A Proposed Personalized Spine Care Protocol (SpineScreen) to Treat Visualized Pain Generators: An Illustrative Study Comparing Clinical Outcomes and Postoperative Reoperations between Targeted Endoscopic Lumbar Decompression Surgery, Minimally Invasive TLIF and Open Laminectomy
Abstract
:1. Introduction
2. Materials and Methods
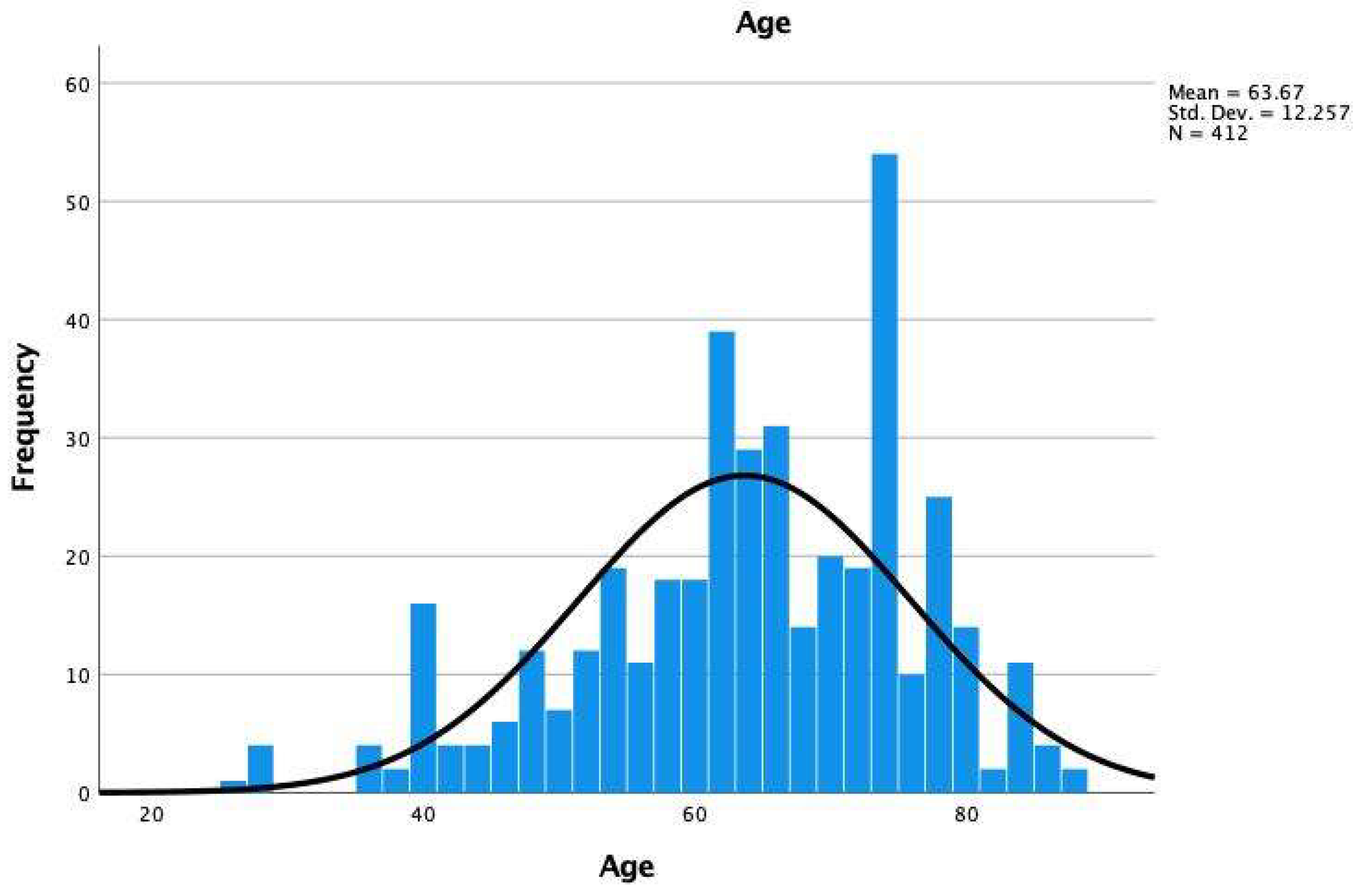
2.1. Patient Population
2.2. Preoperative Work Up and Surgical Decision Making
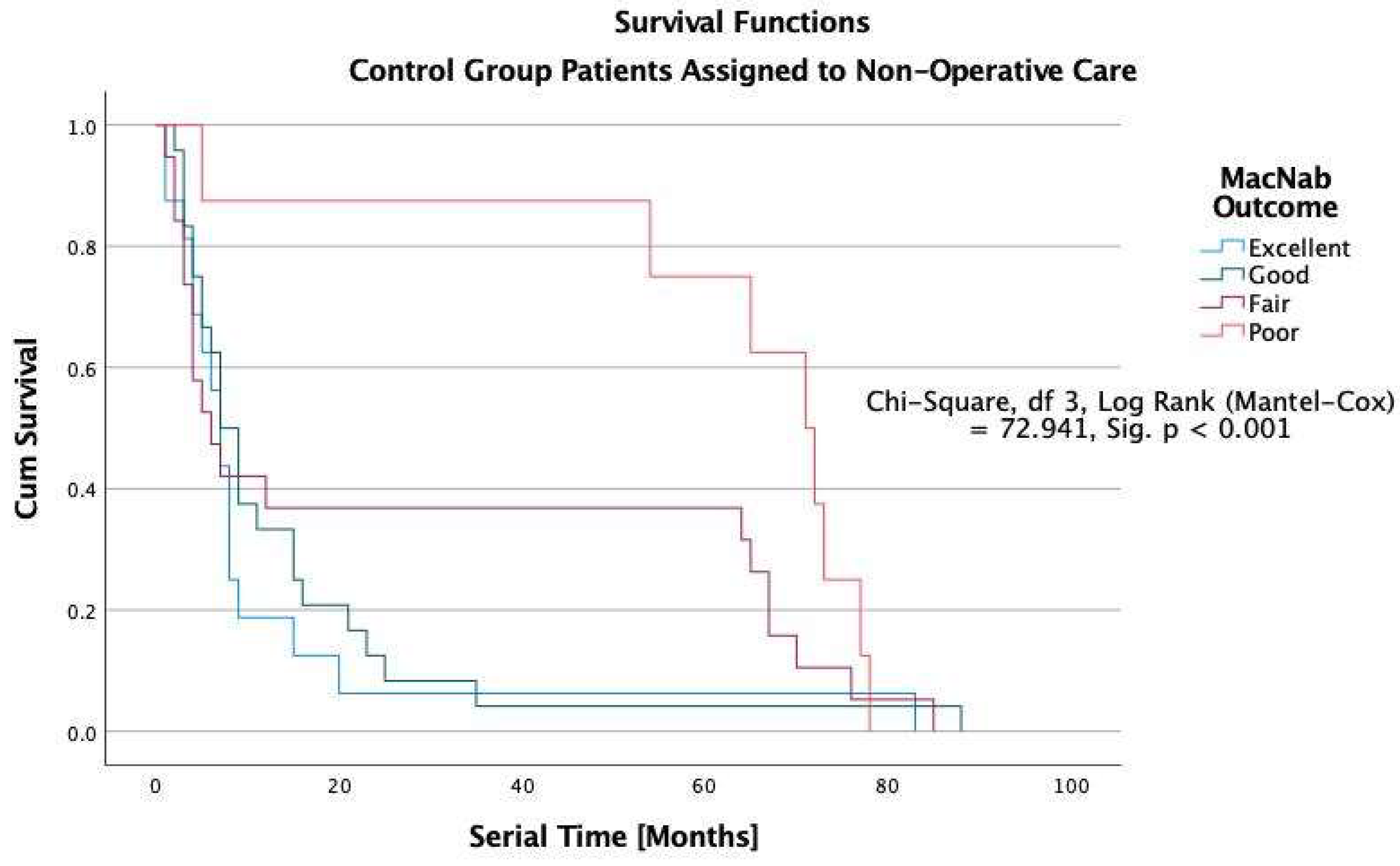
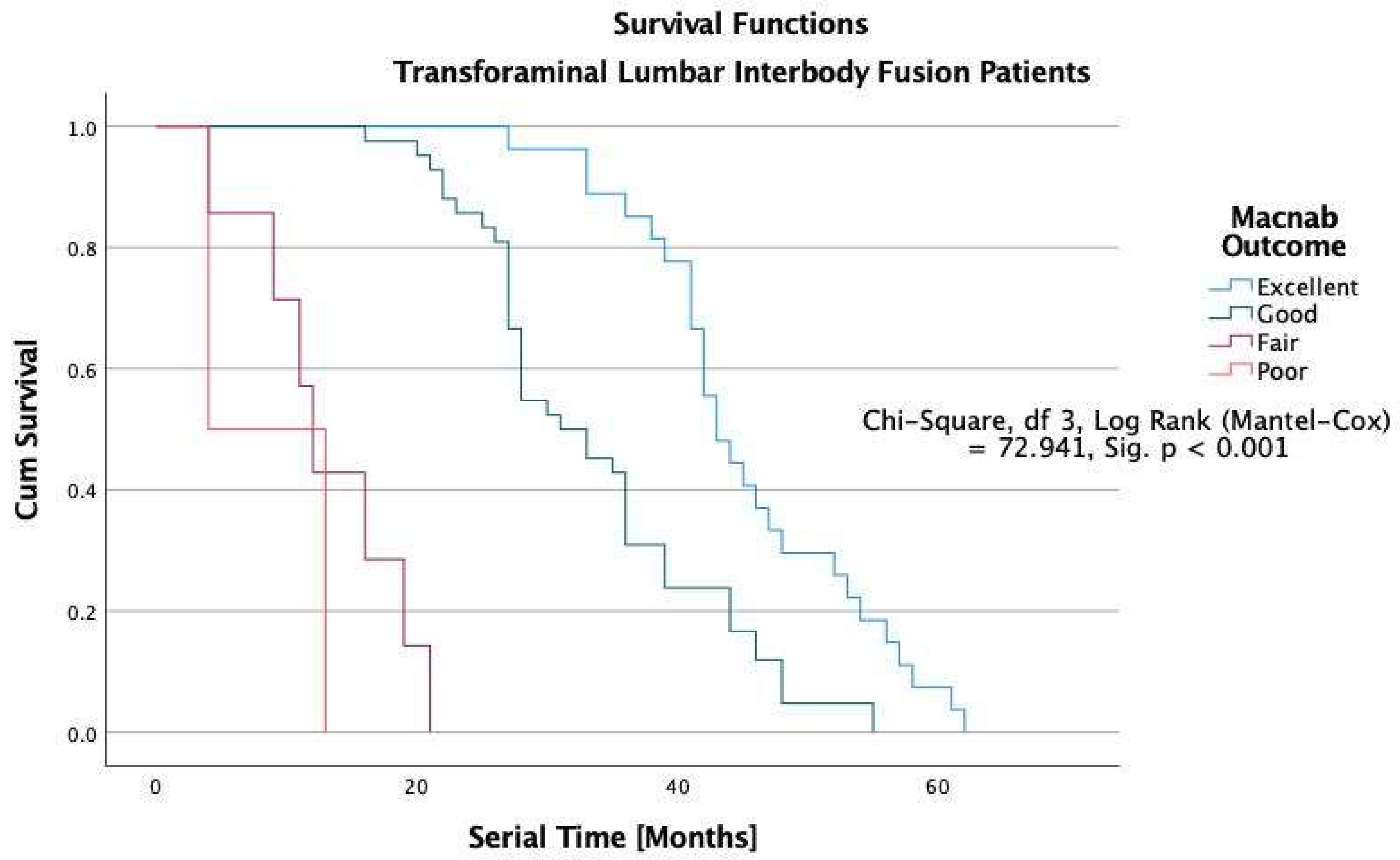
2.3. Clinical Follow-Up
2.4. Surgical Techniques and Postoperative Rehabilitation
2.5. Postoperative Utilization Analysis
2.6. Correlative Surgical Outcome Analysis
3. Results
4. Discussion
- Structural, cultural, and psychological resistance to randomization,
- The inherent variability of surgical procedures and the need for a precise definition of interventions and quality monitoring,
- Surgical learning curves of new techniques,
- Patient’s equipoise, given the differences in the risks of surgical and non-surgical treatments,
- Difficulties with recruitment.
- Consent and randomization in rare conditions and urgent and life-threatening situations.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lewandrowski, K.U. Retrospective analysis of accuracy and positive predictive value of preoperative lumbar MRI grading after successful outcome following outpatient endoscopic decompression for lumbar foraminal and lateral recess stenosis. Clin. Neurol. Neurosurg. 2019, 179, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Lewandrowski, K.U.; Muraleedharan, N.; Eddy, S.A.; Sobti, V.; Reece, B.D.; León, J.F.R.; Shah, S. Reliability Analysis of Deep Learning Algorithms for Reporting of Routine Lumbar MRI Scans. Int. J. Spine Surg. 2020, 14 (Suppl. S3), S98–S107. [Google Scholar] [CrossRef] [PubMed]
- Lurie, J.D.; Tosteson, A.N.; Tosteson, T.D.; Carragee, E.; Carrino, J.A.; Kaiser, J.; Sequeiros, R.T.; Lecomte, A.R.; Grove, M.R.; Blood, E.A.; et al. Reliability of magnetic resonance imaging readings for lumbar disc herniation in the Spine Patient Outcomes Research Trial (SPORT). Spine 2008, 33, 991–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, A.K.; Sharma, V.; Robinson, L.C.; Mummaneni, P.V. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg. Clin. N. Am. 2019, 30, 353–364. [Google Scholar] [CrossRef]
- Cheng, J.S.; Lee, M.J.; Massicotte, E.; Ashman, B.; Gruenberg, M.; Pilcher, L.E.; Skelly, A.C. Clinical guidelines and payer policies on fusion for the treatment of chronic low back pain. Spine 2011, 36 (Suppl. S21), S144–S163. [Google Scholar] [CrossRef] [PubMed]
- Choudhri, T.F.; Mummaneni, P.V.; Dhall, S.S.; Eck, J.C.; Groff, M.W.; Ghogawala, Z.; Watters, W.C., 3rd; Dailey, A.T.; Resnick, D.K.; Sharan, A.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: Radiographic assessment of fusion status. J. Neurosurg. Spine 2014, 21, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Dailey, A.T.; Ghogawala, Z.; Choudhri, T.F.; Watters, W.C., 3rd; Resnick, D.K.; Sharan, A.; Eck, J.C.; Mummaneni, P.V.; Wang, J.C.; Groff, M.W.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 14: Brace therapy as an adjunct to or substitute for lumbar fusion. J. Neurosurg. Spine 2014, 21, 91–101. [Google Scholar] [CrossRef] [Green Version]
- Dhall, S.S.; Choudhri, T.F.; Eck, J.C.; Groff, M.W.; Ghogawala, Z.; Watters, W.C., 3rd; Dailey, A.T.; Resnick, D.K.; Sharan, A.; Mummaneni, P.V.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 5: Correlation between radiographic outcome and function. J. Neurosurg. Spine 2014, 21, 31–36. [Google Scholar] [CrossRef] [Green Version]
- Eck, J.C.; Sharan, A.; Ghogawala, Z.; Resnick, D.K.; Watters, W.C., 3rd; Mummaneni, P.V.; Dailey, A.T.; Choudhri, T.F.; Groff, M.W.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: Lumbar fusion for intractable low-back pain without stenosis or spondylolisthesis. J. Neurosurg. Spine 2014, 21, 42–47. [Google Scholar] [CrossRef] [Green Version]
- Eck, J.C.; Sharan, A.; Resnick, D.K.; Watters, W.C., 3rd; Ghogawala, Z.; Dailey, A.T.; Mummaneni, P.V.; Groff, M.W.; Wang, J.C.; Choudhri, T.F.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 6: Discography for patient selection. J. Neurosurg. Spine 2014, 21, 37–41. [Google Scholar] [CrossRef] [Green Version]
- Ghogawala, Z.; Whitmore, R.G.; Watters, W.C., 3rd; Sharan, A.; Mummaneni, P.V.; Dailey, A.T.; Choudhri, T.F.; Eck, J.C.; Groff, M.W.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 3: Assessment of economic outcome. J. Neurosurg. Spine 2014, 21, 14–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haig, A.J. Diagnostic tests the NASS stenosis guidelines. Spine J. 2014, 14, 200–201. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.G.; Groff, M.W.; Watters, W.C., 3rd; Ghogawala, Z.; Mummaneni, P.V.; Dailey, A.T.; Choudhri, T.F.; Eck, J.C.; Sharan, A.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 16: Bone graft extenders and substitutes as an adjunct for lumbar fusion. J. Neurosurg. Spine 2014, 21, 106–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreiner, D.S.; Baisden, J.; Gilbert, T.; Shaffer, W.O.; Summers, J.T. Re: Diagnostic tests the NASS stenosis guidelines. Spine J. 2014, 14, 201–202. [Google Scholar] [CrossRef]
- Lorio, M.; Clerk-Lamalice, O.; Beall, D.P.; Julien, T. International Society for the Advancement of Spine Surgery Guideline-Intraosseous Ablation of the Basivertebral Nerve for the Relief of Chronic Low Back Pain. Int. J. Spine Surg. 2020, 14, 18–25. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Dhall, S.S.; Eck, J.C.; Groff, M.W.; Ghogawala, Z.; Watters, W.C., 3rd; Dailey, A.T.; Resnick, D.K.; Choudhri, T.F.; Sharan, A.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 11: Interbody techniques for lumbar fusion. J. Neurosurg. Spine 2014, 21, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Watters, W.C., 3rd; Resnick, D.K.; Eck, J.C.; Ghogawala, Z.; Mummaneni, P.V.; Dailey, A.T.; Choudhri, T.F.; Sharan, A.; Groff, M.W.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 13: Injection therapies, low-back pain, and lumbar fusion. J. Neurosurg. Spine 2014, 21, 79–90. [Google Scholar] [CrossRef] [Green Version]
- Alvi, M.A.; Sebai, A.; Yolcu, Y.; Wahood, W.; Elder, B.D.; Kaufmann, T.; Bydon, M. Assessing the Differences in Measurement of Degree of Spondylolisthesis Between Supine MRI and Erect X-Ray: An Institutional Analysis of 255 Cases. Oper. Neurosurg. 2020, 18, 438–443. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Lee, J.W.; Chai, J.W.; Yoo, H.J.; Kang, Y.; Seo, J.; Ahn, J.M.; Kang, H.S. A New MRI Grading System for Cervical Foraminal Stenosis Based on Axial T2-Weighted Images. Korean J. Radiol. 2015, 16, 1294–1302. [Google Scholar] [CrossRef] [Green Version]
- Kuittinen, P.; Sipola, P.; Saari, T.; Aalto, T.J.; Sinikallio, S.; Savolainen, S.; Kroger, H.; Turunen, V.; Leinonen, V.; Airaksinen, O. Visually assessed severity of lumbar spinal canal stenosis is paradoxically associated with leg pain and objective walking ability. BMC Musculoskelet. Disord. 2014, 15, 348. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.J.; Kim, H.J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Fredrickson, V.; Resnick, D.K. How should we grade lumbar disc herniation and nerve root compression? A systematic review. Clin. Orthop. Relat. Res. 2015, 473, 1896–1902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lonne, G.; Odegard, B.; Johnsen, L.G.; Solberg, T.K.; Kvistad, K.A.; Nygaard, O.P. MRI evaluation of lumbar spinal stenosis: Is a rapid visual assessment as good as area measurement? Eur. Spine J. 2014, 23, 1320–1324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rüegg, T.B.; Wicki, A.G.; Aebli, N.; Wisianowsky, C.; Krebs, J. The diagnostic value of magnetic resonance imaging measurements for assessing cervical spinal canal stenosis. J. Neurosurg. Spine 2015, 22, 230–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroeder, G.D.; Kurd, M.F.; Vaccaro, A.R. Lumbar Spinal Stenosis: How Is It Classified? J. Am. Acad. Orthop. Surg. 2016, 24, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Dowling, A.; Lewandrowski, K.U.; da Silva, F.H.P.; Parra, J.A.A.; Portillo, D.M.; Gimenez, Y.C.P. Patient selection protocols for endoscopic transforaminal, interlaminar, and translaminar decompression of lumbar spinal stenosis. J. Spine Surg. 2020, 6 (Suppl. S1), S120–S132. [Google Scholar] [CrossRef]
- Narain, A.S.; Hijji, F.Y.; Haws, B.E.; Khechen, B.; Kudaravalli, K.T.; Yom, K.H.; Singh, K. Risk Factors for Medical and Surgical Complications after 1-2-Level Anterior Cervical Discectomy and Fusion Procedures. Int. J. Spine Surg. 2020, 14, 286–293. [Google Scholar] [CrossRef]
- Yeung, A.; Lewandrowski, K.U. Early and staged endoscopic management of common pain generators in the spine. J. Spine Surg. 2020, 6 (Suppl. S1), S1–S5. [Google Scholar] [CrossRef]
- Lewandrowski, K.U.; Ransom, N.A.; Yeung, A. Return to work and recovery time analysis after outpatient endoscopic lumbar transforaminal decompression surgery. J. Spine Surg. 2020, 6 (Suppl. S1), S100–S115. [Google Scholar] [CrossRef]
- Wang, M.Y.; Cummock, M.D.; Yu, Y.; Trivedi, R.A. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J. Neurosurg. Spine 2010, 12, 694–699. [Google Scholar] [CrossRef]
- Adogwa, O.; Parker, S.L.; Shau, D.N.; Mendenhall, S.K.; Aaronson, O.; Cheng, J.S.; Devin, C.J.; McGirt, M.J. Cost per quality-adjusted life year gained of revision neural decompression and instrumented fusion for same-level recurrent lumbar stenosis: Defining the value of surgical intervention. J. Neurosurg. Spine 2012, 16, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Modhia, U.; Takemoto, S.; Braid-Forbes, M.J.; Weber, M.; Berven, S.H. Readmission rates after decompression surgery in patients with lumbar spinal stenosis among Medicare beneficiaries. Spine 2013, 38, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Al-Khouja, L.T.; Baron, E.M.; Johnson, J.P.; Kim, T.T.; Drazin, D. Cost-effectiveness analysis in minimally invasive spine surgery. Neurosurg. Focus 2014, 36, E4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, J.N.; Tosteson, A.N.; Tosteson, T.D.; Lurie, J.D.; Abdu, W.A.; Mirza, S.K.; Zhao, W.; Morgan, T.S.; Nelson, E.C. The SPORT value compass: Do the extra costs of undergoing spine surgery produce better health benefits? Med. Care 2014, 52, 1055–1063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adogwa, O.; Parker, S.L.; Shau, D.; Mendelhall, S.K.; Aaronson, O.; Cheng, J.; Devin, C.J.; McGirt, M.J. Cost per quality-adjusted life year gained of revision fusion for lumbar pseudoarthrosis: Defining the value of surgery. J. Spinal Disord. Tech. 2015, 28, 101–105. [Google Scholar] [CrossRef]
- Parker, S.L.; Anderson, L.H.; Nelson, T.; Patel, V.V. Cost-effectiveness of three treatment strategies for lumbar spinal stenosis: Conservative care, laminectomy, and the Superion interspinous spacer. Int. J. Spine Surg. 2015, 9, 28. [Google Scholar] [CrossRef] [Green Version]
- Whitmore, R.G.; Curran, J.N.; Ali, Z.S.; Mummaneni, P.V.; Shaffrey, C.I.; Heary, R.F.; Kaiser, M.G.; Asher, A.L.; Malhotra, N.R.; Cheng, J.S.; et al. Predictive value of 3-month lumbar discectomy outcomes in the NeuroPoint-SD Registry. J. Neurosurg. Spine 2015, 23, 459–466. [Google Scholar] [CrossRef] [Green Version]
- Ament, J.D.; Thaci, B.; Yang, Z.; Kursumovic, A.; Bostelmann, R.; Lanman, T.; Patrick Johnson, J.; Fröhlich, S.; Kim, K.D. Postoperative direct health care costs of lumbar discectomy are reduced with the use of a novel annular closure device in high-risk patients. Spine J. 2019, 19, 1170–1179. [Google Scholar] [CrossRef]
- Djurasovic, M.; Gum, J.L.; Crawford, C.H.; Owens, K.; Brown, M.; Steele, P.; Glassman, S.D.; Carreon, L.Y. Cost-effectiveness of minimally invasive midline lumbar interbody fusion versus traditional open transforaminal lumbar interbody fusion. J. Neurosurg. Spine 2019, 32, 31–35. [Google Scholar] [CrossRef]
- Lewandrowski, K.U. Incidence, Management, and Cost of Complications After Transforaminal Endoscopic Decompression Surgery for Lumbar Foraminal and Lateral Recess Stenosis: A Value Proposition for Outpatient Ambulatory Surgery. Int. J. Spine Surg. 2019, 13, 53–67. [Google Scholar] [CrossRef]
- Wang, D.; Xie, W.; Cao, W.; He, S.; Fan, G.; Zhang, H. A Cost-utility Analysis of Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Lumbar Disc Herniation: Transforaminal versus Interlaminar. Spine 2019, 44, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Weir, S.; Samnaliev, M.; Kuo, T.C.; Tierney, T.S.; Manca, A.; Taylor, R.S.; Bruce, J.; Eldabe, S.; Cumming, D. Persistent postoperative pain and healthcare costs associated with instrumented and non-instrumented spinal surgery: A case-control study. J. Orthop. Surg. Res. 2020, 15, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, J.N.; Lurie, J.D.; Tosteson, T.D.; Hanscom, B.; Tosteson, A.N.; Blood, E.A.; Birkmeyer, N.J.; Hilibrand, A.S.; Herkowitz, H.; Cammisa, F.P.; et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N. Engl. J. Med. 2007, 356, 2257–2270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, J.N.; Tosteson, T.D.; Lurie, J.D.; Tosteson, A.N.; Blood, E.; Hanscom, B.; Herkowitz, H.; Cammisa, F.; Albert, T.; Boden, S.D.; et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N. Engl. J. Med. 2008, 358, 794–810. [Google Scholar] [CrossRef] [Green Version]
- Radcliff, K.E.; Rihn, J.; Hilibrand, A.; DiIorio, T.; Tosteson, T.; Lurie, J.D.; Zhao, W.; Vaccaro, A.R.; Albert, T.J.; Weinstein, J.N. Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes? Analysis of the Spine Outcomes Research Trial. Spine 2011, 36, 2197–2210. [Google Scholar] [CrossRef] [Green Version]
- Kerr, D.; Zhao, W.; Lurie, J.D. What Are Long-term Predictors of Outcomes for Lumbar Disc Herniation? A Randomized and Observational Study. Clin. Orthop. Relat. Res. 2015, 473, 1920–1930. [Google Scholar] [CrossRef] [Green Version]
- Tsou, P.M.; Alan Yeung, C.; Yeung, A.T. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: A minimal access visualized intradiscal surgical procedure. Spine J. 2004, 4, 564–573. [Google Scholar] [CrossRef]
- Yeung, A.T.; Gore, S. In-vivo Endoscopic Visualization of Patho-anatomy in Symptomatic Degenerative Conditions of the Lumbar Spine II: Intradiscal, Foraminal, and Central Canal Decompression. Surg. Technol. Int. 2011, 21, 299–319. [Google Scholar]
- Gore, S.; Yeung, A. The "inside out" transforaminal technique to treat lumbar spinal pain in an awake and aware patient under local anesthesia: Results and a review of the literature. Int. J. Spine Surg. 2014, 8, 28. [Google Scholar] [CrossRef] [Green Version]
- Yeung, A.; Gore, S. Endoscopic foraminal decompression for failed back surgery syndrome under local anesthesia. Int. J. Spine Surg. 2014, 8, 22. [Google Scholar] [CrossRef] [Green Version]
- Lewandrowski, K.U.; Yeung, A. Lumbar Endoscopic Bony and Soft Tissue Decompression With the Hybridized Inside-Out Approach: A Review And Technical Note. Neurospine 2020, 17 (Suppl. S1), S34–S43. [Google Scholar] [CrossRef] [PubMed]
- Lewandrowski, K.-U.; Yeung, A. Meaningful outcome research to validate endoscopic treatment of common lumbar pain generators with durability analysis. J. Spine Surg. 2019, 6 (Suppl. S1), S6–S13. [Google Scholar] [CrossRef] [PubMed]
- Dregalla, R.C.; Uribe, Y.; Bodor, M. Human mesenchymal stem cells respond differentially to platelet preparations and synthesize hyaluronic acid in nucleus pulposus extracellular matrix. Spine J. 2020, 20, 1850–1860. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.J.; Hung, C.Y.; Lee, C.W.; Lam, S.; Clark, T.B.; Chang, K.V. Ultrasound-Guided Lumbar Intradiscal Injection for Discogenic Pain: Technical Innovation and Presentation of Two Cases. J. Pain Res. 2020, 13, 1103–1107. [Google Scholar] [CrossRef]
- Everts, P.A.; van Erp, A.; DeSimone, A.; Cohen, D.S.; Gardner, R.D. Platelet Rich Plasma in Orthopedic Surgical Medicine. Platelets 2021, 32, 163–174. [Google Scholar] [CrossRef]
- Pereira, P.; Severo, M.; Monteiro, P.; Silva, P.A.; Rebelo, V.; Castro-Lopes, J.M.; Vaz, R. Results of Lumbar Endoscopic Adhesiolysis Using a Radiofrequency Catheter in Patients with Postoperative Fibrosis and Persistent or Recurrent Symptoms After Discectomy. Pain Pract. 2016, 16, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Lewandrowski, K.U.; Ransom, N.A.; Yeung, A. Subsidence induced recurrent radiculopathy after staged two-level standalone endoscopic lumbar interbody fusion with a threaded cylindrical cage: A case report. J. Spine Surg. 2020, 6 (Suppl. S1), S286–S293. [Google Scholar] [CrossRef]
- Sidhu, G.S.; Henkelman, E.; Vaccaro, A.R.; Albert, T.J.; Hilibrand, A.; Anderson, D.G.; Rihn, J.A. Minimally invasive versus open posterior lumbar interbody fusion: A systematic review. Clin. Orthop. Relat. Res. 2014, 472, 1792–1799. [Google Scholar] [CrossRef] [Green Version]
- Mullin, B.B.; Rea, G.L.; Irsik, R.; Catton, M.; Miner, M.E. The effect of postlaminectomy spinal instability on the outcome of lumbar spinal stenosis patients. J. Spinal Disord. 1996, 9, 107–116. [Google Scholar] [CrossRef]
- Katzell, J.L. Risk factors predicting less favorable outcomes in endoscopic lumbar discectomies. J. Spine Surg. 2020, 6 (Suppl. S1), S155–S164. [Google Scholar] [CrossRef]
- Lee, C.S.; Hwang, C.J.; Lee, S.W.; Ahn, Y.J.; Kim, Y.T.; Lee, D.H.; Lee, M.Y. Risk factors for adjacent segment disease after lumbar fusion. Eur. Spine J. 2009, 18, 1637–1643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boswell, M.V.; Shah, R.V.; Everett, C.R.; Sehgal, N.; McKenzie Brown, A.M.; Abdi, S.; Bowman, R.C., 2nd; Deer, T.R.; Datta, S.; Colson, J.D.; et al. Interventional techniques in the management of chronic spinal pain: Evidence-based practice guidelines. Pain Physician 2005, 8, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Boswell, M.V.; Trescot, A.M.; Datta, S.; Schultz, D.M.; Hansen, H.C.; Abdi, S.; Sehgal, N.; Shah, R.V.; Singh, V.; Benyamin, R.M.; et al. Interventional techniques: Evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician 2007, 10, 7–111. [Google Scholar] [PubMed]
- Geurts, J.W.; Kallewaard, J.W.; Richardson, J.; Groen, G.J. Targeted methylprednisolone acetate/hyaluronidase/clonidine injection after diagnostic epiduroscopy for chronic sciatica: A prospective, 1-year follow-up study. Reg. Anesth. Pain Med. 2002, 27, 343–352. [Google Scholar] [CrossRef]
- Lee, I.S.; Kim, S.H.; Lee, J.W.; Hong, S.H.; Choi, J.Y.; Kang, H.S.; Song, J.W.; Kwon, A.K. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: Conventional versus posterolateral technique. AJNR Am. J. Neuroradiol. 2007, 28, 204–208. [Google Scholar]
- Lee, J.W.; Kim, S.H.; Lee, I.S.; Choi, J.A.; Choi, J.Y.; Hong, S.H.; Kang, H.S. Therapeutic effect and outcome predictors of sciatica treated using transforaminal epidural steroid injection. AJR Am. J. Roentgenol. 2006, 187, 1427–1431. [Google Scholar] [CrossRef]
- Lewandrowski, K.U. Successful outcome after outpatient transforaminal decompression for lumbar foraminal and lateral recess stenosis: The positive predictive value of diagnostic epidural steroid injection. Clin. Neurol. Neurosurg. 2018, 173, 38–45. [Google Scholar] [CrossRef]
- Battaglia, P.J.; Maeda, Y.; Welk, A.; Hough, B.; Kettner, N. Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J. Manip. Physiol. Ther. 2014, 37, 190–197. [Google Scholar] [CrossRef]
- Mysliwiec, L.W.; Cholewicki, J.; Winkelpleck, M.D.; Eis, G.P. MSU classification for herniated lumbar discs on MRI: Toward developing objective criteria for surgical selection. Eur. Spine J. 2010, 19, 1087–1093. [Google Scholar] [CrossRef] [Green Version]
- Thalgott, J.S.; Albert, T.J.; Vaccaro, A.R.; Aprill, C.N.; Giuffre, J.M.; Drake, J.S.; Henke, J.P. A new classification system for degenerative disc disease of the lumbar spine based on magnetic resonance imaging, provocative discography, plain radiographs and anatomic considerations. Spine J. 2004, 4, 167s–172s. [Google Scholar] [CrossRef]
- Hasegawa, T.; An, H.S.; Haughton, V.M.; Nowicki, B.H. Lumbar foraminal stenosis: Critical heights of the intervertebral discs and foramina. A cryomicrotome study in cadavera. J. Bone Jt. Surg. Am. 1995, 77, 32–38. [Google Scholar] [CrossRef]
- Reed, C.C.; Wolf, W.A.; Cotton, C.C.; Dellon, E.S. A visual analogue scale and a Likert scale are simple and responsive tools for assessing dysphagia in eosinophilic oesophagitis. Aliment. Pharm. Ther. 2017, 45, 1443–1448. [Google Scholar] [CrossRef] [PubMed]
- Macnab, I. The surgery of lumbar disc degeneration. Surg. Annu. 1976, 8, 447–480. [Google Scholar] [PubMed]
- Tsou, P.M.; Yeung, A.T. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: Outcome and technique. Spine J. 2002, 2, 41–48. [Google Scholar] [CrossRef]
- Yeung, A.T. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon’s Experience Incorporating Adjunctive Techologies. SAS J. 2007, 1, 108–117. [Google Scholar] [CrossRef] [Green Version]
- Hoogland, T.; Schubert, M.; Miklitz, B.; Ramirez, A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: A prospective randomized study in 280 consecutive cases. Spine 2006, 31, E890–E897. [Google Scholar] [CrossRef]
- Hoogland, T.; van den Brekel-Dijkstra, K.; Schubert, M.; Miklitz, B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: A prospective, cohort evaluation of 262 consecutive cases. Spine 2008, 33, 973–978. [Google Scholar] [CrossRef] [Green Version]
- Lewandrowski, K.U. “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: A retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int. J. Spine Surg. 2014, 8, 26. [Google Scholar] [CrossRef] [Green Version]
- Lewandrowski, K.U. The strategies behind “inside-out” and “outside-in” endoscopy of the lumbar spine: Treating the pain generator. J. Spine Surg. 2020, 6 (Suppl. S1), S35–S39. [Google Scholar] [CrossRef]
- Choi, W.S.; Kim, J.S.; Hur, J.W.; Seong, J.H. Minimally Invasive Transforaminal Lumbar Interbody Fusion Using Banana-Shaped and Straight Cages: Radiological and Clinical Results from a Prospective Randomized Clinical Trial. Neurosurgery 2018, 82, 289–298. [Google Scholar] [CrossRef]
- McClelland, S., 3rd; Goldstein, J.A. Minimally Invasive versus Open Spine Surgery: What Does the Best Evidence Tell Us? J. Neurosci. Rural Pract. 2017, 8, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Hawasli, A.H.; Khalifeh, J.M.; Chatrath, A.; Yarbrough, C.K.; Ray, W.Z. Minimally invasive transforaminal lumbar interbody fusion with expandable versus static interbody devices: Radiographic assessment of sagittal segmental and pelvic parameters. Neurosurg. Focus 2017, 43, E10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.W.; Doerr, T.M.; Luna, I.Y.; Joshua, G.; Shen, S.R.; Fu, X.; Wu, A.M. Minimally Invasive Transforaminal Lumbar Interbody Fusion Using Expandable Technology: A Clinical and Radiographic Analysis of 50 Patients. World Neurosurg. 2016, 90, 228–235. [Google Scholar] [CrossRef]
- Choi, W.S.; Kim, J.S.; Ryu, K.S.; Hur, J.W.; Seong, J.H. Minimally Invasive Transforaminal Lumbar Interbody Fusion at L5-S1 through a Unilateral Approach: Technical Feasibility and Outcomes. BioMed Res. Int. 2016, 2016, 2518394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.A.; Zfass-Mendez, M.; Lebwohl, N.H.; Wang, M.Y.; Green, B.A.; Levi, A.D.; Vanni, S.; Williams, S.K. Minimally Invasive Versus Open Lumbar Fusion: A Comparison of Blood Loss, Surgical Complications, and Hospital Course. Iowa Orthop. J. 2015, 35, 130–134. [Google Scholar]
- Lewandrowski, K.U.; Dowling, A.; Calderaro, A.L.; Dos Santos, T.S.; Bergamaschi, J.P.M.; Leon, J.F.R.; Yeung, A. Dysethesia due to irritation of the dorsal root ganglion following lumbar transforaminal endoscopy: Analysis of frequency and contributing factors. Clin. Neurol. Neurosurg. 2020, 197, 106073. [Google Scholar] [CrossRef]
- Kaplan, E.; Meier, P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Lewandrowski, K.U.; Ransom, N.A. Five-year clinical outcomes with endoscopic transforaminal outside-in foraminoplasty techniques for symptomatic degenerative conditions of the lumbar spine. J. Spine Surg. 2020, 6 (Suppl. S1), S54–S65. [Google Scholar] [CrossRef]
- Yeung, A.; Lewandrowski, K.U. Five-year clinical outcomes with endoscopic transforaminal foraminoplasty for symptomatic degenerative conditions of the lumbar spine: A comparative study of inside-out versus outside-in techniques. J. Spine Surg. 2020, 6 (Suppl. S1), S66–S83. [Google Scholar] [CrossRef]
- Wang, X.; Borgman, B.; Vertuani, S.; Nilsson, J. A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv. Res. 2017, 17, 446. [Google Scholar] [CrossRef] [Green Version]
- Lewandrowski, K.U.; Abraham, I.; Ramírez León, J.F.; Soriano Sánchez, J.A.; Dowling, Á.; Hellinger, S.; Freitas Ramos, M.R.; Teixeira De Carvalho, P.S.; Yeung, C.; Salari, N.; et al. Differential Agnostic Effect Size Analysis of Lumbar Stenosis Surgeries. Int. J. Spine Surg. 2022, 16, 318–342. [Google Scholar] [CrossRef] [PubMed]
- Lewandrowski, K.U.; de Carvalho, P.S.T.; de Carvalho, P.A.U.L.O.; Yeung, A. Minimal Clinically Important Difference in Patient-Reported Outcome Measures with the Transforaminal Endoscopic Decompression for Lateral Recess and Foraminal Stenosis. Int. J. Spine Surg. 2020, 14, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Jarebi, M.; Awaf, A.; Lefranc, M.; Peltier, J. A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: A 2-year retrospective cohort study. Spine J. 2021, 21, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Gadjradj, P.S.; Harhangi, B.S.; Amelink, J.; van Susante, J.; Kamper, S.; van Tulder, M.; Peul, W.C.; Vleggeert-Lankamp, C.; Rubinstein, S.M. Percutaneous Transforaminal Endoscopic Discectomy Versus Open Microdiscectomy for Lumbar Disc Herniation: A Systematic Review and Meta-analysis. Spine 2021, 46, 538–549. [Google Scholar] [CrossRef]
- Yun, D.J.; Park, S.J.; Lee, S.H. Open Lumbar Microdiscectomy and Posterolateral Endoscopic Lumbar Discectomy for Antero- and Retrospondylolisthesis. Pain Physician 2020, 23, 393–404. [Google Scholar] [CrossRef]
- Bechara, B.P.; Agarwal, V.; Boardman, J.; Perera, S.; Weiner, D.K.; Vo, N.; Kang, J.; Sowa, G.A. Correlation of pain with objective quantification of magnetic resonance images in older adults with chronic low back pain. Spine 2014, 39, 469–475. [Google Scholar] [CrossRef]
- Nami, M.; Thatcher, R.; Kashou, N.; Lopes, D.; Lobo, M.; Bolanos, J.F.; Morris, K.; Sadri, M.; Bustos, T.; Sanchez, G.E.; et al. A Proposed Brain-, Spine-, and Mental- Health Screening Methodology (NEUROSCREEN) for Healthcare Systems: Position of the Society for Brain Mapping and Therapeutics. J. Alzheimers Dis. 2022, 86, 21–42. [Google Scholar] [CrossRef]
- Cummins, D.D.; Callahan, M.; Scheffler, A.; Theologis, A.A. 5-Year Revision Rates After Elective Multilevel Lumbar/Thoracolumbar Instrumented Fusions in Older Patients: An Analysis of State Databases. J. Am. Acad. Orthop. Surg. 2022, 30, 476–483. [Google Scholar] [CrossRef]
- Katz, J.N.; Zimmerman, Z.E.; Mass, H.; Makhni, M.C. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA 2022, 327, 1688–1699. [Google Scholar] [CrossRef]
- Ziino, C.; Mertz, K.; Hu, S.; Kamal, R. Decompression With or Without Fusion for Lumbar Stenosis: A Cost Minimization Analysis. Spine 2020, 45, 325–332. [Google Scholar] [CrossRef]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010, 303, 1259–1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, J.N.; Lurie, J.D.; Olson, P.R.; Bronner, K.K.; Fisher, E.S. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine 2006, 31, 2707–2714. [Google Scholar] [CrossRef] [PubMed]
- Parker, S.L.; Adogwa, O.; Bydon, A.; Cheng, J.; McGirt, M.J. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. 2012, 78, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Yeramaneni, S.; Kebaish, K.M.; Raad, M.; Gum, J.L.; Klineberg, E.O.; Hassanzadeh, H.; Kelly, M.P.; Passias, P.G.; Ames, C.P.; et al. Cost-Utility Analysis of rhBMP-2 Use in Adult Spinal Deformity Surgery. Spine 2020, 45, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Atlas, S.J.; Keller, R.B.; Wu, Y.A.; Deyo, R.A.; Singer, D.E. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine 2005, 30, 936–943. [Google Scholar] [CrossRef] [Green Version]
- Toivonen, L.A.; Mäntymäki, H.; Häkkinen, A.; Kautiainen, H.; Neva, M.H. Isthmic Spondylolisthesis is Associated with Less Revisions for Adjacent Segment Disease After Lumbar Spine Fusion Than Degenerative Spinal Conditions: A 10-Year Follow-Up Study. Spine 2022, 47, 303–308. [Google Scholar] [CrossRef]
- Casper, D.S.; Schroeder, G.D.; Zmistowski, B.; Rihn, J.A.; Anderson, D.G.; Hilibrand, A.S.; Vaccaro, A.R.; Kepler, C.K. Medicaid Reimbursement for Common Orthopedic Procedures Is Not Consistent. Orthopedics 2019, 42, e193–e196. [Google Scholar] [CrossRef]
- Bajpai, J.; Saini, S.; Singh, R. Clinical correlation of magnetic resonance imaging with symptom complex in prolapsed intervertebral disc disease: A cross-sectional double blind analysis. J. Craniovertebr. Junction Spine 2013, 4, 16–20. [Google Scholar] [CrossRef]
- Okada, E.; Daimon, K.; Fujiwara, H.; Nishiwaki, Y.; Nojiri, K.; Watanabe, M.; Katoh, H.; Shimizu, K.; Ishihama, H.; Fujita, N.; et al. Twenty-year Longitudinal Follow-up MRI Study of Asymptomatic Volunteers: The Impact of Cervical Alignment on Disk Degeneration. Clin. Spine Surg. 2018, 31, 446–451. [Google Scholar] [CrossRef]
- Yeung, A.T.; Lewandrowski, K.U. Retrospective analysis of accuracy and positive predictive value of preoperative lumbar MRI grading after successful outcome following outpatient endoscopic decompression for lumbar foraminal and lateral recess stenosis. Clin. Neurol. Neurosurg. 2019, 181, 52. [Google Scholar] [CrossRef]
- Lewandrowski, K.U.; de Carvalho, P.S.T.; Calderaro, A.L.; Dos Santos, T.S.; de Lima, E.S.M.S.; de Carvalho, P., Jr.; Yeung, A. Outcomes with transforaminal endoscopic versus percutaneous laser decompression for contained lumbar herniated disc: A survival analysis of treatment benefit. J. Spine Surg. 2020, 6 (Suppl. S1), S84–S99. [Google Scholar] [CrossRef] [PubMed]
- Jasper, G.P.; Francisco, G.M.; Telfeian, A. Outpatient, awake, ultra-minimally invasive endoscopic treatment of lumbar disc herniations. Rhode Isl. Med. J. 2014, 97, 47–49. [Google Scholar]
- Lewandrowski, K.U. Readmissions After Outpatient Transforaminal Decompression for Lumbar Foraminal and Lateral Recess Stenosis. Int. J. Spine Surg. 2018, 12, 342–351. [Google Scholar] [CrossRef] [Green Version]
- Abrão, J.O.; Dowling, A.l.; León, J.F.R.R.; Lewandrowski, K.-U. Anesthesia For Endoscopic Spine Surgery Of The Spine In An Ambulatory Surgery Center. Glob. J. Anesth. Pain Med. (GJAPM) 2020, 3, 326–336. [Google Scholar] [CrossRef]
- McCulloch, P.; Taylor, I.; Sasako, M.; Lovett, B.; Griffin, D. Randomised trials in surgery: Problems and possible solutions. BMJ 2002, 324, 1448–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conroy, E.J.; Rosala-Hallas, A.; Blazeby, J.M.; Burnside, G.; Cook, J.A.; Gamble, C. Randomized trials involving surgery did not routinely report considerations of learning and clustering effects. J. Clin. Epidemiol. 2019, 107, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Robinson, N.B.; Fremes, S.; Hameed, I.; Rahouma, M.; Weidenmann, V.; Demetres, M.; Morsi, M.; Soletti, G.; Di Franco, A.; Zenati, M.A.; et al. Characteristics of Randomized Clinical Trials in Surgery From 2008 to 2020: A Systematic Review. JAMA Netw. Open 2021, 4, e2114494. [Google Scholar] [CrossRef]
- Solheim, O. Randomized controlled trials in surgery and the glass ceiling effect. Acta Neurochir. 2019, 161, 623–625. [Google Scholar] [CrossRef] [Green Version]
- Wartolowska, K.; Collins, G.S.; Hopewell, S.; Judge, A.; Dean, B.J.; Rombach, I.; Beard, D.J.; Carr, A.J. Feasibility of surgical randomised controlled trials with a placebo arm: A systematic review. BMJ Open 2016, 6, e010194. [Google Scholar] [CrossRef]



| Sugical Level | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| L2/3 | 18 | 4.4 | 4.4 |
| L2/3 L3/4 | 2 | 0.5 | 4.9 |
| L3-5 | 4 | 1.0 | 5.8 |
| L3/4 | 28 | 6.8 | 12.6 |
| L3/4 L5/S1 | 2 | 0.5 | 13.1 |
| L3/4 L4-S1 | 6 | 1.5 | 14.6 |
| L3/4 L4/5 | 12 | 2.9 | 17.5 |
| L4-S1 | 67 | 16.3 | 33.7 |
| L4/5 | 170 | 41.3 | 75.0 |
| L5/S1 | 103 | 25.0 | 100.0 |
| Total | 412 | 100.0 |
| Endoscopically Visualized Pain Generator | MRI Negative | MRI Positive | Total: |
|---|---|---|---|
| Hypertrophied Ligamentum Flavum | 7 | 35 | 42 |
| 7.3% | 31.8% | 20.4% | |
| Contained Herniated Disc | 6 | 25 | 31 |
| 6.3% | 22.7% | 15.0% | |
| Hypertrophied Superior Articular Process | 3 | 24 | 27 |
| 3.1% | 21.8% | 13.1% | |
| Inflammed Disc With Toxic Annular Tear | 25 | 0 | 25 |
| 26.0% | 0.0% | 12.1% | |
| Extruded Herniated Disc | 5 | 19 | 24 |
| 5.2% | 17.3% | 11.7% | |
| Delaminated And Fissured Disc Tissue | 17 | 0 | 17 |
| 17.7% | 0.0% | 8.3% | |
| Intra-Annular Granulation Tissue | 9 | 0 | 9 |
| 9.4% | 0.0% | 4.4% | |
| Facet Cyst | 1 | 7 | 8 |
| 1.0% | 6.4% | 3.9% | |
| Hidden Shoulder Osteophyte | 7 | 0 | 7 |
| 7.3% | 0.0% | 3.4% | |
| Inflamed Nerve | 6 | 0 | 6 |
| 6.3% | 0.0% | 2.9% | |
| Tethered and Furcal Nerve Roots | 6 | 0 | 6 |
| 6.3% | 0.0% | 2.9% | |
| Contracted Foraminal Ligaments | 4 | 0 | 4 |
| 4.2% | 0.0% | 1.9% | |
| Total ELD Patients | 96 | 110 | 206 |
| 100.0% | 100.0% | 100.0% |
| Control | Index Surgery Type | Total | |||
|---|---|---|---|---|---|
| Macnab Outcome | Recruited from patients referred for surgery, who declined | ELD | TLIF | Laminectomy | |
| Excellent | 16 | 110 | 27 | 13 | 166 |
| 9.6% | 66.3% | 16.3% | 7.8% | 100.0% | |
| Good | 24 | 74 | 42 | 40 | 180 |
| 13.3% | 41.1% | 23.3% | 22.2% | 100.0% | |
| Fair | 19 | 19 | 7 | 6 | 51 |
| 37.3% | 37.3% | 13.7% | 11.8% | 100.0% | |
| Poor | 8 | 3 | 2 | 2 | 15 |
| 53.3% | 20.0% | 13.3% | 13.3% | 100.0% | |
| Total: | 67 | 206 | 78 | 61 | 412 |
| 16.3% | 50.0% | 18.9% | 14.8% | 100.0% | |
| New Onset Postoperative Symptom | Type of Lumbar Index Surgery | Total | ||||
|---|---|---|---|---|---|---|
| Control | ELD | Laminectomy | TLIF | |||
| N/A | 0 | 143 | 37 | 12 | 192 | |
| 0.0% | 74.4% | 19.3% | 6.3% | 100.0% | ||
| Axial back pain | 0 | 11 | 20 | 9 | 40 | |
| 0.0% | 27.5% | 50.0% | 22.5% | 100.0% | ||
| Other level pain | 0 | 12 | 4 | 0 | 16 | |
| 0.0% | 75.0% | 25.0% | 0.0% | 100.0% | ||
| Persistent Pain | 16 | 3 | 2 | 0 | 21 | |
| 76.2% | 14.3% | 9.5% | 0.0% | 100.0% | ||
| Recurrent HNP | 0 | 9 | 0 | 0 | 9 | |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | ||
| Recurrent pain | 51 | 14 | 6 | 40 | 111 | |
| 45.9% | 12.6% | 5.4% | 36.0% | 100.0% | ||
| Sacral Iliac Joint Pain | 0 | 1 | 0 | 0 | 1 | |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | ||
| Same level other side pain | 0 | 11 | 9 | 0 | 20 | |
| 0.0% | 55.0% | 45.0% | 0.0% | 100.0% | ||
| Total: | 67 | 206 | 78 | 61 | 412 | |
| 16.3% | 50.0% | 18.9% | 14.8% | 100.0% | ||
| Chi-Square Tests | df | Asymptotic Significance (2-sided) | ||||
| Pearson Chi-Square = 312.275 | 24 | p < 0.001 | ||||
| Likelihood Ratio = 339.800 | 24 | p < 0.001 | ||||
| N of Valid Cases: 412 | ||||||
| Postoperative Treatments | Surgery Type | Total | |||
|---|---|---|---|---|---|
| Control | ELD | TLIF | Laminectomy | ||
| N/A | 15 | 125 | 31 | 12 | 183 |
| 8.2% | 68.3% | 16.9% | 6.6% | 100.0% | |
| TESI | 27 | 24 | 18 | 22 | 91 |
| 29.7% | 26.4% | 19.8% | 24.2% | 100.0% | |
| Adjacent Level TLIF | 0 | 0 | 2 | 0 | 2 |
| 0.0% | 0.0% | 100.0% | 0.0% | 100.0% | |
| ASD Fusion | 0 | 0 | 3 | 0 | 3 |
| 0.0% | 0.0% | 100.0% | 0.0% | 100.0% | |
| ASD Laminectomy | 0 | 0 | 1 | 0 | 1 |
| 0.0% | 0.0% | 100.0% | 0.0% | 100.0% | |
| ELD | 9 | 0 | 0 | 0 | 9 |
| 100.0% | 0.0% | 0.0% | 0.0% | 100.0% | |
| ELD Adjacent Level | 0 | 11 | 0 | 0 | 11 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| ELD Opposite side | 0 | 11 | 0 | 0 | 11 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| ELD same side and level | 0 | 2 | 0 | 0 | 2 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Hemilaminectomy | 0 | 1 | 0 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Laminectomy | 7 | 0 | 0 | 0 | 7 |
| 100.0% | 0.0% | 0.0% | 0.0% | 100.0% | |
| Multilevel Laminectomy | 0 | 1 | 0 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Multilevel Rhizotomy | 0 | 7 | 8 | 7 | 22 |
| 0.0% | 31.8% | 36.4% | 31.8% | 100.0% | |
| Repeat ELD For Recurrent HNP | 0 | 2 | 0 | 0 | 2 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Revision ELD | 0 | 0 | 0 | 7 | 7 |
| 0.0% | 0.0% | 0.0% | 100.0% | 100.0% | |
| Revision Laminectomy | 0 | 0 | 0 | 10 | 10 |
| 0.0% | 0.0% | 0.0% | 100.0% | 100.0% | |
| Revision TLIF | 0 | 14 | 15 | 3 | 32 |
| 0.0% | 43.8% | 46.9% | 9.4% | 100.0% | |
| Same and Adjacent Level TLIF | 0 | 1 | 0 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Same Level ALIF | 0 | 3 | 0 | 0 | 3 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Same Level Laminectomy | 0 | 1 | 0 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Same Level Rhizotomy | 0 | 2 | 0 | 0 | 2 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| SI Ablation | 0 | 1 | 0 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| TLIF | 9 | 0 | 0 | 0 | 9 |
| 100.0% | 0.0% | 0.0% | 0.0% | 100.0% | |
| 67 | 206 | 78 | 61 | 412 | |
| 16.3% | 50.0% | 18.9% | 14.8% | 100.0% | |
| Chi-Square Tests | df | Asymptotic Significance (2-sided | |||
| Pearson Chi-Square = 374.425 | 66 | p < 0.001 | |||
| Likelihood Ratio = 317.104 | 66 | p < 0.001 | |||
| N of Valid Cases: 412 | |||||
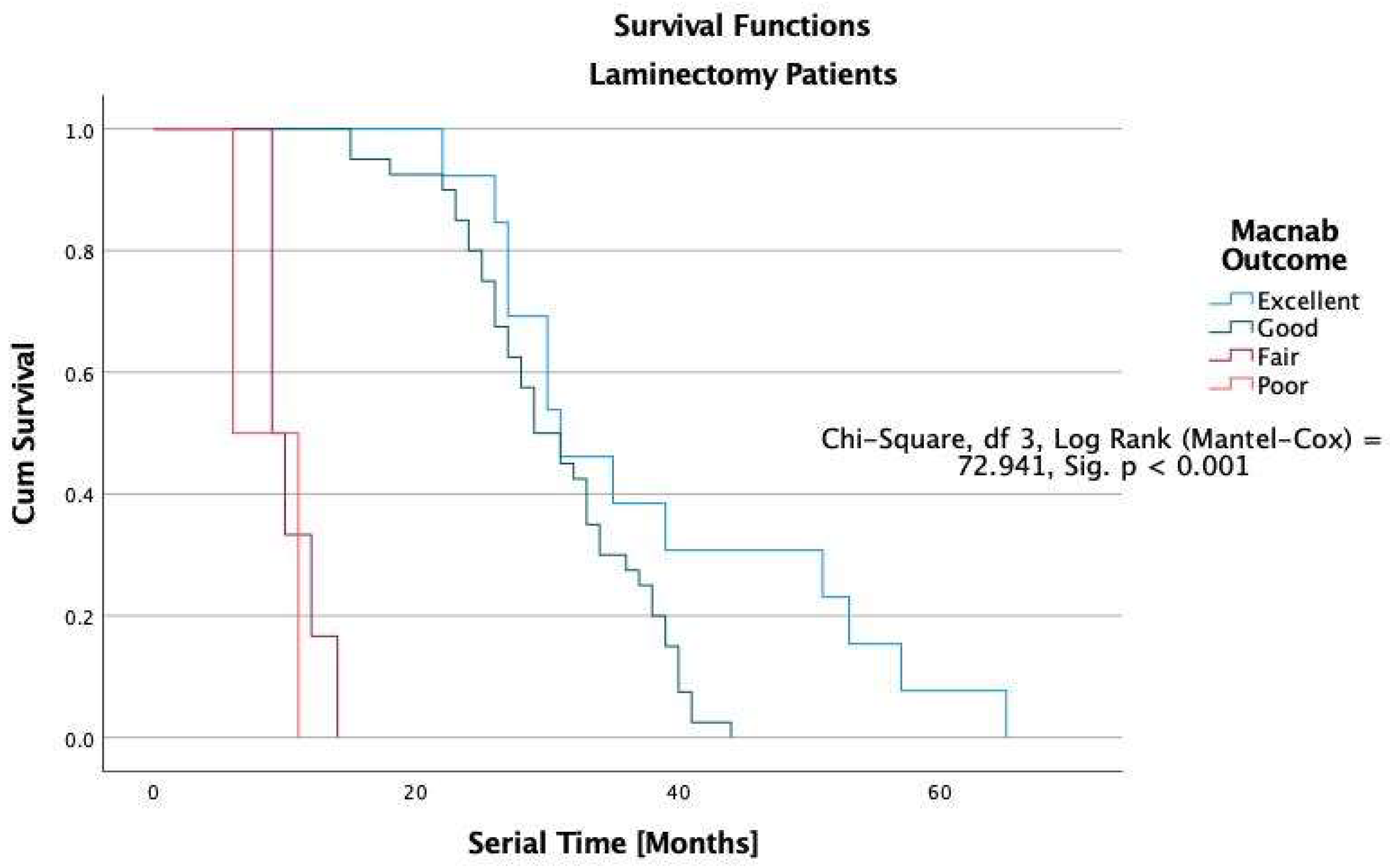
| Group | Macnab Outcome | Median | |||
|---|---|---|---|---|---|
| Estimate | Std. Error | 95% Confidence Interval | |||
| Lower Bound | Upper Bound | ||||
| Control | Excellent | 7.000 | 0.992 | 5.055 | 8.945 |
| Good | 7.000 | 1.225 | 4.600 | 9.400 | |
| Fair | 6.000 | 2.176 | 1.734 | 10.266 | |
| Poor | 71.000 | 4.950 | 61.298 | 80.702 | |
| Overall | 8.000 | 0.942 | 6.154 | 9.846 | |
| ELD | Excellent | 62.000 | 0.982 | 60.076 | 63.924 |
| Good | 31.000 | 8.124 | 15.076 | 46.924 | |
| Fair | 16.000 | 1.435 | 13.188 | 18.812 | |
| Poor | 5.000 | 1.633 | 1.799 | 8.201 | |
| Overall | 54.000 | 2.392 | 49.311 | 58.689 | |
| Laminectomy | Excellent | 31.000 | 3.595 | 23.954 | 38.046 |
| Good | 29.000 | 1.897 | 25.281 | 32.719 | |
| Fair | 9.000 | . | . | . | |
| Poor | 6.000 | . | . | . | |
| Overall | 29.000 | 1.672 | 25.724 | 32.276 | |
| TLIF | Excellent | 43.000 | 1.731 | 39.608 | 46.392 |
| Good | 31.000 | 2.592 | 25.919 | 36.081 | |
| Fair | 12.000 | 1.309 | 9.434 | 14.566 | |
| Poor | 4.000 | . | . | . | |
| Overall | 36.000 | 2.752 | 30.607 | 41.393 | |
| Overall | Overall | 38.000 | 1.864 | 34.347 | 41.653 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandrowski, K.-U.; Abraham, I.; Ramírez León, J.F.; Telfeian, A.E.; Lorio, M.P.; Hellinger, S.; Knight, M.; De Carvalho, P.S.T.; Ramos, M.R.F.; Dowling, Á.; et al. A Proposed Personalized Spine Care Protocol (SpineScreen) to Treat Visualized Pain Generators: An Illustrative Study Comparing Clinical Outcomes and Postoperative Reoperations between Targeted Endoscopic Lumbar Decompression Surgery, Minimally Invasive TLIF and Open Laminectomy. J. Pers. Med. 2022, 12, 1065. https://doi.org/10.3390/jpm12071065
Lewandrowski K-U, Abraham I, Ramírez León JF, Telfeian AE, Lorio MP, Hellinger S, Knight M, De Carvalho PST, Ramos MRF, Dowling Á, et al. A Proposed Personalized Spine Care Protocol (SpineScreen) to Treat Visualized Pain Generators: An Illustrative Study Comparing Clinical Outcomes and Postoperative Reoperations between Targeted Endoscopic Lumbar Decompression Surgery, Minimally Invasive TLIF and Open Laminectomy. Journal of Personalized Medicine. 2022; 12(7):1065. https://doi.org/10.3390/jpm12071065
Chicago/Turabian StyleLewandrowski, Kai-Uwe, Ivo Abraham, Jorge Felipe Ramírez León, Albert E. Telfeian, Morgan P. Lorio, Stefan Hellinger, Martin Knight, Paulo Sérgio Teixeira De Carvalho, Max Rogério Freitas Ramos, Álvaro Dowling, and et al. 2022. "A Proposed Personalized Spine Care Protocol (SpineScreen) to Treat Visualized Pain Generators: An Illustrative Study Comparing Clinical Outcomes and Postoperative Reoperations between Targeted Endoscopic Lumbar Decompression Surgery, Minimally Invasive TLIF and Open Laminectomy" Journal of Personalized Medicine 12, no. 7: 1065. https://doi.org/10.3390/jpm12071065
APA StyleLewandrowski, K.-U., Abraham, I., Ramírez León, J. F., Telfeian, A. E., Lorio, M. P., Hellinger, S., Knight, M., De Carvalho, P. S. T., Ramos, M. R. F., Dowling, Á., Rodriguez Garcia, M., Muhammad, F., Hussain, N., Yamamoto, V., Kateb, B., & Yeung, A. (2022). A Proposed Personalized Spine Care Protocol (SpineScreen) to Treat Visualized Pain Generators: An Illustrative Study Comparing Clinical Outcomes and Postoperative Reoperations between Targeted Endoscopic Lumbar Decompression Surgery, Minimally Invasive TLIF and Open Laminectomy. Journal of Personalized Medicine, 12(7), 1065. https://doi.org/10.3390/jpm12071065










