Digital Anthropometry for Body Circumference Measurements: European Phenotypic Variations throughout the Decades
Abstract
1. Introduction
2. Assessment of Waist and Hip Circumferences
3. Assessment of Limb Circumferences
4. Digital Anthropometry
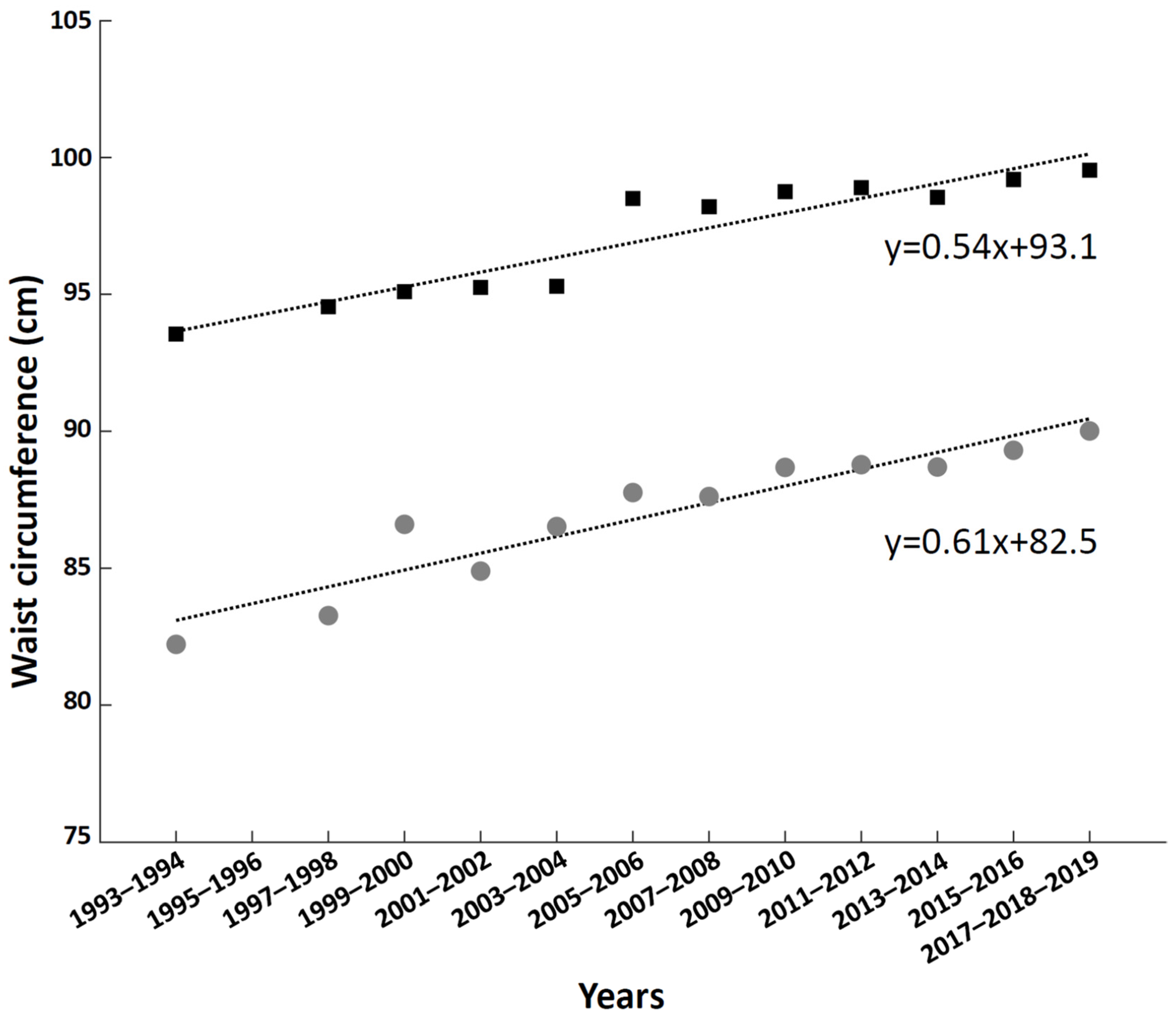
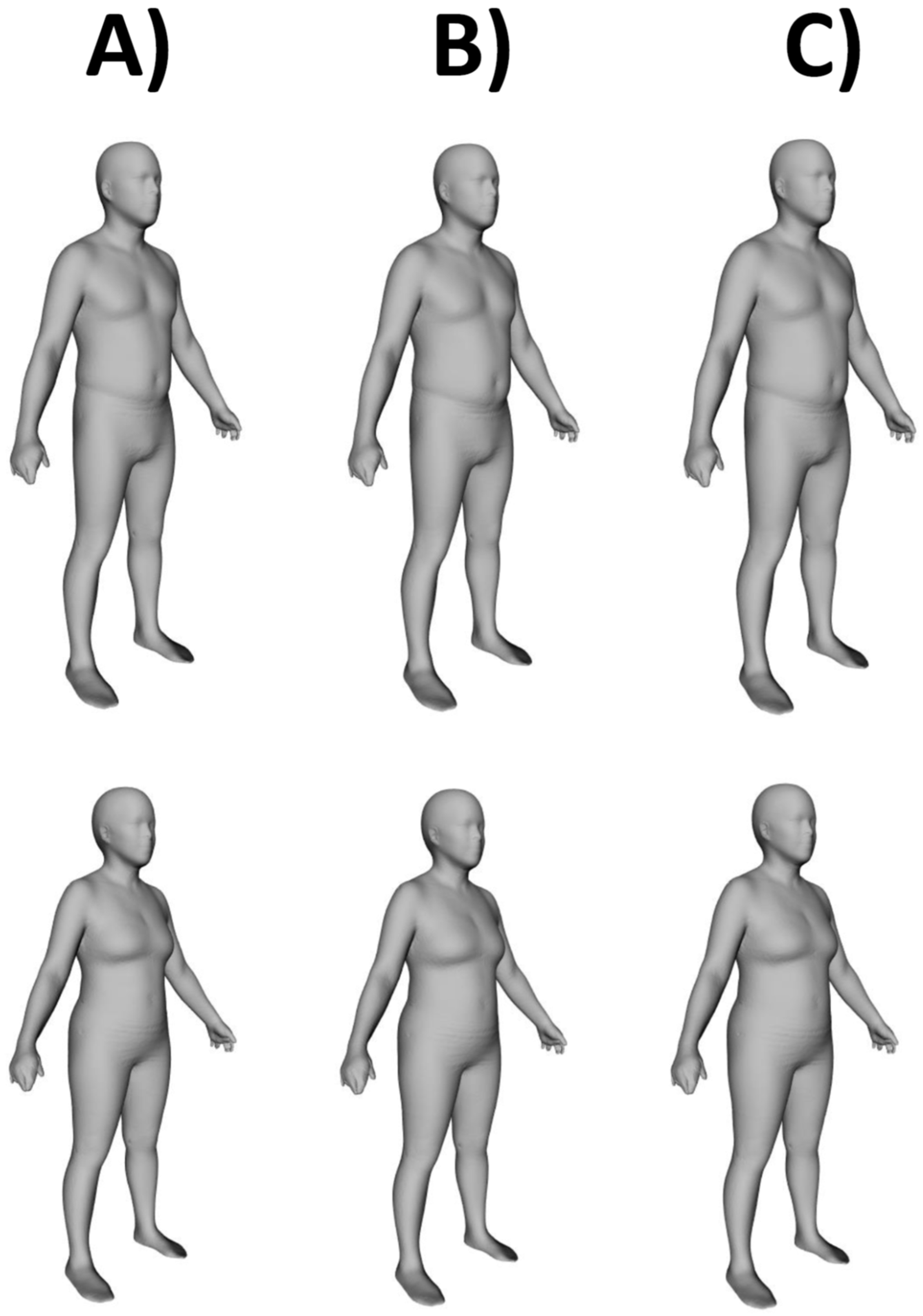
5. European Phenotypic Variations throughout the Decades
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Chromy, A.; Zalud, L.; Dobsak, P.; Suskevic, I.; Mrkvicova, V. Limb volume measurements: Comparison of accuracy and decisive parameters of the most used present methods. Springerplus 2015, 4, 707. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Committee on Physical Status: The Use and Interpretation of Anthropometry (1993: Geneva Switzerland) & World Health Organization. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee. World Health Organization. 1995. Available online: https://apps.who.int/iris/handle/10665/37003 (accessed on 20 May 2021).
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 1998; pp. 51S–209S.
- Huang, P.L. A comprehensive definition for metabolic syndrome. Dis. Model. Mech. 2009, 2, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation (8–11 December 2008, Geneva, Switzerland). World Health Organization. 2011. Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 23 March 2022).
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.C.; Correia, M.I.T.D.; Heymsfield, S.B. A requiem for BMI in the clinical setting. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Bozeman, S.R.; Hoaglin, D.C.; Burton, T.M.; Pashos, C.L.; Ben-Joseph, R.H.; Hollenbeak, C.S. Predicting waist circumference from body mass index. BMC Med. Res. Methodol. 2012, 12, 115. [Google Scholar] [CrossRef]
- Lee, D.H.; Keum, N.; Hu, F.B.; Orav, E.J.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Giovannucci, E.L. Development and validation of anthropometric prediction equations for lean body mass, fat mass and percent fat in adults using the National Health and Nutrition Examination Survey (NHANES) 1999–2006. Br. J. Nutr. 2017, 118, 858–866. [Google Scholar] [CrossRef]
- Woolcott, O.O.; Bergman, R.N. Relative fat mass (RFM) as a new estimator of whole-body fat percentage—A cross-sectional study in American adult individuals. Sci. Rep. 2018, 8, 10980. [Google Scholar] [CrossRef]
- Al-Gindan, Y.Y.; Hankey, C.; Govan, L.; Gallagher, D.; Heymsfield, S.B.; Lean, M.E. Derivation and validation of simple equations to predict total muscle mass from simple anthropometric and demographic data. Am. J. Clin. Nutr. 2014, 100, 1041–1051. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Stanley, A.; Pietrobelli, A.; Heo, M. Simple Skeletal Muscle Mass Estimation Formulas: What We Can Learn from Them. Front. Endocrinol. 2020, 11, 31. [Google Scholar] [CrossRef]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef]
- Lee, C.M.; Huxley, R.R.; Wildman, R.P.; Woodward, M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: A meta-analysis. J. Clin. Epidemiol. 2008, 61, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Thornton, J.C.; Pi-Sunyer, F.X.; Heymsfield, S.B.; Wang, J.; Pierson, R.N., Jr.; Blanck, H.M.; Gallagher, D. The body adiposity index (hip circumference ÷ height (1.5)) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity 2012, 20, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Heitmann, B.L.; Frederiksen, P. Thigh circumference and risk of heart disease and premature death: Prospective cohort study. BMJ 2009, 339, b3292. [Google Scholar] [CrossRef]
- Ashwell, M.; Chinn, S.; Stalley, S.; Garrow, J.S. Female fat distribution-a simple classification based on two circumference measurements. Int. J. Obes. 1982, 6, 143–152. [Google Scholar]
- Seidell, J.C.; Oosterlee, A.; Thijssen, M.A.; Burema, J.; Deurenberg, P.; Hautvast, J.G.; Ruijs, J.H. Assessment of intra-abdominal and subcutaneous abdominal fat: Relation between anthropometry and computed tomography. Am. J. Clin. Nutr. 1987, 45, 7–13. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Hsu, K.H.; Hwang, C.J.; Hu, P.M.; Lin, T.M.; Chiou, W.K. Waist-to-thigh ratio can also be a better indicator associated with type 2 diabetes than traditional anthropometrical measurements in Taiwan population. Ann. Epidemiol. 2006, 16, 321–331. [Google Scholar] [CrossRef]
- Li, C.; Ford, E.S.; Zhao, G.; Kahn, H.S.; Mokdad, A.H. Waist-to-thigh ratio and diabetes among US adults: The Third National Health and Nutrition Examination Survey. Diabetes Res. Clin. Pract. 2010, 89, 79–87. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. An Anthropometric Risk Index Based on Combining Height, Weight, Waist, and Hip Measurements. J. Obes. 2016, 2016, 8094275. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Tsilidis, K.K.; Muller, D.C.; Freisling, H.; Weiderpass, E.; Overvad, K.; Söderberg, S.; Häggström, C.; Pischon, T.; Dahm, C.C.; et al. A Body Shape Index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: Results from a large European cohort. Sci. Rep. 2020, 10, 14541. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Tsilidis, K.K.; Evangelou, E.; Riboli, E. Association of body-shape phenotypes with imaging measures of body composition in the UK Biobank cohort: Relevance to colon cancer risk. BMC Cancer 2021, 21, 1106. [Google Scholar] [CrossRef]
- Christakoudi, S.; Tsilidis, K.K.; Evangelou, E.; Riboli, E. A Body Shape Index (ABSI), hip index, and risk of cancer in the UK Biobank cohort. Cancer Med. 2021, 10, 5614–5628. [Google Scholar] [CrossRef]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef]
- Rico-Martín, S.; Calderón-García, J.F.; Sánchez-Rey, P.; Franco-Antonio, C.; Martínez Alvarez, M.; Sánchez Muñoz-Torrero, J.F. Effectiveness of body roundness index in predicting metabolic syndrome: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13023. [Google Scholar] [CrossRef]
- Li, Y.; He, Y.; Yang, L.; Liu, Q.; Li, C.; Wang, Y.; Yang, P.; Wang, J.; Chen, Z.; Huang, X. Body Roundness Index and Waist-Hip Ratio Result in Better Cardiovascular Disease Risk Stratification: Results from a Large Chinese Cross-Sectional Study. Front. Nutr. 2022, 9, 801582. [Google Scholar] [CrossRef]
- Rolland, Y.; Lauwers-Cances, V.; Cournot, M.; Nourhashémi, F.; Reynish, W.; Rivière, D.; Vellas, B.; Grandjean, H. Sarcopenia, calf circumference, and physical function of elderly women: A cross-sectional study. J. Am. Geriatr. Soc. 2003, 51, 1120–1124. [Google Scholar] [CrossRef]
- Gonzalez, M.C.; Mehrnezhad, A.; Razaviarab, N.; Barbosa-Silva, T.G.; Heymsfield, S.B. Calf circumference: Cutoff values from the NHANES 1999–2006. Am. J. Clin. Nutr. 2021, 113, 1679–1687. [Google Scholar] [CrossRef]
- Ishii, S.; Tanaka, T.; Shibasaki, K.; Ouchi, Y.; Kikutani, T.; Higashiguchi, T.; Obuchi, S.P.; Ishikawa-Takata, K.; Hirano, H.; Kawai, H.; et al. Development of a simple screening test for sarcopenia in older adults. Geriatr. Gerontol. Int. 2014, 14, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, T.G.; Menezes, A.M.; Bielemann, R.M.; Malmstrom, T.K.; Gonzalez, M.C.; Grupo de Estudos em Composição Corporal e Nutrição (COCONUT). Enhancing SARC-F: Improving Sarcopenia Screening in the Clinical Practice. J. Am. Med. Dir. Assoc. 2016, 17, 1136–1141. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, V.; Nigg, B.M.; Hintermann, B.; Goepfert, B.; Dick, W.; Frank, C.B.; Herzog, W.; von Tscharner, V. Muscular lower leg asymmetry in middle-aged people. Foot Ankle Int. 2007, 28, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Lee, S.A.; Soh, Y.; Kim, Y.; Won, C.W.; Chon, J. Association between asymmetry in lower extremity lean mass and functional mobility in older adults living in the community: Results from the Korean Frailty and Aging Cohort Study. Medicine 2019, 98, e17882. [Google Scholar] [CrossRef] [PubMed]
- Stein, P.D.; Henry, J.W.; Gopalakrishnan, D.; Relyea, B. Asymmetry of the calves in the assessment of patients with suspected acute pulmonary embolism. Chest 1995, 107, 936–939. [Google Scholar] [CrossRef]
- Landi, F.; Russo, A.; Liperoti, R.; Pahor, M.; Tosato, M.; Capoluongo, E.; Bernabei, R.; Onder, G. Midarm muscle circumference, physical performance and mortality: Results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Clin. Nutr. 2010, 29, 441–447. [Google Scholar] [CrossRef]
- Landi, F.; Onder, G.; Russo, A.; Liperoti, R.; Tosato, M.; Martone, A.M.; Capoluongo, E.; Bernabei, R. Calf circumference, frailty and physical performance among older adults living in the community. Clin. Nutr. 2014, 33, 539–544. [Google Scholar] [CrossRef]
- Wei, J.; Jiao, J.; Chen, C.L.; Tao, W.Y.; Ying, Y.J.; Zhang, W.W.; Wu, X.J.; Zhang, X.M. The association between low calf circumference and mortality: A systematic review and meta-analysis. Eur. Geriatr. Med. 2022, 13, 597–609. [Google Scholar] [CrossRef]
- Guigoz, Y.; Lauque, S.; Vellas, B.J. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin. Geriatr. Med. 2002, 18, 737–757. [Google Scholar] [CrossRef]
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA-Its history and challenges. J. Nutr. Health Aging 2006, 10, 456–463. [Google Scholar]
- Deltombe, T.; Jamart, J.; Recloux, S.; Legrand, C.; Vandenbroeck, N.; Theys, S.; Hanson, P. Reliability and limits of agreement of circumferential, water displacement, and optoelectronic volumetry in the measurement of upper limb lymphedema. Lymphology 2007, 40, 26–34. [Google Scholar]
- Kaulesar Sukul, D.M.; den Hoed, P.T.; Johannes, E.J.; van Dolder, R.; Benda, E. Direct and indirect methods for the quantification of leg volume: Comparison between water displacement volumetry, the disk model method and the frustum sign model method, using the correlation coefficient and the limits of agreement. J. Biomed. Eng. 1993, 15, 477–480. [Google Scholar] [CrossRef]
- Nordhamn, K.; Södergren, E.; Olsson, E.; Karlström, B.; Vessby, B.; Berglund, L. Reliability of anthropometric measurements in overweight and lean subjects: Consequences for correlations between anthropometric and other variables. Int. J. Obes. Relat. Metab Disord. 2000, 24, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Verweij, L.M.; Terwee, C.B.; Proper, K.I.; Hulshof, C.T.; van Mechelen, W. Measurement error of waist circumference: Gaps in knowledge. Public Health Nutr. 2013, 16, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.P.; Liu, Y.E.; Quon, B.K.; Kelly, N.N.; Wong, M.C.; Kennedy, S.F.; Chow, D.C.; Garber, A.K.; Weiss, E.J.; Heymsfield, S.B.; et al. Assessment of clinical measures of total and regional body composition from a commercial 3-dimensional optical body scanner. Clin. Nutr. 2022, 41, 211–218. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Bourgeois, B.; Ng, B.K.; Sommer, M.J.; Li, X.; Shepherd, J.A. Digital anthropometry: A critical review. Eur. J. Clin. Nutr. 2018, 72, 680–687. [Google Scholar] [CrossRef]
- Sobhiyeh, S.; Kennedy, S.; Dunkel, A.; Dechenaud, M.E.; Weston, J.A.; Shepherd, J.; Wolenski, P.; Heymsfield, S.B. Digital anthropometry for body circumference measurements: Toward the development of universal three-dimensional optical system analysis software. Obes. Sci. Pract. 2020, 7, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Ng, B.K.; Hinton, B.J.; Fan, B.; Kanaya, A.M.; Shepherd, J.A. Clinical anthropometrics and body composition from 3D whole-body surface scans. Eur. J. Clin. Nutr. 2016, 70, 1265–1270. [Google Scholar] [CrossRef]
- Tinsley, G.M.; Moore, M.L.; Benavides, M.L.; Dellinger, J.R.; Adamson, B.T. 3-Dimensional optical scanning for body composition assessment: A 4-component model comparison of four commercially available scanners. Clin. Nutr. 2020, 39, 3160–3167. [Google Scholar] [CrossRef]
- Tinsley, G.M.; Moore, M.L.; Dellinger, J.R.; Adamson, B.T.; Benavides, M.L. Digital anthropometry via three-dimensional optical scanning: Evaluation of four commercially available systems. Eur. J. Clin. Nutr. 2020, 74, 1054–1064. [Google Scholar] [CrossRef]
- Dechenaud, M.E.; Kennedy, S.; Sobhiyeh, S.; Shepherd, J.; Heymsfield, S.B. Total body and regional surface area: Quantification with low-cost three-dimensional optical imaging systems. Am. J. Phys. Anthropol. 2021, 175, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Sobhiyeh, S.; Dunkel, A.; Dechenaud, M.; Mehrnezhad, A.; Kennedy, S.; Shepherd, J.; Wolenski, P.; Heymsfield, S.B. Digital anthropometric volumes: Toward the development and validation of a universal software. Med. Phys. 2021, 48, 3654–3664. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Bosy-Westphal, A.; Braun, W.; Wong, M.C.; Shepherd, J.A.; Heymsfield, S.B. What Is a 2021 Reference Body? Nutrients 2022, 14, 1526. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.; McCarthy, C.; Fearnbach, N.; Yang, S.; Shepherd, J.A.; Heymsfield, S.B. Emergence of the obesity epidemic: 6-decade visualization with humanoid avatars. Am. J. Clin. Nutr. 2022, 115, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Elobeid, M.A.; Desmond, R.A.; Thomas, O.; Keith, S.W.; Allison, D.B. Waist circumference values are increasing beyond those expected from BMI increases. Obesity 2007, 15, 2380–2383. [Google Scholar] [CrossRef]
- Ford, E.S.; Maynard, L.M.; Li, C. Trends in mean waist circumference and abdominal obesity among US adults, 1999–2012. JAMA 2014, 312, 1151–1153. [Google Scholar] [CrossRef]
- Palli, D.; Berrino, F.; Vineis, P.; Tumino, R.; Panico, S.; Masala, G.; Saieva, C.; Salvini, S.; Ceroti, M.; Pala, V.; et al. A molecular epidemiology project on diet and cancer: The EPIC-Italy Prospective Study. Design and baseline characteristics of participants. Tumori 2003, 89, 586–593. [Google Scholar] [CrossRef]
- García-Alvarez, A.; Serra-Majem, L.; Ribas-Barba, L.; Castell, C.; Foz, M.; Uauy, R.; Plasencia, A.; Salleras, L. Obesity and overweight trends in Catalonia, Spain (1992–2003): Gender and socio-economic determinants. Public Health Nutr. 2007, 10, 1368–1378. [Google Scholar] [CrossRef]
- Goldberg, M.; Leclerc, A.; Bonenfant, S.; Chastang, J.F.; Schmaus, A.; Kaniewski, N.; Zins, M. Cohort profile: The GAZEL Cohort Study. Int. J. Epidemiol. 2007, 36, 32–39. [Google Scholar] [CrossRef]
- Howel, D. Trends in the prevalence of abdominal obesity and overweight in English adults (1993–2008). Obesity 2012, 20, 1750–1752. [Google Scholar] [CrossRef][Green Version]
- Kinge, J.M. Waist circumference, body mass index, and employment outcomes. Eur. J. Health Econ. 2017, 18, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Midthjell, K.; Lee, C.M.; Langhammer, A.; Krokstad, S.; Holmen, T.L.; Hveem, K.; Colagiuri, S.; Holmen, J. Trends in overweight and obesity over 22 years in a large adult population: The HUNT Study, Norway. Clin. Obes. 2013, 3, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Agnoli, C.; Sieri, S.; Ricceri, F.; Macciotta, A.; Masala, G.; Bendinelli, B.; Panico, S.; Mattiello, A.; Tumino, R.; Frasca, G.; et al. Macronutrient composition of the diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 67–75. [Google Scholar] [CrossRef]
- National Health System. Health Survey for England. UK Data Archive, University of Essex, UK. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england (accessed on 1 February 2022).
- Shepherd, J.A. Optical Body Composition and Health Assessment (Shape Up! Adults) Study. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03637855 (accessed on 21 April 2022).
- Ng, B.K.; Sommer, M.J.; Wong, M.C.; Pagano, I.; Nie, Y.; Fan, B.; Kennedy, S.; Bourgeois, B.; Kelly, N.; Liu, Y.E.; et al. Detailed 3-dimensional body shape features predict body composition, blood metabolites, and functional strength: The Shape Up! studies. Am. J. Clin. Nutr. 2019, 110, 1316–1326. [Google Scholar] [CrossRef] [PubMed]
- Panizza, C.E.; Wong, M.C.; Kelly, N.; Liu, Y.E.; Shvetsov, Y.B.; Lowe, D.A.; Weiss, E.J.; Heymsfield, S.B.; Kennedy, S.; Boushey, C.J.; et al. Diet Quality and Visceral Adiposity among a Multiethnic Population of Young, Middle, and Older Aged Adults. Curr. Dev. Nutr. 2020, 4, nzaa090. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.K. Three-dimensional optical scanning for clinical body shape assessment comes of age. Am. J. Clin. Nutr. 2019, 110, 1272–1274. [Google Scholar] [CrossRef] [PubMed]

| Prediction Equations | References |
|---|---|
| WC (female) = 28.81919 + (2.218007 × BMI) + (−3.688953 × AGE CLASS) + (0.125975 × AGE × AGE CLASS) + (−0.6570163 × BLACK) + (0.1818819 × HISPANIC) WC (male) = 22.61306 + (2.520738 × BMI) + (0.1583812 × AGE) + (−3.703501 × BLACK) + (−1.736731 × HISPANIC) | [9] |
| Lean mass (female) = −10.683 + (−0.039 × AGE) + (0.186 × HEIGHT) + (0.383 × WEIGHT) + (−0.043 × WC) Lean mass (male) = 19.363 + (0.001 × AGE) + (0.064 × HEIGHT) + (0.756 × WEIGHT) + (−0.366 × WC) | [10] |
| Fat mass (female) = 11.817 + (0.041 × AGE) + (−0.199 × HEIGHT) + (0.610 × WEIGHT) + (0.044 × WC) Fat mass (male) = −18.592 + (−0.009 × AGE) + (−0.080 × HEIGHT) + (0.226 × WEIGHT) + (0.387 × WC) | [10] |
| Relative fat mass (female) = 64 − [20 × (HEIGHT/WC)] + 12 Relative fat mass (male) = 64 − [20 × (HEIGHT/WC)] | [11] |
| SM (female) = 2.89 + (0.255 × WEIGHT) + (−0.175 × HC) + (−0.0384 × AGE) + (0.118 × HEIGHT) SM (male) = 39.5 + (0.665 × WEIGHT) + (−0.185 × WC) + (−0.418 × HC) + (−0.0805 × AGE) | [12] |
| SM (female) = (0.25 × WEIGHT) + (0.09 × HEIGHT) + (−0.111 × AGE) + (0.0005 × AGE2) + (−0.06 × WC) + (2.0 × RACE) − 4.5 SM (male) = (0.47 × WEIGHT) + (0.03 × HEIGHT) + (0.012 × AGE) + (−0.001 × AGE2) + (−0.29 × WC) + (1.6 × RACE) + 13.5 | [13] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minetto, M.A.; Pietrobelli, A.; Busso, C.; Bennett, J.P.; Ferraris, A.; Shepherd, J.A.; Heymsfield, S.B. Digital Anthropometry for Body Circumference Measurements: European Phenotypic Variations throughout the Decades. J. Pers. Med. 2022, 12, 906. https://doi.org/10.3390/jpm12060906
Minetto MA, Pietrobelli A, Busso C, Bennett JP, Ferraris A, Shepherd JA, Heymsfield SB. Digital Anthropometry for Body Circumference Measurements: European Phenotypic Variations throughout the Decades. Journal of Personalized Medicine. 2022; 12(6):906. https://doi.org/10.3390/jpm12060906
Chicago/Turabian StyleMinetto, Marco Alessandro, Angelo Pietrobelli, Chiara Busso, Jonathan P. Bennett, Andrea Ferraris, John A. Shepherd, and Steven B. Heymsfield. 2022. "Digital Anthropometry for Body Circumference Measurements: European Phenotypic Variations throughout the Decades" Journal of Personalized Medicine 12, no. 6: 906. https://doi.org/10.3390/jpm12060906
APA StyleMinetto, M. A., Pietrobelli, A., Busso, C., Bennett, J. P., Ferraris, A., Shepherd, J. A., & Heymsfield, S. B. (2022). Digital Anthropometry for Body Circumference Measurements: European Phenotypic Variations throughout the Decades. Journal of Personalized Medicine, 12(6), 906. https://doi.org/10.3390/jpm12060906







