; Turner, C. A nurse-led model of chronic disease management in general practice: Patients’ perspectives. Aust. Fam. Physician 2016, 45, 912–916. [Google Scholar] [PubMed]
- ICGP. Submission to the Oireachtas Joint Committee on Health; 25 January 2022; Irish College of General Practice: Dublin, Ireland, 2022. [Google Scholar]
- Groenewegen, P.; Bosmans, M.; Boerma, W. Rural and urban general practice: A comparison in 34 countries. Eur. J. Public Health 2019, 29, ckz185.409. [Google Scholar] [CrossRef]
- Zhang, D.; Son, H.; Shen, Y.; Chen, Z.; Rajbhandari-Thapa, J.; Li, Y.; Eom, H.; Bu, D.; Mu, L.; Li, G.; et al. Assessment of Changes in Rural and Urban Primary Care Workforce in the United States From 2009 to 2017. JAMA Netw. Open 2020, 3, e2022914. [Google Scholar] [CrossRef] [PubMed]
- Bury, G.; Twomey, L.; Egan, M. General practice nursing: The views and experience of practice nurses and GPs in one county. Ir. J. Med. Sci. 2021, 190, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y. Single-Handed General Practice in Urban Areas of Scotland; University of Glasgow: Glasgow, Scotland, 2009. [Google Scholar]


| Characteristics | Rural | Post Graduate Training Centre | GMS Patients | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GPs | All (N = 122) (n, %) | Yes (N = 28) (n, %) | No (N = 94) (n, %) | p Value | All (N = 118) (n, %) | Yes (N = 68) (n, %) | No (N = 50) (n, %) | p Value | All (N = 111) (n, %) | ≤1500 (N = 50) (n, %) | >1500 (N = 61) (n, %) | p Value |
| 1 GP (doctor) | 25 (20.5) | 12 (42.8) | 13 (13.8) | 0.01 | 23 (19.5) | 8 (11.8) | 15 (30.0) | <0.05 * | 20 (18.0) | 17 (34.0) | 3 (4.9) | 0.001 |
| 2–3 GPs | 70 (57.4) | 12 (42.8) | 58 (61.7) | 69 (58.5) | 41 (60.3) | 28 (56.0) | 64 (57.7) | 31 (62.0) | 33 (54.2) | |||
| ≥4 GPs | 27 (22.1) | 4 (14.4) | 23 (24.5) | 26 (22.0) | 19 (27.9) | 7 (14.0) | 27 (24.3) | 2 (4.0) | 25 (40.9) | |||
| Practice nurses | All (N = 119) (n, %) | Yes (N = 27) (n, %) | No (N = 92) (n, %) | p Value | All (N = 115) (n, %) | Yes (N = 67) (n, %) | No (N = 48) (n, %) | p Value | All (N = 108) (n, %) | ≤1500 (N = 47) (n, %) | >1500 (N = 61) (n, %) | p Value |
| 1 nurse | 53 (44.5) | 10 (37.0) | 43 (46.7) | 0.63 | 52 (45.2) | 27 (40.3) | 25 (52.1) | 0.12 | 48 (44.4) | 29 (61.7) | 19 (31.1) | 0.001 |
| 2–3 nurses | 56 (47.1) | 14 (51.9) | 42 (45.7) | 54 (46.9) | 32 (47.8) | 22 (45.8) | 50 (46.3) | 18 (38.3) | 32 (52.5) | |||
| ≥4 nurses | 10 (8.4) | 3 (11.1) | 7 (7.6) | 9 (7.9) | 8 (11.9) | 1 (2.1) | 10 (9.3) | 0 (0.0) | 10 (16.4) | |||
| Mean Number of GPs | At Least One Practice Nurse | Rural Location | Single GP | |
|---|---|---|---|---|
| Our study | 3.2 | 95% | 22% | 20.5% |
| Collins et al. [9] | 2.9 | 94% | 18.9% | 18% |
| Total Staff ¶ | More Than 2 Doctors Involve in CDM £ | More Than 2 Nurse Involve in CDM £ | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 OR [CI] | Model 2 OR [CI] | Model 3 OR [CI] | Model 4 OR [CI] | Model 1 PR [CI] | Model 2 PR [CI] | Model 3 PR [CI] | Model 4 PR [CI] | Model 1 PR [CI] | Model 2 PR [CI] | Model 3 PR [CI] | Model 4 PR [CI] | |
| Rural | 1.05 [0.89–1.23] | 0.79 [0.68–0.92] * | 1.01 [0.86–1.19] | 0.34 [0.12–0.97] * | 0.19 [0.06–0.60] * | 0.24 [0.07–0.80] * | 1.91 [0.55–6.21] | 0.82 [0.29–2.23] | 1.85 [0.51–6.64] | |||
| GMS > 1500 patients | 1.92 [1.68–2.20] * | 1.80 [1.58–2.06] * | 1.81 [1.57–2.08] * | 2.12 [1.25–3.61] * | 3.08 [1.59–4.14] * | 2.32 [1.20–4.46] * | 9.47 [2.66–33.78] * | 7.71 [2.32–25.51] * | 9.41 [2.54–34.90] * | |||
| Postgraduate training | 1.43 [1.26–1.62] * | 1.24 [1.09–1.41] * | 1.24 [1.09–1.41] * | 1.92 [1.20–3.06] * | 2.60 [1.08–9.32] * | 2.16 [1.14–4.11] * | 3.65 [1.14–6.14] * | 2.17 [0.78–6.02] | 2.14 [0.76–6.02] | |||
| Equipment | Rural | Post-Graduate Training | GMS Patients | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Yes | No | p Value | All | Yes | No | p Value | All | ≤ 1500 | ≥ 1500 | p Value | |
| 12 lead ECG machine (N = 123) | 113 (91.8) | 28 (24.7) | 85 (75.3) | 0.11 | 110 (89.4) | 66 (60.0) | 44 (40.0) | <0.05 | 102 (82.9) | 45 (44.1) | 57 (55.9) | 0.18 |
| ABP monitor (N = 123) | 122 (99.2) | 28 (22.9) | 94 (77.1) | 0.93 | 119 (96.7) | 68 (57.1) | 51 (42.8) | NA | 111 (90.2) | 51 (45.9) | 60 (54.0) | 0.46 |
| Sphygmomanometer (N = 123) | 121 (98.4) | 28 (23.1) | 93 (76.8) | 0.92 | 117 (95.1) | 67 (57.3) | 50 (42.7) | 0.92 | 110 (89.4) | 51 (46.4) | 59 (53.6) | 0.93 |
| Glucometer (N = 123) | 123 (100.0) | 28 (22.7) | 95 (77.3) | NA | 119 (96.7) | 68 (57.1) | 51 (42.9) | NA | 112 (91.0) | 52 (46.4) | 60 (53.6) | NA |
| Weighing scales (N = 123) | 123 (100.0) | 28 (22.7) | 95 (77.3) | NA | 119 (96.7) | 68 (57.1) | 51 (42.9) | NA | 112 (91.0) | 52 (46.4) | 60 (53.6) | NA |
| Height measurement (N = 123) | 122 (99.2) | 28 (22.9) | 94 (77.1) | 0.96 | 118 (95.9) | 67 (56.8) | 51 (43.2) | 0.92 | 111 (90.2) | 52 (46.8) | 59 (53.1) | 0.94 |
| Peak Flow Meter (N = 122) | 113 (92.6) | 28 (24.8) | 85 (75.2) | 0.12 | 110 (90.2) | 63 (57.3) | 47 (42.7) | 0.75 | 102 (83.6) | 46 (45.1) | 56 (54.9) | 0.73 |
| Spirometry (N = 120) | 57 (47.5) | 13 (22.8) | 44 (77.2) | 0.98 | 54 (45.0) | 36 (66.7) | 18 (33.3) | 0.07 | 50 (41.7) | 16 (32.0) | 34 (68.0) | <0.05 |
| Practice routinely codes for: | ||||||||||||
| Asthma (N = 122) | 110 (90.2) | 26 (23.6) | 84 (76.4) | 0.73 | 108 (88.5) | 66 (61.1) | 42 (38.9) | <0.05 | 101 (82.8) | 46 (45.5) | 55 (54.4) | 0.51 |
| COPD (N = 121) | 111 (91.7) | 27 (24.3) | 84 (75.7) | 0.45 | 108 (89.3) | 64 (59.3) | 44 (40.7) | 0.16 | 102 (84.3) | 48 (47.1) | 54 (52.9) | 0.97 |
| Heart disease (N = 122) | 111 (91.0) | 27 (24.3) | 84 (75.7) | 0.45 | 108 (88.5) | 64 (59.3) | 44 (40.7) | 0.32 | 101 (82.8) | 48 (47.5) | 53 (52.5) | 0.75 |
| Diabetes (N = 122) | 114 (93.4) | 27 (23.7) | 87 (76.3) | 0.68 | 111 (91.0) | 66 (59.5) | 45 (40.5) | 0.13 | 104 (85.2) | 49 (47.1) | 55 (52.9) | 0.95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tandan, M.; Twomey, B.; Twomey, L.; Egan, M.; Bury, G. National Chronic Disease Management Programmes in Irish General Practice-Preparedness and Challenges. J. Pers. Med. 2022, 12, 1157. https://doi.org/10.3390/jpm12071157
Tandan M, Twomey B, Twomey L, Egan M, Bury G. National Chronic Disease Management Programmes in Irish General Practice-Preparedness and Challenges. Journal of Personalized Medicine. 2022; 12(7):1157. https://doi.org/10.3390/jpm12071157
Chicago/Turabian StyleTandan, Meera, Bebhinn Twomey, Liam Twomey, Mairead Egan, and Gerard Bury. 2022. "National Chronic Disease Management Programmes in Irish General Practice-Preparedness and Challenges" Journal of Personalized Medicine 12, no. 7: 1157. https://doi.org/10.3390/jpm12071157
APA StyleTandan, M., Twomey, B., Twomey, L., Egan, M., & Bury, G. (2022). National Chronic Disease Management Programmes in Irish General Practice-Preparedness and Challenges. Journal of Personalized Medicine, 12(7), 1157. https://doi.org/10.3390/jpm12071157






