Progress in Personalized Psychiatric Therapy with the Example of Using Intranasal Oxytocin in PTSD Treatment
Abstract
:1. Post-Traumatic Stress Disorder—The Problem of Our Time Demanding Personalized Solutions?
2. Oxytocin in Medicine—How Did it Start and Where Are We Now?
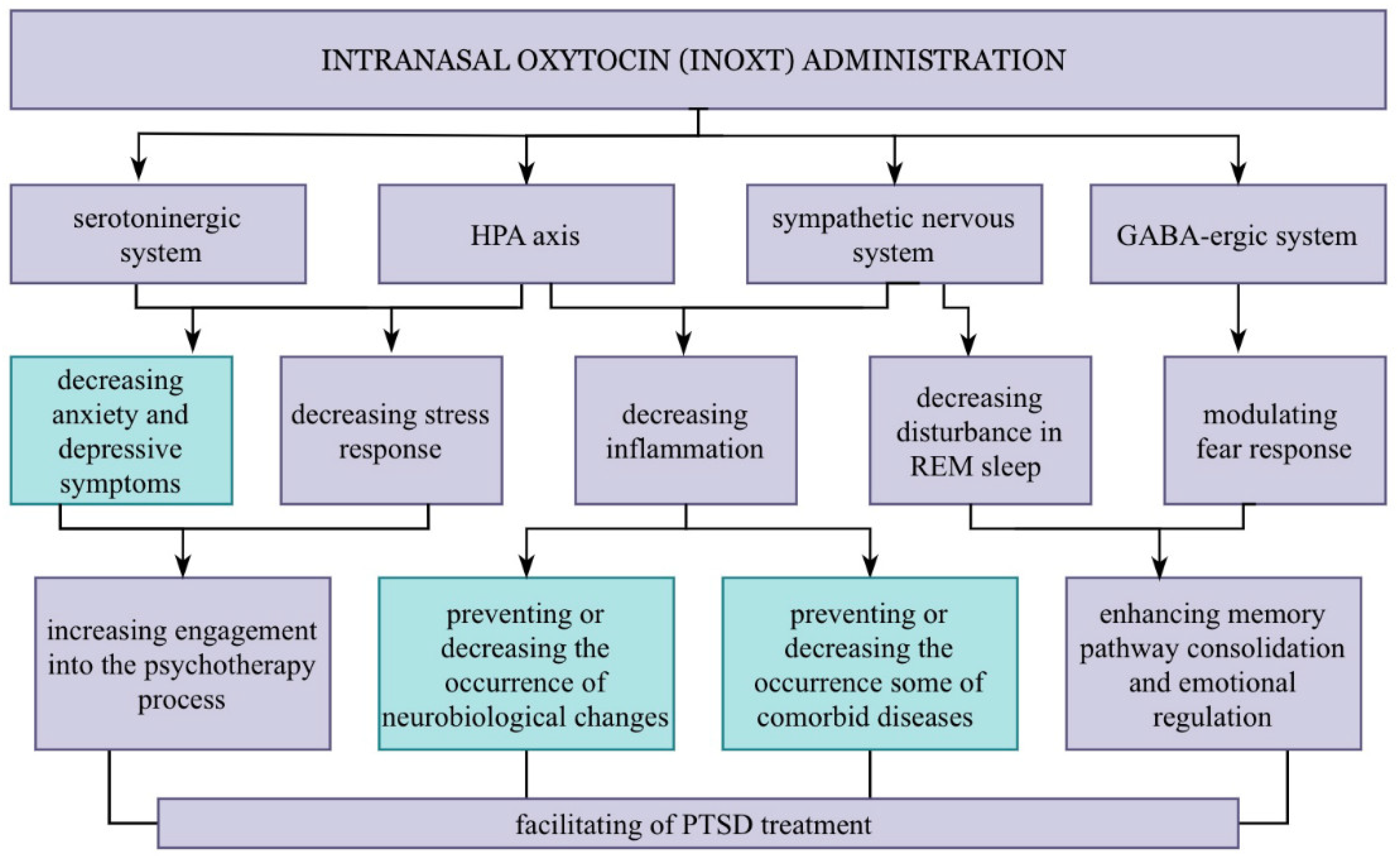
3. Pleiotropic Effects of Oxytocin
4. Oxytocinergic System in Light of Inter-Individual Variable Factors
5. Further Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abdul-Hamid, W.K.; Hughes, J.H. Nothing new under the sun: Post-traumatic stress disorders in the ancient world. Early Sci. Med. 2014, 19, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Ben–Ezra, M. Trauma in Antiquity: 4000 Year Old Post-Traumatic Reactions? Stress Health 2004, 20, 121–125. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Arlington, TA, USA, 2013; ISBN 9780890425572. [Google Scholar]
- James, M.K.; Robitsek, R.J.; McKenzie, K.; Valenzuela, J.Y.; Esposito, T.J. COVID-19 induced PTSD: Stressors for trauma and acute care surgeons. Am. J. Surg. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Liyanage-Don, N.A.; Winawer, M.R.; Hamberger, M.J.; Agarwal, S.; Trainor, A.R.; Quispe, K.A.; Kronish, I.M. Association of depression and COVID-induced PTSD with cognitive symptoms after COVID-19 illness. Gen. Hosp. Psychiatry 2022, 76, 45–48. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, A.M.; Ritchie, K.; McCabe, R.E.; Lanius, R.A.; Heber, A.; Smith, P.; Malain, A.; Schielke, H.; O’Connor, C.; Hosseiny, F. Healthcare Workers and COVID-19-Related Moral Injury: An Interpersonally-Focused Approach Informed by PTSD. Front. Psychiatry 2022, 12, 784523. [Google Scholar] [CrossRef] [PubMed]
- Haviland, M.G.; Banta, J.E.; Sonne, J.L.; Przekop, P. Posttraumatic Stress Disorder–Related Hospitalizations in the United States (2002–2011). J. Nerv. Ment. Dis. 2016, 204, 78–86. [Google Scholar] [CrossRef]
- Pacella, M.L.; Hruska, B.; Delahanty, D.L. The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. J. Anxiety Disord. 2013, 27, 33–46. [Google Scholar] [CrossRef]
- Vancampfort, D.; Rosenbaum, S.; Ward, P.B.; Steel, Z.; Lederman, O.; Lamwaka, A.V.; Richards, J.W.; Stubbs, B. Type 2 Diabetes Among People with Posttraumatic Stress Disorder. Psychosom. Med. 2016, 78, 465–473. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Stubbs, B.; Ward, P.B.; Steel, Z.; Lederman, O.; Vancampfort, D. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: A systematic review and meta-analysis. Metabolism 2015, 64, 926–933. [Google Scholar] [CrossRef] [Green Version]
- Bartoli, F.; Carrà, G.; Crocamo, C.; Carretta, D.; Clerici, M. Metabolic Syndrome in People Suffering from Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis. Metab. Syndr. Relat. Disord. 2013, 11, 301–308. [Google Scholar] [CrossRef]
- Rydder, A.L.; Azcarate, P.M.; Cohen, B.E. PTSD and Physical Health. Curr. Psychiatry Rep. 2018, 20, 116. [Google Scholar] [CrossRef] [PubMed]
- Auxéméry, Y. Post-traumatic psychiatric disorders: PTSD is not the only diagnosis. La Presse Médicale 2018, 47, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Najavits, L.M.; Capezza, N.M. Depression and Posttraumatic Stress Disorder Comorbidity; Oxford Library of Psychology Publisher: Oxford, England, 2014. [Google Scholar]
- Bradley, R.; Greene, J.; Russ, E.; Dutra, L.; Westen, D. A multidimensional meta-analysis of psychotherapy for PTSD. Am. J. Psychiatry 2005, 162, 214–227, Erratum in: Am. J. Psychiatry 2005, 162, 832Erratum in: Am. J. Psychiatry 2006, 163, 330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eftekhari, A.; Ruzek, J.I.; Crowley, J.J.; Rosen, C.S.; Greenbaum, M.A.; Karlin, B.E. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry 2013, 70, 949–955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, S.B.J.; van Zuiden, M.; Nawijn, L.; Frijling, J.L.; Veltman, D.J.; Olff, M. Intranasal oxytocin as strategy for medication-enhanced psychotherapy of PTSD: Salience processing and fear inhibition processes. Psychoneuroendocrinology 2014, 40, 242–256. [Google Scholar] [CrossRef] [PubMed]
- Olff, M.; Langeland, W.; Witteveen, A.; Denys, D. A Psychobiological Rationale for Oxytocin in the Treatment of Posttraumatic Stress Disorder. CNS Spectr. 2010, 15, 522–530. [Google Scholar] [CrossRef]
- Dale, H.H. On some physiological actions of ergot. J. Physiol. 1906, 34, 163–206. [Google Scholar] [CrossRef]
- Pang, W.W.; Hartmann, P.E. Initiation of Human Lactation: Secretory Differentiation and Secretory Activation. J. Mammary Gland. Biol. Neoplasia 2007, 12, 211–221. [Google Scholar] [CrossRef]
- MacDonald, K.; MacDonald, T.M. The Peptide That Binds. Harv. Rev. Psychiatry 2010, 18, 1–21. [Google Scholar] [CrossRef]
- Bartz, A.J.; Hollander, E. The neuroscience of affiliation: Forging links between basic and clinical research on neuropeptides and social behavior. Horm. Behav. 2006, 50, 518–528. [Google Scholar] [CrossRef]
- MacDonald, K.; Feifel, D. Oxytocin’s role in anxiety: A critical appraisal. Brain Res. 2014, 1580, 22–56. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Macbeth, A.H.; Pagani, J.; Young, W.S. Oxytocin: The Great Facilitator of Life. Prog. Neurobiol. 2009, 88, 127–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jurek, B.; Neumann, I.D. The Oxytocin Receptor: From Intracellular Signaling to Behavior. Physiol Rev. 2018, 98, 1805–1908. [Google Scholar] [CrossRef] [PubMed]
- Viero, C.; Shibuya, I.; Kitamura, N.; Verkhratsky, A.; Fujihara, H.; Katoh, A.; Ueta, Y.; Zingg, H.H.; Chvatal, A.; Sykova, E.; et al. REVIEW: Oxytocin: Crossing the bridge between basic science and pharmacotherapy. CNS Neurosci. Ther. 2010, 16, e138–e156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Striepens, N.; Kendrick, K.M.; Hanking, V.; Landgraf, R.; Wüllner, U.; Maier, W.; Hurlemann, R. Elevated cerebrospinal fluid and blood concentrations of oxytocin following its intranasal administration in humans. Sci. Rep. 2013, 3, 3440. [Google Scholar] [CrossRef]
- Tanaka, A.; Furubayashi, T.; Arai, M.; Inoue, D.; Kimura, S.; Kiriyama, A.; Kusamori, K.; Katsumi, H.; Yutani, R.; Sakane, T. Delivery of Oxytocin to the Brain for the Treatment of Autism Spectrum Disorder by Nasal Application. Mol. Pharm. 2018, 15, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.R.; Weerts, E.M. Oxytocin for the treatment of drug and alcohol use disorders. Behav. Pharmacol. 2016, 27, 640–648. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Huang, X.; Ebstein, R.P.; Yu, R. Intranasal oxytocin in the treatment of autism spectrum disorders: A multilevel meta-analysis. Neurosci. Biobehav. Rev. 2021, 122, 18–27. [Google Scholar] [CrossRef]
- Shilling, P.D.; Feifel, D. Potential of Oxytocin in the Treatment of Schizophrenia. CNS Drugs 2016, 30, 193–208. [Google Scholar] [CrossRef]
- Amad, A.; Thomas, P.; Perez-Rodriguez, M. Borderline Personality Disorder and Oxytocin: Review of Clinical Trials and Future Directions. Curr. Pharm. Des. 2015, 21, 3311–3316. [Google Scholar] [CrossRef]
- Flanagan, J.C.; Sippel, L.M.; Wahlquist, A.; Moran-Santa Maria, M.M.; Back, S.E. Augmenting Prolonged Exposure therapy for PTSD with intranasal oxytocin: A randomized, placebo-controlled pilot trial. J. Psychiatr. Res. 2018, 98, 64–69. [Google Scholar] [CrossRef] [PubMed]
- van Zuiden, M.; Frijling, J.L.; Nawijn, L.; Koch, S.B.J.; Goslings, J.C.; Luitse, J.S.; Biesheuvel, T.H.; Honig, A.; Veltman, D.J.; Olff, M. Intranasal Oxytocin to Prevent Posttraumatic Stress Disorder Symptoms: A Randomized Controlled Trial in Emergency Department Patients. Biol. Psychiatry 2017, 81, 1030–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshida, M.; Takayanagi, Y.; Inoue, K.; Kimura, T.; Young, L.J.; Onaka, T.; Nishimori, K. Evidence That Oxytocin Exerts Anxiolytic Effects via Oxytocin Receptor Expressed in Serotonergic Neurons in Mice. J. Neurosci. 2009, 29, 2259–2271. [Google Scholar] [CrossRef] [PubMed]
- Baldi, E.; Costa, A.; Rani, B.; Passani, M.B.; Blandina, P.; Romano, A.; Provensi, G. Oxytocin and Fear Memory Extinction: Possible Implications for the Therapy of Fear Disorders? Int. J. Mol. Sci. 2021, 22, 10000. [Google Scholar] [CrossRef]
- Kirby, L.G.; Rice, K.C.; Valentino, R.J. Effects of corticotropin-releasing factor on neuronal activity in the serotonergic dorsal raphe nucleus. Neuropsychopharmacology 2000, 22, 148–162, Erratum in: Neuropsychopharmacology 2000, 22, 449. [Google Scholar] [CrossRef] [PubMed]
- Bangasser, D.A. Sex differences in stress-related receptors: “micro” differences with “macro” implications for mood and anxiety disorders. Biol. Sex Differ. 2013, 4, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janeček, M.; Dabrowska, J. Oxytocin facilitates adaptive fear and attenuates anxiety responses in animal models and human studies—Potential interaction with the corticotropin-releasing factor (CRF) system in the bed nucleus of the stria terminalis (BNST). Cell Tissue Res. 2019, 375, 143–172. [Google Scholar] [CrossRef]
- McEwen, B.S. Stress, sex, and neural adaptation to a changing environment: Mechanisms of neuronal remodeling. Ann. N. Y. Acad. Sci. 2010, 1204, 38–59. [Google Scholar] [CrossRef] [Green Version]
- Preckel, K.; Scheele, D.; Kendrick, K.M.; Maier, W.; Hurlemann, R. Oxytocin facilitates social approach behavior in women. Front. Behav. Neurosci. 2014, 8, 191. [Google Scholar] [CrossRef] [Green Version]
- Craske, M.G.; Kircanski, K.; Zelikowsky, M.; Mystkowski, J.; Chowdhury, N.; Baker, A. Optimizing inhibitory learning during exposure therapy. Behav. Res. Ther. 2008, 46, 5–27. [Google Scholar] [CrossRef]
- Rothbaum, B.O.; Davis, M. Applying Learning Principles to the Treatment of Post-Trauma Reactions. Ann. N. Y. Acad. Sci. 2003, 1008, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Sripada, R.K.; King, A.P.; Garfinkel, S.N.; Wang, X.; Sripada, C.S.; Welsh, R.C.; Liberzon, I. Altered resting-state amygdala functional connectivity in men with posttraumatic stress disorder. J. Psychiatry Neurosci. 2012, 37, 241–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.; Yan, X.; Li, M.; Ma, Y. Neural substrates underlying the effects of oxytocin: A quantitative meta-analysis of pharmaco-imaging studies. Soc. Cogn. Affect. Neurosci. 2017, 12, 1565–1573. [Google Scholar] [CrossRef] [PubMed]
- Windle, R.J. Oxytocin Attenuates Stress-Induced c-fos mRNA Expression in Specific Forebrain Regions Associated with Modulation of Hypothalamo-Pituitary-Adrenal Activity. J. Neurosci. 2004, 24, 2974–2982. [Google Scholar] [CrossRef]
- Sautter, F.J.; Bissette, G.; Wiley, J.; Manguno-Mire, G.; Schoenbachler, B.; Myers, L.; Johnson, J.E.; Cerbone, A.; Malaspina, D. Corticotropin-releasing factor in posttraumatic stress disorder (PTSD) with secondary psychotic symptoms, nonpsychotic PTSD, and healthy control subjects. Biol. Psychiatry 2003, 54, 1382–1388. [Google Scholar] [CrossRef] [PubMed]
- Bremner, J.D.; Licinio, J.; Darnell, A.; Krystal, J.H.; Owens, M.J.; Southwick, S.M.; Nemeroff, C.B.; Charney, D.S. Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am. J. Psychiatry. 1997, 154, 624–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daskalakis, N.P.; Cohen, H.; Nievergelt, C.M.; Baker, D.G.; Buxbaum, J.D.; Russo, S.J.; Yehuda, R. New translational perspectives for blood-based biomarkers of PTSD: From glucocorticoid to immune mediators of stress susceptibility. Exp. Neurol. 2016, 284, 133–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, M.C.; Compas, B.E.; Garber, J. Relations among posttraumatic stress disorder, comorbid major depression, and HPA function: A systematic review and meta-analysis. Clin. Psychol. Rev. 2012, 32, 301–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meewisse, M.L.; Reitsma, J.B.; de Vries, G.J.; Gersons, B.P.; Olff, M. Cortisol and post-traumatic stress disorder in adults: Systematic review and meta-analysis. Br. J. Psychiatry 2007, 191, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Myers, B.; McKlveen, J.M.; Herman, J.P. Glucocorticoid actions on synapses, circuits, and behavior: Implications for the energetics of stress. Front. Neuroendocrinol. 2014, 35, 180–196. [Google Scholar] [CrossRef] [Green Version]
- Sherin, J.E.; Nemeroff, C.B. Post-traumatic stress disorder: The neurobiological impact of psychological trauma. Dialogues Clin. Neurosci. 2011, 13, 263–278. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.W.; Lin, A.P.; Wolf, E.J.; Miller, D.R. Oxidative Stress, Inflammation, and Neuroprogression in Chronic PTSD. Harv. Rev. Psychiatry 2018, 26, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Hori, H.; Kim, Y. Inflammation and post-traumatic stress disorder. Psychiatry Clin. Neurosci. 2019, 73, 143–153. [Google Scholar] [CrossRef] [Green Version]
- Guo, M.; Liu, T.; Guo, J.-C.; Jiang, X.-L.; Chen, F.; Gao, Y.-S. Study on serum cytokine levels in posttraumatic stress disorder patients. Asian Pac. J. Trop. Med. 2012, 5, 323–325. [Google Scholar] [CrossRef] [Green Version]
- Passos, I.C.; Vasconcelos-Moreno, M.P.; Costa, L.G.; Kunz, M.; Brietzke, E.; Quevedo, J.; Salum, G.; Magalhães, P.V.; Kapczinski, F.; Kauer-Sant’Anna, M. Inflammatory markers in post-traumatic stress disorder: A systematic review, meta-analysis, and meta-regression. Lancet Psychiatry 2015, 2, 1002–1012. [Google Scholar] [CrossRef]
- de Oliveira, J.F.; Wiener, C.D.; Jansen, K.; Portela, L.V.; Lara, D.R.; Souza, L.D.d.M.; da Silva, R.A.; Moreira, F.P.; Oses, J.P. Serum levels of interleukins IL-6 and IL-10 in individuals with posttraumatic stress disorder in a population-based sample. Psychiatry Res. 2018, 260, 111–115. [Google Scholar] [CrossRef]
- Levin, S.G.; Godukhin, O.V. Modulating Effect of Cytokines on Mechanisms of Synaptic Plasticity in the Brain. Biochemistry 2017, 82, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Colonna, M.; Butovsky, O. Microglia Function in the Central Nervous System During Health and Neurodegeneration. Annu. Rev. Immunol. 2017, 35, 441–468. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-C.; Lin, C.-C.; Chen, C.-C.; Tzeng, N.-S.; Liu, Y.-P. Effects of Oxytocin on Fear Memory and Neuroinflammation in a Rodent Model of Posttraumatic Stress Disorder. Int. J. Mol. Sci. 2018, 19, 3848. [Google Scholar] [CrossRef] [Green Version]
- Petersson, M.; Diaz-Cabiale, Z.; Angel Narváez, J.; Fuxe, K.; Uvnäs-Moberg, K. Oxytocin increases the density of high affinity α2-adrenoceptors within the hypothalamus, the amygdala and the nucleus of the solitary tract in ovariectomized rats. Brain Res. 2005, 1049, 234–239. [Google Scholar] [CrossRef]
- Quintana, D.S.; Kemp, A.H.; Alvares, G.A.; Guastella, A.J. A role for autonomic cardiac control in the effects of oxytocin on social behavior and psychiatric illness. Front. Neurosci. 2013, 7, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanev, K.S.; Orr, S.P.; Pace-Schott, E.F.; Griffin, M.; Pitman, R.K.; Resick, P.A. Positive Association Between Nightmares and Heart Rate Response to Loud Tones. J. Nerv. Ment. Dis. 2017, 205, 308–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colvonen, P.J.; Straus, L.D.; Acheson, D.; Gehrman, P. A Review of the Relationship Between Emotional Learning and Memory, Sleep, and PTSD. Curr. Psychiatry Rep. 2019, 21, 2. [Google Scholar] [CrossRef] [PubMed]
- Bottary, R.; Seo, J.; Daffre, C.; Gazecki, S.; Moore, K.N.; Kopotiyenko, K.; Dominguez, J.P.; Gannon, K.; Lasko, N.B.; Roth, B.; et al. Fear extinction memory is negatively associated with REM sleep in insomnia disorder. Sleep 2020, 43, zsaa007. [Google Scholar] [CrossRef] [PubMed]
- Germain, A. Sleep Disturbances as the Hallmark of PTSD: Where Are We Now? Am. J. Psychiatry 2013, 170, 372–382. [Google Scholar] [CrossRef]
- Gimpl, G.; Fahrenholz, F. The Oxytocin Receptor System: Structure, Function, and Regulation. Physiol. Rev. 2001, 81, 629–683. [Google Scholar] [CrossRef] [Green Version]
- Christiansen, D.M.; Berke, E.T. Gender- and Sex-Based Contributors to Sex Differences in PTSD. Curr. Psychiatry Rep. 2020, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Abramova, O.; Zorkina, Y.; Ushakova, V.; Zubkov, E.; Morozova, A.; Chekhonin, V. The role of oxytocin and vasopressin dysfunction in cognitive impairment and mental disorders. Neuropeptides 2020, 83, 102079. [Google Scholar] [CrossRef] [PubMed]
- Zink, C.F.; Stein, J.L.; Kempf, L.; Hakimi, S.; Meyer-Lindenberg, A. Vasopressin Modulates Medial Prefrontal Cortex-Amygdala Circuitry during Emotion Processing in Humans. J. Neurosci. 2010, 30, 7017–7022. [Google Scholar] [CrossRef]
- Zink, C.F.; Kempf, L.; Hakimi, S.; Rainey, C.A.; Stein, J.L.; Meyer-Lindenberg, A. Vasopressin modulates social recognition-related activity in the left temporoparietal junction in humans. Transl. Psychiatry 2011, 1, e3. [Google Scholar] [CrossRef] [Green Version]
- Bao, A.-M.; Fischer, D.F.; Wu, Y.-H.; Hol, E.M.; Balesar, R.; Unmehopa, U.A.; Zhou, J.-N.; Swaab, D.F. A direct androgenic involvement in the expression of human corticotropin-releasing hormone. Mol. Psychiatry 2006, 11, 567–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, A.-M.; Hestiantoro, A.; Van Someren, E.J.W.; Swaab, D.F.; Zhou, J.-N. Colocalization of corticotropin-releasing hormone and oestrogen receptor-α in the paraventricular nucleus of the hypothalamus in mood disorders. Brain 2005, 128, 1301–1313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milad, M.R.; Zeidan, M.A.; Contero, A.; Pitman, R.K.; Klibanski, A.; Rauch, S.L.; Goldstein, J.M. The influence of gonadal hormones on conditioned fear extinction in healthy humans. Neuroscience 2010, 168, 652–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodrigues, S.M.; Saslow, L.R.; Garcia, N.; John, O.P.; Keltner, D. Oxytocin receptor genetic variation relates to empathy and stress reactivity in humans. Proc. Natl. Acad. Sci. USA 2009, 106, 21437–21441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, B.; Pini, S.; Gabelloni, P.; Abelli, M.; Lari, L.; Cardini, A.; Muti, M.; Gesi, C.; Landi, S.; Galderisi, S. Oxytocin receptor polymorphisms and adult attachment style in patients with depression. Psychoneuroendocrinology 2009, 34, 1506–1514. [Google Scholar] [CrossRef]
- Li, J.; Zhao, Y.; Li, R.; Broster, L.S.; Zhou, C.; Yang, S. Association of Oxytocin Receptor Gene (OXTR) rs53576 Polymorphism with Sociality: A Meta-Analysis. PLoS ONE 2015, 10, e0131820. [Google Scholar] [CrossRef]
- Wang, J.; Braskie, M.N.; Hafzalla, G.W.; Faskowitz, J.; McMahon, K.L.; de Zubicaray, G.I.; Wright, M.J.; Yu, C.; Thompson, P.M. Relationship of a common OXTR gene variant to brain structure and default mode network function in healthy humans. NeuroImage 2017, 147, 500–506. [Google Scholar] [CrossRef] [Green Version]
- Raichle, M.E. The brain’s default mode network. Annu. Rev. Neurosci. 2015, 38, 433–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitfield-Gabrieli, S.; Ford, J.M. Default Mode Network Activity and Connectivity in Psychopathology. Annu. Rev. Clin. Psychol. 2012, 8, 49–76. [Google Scholar] [CrossRef]
- Zimmermann, J.; Deris, N.; Montag, C.; Reuter, M.; Felten, A.; Becker, B.; Weber, B.; Markett, S. A common polymorphism on the oxytocin receptor gene (rs2268498) and resting-state functional connectivity of amygdala subregions—A genetic imaging study. NeuroImage 2018, 179, 1–10. [Google Scholar] [CrossRef]
- Miguel, P.M.; Pereira, L.O.; Silveira, P.P.; Meaney, M.J. Early environmental influences on the development of children’s brain structure and function. Dev. Med. Child. Neurol. 2019, 61, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, E.; Dadds, M.R.; Brennan, J.L.; Williams, K.; Levy, F.; Cauchi, A.J. A review of safety, side-effects and subjective reactions to intranasal oxytocin in human research. Psychoneuroendocrinology 2011, 36, 1114–1126. [Google Scholar] [CrossRef] [PubMed]
- Walum, H.; Waldman, I.D.; Young, L.J. Statistical and Methodological Considerations for the Interpretation of Intranasal Oxytocin Studies. Biol. Psychiatry 2016, 79, 251–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giovanna, G.; Damiani, S.; Fusar-Poli, L.; Rocchetti, M.; Brondino, N.; de Cagna, F.; Mori, A.; Politi, P. Intranasal oxytocin as a potential therapeutic strategy in post-traumatic stress disorder: A systematic review. Psychoneuroendocrinology 2020, 115, 104605. [Google Scholar] [CrossRef] [PubMed]
- Litz, B.T.; Salters-Pedneault, K.; Steenkamp, M.M.; Hermos, J.A.; Bryant, R.A.; Otto, M.W.; Hofmann, S.G. A randomized placebo-controlled trial of d-cycloserine and exposure therapy for posttraumatic stress disorder. J. Psychiatr. Res. 2012, 46, 1184–1190. [Google Scholar] [CrossRef]
- de Kleine, R.A.; Hendriks, G.-J.; Kusters, W.J.C.; Broekman, T.G.; van Minnen, A. A Randomized Placebo-Controlled Trial of d-Cycloserine to Enhance Exposure Therapy for Posttraumatic Stress Disorder. Biol. Psychiatry 2012, 71, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Singewald, N.; Schmuckermair, C.; Whittle, N.; Holmes, A.; Ressler, K.J. Pharmacology of cognitive enhancers for exposure-based therapy of fear, anxiety and trauma-related disorders. Pharmacol. Ther. 2015, 149, 150–190. [Google Scholar] [CrossRef] [Green Version]
- Tuerk, P.W.; Wangelin, B.C.; Powers, M.B.; Smits, J.A.J.; Acierno, R.; Myers, U.S.; Orr, S.P.; Foa, E.B.; Hamner, M.B. Augmenting treatment efficiency in exposure therapy for PTSD: A randomized double-blind placebo-controlled trial of yohimbine HCl. Cogn. Behav. Ther. 2018, 47, 351–371. [Google Scholar] [CrossRef]
- de Kleine, R.A.; Rothbaum, B.O.; van Minnen, A. Pharmacological enhancement of exposure-based treatment in PTSD: A qualitative review. Eur. J. Psychotraumatology 2013, 4, 21626. [Google Scholar] [CrossRef]
- Zoellner, L.A.; Telch, M.; Foa, E.B.; Farach, F.J.; McLean, C.P.; Gallop, R.; Bluett, E.J.; Cobb, A.; Gonzalez-Lima, F. Enhancing Extinction Learning in Posttraumatic Stress Disorder with Brief Daily Imaginal Exposure and Methylene Blue. J. Clin. Psychiatry 2017, 78, e782–e789. [Google Scholar] [CrossRef]
- Yazar-Klosinski, B.; Mitchell, J. A Randomized, Double-Blind, Placebo Controlled Phase 3 Study Assessing Efficacy and Safety of MDMA-Assisted Therapy for the Treatment of Severe PTSD. Biol. Psychiatry 2021, 89, S105. [Google Scholar] [CrossRef]
- Szafoni, S.; Wieckiewicz, G.; Pudlo, R.; Gorczyca, P.; Piegza, M. Will MDMA-assistedpsychotherapy become a breakthrough in treatment-resistant post-traumatic stress dis-order? A critical narrative review. Psychiatr. Pol. 2021, 228, 1–14. [Google Scholar] [CrossRef]
- Krystal, J.H.; Abdallah, C.G.; Averill, L.A.; Kelmendi, B.; Harpaz-Rotem, I.; Sanacora, G.; Southwick, S.M.; Duman, R.S. Synaptic Loss and the Pathophysiology of PTSD: Implications for Ketamine as a Prototype Novel Therapeutic. Curr. Psychiatry Rep. 2017, 19, 74. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.A.; Harricharan, S.; Densmore, M.; Neufeld, R.W.J.; Ros, T.; McKinnon, M.C.; Frewen, P.A.; Théberge, J.; Jetly, R.; Pedlar, D. Classifying heterogeneous presentations of PTSD via the default mode, central executive, and salience networks with machine learning. NeuroImage Clin. 2020, 27, 102262. [Google Scholar] [CrossRef] [PubMed]
- Bandelow, B.; Baldwin, D.; Abelli, M.; Bolea-Alamanac, B.; Bourin, M.; Chamberlain, S.R.; Cinosi, E.; Davies, S.; Domschke, K.; Fineberg, N.; et al. Biological markers for anxiety disorders, OCD and PTSD: A consensus statement. Part II: Neurochemistry, neurophysiology and neurocognition. World J. Biol. Psychiatry 2017, 18, 162–214. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szafoni, S.; Piegza, M. Progress in Personalized Psychiatric Therapy with the Example of Using Intranasal Oxytocin in PTSD Treatment. J. Pers. Med. 2022, 12, 1067. https://doi.org/10.3390/jpm12071067
Szafoni S, Piegza M. Progress in Personalized Psychiatric Therapy with the Example of Using Intranasal Oxytocin in PTSD Treatment. Journal of Personalized Medicine. 2022; 12(7):1067. https://doi.org/10.3390/jpm12071067
Chicago/Turabian StyleSzafoni, Sandra, and Magdalena Piegza. 2022. "Progress in Personalized Psychiatric Therapy with the Example of Using Intranasal Oxytocin in PTSD Treatment" Journal of Personalized Medicine 12, no. 7: 1067. https://doi.org/10.3390/jpm12071067
APA StyleSzafoni, S., & Piegza, M. (2022). Progress in Personalized Psychiatric Therapy with the Example of Using Intranasal Oxytocin in PTSD Treatment. Journal of Personalized Medicine, 12(7), 1067. https://doi.org/10.3390/jpm12071067





