Quantifying Spatial Heterogeneity of Tumor-Infiltrating Lymphocytes to Predict Survival of Individual Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Data Preprocessing
2.3. Methods for Spatial Structure Analysis (Spatial Measures)
2.3.1. Methods Developed for Analysis of Spatial Molecular Data
2.3.2. Clustering-Based Methods
2.3.3. Other Methods
2.4. Survival Analysis
2.5. Statistical Analysis
3. Results
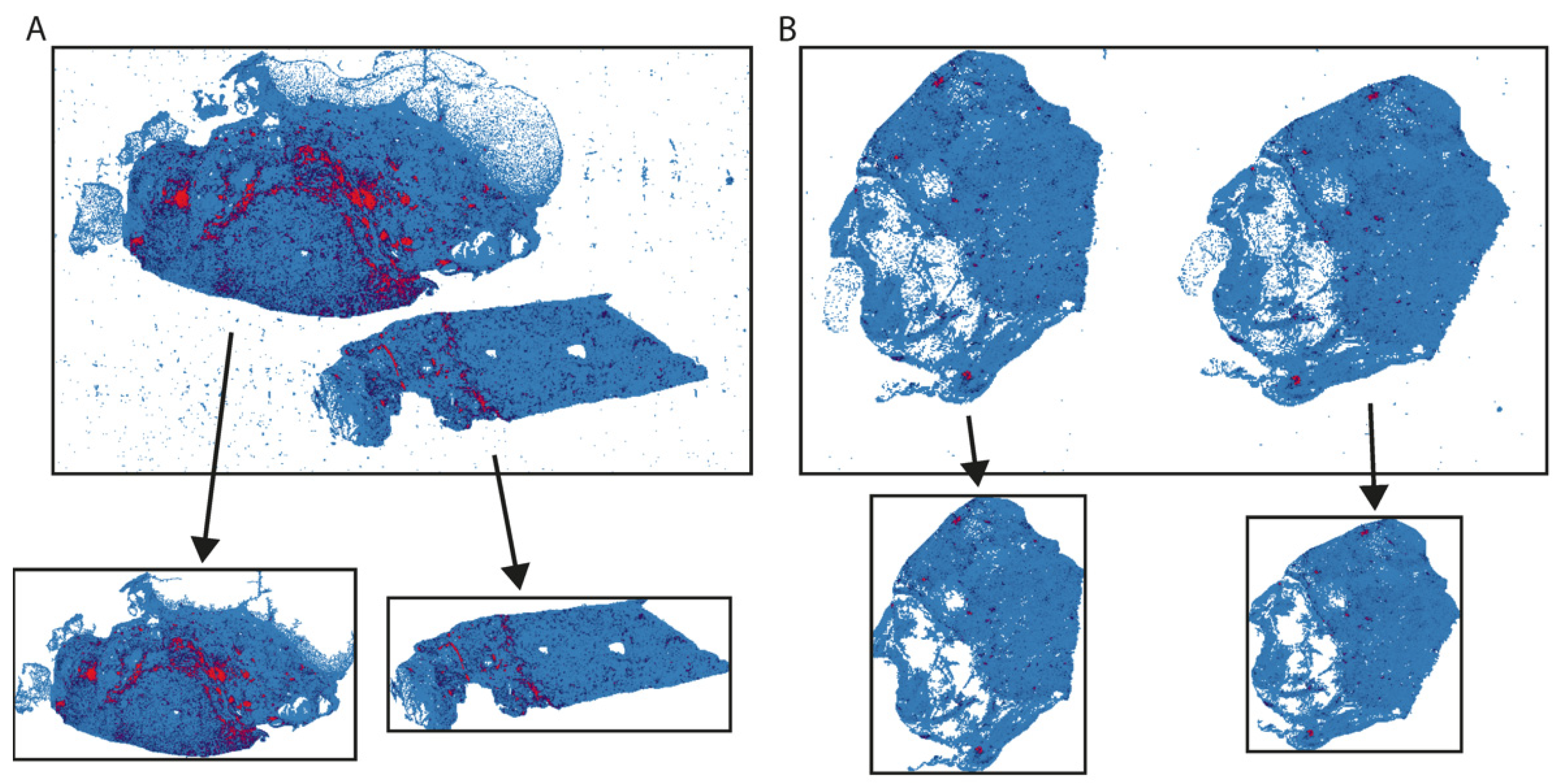
3.1. Definition of Region-of-Interest (ROI)
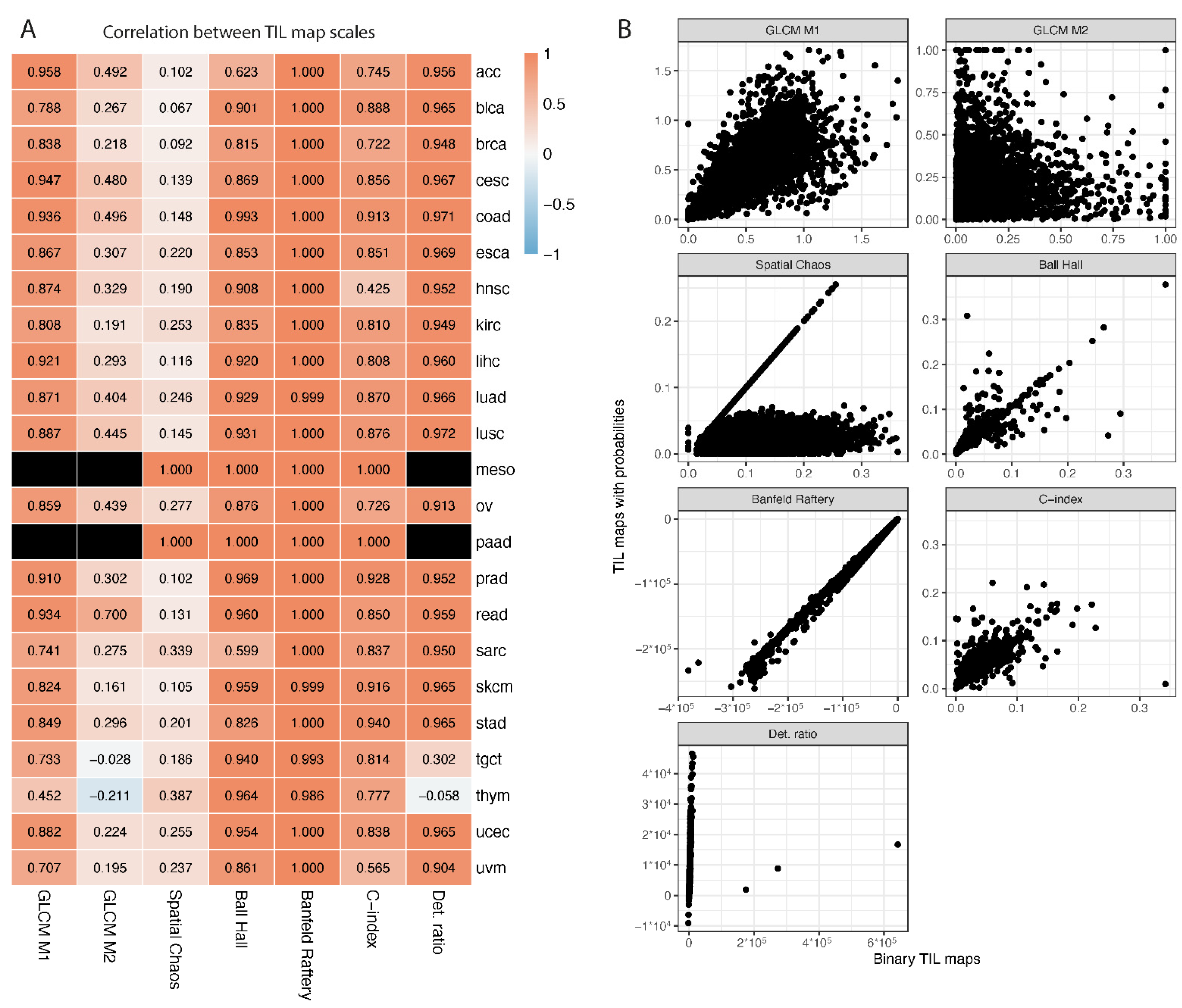
3.2. Different Representation of TIL Maps
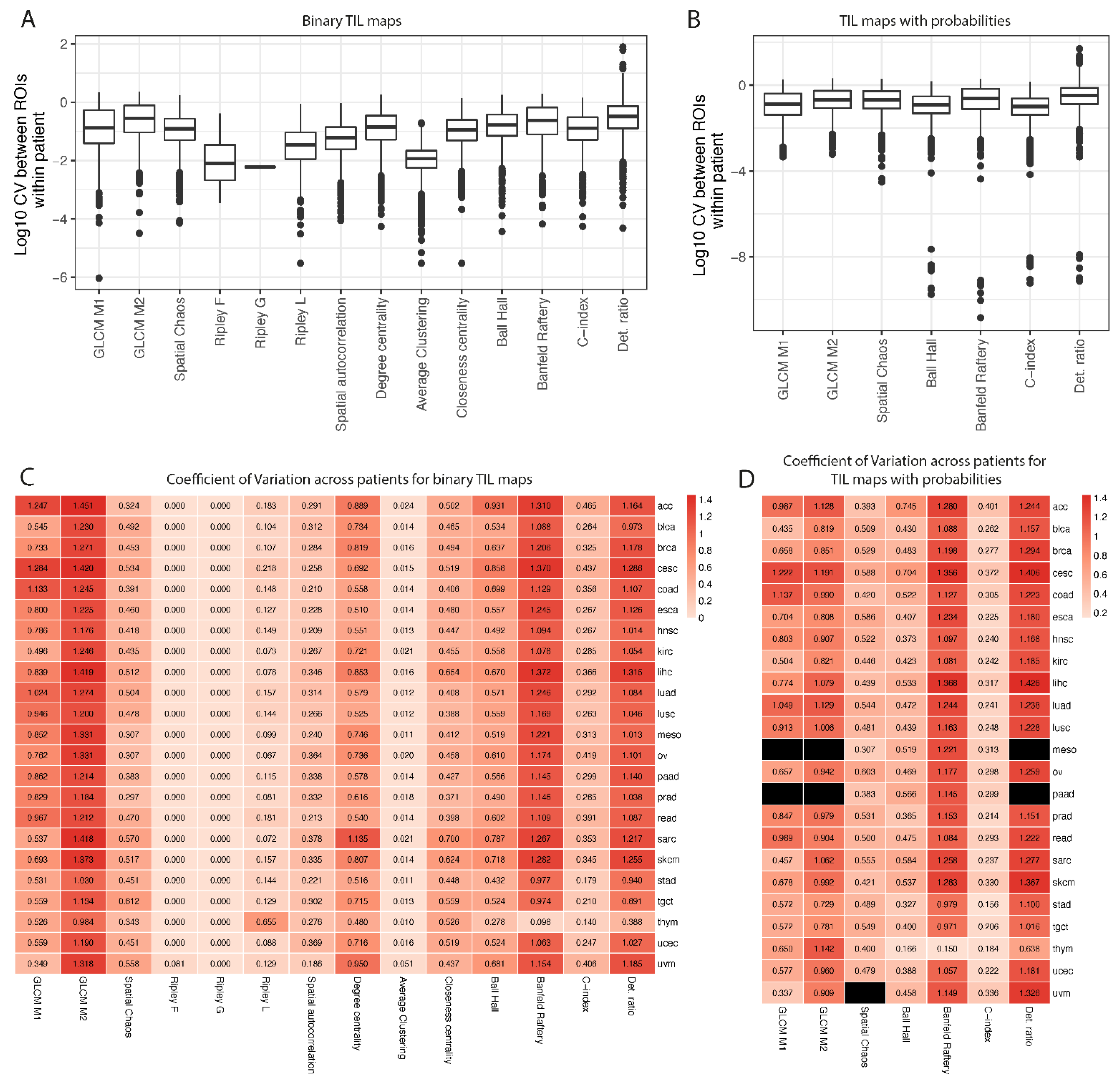
3.3. Reproducibility of Spatial Measures across ROIs and Variation across Patients
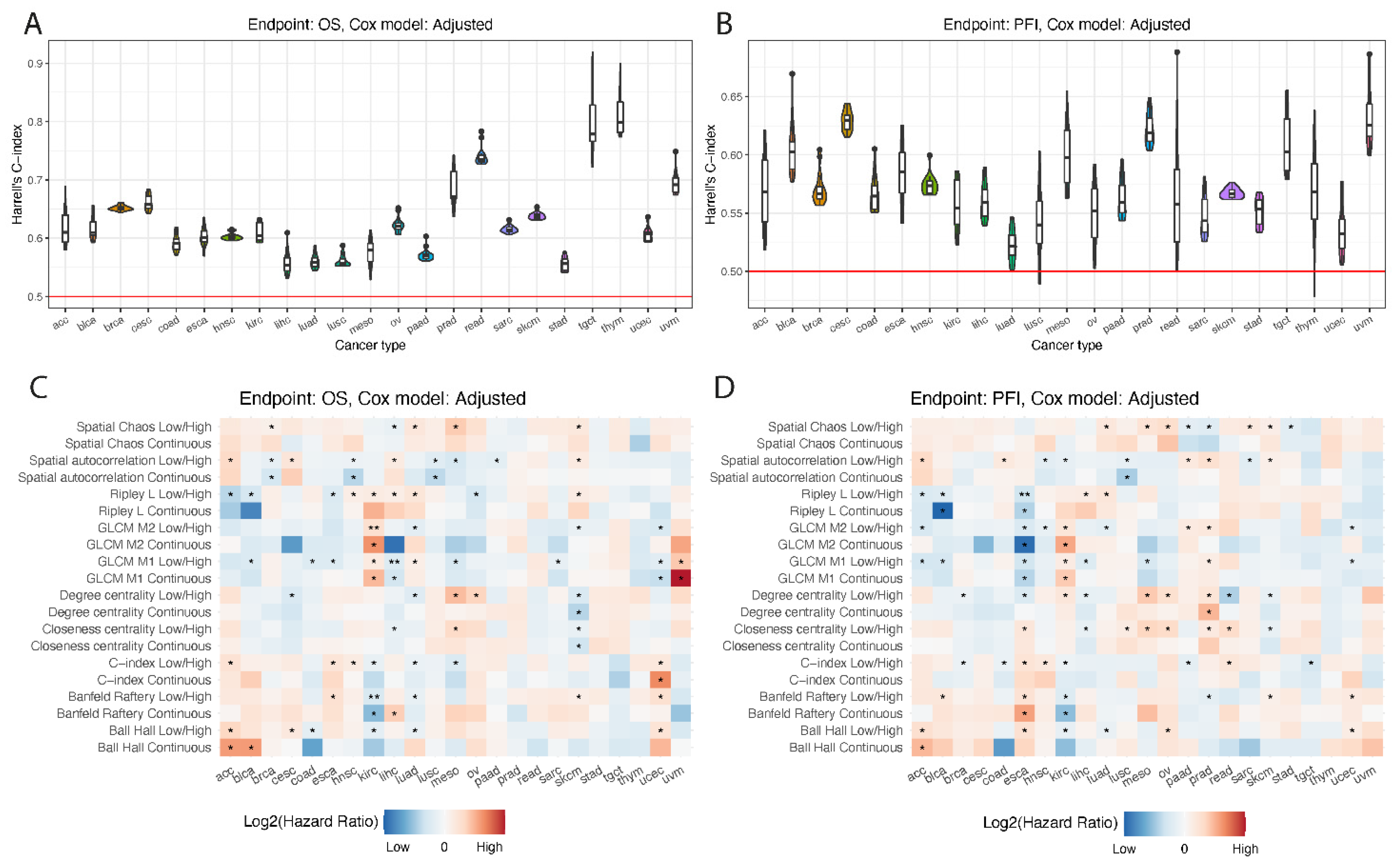
3.4. Survival Prediction by Different Measures in Cancer Patients
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delhalle, S.; Bode, S.; Balling, R.; Ollert, M.; He, F.Q. A roadmap towards personalized immunology. NPJ Syst. Biol. Appl. 2018, 4, 9. [Google Scholar] [CrossRef]
- Binnewies, M.; Roberts, E.W.; Kersten, K.; Chan, V.; Fearon, D.F.; Merad, M.; Coussens, L.M.; Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Hedrick, C.C.; et al. Understanding the Tumor Immune Microenvironment (Time) for Effective Therapy. Nat. Med. 2018, 24, 541–550. [Google Scholar] [CrossRef]
- Denkert, C.; Wienert, S.; Poterie, A.; Loibl, S.; Budczies, J.; Badve, S.; Bago-Horvath, Z.; Bane, A.; Bedri, S.; Brock, J.; et al. Standardized Evaluation of Tumor-Infiltrating Lymphocytes in Breast Cancer: Results of the Ring Studies of the International Immuno-Oncology Biomarker Working Group. Mod. Pathol. 2016, 29, 1155–1164. [Google Scholar] [CrossRef]
- Salgado, R.; Loi, S. Tumour infiltrating lymphocytes in breast cancer: Increasing clinical relevance. Lancet Oncol. 2018, 19, 3–5. [Google Scholar] [CrossRef]
- Loi, S.; Drubay, D.; Adams, S.; Pruneri, G.; Francis, P.A.; Lacroix-Triki, M.; Joensuu, H.; Dieci, M.V.; Badve, S.; Demaria, S.; et al. Tumor-Infiltrating Lymphocytes and Prognosis: A Pooled Individual Patient Analysis of Early-Stage Triple-Negative Breast Cancers. J. Clin. Oncol. 2019, 37, 559–569. [Google Scholar] [CrossRef]
- Brambilla, E.; Le Teuff, G.; Marguet, S.; Lantuejoul, S.; Dunant, A.; Graziano, S.; Pirker, R.; Douillard, J.-Y.; Le Chevalier, T.; Filipits, M.; et al. Prognostic Effect of Tumor Lymphocytic Infiltration in Resectable Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2016, 34, 1223–1230. [Google Scholar] [CrossRef]
- Antohe, M.; Nedelcu, R.I.; Nichita, L.; Popp, C.G.; Cioplea, M.; Brinzea, A.; Hodorogea, A.; Calinescu, A.; Balaban, M.; Ion, D.; et al. Tumor infiltrating lymphocytes: The regulator of melanoma evolution (Review). Oncol. Lett. 2019, 17, 4155–4161. [Google Scholar] [CrossRef]
- Haddad, R.; Zlotnik, O.; Goshen-Lago, T.; Levi, M.; Brook, E.; Brenner, B.; Kundel, Y.; Ben-Aharon, I.; Kashtan, H. Tumor Lymphocyte Infiltration Is Correlated with a Favorable Tumor Regression Grade after Neoadjuvant Treatment for Esophageal Adenocarcinoma. J. Pers. Med. 2022, 12, 627. [Google Scholar] [CrossRef]
- Dieci, M.V.; Radosevic-Robin, N.; Fineberg, S.; Van den Eynden, G.; Ternes, N.; Penault-Llorca, F.; Pruneri, G.; D’Alfonso, T.M.; Demaria, S.; Castaneda, C.; et al. Update on Tumor-Infiltrating Lymphocytes (Tils) in Breast Cancer, Including Recommendations to Assess Tils in Residual Disease after Neoadjuvant Therapy and in Carcinoma in Situ: A Report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin. Cancer Biol. 2018, 52, 16–25. [Google Scholar]
- Saltz, J.; Gupta, R.; Hou, L.; Kurc, T.; Singh, P.; Nguyen, V.; Samaras, D.; Shroyer, K.R.; Zhao, T.; Batiste, R.; et al. Spatial Organization and Molecular Correlation of Tumor-Infiltrating Lymphocytes Using Deep Learning on Pathology Images. Cell Rep. 2018, 23, 181–193.e7. [Google Scholar] [CrossRef]
- Gruosso, T.; Gigoux, M.; Manem, V.S.K.; Bertos, N.; Zuo, D.; Perlitch, I.; Saleh, S.M.I.; Zhao, H.; Souleimanova, M.; Johnson, R.M.; et al. Spatially Distinct Tumor Immune Microenvironments Stratify Triple-Negative Breast Cancers. J. Clin. Investig. 2019, 129, 1785–1800. [Google Scholar] [CrossRef]
- Abousamra, S.; Gupta, R.; Hou, L.; Batiste, R.; Zhao, T.; Shankar, A.; Rao, A.; Chen, C.; Samaras, D.; Kurc, T.; et al. Deep Learning-Based Mapping of Tumor Infiltrating Lymphocytes in Whole Slide Images of 23 Types of Cancer. Front. Oncol. 2022, 11, 806603. [Google Scholar] [CrossRef]
- PPalla, G.; Spitzer, H.; Klein, M.; Fischer, D.; Schaar, A.C.; Kuemmerle, L.B.; Rybakov, S.; Ibarra, I.L.; Holmberg, O.; Virshup, I.; et al. Squidpy: A scalable framework for spatial omics analysis. Nat. Methods 2022, 19, 171–178. [Google Scholar] [CrossRef]
- Frey, B.J.; Delbert, D. Clustering by Passing Messages between Data Points. Science 2007, 315, 972–976. [Google Scholar] [CrossRef]
- Ramola, A.; Shakya, A.K.; Van Pham, D. Study of statistical methods for texture analysis and their modern evolutions. Eng. Rep. 2020, 2, e12149. [Google Scholar] [CrossRef]
- Wijetunge, C.D.; Saeed, I.; Boughton, B.A.; Spraggins, J.M.; Caprioli, R.M.; Bacic, A.; Roessner, U.; Halgamuge, S.K. Exims: An Improved Data Analysis Pipeline Based on a New Peak Picking Method for Exploring Imaging Mass Spectrometry Data. Bioinformatics 2015, 31, 3198–3206. [Google Scholar] [CrossRef][Green Version]
- Alexandrov, T.; Bartels, A. Testing for presence of known and unknown molecules in imaging mass spectrometry. Bioinformatics 2013, 29, 2335–2342. [Google Scholar] [CrossRef]
- Miller, R.; Siegmund, D. Maximally Selected Chi Square Statistics. Biometrics 1982, 38, 1011–1016. [Google Scholar] [CrossRef]
- Mazumdar, M.; Glassman, J.R. Categorizing a Prognostic Variable: Review of Methods, Code for Easy Implementation and Applications to Decision-Making About Cancer Treatments. Stat. Med. 2000, 19, 113–132. [Google Scholar] [CrossRef]
- Klauschen, F.; Müller, K.-R.; Binder, A.; Bockmayr, M.; Hägele, M.; Seegerer, P.; Wienert, S.; Pruneri, G.; de Maria, S.; Badve, S.; et al. Scoring of tumor-infiltrating lymphocytes: From visual estimation to machine learning. Semin. Cancer Biol. 2018, 52, 151–157. [Google Scholar] [CrossRef]
- Corredor, G.; Wang, X.; Zhou, Y.; Lu, C.; Fu, P.; Syrigos, K.N.; Rimm, D.L.; Yang, M.; Romero, E.; Schalper, K.A.; et al. Spatial Architecture and Arrangement of Tumor-Infiltrating Lymphocytes for Predicting Likelihood of Recurrence in Early-Stage Non–Small Cell Lung Cancer. Clin. Cancer Res. 2019, 25, 1526–1534. [Google Scholar] [CrossRef] [PubMed]
- Fassler, D.J.; Torre-Healy, L.A.; Gupta, R.; Hamilton, A.M.; Kobayashi, S.; Van Alsten, S.C.; Zhang, Y.; Kurc, T.; Moffitt, R.A.; Troester, M.A.; et al. Spatial Characterization of Tumor-Infiltrating Lymphocytes and Breast Cancer Progression. Cancers 2022, 14, 2148. [Google Scholar] [CrossRef] [PubMed]
- Corredor, G.; Toro, P.; Koyuncu, C.; Lu, C.; Buzzy, C.; Bera, K.; Fu, P.; Mehrad, M.; Ely, K.A.; Mokhtari, M.; et al. An Imaging Biomarker of Tumor-Infiltrating Lymphocytes to Risk-Stratify Patients With HPV-Associated Oropharyngeal Cancer. JNCI: J. Natl. Cancer Inst. 2022, 114, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Azarianpour, S.; Corredor, G.; Bera, K.; Leo, P.; Fu, P.; Toro, P.; Joehlin-Price, A.; Mokhtari, M.; Mahdi, H.; Madabhushi, A. Computational image features of immune architecture is associated with clinical benefit and survival in gynecological cancers across treatment modalities. J. Immunother. Cancer 2022, 10, e003833. [Google Scholar] [CrossRef] [PubMed]

| Cancer | Acronym | Patients | TIL Maps | ROIs |
|---|---|---|---|---|
| Adrenocortical carcinoma | acc | 92 | 323 | 391 |
| Bladder urothelial carcinoma | blca | 179 | 179 | 223 |
| Breast invasive carcinoma | brca | 1067 | 1068 | 1312 |
| Cervical squamous cell carcinoma and endocervical adenocarcinoma | cesc | 268 | 268 | 526 |
| Colon adenocarcinoma | coad | 452 | 453 | 630 |
| Esophageal carcinoma | esca | 156 | 156 | 223 |
| Head and neck squamous cell carcinoma | hnsc | 450 | 450 | 698 |
| Kidney renal clear cell carcinoma | kirc | 513 | 514 | 626 |
| Liver hepatocellular carcinoma | lihc | 365 | 365 | 490 |
| Lung adenocarcinoma | luad | 479 | 480 | 662 |
| Lung squamous cell carcinoma | lusc | 484 | 484 | 655 |
| Mesothelioma | meso | 87 | 175 | 347 |
| Ovarian serous cystadenocarcinoma | ov | 106 | 106 | 180 |
| Pancreatic adenocarcinoma | paad | 183 | 189 | 253 |
| Prostate adenocarcinoma | prad | 403 | 403 | 548 |
| Rectum adenocarcinoma | read | 165 | 165 | 251 |
| Sarcoma | sarc | 255 | 255 | 316 |
| Skin cutaneous melanoma | skcm | 434 | 448 | 611 |
| Stomach adenocarcinoma | stad | 434 | 434 | 454 |
| Testicular germ cell tumors | tgct | 149 | 154 | 190 |
| Thymoma | thym | 121 | 121 | 152 |
| Uterine corpus endometrial carcinoma | ucec | 504 | 506 | 699 |
| Uveal melanoma | uvm | 80 | 80 | 95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suwalska, A.; Zientek, L.; Polanska, J.; Marczyk, M. Quantifying Spatial Heterogeneity of Tumor-Infiltrating Lymphocytes to Predict Survival of Individual Cancer Patients. J. Pers. Med. 2022, 12, 1113. https://doi.org/10.3390/jpm12071113
Suwalska A, Zientek L, Polanska J, Marczyk M. Quantifying Spatial Heterogeneity of Tumor-Infiltrating Lymphocytes to Predict Survival of Individual Cancer Patients. Journal of Personalized Medicine. 2022; 12(7):1113. https://doi.org/10.3390/jpm12071113
Chicago/Turabian StyleSuwalska, Aleksandra, Lukasz Zientek, Joanna Polanska, and Michal Marczyk. 2022. "Quantifying Spatial Heterogeneity of Tumor-Infiltrating Lymphocytes to Predict Survival of Individual Cancer Patients" Journal of Personalized Medicine 12, no. 7: 1113. https://doi.org/10.3390/jpm12071113
APA StyleSuwalska, A., Zientek, L., Polanska, J., & Marczyk, M. (2022). Quantifying Spatial Heterogeneity of Tumor-Infiltrating Lymphocytes to Predict Survival of Individual Cancer Patients. Journal of Personalized Medicine, 12(7), 1113. https://doi.org/10.3390/jpm12071113







