Embolization of Recurrent Pulmonary Arteriovenous Malformations by Ethylene Vinyl Alcohol Copolymer (Onyx®) in Hereditary Hemorrhagic Telangiectasia: Safety and Efficacy
Abstract
:1. Introduction
2. Materials and Methods
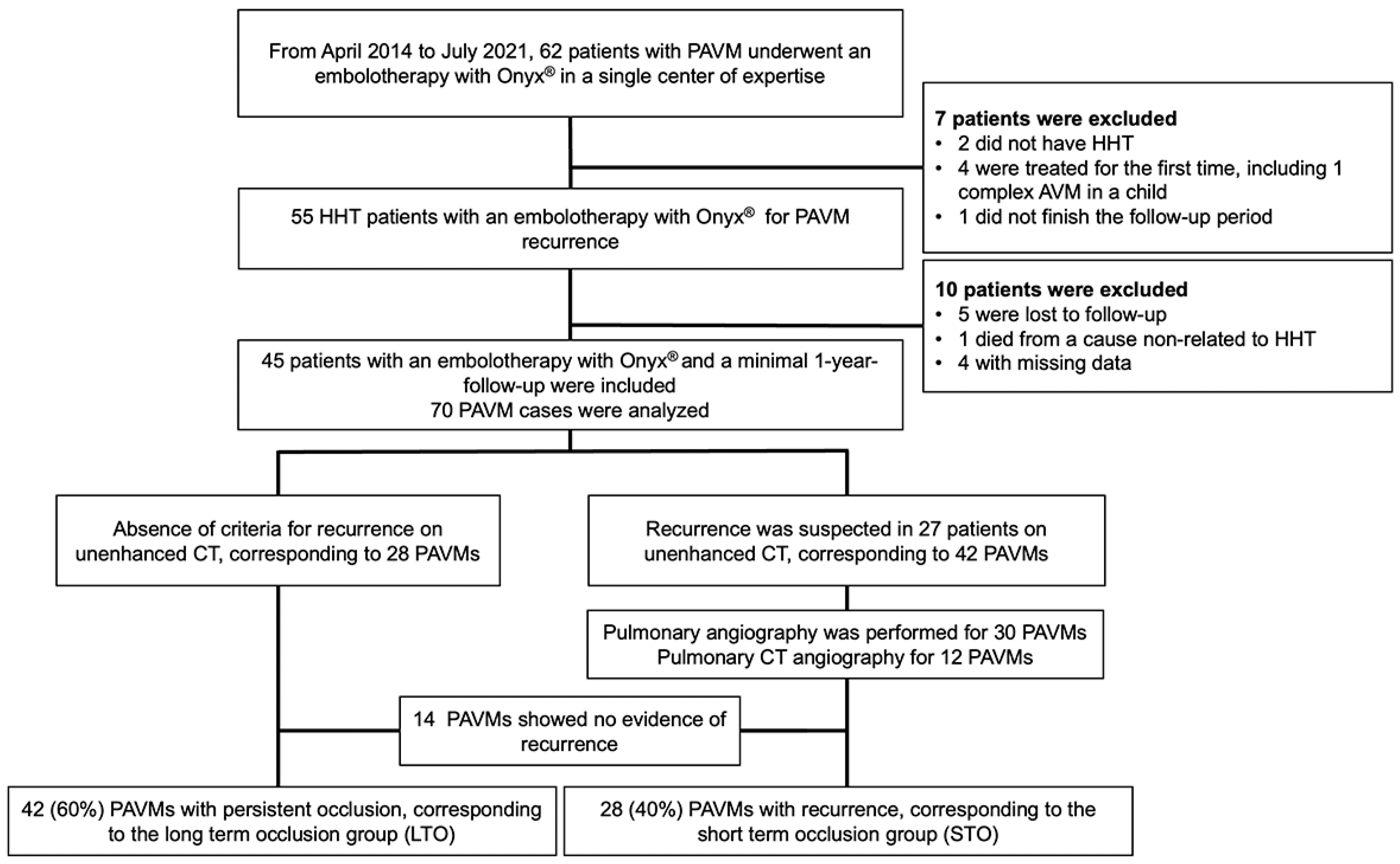
2.1. Study Design
2.2. Study Population
2.3. Clinical and Biological Data
2.4. Follow-Up Imaging Protocol
2.5. Pulmonary Arteriovenous Malformation Imaging
2.6. Embolization
2.7. Statistical Analysis
3. Results
3.1. Study Population
3.2. PAVM Characteristics before Embolization
3.3. Safety
3.4. Short-Term Efficacy
3.5. Long-Term Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Shovlin, C.L.; Guttmacher, A.E.; Buscarini, E.; Faughnan, M.E.; Hyland, R.H.; Westermann, C.J.; Kjeldsen, A.D.; Plauchu, H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Ren-du-Osler-Weber syndrome). Am. J. Med. Genet. 2000, 91, 66–67. [Google Scholar] [CrossRef]
- Berg, J.N.; Guttmacher, A.E.; Marchuk, D.A.; Porteous, M.E. Clinical heterogeneity in hereditary haemorrhagic telangiectasia: Are pulmonary arteriovenous malformations more common in families linked to endoglin? J. Med. Genet. 1996, 33, 256–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Etievant, J.; Si-Mohamed, S.; Vinurel, N.; Dupuis-Girod, S.; Decullier, E.; Gamondes, D.; Khouatra, C.; Cottin, V.; Revel, D. Pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia: Correlations between computed tomography findings and cerebral complications. Eur. Radiol. 2018, 28, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.L.; Jackson, J.E.; Bamford, K.B.; Jenkins, I.H.; Benjamin, A.R.; Ramadan, H.; Kulinskaya, E. Primary determinants of ischaemic stroke/brain abscess risks are independent of severity of pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia. Thorax 2008, 63, 259–266. [Google Scholar] [CrossRef] [Green Version]
- Cottin, V.; Chinet, T.; Lavolé, A.; Corre, R.; Marchand, E.; Reynaud-Gaubert, M.; Plauchu, H.; Cordier, J.-F. Pulmonary Arteriovenous Malformations in Hereditary Hemorrhagic Telangiectasia: A series of 126 patients. Medicine 2007, 86, 1–17. [Google Scholar] [CrossRef]
- Dupuis-Girod, S.; Cottin, V.; Shovlin, C. The Lung in Hereditary Hemorrhagic Telangiectasia. Respiration 2017, 94, 315–330. [Google Scholar] [CrossRef]
- Shovlin, C.; Condliffe, R.; Donaldson, J.W.; Kiely, D.G.; Wort, S.J. British Thoracic Society Clinical Statement on Pulmonary Arteriovenous Malformations. Thorax 2017, 72, 1154–1163. [Google Scholar] [CrossRef] [Green Version]
- Gamondès, D.; Si-Mohamed, S.; Cottin, V.; Gonidec, S.; Boussel, L.; Douek, P.; Revel, D. Vein Diameter on Unenhanced Multidetector CT Predicts Reperfusion of Pulmonary Arteriovenous Malformation after Embolotherapy. Eur. Radiol. 2016, 26, 2723–2729. [Google Scholar] [CrossRef]
- Remy-Jardin, M.; Dumont, P.; Brillet, P.-Y.; Dupuis, P.; Duhamel, A.; Remy, J. Pulmonary Arteriovenous Malformations Treated with Embolotherapy: Helical CT Evaluation of Long-term Effectiveness after 2–21-Year Follow-up 1. Radiology 2006, 239, 576–585. [Google Scholar] [CrossRef]
- Woodward, C.S.; Pyeritz, R.E.; Chittams, J.L.; Trerotola, S.O. Treated Pulmonary Arteriovenous Malformations: Patterns of Persistence and Associated Retreatment Success. Vasc. Interv. Radiol. 2013, 269, 8. [Google Scholar] [CrossRef]
- Cusumano, L.R. Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique. Cardiovasc. Interv. Radiol. 2020, 43, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Milic, A.; Chan, R.P.; Cohen, J.H.; Faughnan, M.E. Reperfusion of Pulmonary Arteriovenous Malformations after Embolotherapy. J. Vasc. Interv. Radiol. 2005, 16, 1675–1683. [Google Scholar] [CrossRef] [PubMed]
- Szajner, M.; Roman, T.; Markowicz, J.; Szczerbo-Trojanowska, M. Onyx® in endovascular treatment of cerebral arteriovenous malformations—A review. Pol. J. Radiol. 2013, 78, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kilani, M.S.; Izaaryene, J.; Cohen, F.; Varoquaux, A.; Gaubert, J.; Louis, G.; Jacquier, A.; Bartoli, J.; Moulin, G.; Vidal, V. Ethylene vinyl alcohol copolymer (Onyx®) in peripheral interventional radiology: Indications, advantages and limitations. Diagn. Interv. Imaging 2015, 96, 319–326. [Google Scholar] [CrossRef]
- Pollak, J.S.; Saluja, S.; Thabet, A.; Henderson, K.J.; Denbow, N.; White, R.I. Clinical and anatomic outcomes after embolotherapy of pulmonary arteriovenous malformations. J. Vasc. Interv. Radiol. 2006, 17, 35–45. [Google Scholar] [CrossRef] [Green Version]
- White, R.I. Pulmonary arteriovenous malformations: How do we diagnose them and why is it important to do so? Radiology 1992, 182, 633–635. [Google Scholar] [CrossRef]
- Stein, E.J.; Chittams, J.L.; Miller, M.; Trerotola, S.O. Persistence in Coil-Embolized Pulmonary Arteriovenous Malformations with Feeding Artery Diameters of 3 mm or Less: A Retrospective Single-Center Observational Study. J. Vasc. Interv. Radiol. 2017, 28, 442–449. [Google Scholar] [CrossRef]
- Shimohira, M.; Kiyosue, H.; Osuga, K.; Gobara, H.; Kondo, H.; Nakazawa, T.; Matsui, Y.; Hamamoto, K.; Ishiguro, T.; Maruno, M.; et al. Location of embolization affects patency after coil embolization for pulmonary arteriovenous malformations: Importance of time-resolved magnetic resonance angiography for diagnosis of patency. Eur. Radiol. 2021, 31, 5409–5420. [Google Scholar] [CrossRef]
- Brill, R.M.; Guntau, M.; Wildgruber, M.; Brill, E.; Stangl, F.; Taute, B.-M.; Ukkat, J.; Goldann, C.; Wohlgemuth, W.A. Safety and Effectiveness of Ethylene Vinyl Alcohol Copolymer Embolization of Peripheral High-Flow Arteriovenous Malformations: Results of a Prospective Study. J. Vasc. Interv. Radiol. 2021, 32, 1644–1653.e1. [Google Scholar] [CrossRef]
- Shi, Z.-S.; Loh, Y.; Gonzalez, N.; Tateshima, S.; Feng, L.; Jahan, R.; Duckwiler, G.; Viñuela, F. Flow control techniques for Onyx embolization of intracranial dural arteriovenous fistulae. J. NeuroInterventional Surg. 2013, 5, 311–316. [Google Scholar] [CrossRef]
- Brillet, P.-Y.; Dumont, P.; Bouaziz, N.; Duhamel, A.; Laurent, F.; Remy, J.; Remy-Jardin, M. Pulmonary arteriovenous malformation treated with embolotherapy: Systemic collateral supply at multidetector ct angiography after 2–20-year follow-up. Radiology 2007, 242, 267–276. [Google Scholar] [CrossRef] [PubMed]





| Population | 45 | |
|---|---|---|
| Women | 23 (51) | |
| Mean age (SD) (years) | 53 (18) | |
| Mean BMI (SD) | 25.8 (6.2) | |
| Diabetes mellitus | 4 (9) | |
| Tobacco | 18 (40) | |
| Mean oxygen saturation (range) | 96.3 (92–100) | |
| Curacao criteria | ||
| Family history of HHT symptoms | 45 | |
| Epistaxis | 43 (96) | |
| Telangiectasia | 41 (91) | |
| Liver AVM | 7 (16) | |
| Gastro-intestinal AVM | 5 (11) | |
| Brain AVM | 3 (7) | |
| HHT severe complications | ||
| Hemoptysis | 3 (7) | |
| Brain abscess | 5 (11) | |
| Stroke | 7 (16) | |
| Mutation | ||
| HHT1/ENG | 36 (80) | |
| HHT2/ALK1 | 5 (11) | |
| SMAD4 | 0 (0) | |
| Unknown/unconfirmed | 4 (9) | |
| Unique PAVM | 18 (40) | |
| Multiple PAVM | 27 (60) |
| Criteria | Total | Long-Term Occlusion | Short-Term Occlusion | p | |
|---|---|---|---|---|---|
| Previous procedures | 70 (100) | 42 (60) | 28 (40) | NA | |
| PAVMs naive from Onyx® | 64 (91) | 40 (95) | 24 (86) | 0.166 | |
| PAVMs previously treated with Onyx® | 6 (9) | 2 (5) | 4 (14) | 0.166 | |
| Simple PAVMs | 61 (87) | 36 (86) | 25 (89) | 0.664 | |
| Complex PAVMs | 9 (14) | 6 (15) | 3 (13) | 0.664 | |
| Mean number of embolizations before onyx per PAVM (SD) | 2.0 (1.1) | 1.8 (1.1) | 2.5 (1.3) | 0.01 | |
| Mean number of recurrence before Onyx® per PAVM | 0.9 (1.1) | 0.7 (1.0) | 1.4 (1.2) | <0.01 | |
| PAVMs first treated with coils | 70 (100) | 42 (100) | 28 (100) | 1.00 | |
| PAVMs first treated with plugs and coils | 2 (3) | 2 (5) | 0 | 0.245 | |
| Length between aneurysm and plug/coil < 10 mm | 43 (61) | 27 (64) | 16 (57) | 0.550 | |
| Vein diameter (mm) | 4.2 (3.7) | 3.4 (1.0) | 5.5 (5.6) | <0.01 | |
| Aneurysm diameter (mm) | 5.1 (5.4) | 3.4 (4.1) | 8 (6.1) | <0.01 | |
| Lobar location | |||||
| Upper right lobe | 13 (19) | 9 (21) | 4 (14) | 0.455 | |
| Middle lobe | 7 (10) | 4 (10) | 3 (11) | 0.872 | |
| Lower right lobe | 22 (31) | 11 (26) | 11 (39) | 0.251 | |
| Upper left lobe | 6 (9) | 5 (12) | 1 (4) | 0.226 | |
| Lower left lobe | 22 (31) | 13 (31) | 9 (32) | 0.917 | |
| Absence of safety distance | 33 (47) | 17 (60) | 16 (43) | 0.174 | |
| Mechanism of recurrence | |||||
| Recanalization | 69 (98) | 41 (98) | 28 (100) | 0.414 | |
| Reperfusion | 10 (14) | 7 (17) | 3 (11) | 0.489 | |
| Both | 9 (13) | 6 (67) | 3 (23) | 0.664 | |
| Incomplete primary treatment | 0 | 0 | 0 | 1.000 | |
| Territory potentially at risk | |||||
| Lobar | 2 (3) | 1 (2) | 1 (4) | 0.771 | |
| Segmental | 18 (26) | 9 (21) | 9 (32) | 0.318 | |
| Sub-segmental | 50 (71) | 32 (76) | 18 (64) | 0.284 | |
| Immediate Embolization Characteristics | Total | Long-Term Occlusion | Short-Term Occlusion | p | |
|---|---|---|---|---|---|
| Per-embolization occlusion | 70 (100) | 42 (60) | 28 (40) | 1.00 | |
| Treatment type | |||||
| Onyx® only | 53 (76) | 31 (74) | 22 (79) | 0.65 | |
| Onyx® + coils | 17(24) | 11 (26) | 6 (21) | 0.65 | |
| Onyx® volume, mL (SD) | 0.6 (0.5) | 0.5 (0.3) | 0.7 (0.6) | 0.23 | |
| Onyx® distribution ** | |||||
| Upstream | 48 (69) | 30 (71) | 18 (64) | 0.53 | |
| Inside coiling | 51 (73) | 28 (67) | 23 (82) | 0.16 | |
| Downstream | 13 (19) | 7 (17) | 6 (21) | 0.62 | |
| Upstream + inside | 29 (41) | 16 (38) | 13 (46) | 0.49 | |
| Downstream + inside | 13 (19) | 7 (17) | 6 (21) | 0.62 | |
| Upstream + inside + downstream | 5 (7) | 2 (5) | 3 (11) | 0.35 | |
| Upstream leak outside the target | |||||
| At a lobar level | 0 | 0 | 0 | 1.00 | |
| At a segmental level | 4 (6) | 2 (5) | 2 (7) | 1.00 | |
| At a sub-segmental level | 39 (56) | 25 (60) | 14 (50) | 0.68 | |
| Perfusion defect in healthy territory | |||||
| Lobar territory | 0 | 0 | 0 | 1.00 | |
| Segmental territory | 0 | 0 | 0 | 1.00 | |
| Sub-segmental territory | 20 (29) | 13 (31) | 7 (25) | 0.59 | |
| Downstream leak in draining vein or aneurysmal sac | 0 | 0 | 0 | 1.00 | |
| Downstream leak in systemic circulation | 0 | 0 | 0 | 1.00 | |
| Procedure time, min (SD) | 105 (34) | 110 (33) | 99 (35) | 0.15 | |
| Volume of contrast agent, mL (SD) | 110 (49) | 116 (50) | 102 (47) | 0.19 | |
| Adverse events during hospitalization time | 5 (7.1) | 2 (2.8) | 3 (4.3) | 0.35 | |
| Allergy | 1 (20) | 0 | 1 (33.3) | 0.22 | |
| Chest pain | 1 (20) | 0 | 1 (33.3) | 0.22 | |
| Pleural effusion | 0 | 0 | 0 | 1.00 | |
| Lung distal infarction | 3 (60) | 2 (100) | 1 (33.3) | 0.81 | |
| Lung infection | 0 | 0 | 0 | 1.00 | |
| Brain abscess | 0 | 0 | 0 | 1.00 | |
| Stroke | 0 | 0 | 0 | 1.00 | |
| Access site complication | 0 | 0 | 0 | 1.00 | |
| Long Time Follow-Up | Total | Long-Term Occlusion | Short-Term Occlusion | p | |
|---|---|---|---|---|---|
| Number of PAVMs | 70 (100) | 42 (60) | 28 (40) | ||
| Follow-up time, months (SD) | 34.8 (15.3) | 25.2 (13.0) | 34.1 (16.7) | 0.5 | |
| Tobacco consumption | 28 (40) | 14 (33.3) | 14 (50) | 0.111 | |
| Pack-year of tobacco (SD) | 9.3 (17.3) | 8.8 (2.8) | 11.8 (3.1) | 0.133 | |
| PAVM characteristics | |||||
| Aneurysm diameter, mm (SD) | 3.9 (4.7) | 2.1 (3.2) | 7.0 (5.1) | <0.001 | |
| Vein diameter, mm (SD) | 2.9 (1.2) | 2.4 (0.9) | 3.8 (1.0) | <0.001 | |
| Difference in aneurysm diameter, mm (SD) * | 22.9 (37.2) | 40.5 (39.1) | 4.4 (24.4) | <0.01 | |
| Difference in vein diameter, mm (SD) * | 18.7 (21.7) | 29.9 (18.2) | 0.04 (12.1) | <0.001 | |
| Complications | |||||
| Brain abscess | 0 | 0 | 0 | ||
| Stroke | 0 | 0 | 0 | ||
| Hemoptysis | 2 | 0 | 2 | ||
| Hemothorax | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Si-Mohamed, S.A.; Cierco, A.; Gamondes, D.; Restier, L.M.; Delagrange, L.; Cottin, V.; Dupuis-Girod, S.; Revel, D. Embolization of Recurrent Pulmonary Arteriovenous Malformations by Ethylene Vinyl Alcohol Copolymer (Onyx®) in Hereditary Hemorrhagic Telangiectasia: Safety and Efficacy. J. Pers. Med. 2022, 12, 1091. https://doi.org/10.3390/jpm12071091
Si-Mohamed SA, Cierco A, Gamondes D, Restier LM, Delagrange L, Cottin V, Dupuis-Girod S, Revel D. Embolization of Recurrent Pulmonary Arteriovenous Malformations by Ethylene Vinyl Alcohol Copolymer (Onyx®) in Hereditary Hemorrhagic Telangiectasia: Safety and Efficacy. Journal of Personalized Medicine. 2022; 12(7):1091. https://doi.org/10.3390/jpm12071091
Chicago/Turabian StyleSi-Mohamed, Salim A., Alexandra Cierco, Delphine Gamondes, Lauria Marie Restier, Laura Delagrange, Vincent Cottin, Sophie Dupuis-Girod, and Didier Revel. 2022. "Embolization of Recurrent Pulmonary Arteriovenous Malformations by Ethylene Vinyl Alcohol Copolymer (Onyx®) in Hereditary Hemorrhagic Telangiectasia: Safety and Efficacy" Journal of Personalized Medicine 12, no. 7: 1091. https://doi.org/10.3390/jpm12071091
APA StyleSi-Mohamed, S. A., Cierco, A., Gamondes, D., Restier, L. M., Delagrange, L., Cottin, V., Dupuis-Girod, S., & Revel, D. (2022). Embolization of Recurrent Pulmonary Arteriovenous Malformations by Ethylene Vinyl Alcohol Copolymer (Onyx®) in Hereditary Hemorrhagic Telangiectasia: Safety and Efficacy. Journal of Personalized Medicine, 12(7), 1091. https://doi.org/10.3390/jpm12071091







