In Vivo Accuracy of a New Digital Planning System in Terms of Jaw Relation, Extent of Surgical Movements and the Hierarchy of Stability in Orthognathic Surgery
Abstract
:1. Introduction
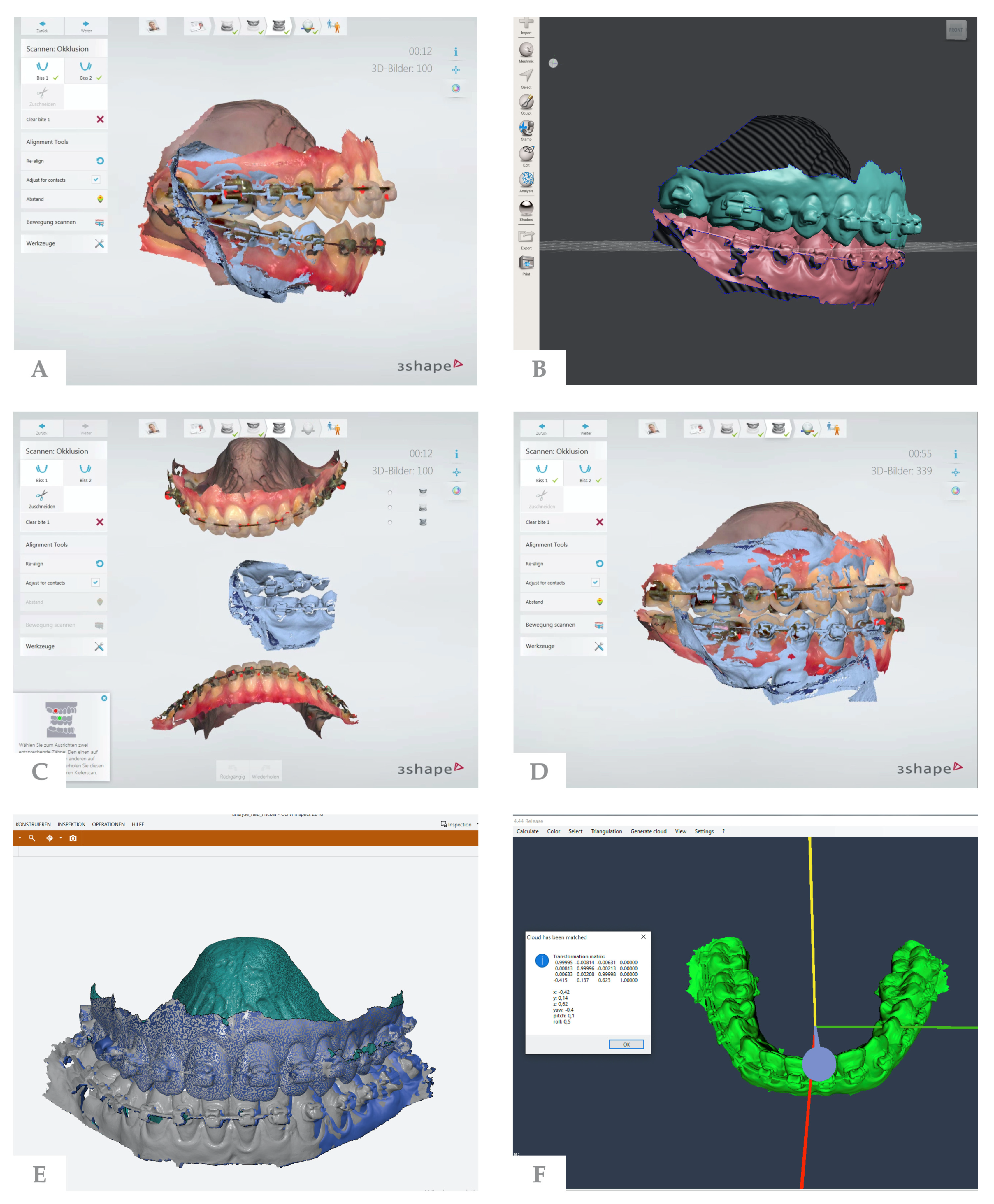
2. Materials and Methods
2.1. Measurement Process
2.2. Statistical Analysis
3. Results
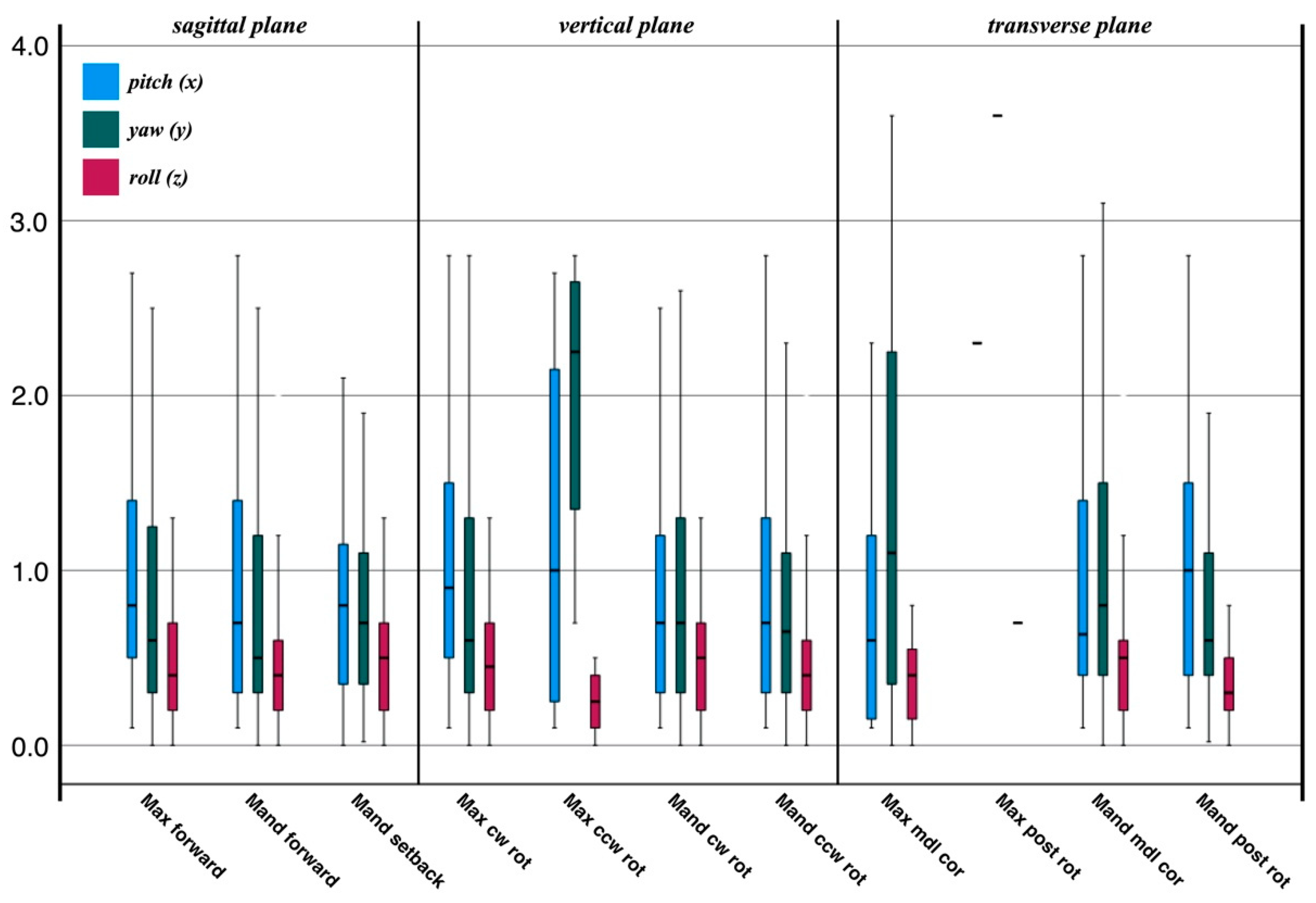
3.1. Conformity between Planned and Postoperative Positions
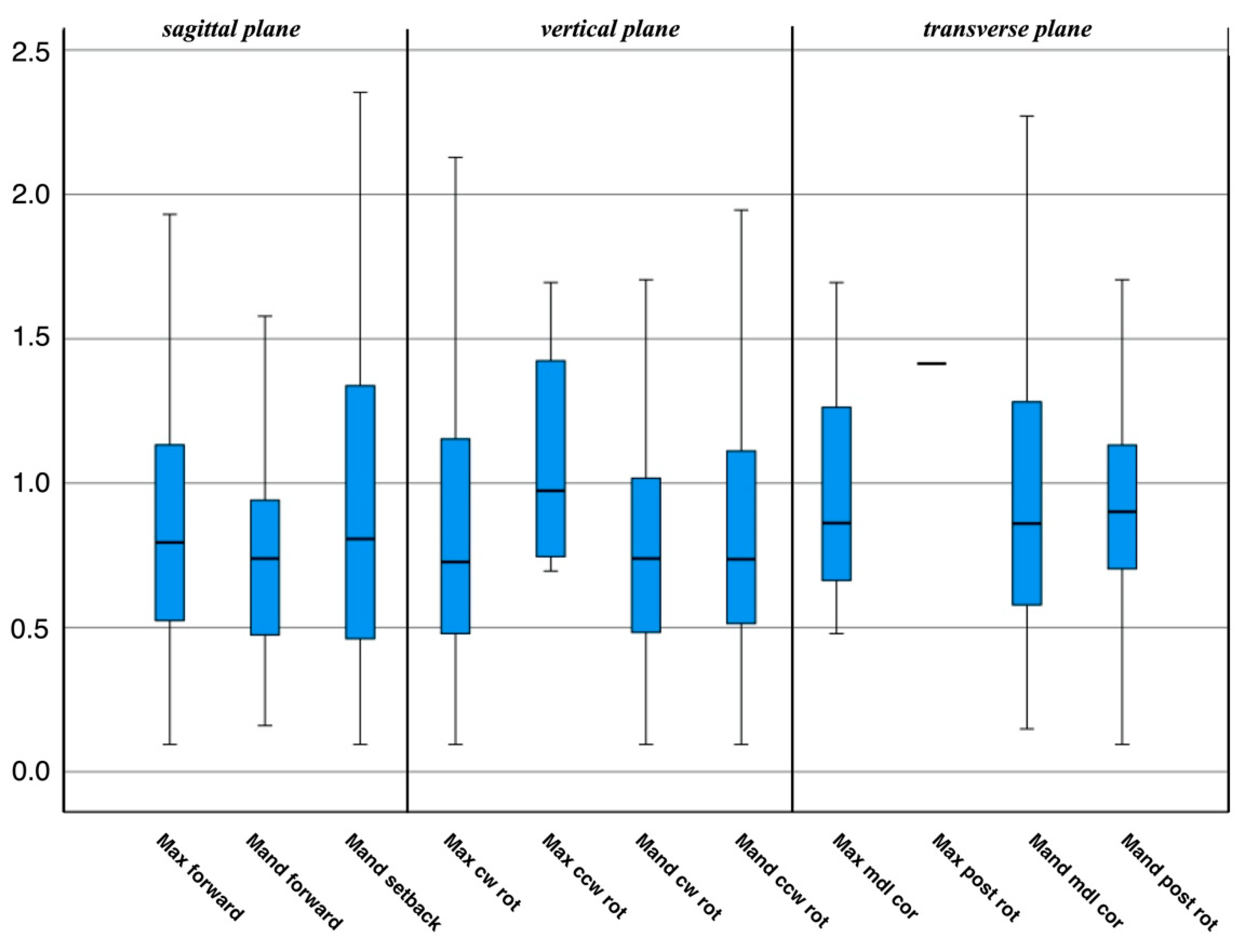
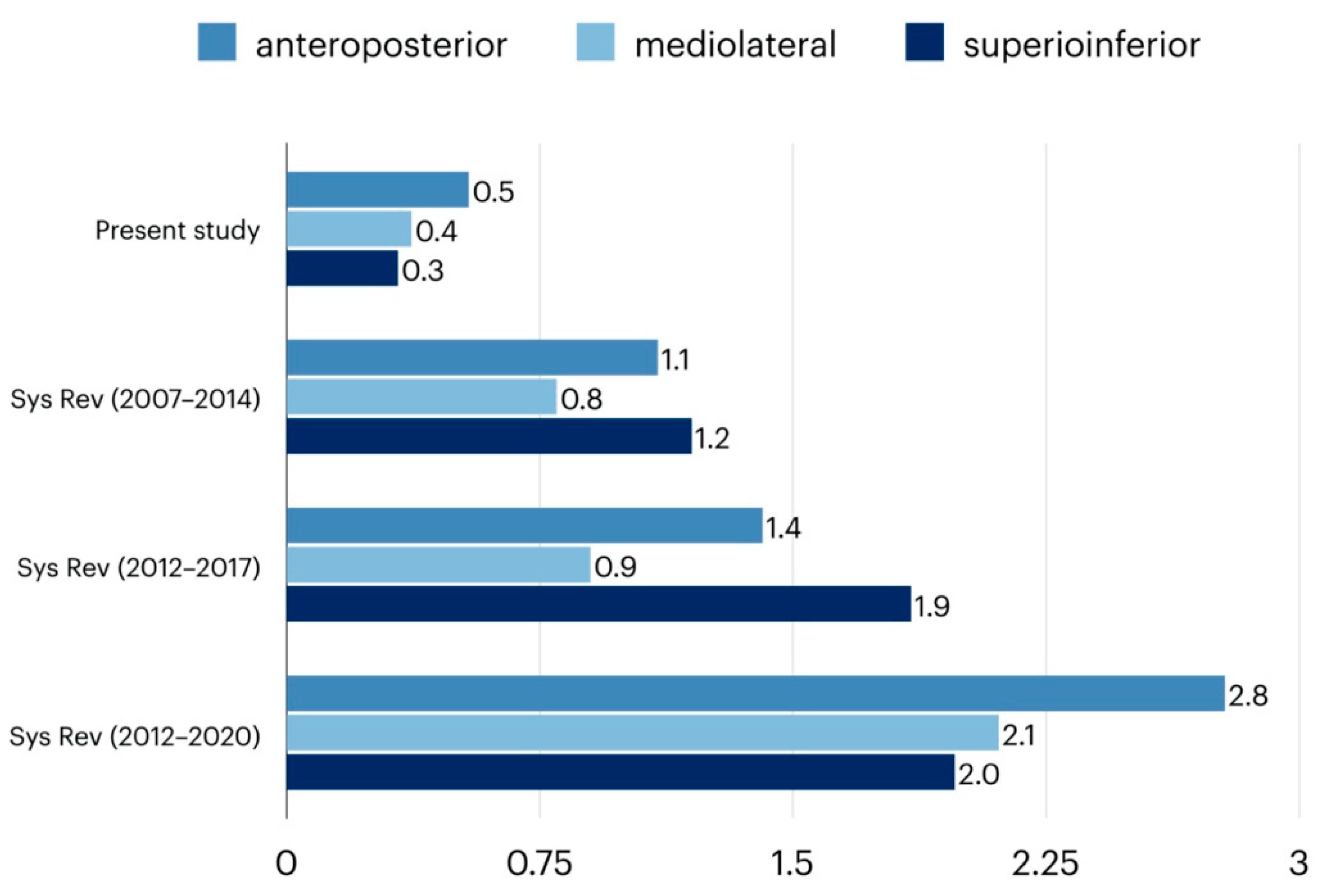
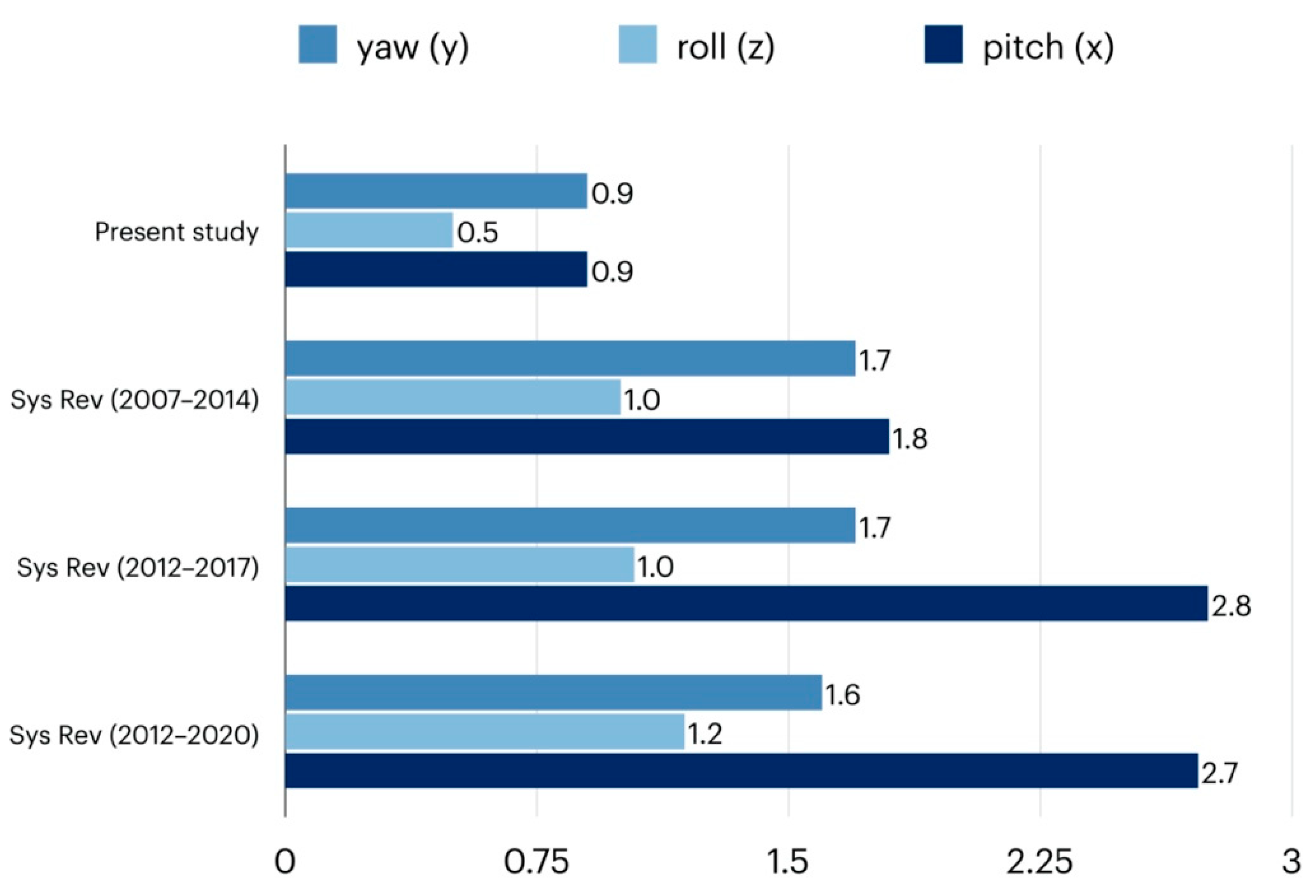
3.2. Magnitude of Surgical Movement and Error Size
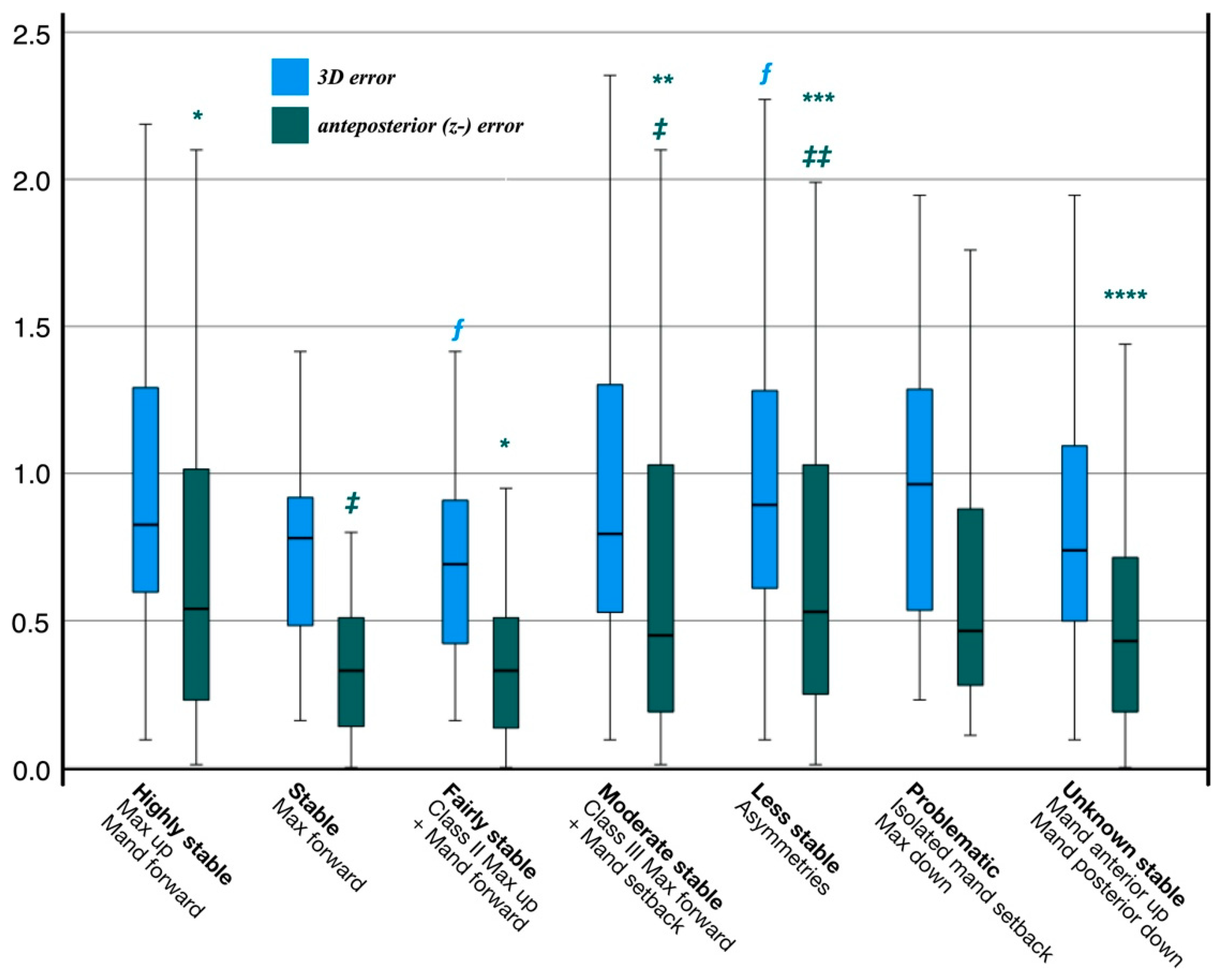
3.3. Categories of Postoperative Stability and Error Size
4. Discussion
Strength and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Paul, N.R.; Baker, S.R.; Gibson, B.J. Decision Making from the Experience of Orthognathic Surgery Patients: A Grounded Theory Approach [published online ahead of print, 2021 May 24]. JDR Clin. Transl. Res. 2021, 23800844211014440. [Google Scholar] [CrossRef]
- Ehmer, U.; Austermann, K.H. Die Rolle des Kieferorthopäden für die Motivation zu chirurgisch-kieferorthopädischen Therapiemaßnahmen. Fortschr. Kieferorthopädie 1987, 48, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Gaber, R.M.; Shaheen, E.; Falter, B.; Araya, S.; Politis, C.; Swennen, G.R.; Jacobs, R. A Systematic Review to Uncover a Universal Protocol for Accuracy Assessment of 3-Dimensional Virtually Planned Orthognathic Surgery. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2017, 75, 2430–2440. [Google Scholar] [CrossRef] [PubMed]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. Orthognathic surgery: A hierarchy of stability. Int. J. Adult Orthod. Orthognath. Surg. 1996, 11, 191–204. [Google Scholar]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: An update and extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef] [Green Version]
- Hernández-Alfaro, F.; Guijarro-Martínez, R. New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study. Int. J. Oral Maxillofac. Surg. 2013, 42, 1547–1556. [Google Scholar] [CrossRef]
- Hsu, S.S.P.; Gateno, J.; Bell, R.B.; Hirsch, D.L.; Markiewicz, M.R.; Teichgraeber, J.F.; Zhou, X.; Xia, J.J. Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: A prospective multicenter study. J. Oral Maxillofac. Surg. 2013, 71, 128–142. [Google Scholar] [CrossRef] [Green Version]
- Marlìere, D.A.A.; Demétrio, M.S.; Schmitt, A.R.M.; Lovisi, C.B.; Asprino, L.; Chaves-Netto, H.D.D.M. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm and color maps: A retrospective cohort study. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e243–e253. [Google Scholar] [CrossRef]
- Ackerman, J.L.; Proffit, W.R.; Sarver, D.M.; Ackerman, M.B.; Kean, M.R. Pitch, roll, and yaw: Describing the spatial orientation of dentofacial traits. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 305–310. [Google Scholar] [CrossRef]
- Dorafshar, A.H.; Brazio, P.S.; Mundinger, G.S.; Mohan, R.; Brown, E.N.; Rodriguez, E.D. Found in space: Computer-assisted orthognathic alignment of a total face allograft in six degrees of freedom. J. Oral Maxillofac. Surg. 2014, 72, 1788–1800. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, K.J.; Yu, H.S.; Jung, Y.S.; Baik, H.S. Three-dimensional effect of pitch, roll, and yaw rotations on maxillomandibular complex movement. J. Cranio-Maxillofac. Surg. 2015, 43, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Schouman, T.; Rouch, P.; Imholz, B.; Fasel, J.; Courvoisier, D.; Scolozzi, P. Accuracy evaluation of CAD/CAM generated splints in orthognathic surgery: A cadaveric study. Head Face Med. 2015, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Liczmanski, K.; Stamm, T.; Sauerland, C.; Blanck-Lubarsch, M. Accuracy of intraoral scans in the mixed dentition: A prospective non-randomized comparative clinical trial. Head Face Med. 2020, 16, 11. [Google Scholar] [CrossRef]
- Xia, J.J.; Gateno, J.; Teichgraeber, J.F.; Christensen, A.M.; Lasky, R.E.; Lemoine, J.J.; Liebschner, M.A. Accuracy of the Computer-Aided Surgical Simulation (CASS) System in the Treatment of Patients With Complex Craniomaxillofacial Deformity: A Pilot Study. J. Oral Maxillofac. Surg. 2007, 65, 248–254. [Google Scholar] [CrossRef]
- Stamm, T.; Böttcher, D.; Kleinheinz, J. The University Münster model surgery system for orthognathic surgery—The digital update. Head Face Med. 2021, 17, 31. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Dawson, P.E. Centric relation. Its effect on occluso-muscle harmony. Dent. Clin. N. Am. 1979, 23, 169–180. [Google Scholar] [CrossRef]
- Haas, O.L.; Becker, O.E.; De Oliveira, R.B. Computer-aided planning in orthognathic surgery—Systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 329–342. [Google Scholar] [CrossRef]
- Shirota, T.; Shiogama, S.; Asama, Y.; Tanaka, M.; Kurihara, Y.; Ogura, H.; Kamatani, T. CAD/CAM splint and surgical navigation allows accurate maxillary segment positioning in Le Fort I osteotomy. Heliyon 2019, 5, e02123. [Google Scholar] [CrossRef] [Green Version]
- Lin, X.; Sun, Y.; Han, X.; Wang, J.; Zhang, M.; Liang, L. Computer-Aided Freehand Maxillary Repositioning. J. Craniofacial Surg. 2018, 29, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Berssenbrügge, P.; Lingemann-Koch, M.; Abeler, A.; Runte, C.; Jung, S.; Kleinheinz, J.; Denz, C.; Dirksen, D. Measuring facial symmetry: A perception-based approach using 3D shape and color. Biomed. Tech. Biomed. Eng. 2015, 60, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Besl, P.J.; McKay, N.D. A method for registration of 3-D shapes. IEEE Trans. Pattern Anal. Mach. Intell. 1992, 14, 239–256. [Google Scholar] [CrossRef]
- Alanko, O.M.E.; Svedstrm-Oristo, A.L.; Tuomisto, M.T. Patients’ perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: A systematic review. Acta Odontol. Scand. 2010, 68, 249–260. [Google Scholar] [CrossRef]
- Proothi, M.; Drew, S.J.; Sachs, S.A. Motivating factors for patients undergoing orthognathic surgery evaluation. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2010, 68, 1555–1559. [Google Scholar] [CrossRef]
- Torgersbråten, N.; Stenvik, A.; Espeland, L. Patient satisfaction after orthognathic surgery: A 3 year follow-up of 60 high-angle Class II individuals. Eur. J. Orthod. 2021, 43, 215–221. [Google Scholar] [CrossRef]
- Mendes de Paula Gomes, A.; Adas Saliba Garbin, C.; da Silva Ferraz, F.W.; Adas Saliba, T.; Isper Garbin, A.J. Dentofacial Deformities and Implications on Quality of Life: A Presurgical Multifactorial Analysis in Patients Seeking Orthognathic Surgical Treatment. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2019, 77, 409.e1–409.e9. [Google Scholar] [CrossRef]
- Zinser, M.J.; Sailer, H.F.; Ritter, L.; Braumann, B.; Maegele, M.; Zöller, J.E. A paradigm shift in orthognathic surgery? A comparison of navigation, computer-aided designed/computer-aided manufactured splints, and “classic” intermaxillary splints to surgical transfer of virtual orthognathic planning. J. Oral Maxillofac. Surg. 2013, 71, 2151.e1–2151.e21. [Google Scholar] [CrossRef]
- Badiali, G.; Bevini, M.; Ruggiero, F.; Cercenelli, L.; Lovero, E.; De Simone, E.; Rucci, P.; Bianchi, A.; Marchetti, C. Validation of a patient-specific system for mandible-first bimaxillary surgery: Ramus and implant positioning precision assessment and guide design comparison. Sci. Rep. 2020, 10, 13317. [Google Scholar] [CrossRef]
- Wong, A.; Goonewardene, M.S.; Allan, B.P.; Mian, A.S.; Rea, A. Accuracy of maxillary repositioning surgery using CAD/CAM customized surgical guides and fixation plates. Int. J. Oral Maxillofac. Surg. 2021, 50, 494–500. [Google Scholar] [CrossRef]
- Almukhtar, A.; Ju, X.; Khambay, B.; McDonald, J.; Ayoub, A. Comparison of the accuracy of voxel based registration and surface based registration for 3D assessment of surgical change following orthognathic surgery. PLoS ONE 2014, 9, e93402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baan, F.; Liebregts, J.; Xi, T.; Schreurs, R.; De Koning, M.; Bergé, S.; Maal, T. A new 3D tool for assessing the accuracy of bimaxillary surgery: The OrthoGnathicanAlyser. PLoS ONE 2016, 11, e0149625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stafeev, A.; Ryakhovsky, A.; Petrov, P.; Chikunov, S.; Khizhuk, A.; Bykova, M.; Vuraki, N. Comparative analysis of the reproduction accuracy of main methods for finding the mandible position in the centric relation using digital research method. Comparison between analog-to-digital and digital methods: A preliminary report. Int. J. Environ. Res. Public Health 2020, 17, 933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tondin, G.M.; Leal, M.D.O.C.D.; Costa, S.T.; Grillo, R.; Jodas, C.R.P.; Teixeira, R.G. Evaluation of the accuracy of virtual planning in bimaxillary orthognathic surgery: Systematic review. Br. J. Oral Maxillofac. Surg. 2021. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0266435621003430 (accessed on 5 May 2022).
- Baan, F.; Sabelis, J.F.; Schreurs, R.; van de Steeg, G.; Xi, T.; van Riet, T.C.; Becking, A.G.; Maal, T.J.J. Validation of the OrthoGnathicAnalyser 2.0—3D accuracy assessment tool for bimaxillary surgery and genioplasty. PLoS ONE. 2021, 16, p. e0246196. [CrossRef]
- Holte, M.B.; Diaconu, A.; Ingerslev, J.; Thorn, J.J.; Pinholt, E.M. Virtual analysis of segmental bimaxillary surgery: A validation study. J. Oral Maxillofac. Surg. 2021, 79, 2320–2333. [Google Scholar] [CrossRef]
- Holte, M.B.; Diaconu, A.; Ingerslev, J.; Thorn, J.J.; Pinholt, E.M. Virtual surgical analysis: Long-term cone beam computed tomography stability assessment of segmental bimaxillary surgery. Int. J. Oral Maxillofac. Surg. 2022, 26, 2320–2333. [Google Scholar] [CrossRef]
- Andriola, F.O.; Haas Junior, O.L.; Guijarro-Martínez, R.; Hernández-Alfaro, F.; Oliveira, R.B.; Pagnoncelli, R.M.; Swennen, G.R. Computed tomography imaging superimposition protocols to assess outcomes in orthognathic surgery: A systematic review with comprehensive recommendations. Dentomaxillofac. Radiol. 2022, 51, 20210340. [Google Scholar] [CrossRef]
| Gender | n | Age Years | Class II | Class III | Open Bite * |
|---|---|---|---|---|---|
| Female | 90 | 28.7 ± 8.7 | 58 (p ≤ 0.05) ** | 32 | 21 |
| Male | 61 | 27.7 ± 6.1 | 25 (p = N.) | 36 | 24 |
| Plane/Procedure | Single- | Two- | Range | 3D Error | R | RMS | |x| | |y| | |z| | Pitch (x) | Yaw (y) | Roll (z) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jaw | Jaws | (mm) | (mm) | (mm) | (mm) | (mm) | (mm) | (°) | (°) | (°) | ||
| Sagittal plane | ||||||||||||
| Max forward | 1 | 82 | 4 (1–5) | 0.9 ± 0.5 | 0.423, p < 0.001 | 1.0 | 0.4 ± 0.3 | 0.3 ± 0.3 | 0.6 ± 0.6 | 1.0 ± 0.8 | 0.9 ± 0.9 | 0.5 ± 0.5 |
| Mand forward | 56 | 37 | 10 (1–11) | 0.8 ± 0.4 | −0.096, p = N. | 0.9 | 0.4 ± 0.3 | 0.4 ± 0.3 | 0.5 ± 0.4 | 0.9 ± 0.8 | 0.9 ± 0.8 | 0.5 ± 0.5 |
| Mand setback | 8 | 43 | 8 (1–9) | 1.0 ± 0.6 | −0.242, p = N. | 1.1 | 0.4 ± 0.3 | 0.3 ± 0.3 | 0.7 ± 0.7 | 0.8 ± 0.6 | 0.8 ± 0.8 | 0.6 ± 0.5 |
| Vertical plane 1 | ||||||||||||
| Max cw rotation 2 | 1 | 69 | 5 (1–6) | 0.9 ± 0.6 | −0.085, p = N. | 1.0 | 0.4 ± 0.3 | 0.4 ± 0.3 | 0.5 ± 0.6 | 1.0 ± 0.8 | 1.0 ± 0.9 | 0.5 ± 0.4 |
| Max ccw rotation | 0 | 4 | 3 (1–4) | 1.1 ± 0.5 | 0.080, p = N. | 1.2 | 0.7 ± 0.3 | 0.3 ± 0.1 | 0.7 ± 0.5 | 1.2 ± 1.2 | 2.0 ± 0.9 | 0.3 ± 0.2 |
| Mand cw rotation | 29 | 52 | 5 (1–6) | 0.9 ± 0.5 | 0.094, p = N. | 1.0 | 0.4 ± 0.3 | 0.4 ± 0.3 | 0.5 ± 0.5 | 0.9 ± 0.7 | 0.9 ± 0.8 | 0.6 ± 0.5 |
| Mand ccw rotation | 42 | 52 | 7 (1–8) | 0.9 ± 0.5 | 0.138, p = N. | 1.0 | 0.4 ± 0.3 | 0.3 ± 0.2 | 0.6 ± 0.5 | 0.9 ± 0.7 | 0.8 ± 0.7 | 0.5 ± 0.4 |
| Horizontal plane 1 | ||||||||||||
| Max midline correction | 1 | 6 | 5 (1–6) | 1.0 ± 0.5 | 0.685, p = N. | 1.1 | 0.5 ± 0.4 | 0.3 ± 0.2 | 0.6 ± 0.5 | 0.8 ± 0.8 | 1.4 ± 1.3 | 0.4 ± 0.3 |
| Max post-rotation | 0 | 1 | 0 (2–2) | 1.4 | − | 1.4 | 1.2 | 0.4 | 0.7 | 2.3 | 3.6 | 0.7 |
| Mand midline correction | 21 | 37 | 7 (1–8) | 1.0 ± 0.6 | 0.108, p = N. | 1.1 | 0.4 ± 0.3 | 0.3 ± 0.3 | 0.7 ± 0.6 | 0.9 ± 0.7 | 1.0 ± 0.8 | 0.6 ± 0.6 |
| Mand post-rotation | 6 | 19 | 3 (1-4) | 1.0 ± 0.5 | −0.075, p = N. | 1.1 | 0.4 ± 0.4 | 0.3 + 0.3 | 0.7 ± 0.5 | 1.0 ± 0.8 | 0.7 ± 0.5 | 0.4 ± 0.4 |
| Stability | Procedures | |z| (mm) | p |
|---|---|---|---|
| Highly stable | Maxilla up 1 | 0.7 ± 0.6 | * |
| Mandible forward | |||
| Stable | Maxilla forward | 0.4 ± 0.4 | ‡ (p ≤ 0.05) ‡‡ (p ≤ 0.05) |
| Fairly stable 2 | Class II (maxilla up + mandible forward) | 0.4 ± 0.4 | * (p ≤ 0.05) ** (p < 0.001) *** (p ≤ 0.05) **** (p ≤ 0.05) |
| Moderate stable 2 | Class III (maxilla forward + mandibular setback) | 0.7 ± 0.7 | ‡ ** |
| Less stable 2 | Asymmetries | 0.7 ± 0.6 | ‡‡ *** |
| Problematic | Isolated mandibular setback | 0.6 ± 0.5 | |
| maxilla down 3 | |||
| Unknown stable 4 | Mandibula anterior up | 0.6 ± 0.5 | **** |
| Mandibula posterior down |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stamm, T.; Andriyuk, E.; Kleinheinz, J.; Jung, S.; Dirksen, D.; Middelberg, C. In Vivo Accuracy of a New Digital Planning System in Terms of Jaw Relation, Extent of Surgical Movements and the Hierarchy of Stability in Orthognathic Surgery. J. Pers. Med. 2022, 12, 843. https://doi.org/10.3390/jpm12050843
Stamm T, Andriyuk E, Kleinheinz J, Jung S, Dirksen D, Middelberg C. In Vivo Accuracy of a New Digital Planning System in Terms of Jaw Relation, Extent of Surgical Movements and the Hierarchy of Stability in Orthognathic Surgery. Journal of Personalized Medicine. 2022; 12(5):843. https://doi.org/10.3390/jpm12050843
Chicago/Turabian StyleStamm, Thomas, Eugenia Andriyuk, Johannes Kleinheinz, Susanne Jung, Dieter Dirksen, and Claudius Middelberg. 2022. "In Vivo Accuracy of a New Digital Planning System in Terms of Jaw Relation, Extent of Surgical Movements and the Hierarchy of Stability in Orthognathic Surgery" Journal of Personalized Medicine 12, no. 5: 843. https://doi.org/10.3390/jpm12050843
APA StyleStamm, T., Andriyuk, E., Kleinheinz, J., Jung, S., Dirksen, D., & Middelberg, C. (2022). In Vivo Accuracy of a New Digital Planning System in Terms of Jaw Relation, Extent of Surgical Movements and the Hierarchy of Stability in Orthognathic Surgery. Journal of Personalized Medicine, 12(5), 843. https://doi.org/10.3390/jpm12050843







