Public Perspectives on Exposure Notification Apps: A Patient and Citizen Co-Designed Study
Abstract
:1. Introduction
1.1. Background
1.2. Objectives of This Study
2. Materials and Methods
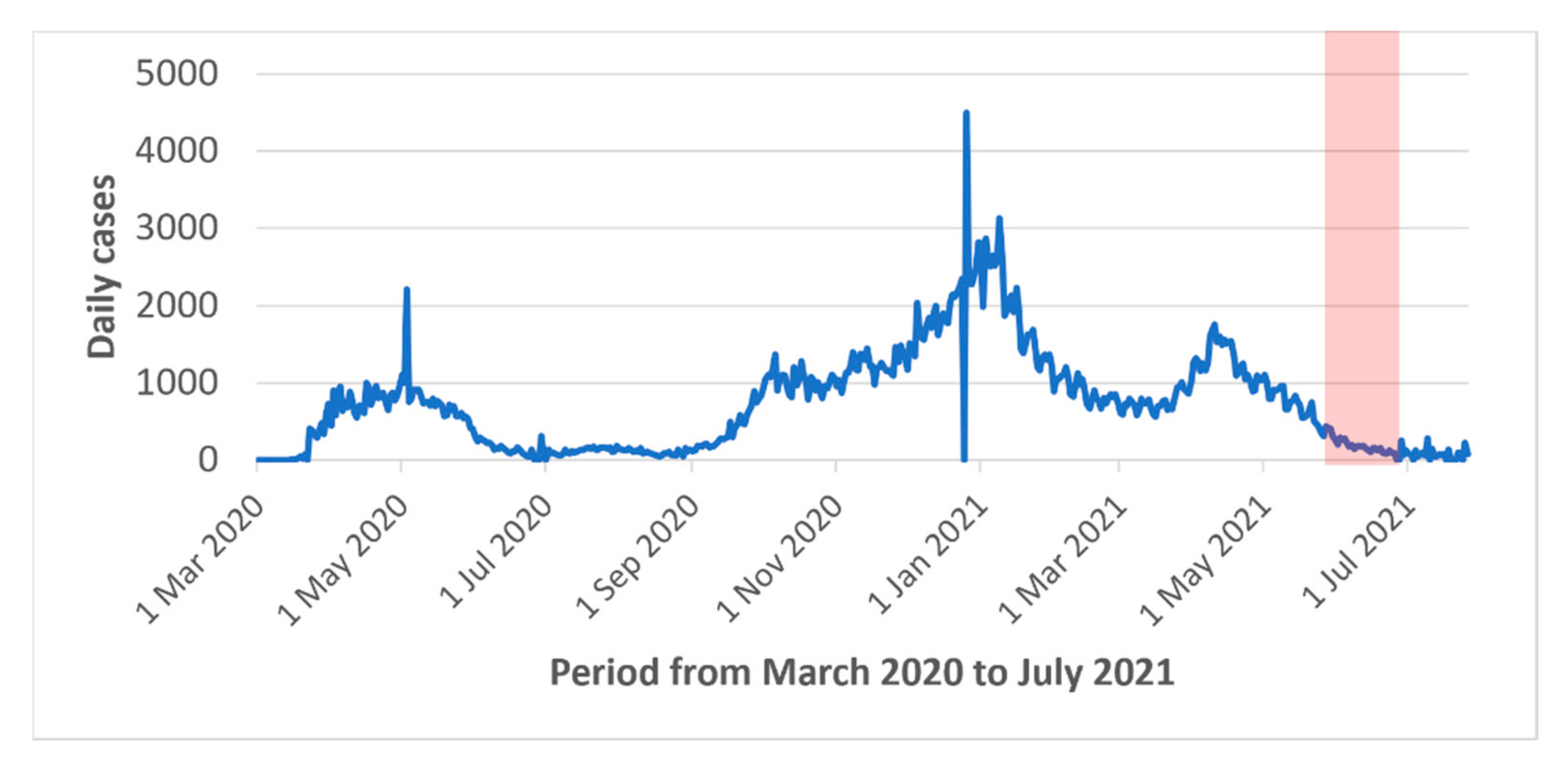
2.1. The COVID Alert App
2.2. Co-Construction of the Questionnaire
2.3. Survey Administration
2.4. Statistical Correction and Analysis
3. Results
3.1. Respondent Characteristics
3.2. App Adoption and User Characteristics
3.3. User Concerns
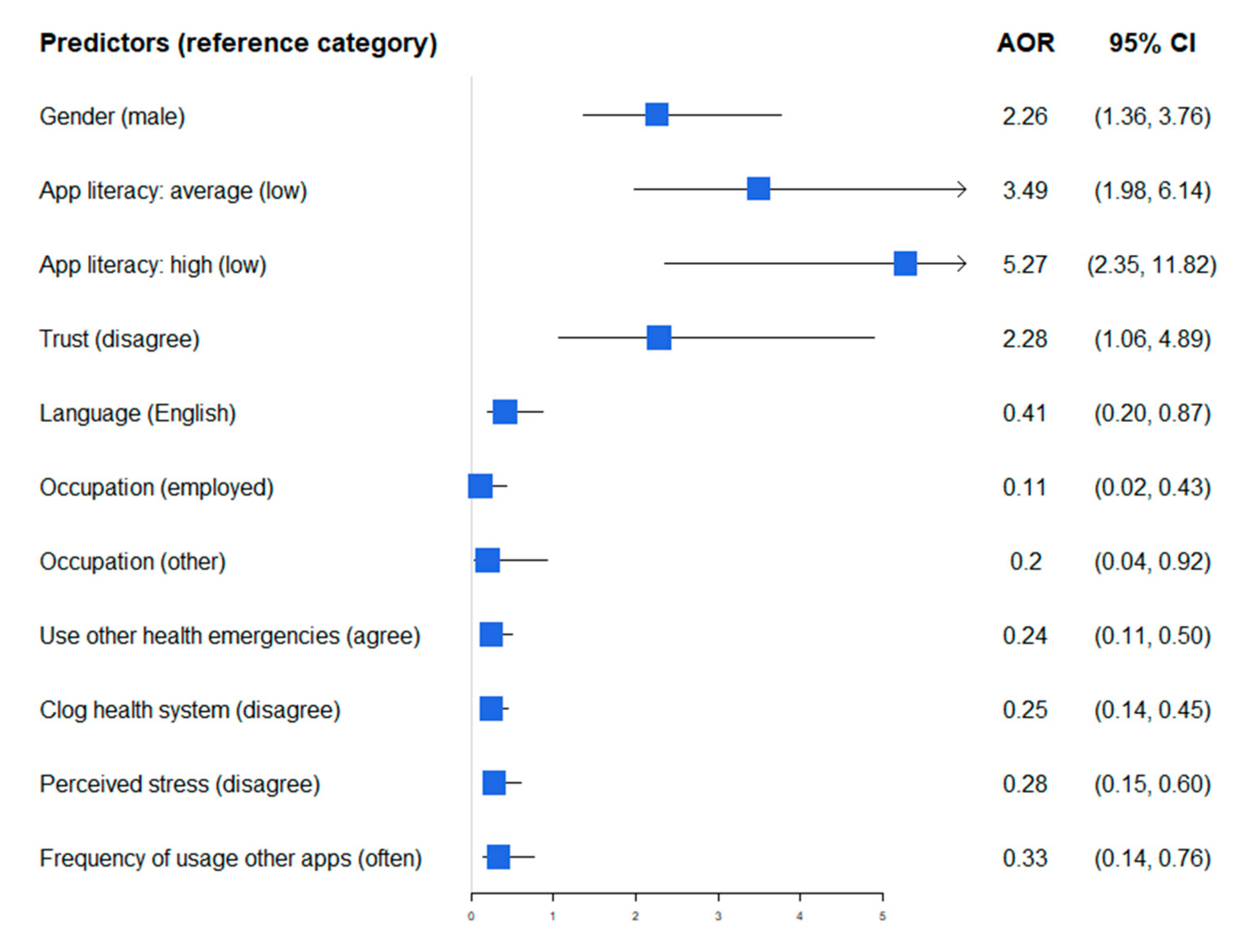
3.4. Predictors of App Download
3.5. Characteristics Associated with User Perceptions and Knowledge of the App
3.6. User Recommendations for App Improvement and the Role of Citizen Engagement
4. Discussion
4.1. Recommendations for Improved Social Aacceptability and Adoption
4.1.1. Communication
4.1.2. Design
4.1.3. Access to Technology
4.1.4. Partnership with the Public
4.2. Study Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferretti, L.; Wymant, C.; Kendall, M.; Zhao, L.; Nurtay, A.; Abeler-Dörner, L.; Parker, M.; Bonsall, D.G.; Fraser, C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science 2020, 368, eabb6936. [Google Scholar] [CrossRef] [Green Version]
- Exposure Notifications: Using Technology to Help Public Health Authorities Fight COVID-19. Available online: https://www.google.com/intl/en_us/covid19/exposurenotifications/ (accessed on 23 February 2022).
- Government of Canada. Download COVID Alert Today. 15 September 2020. Available online: https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/covid-alert.html (accessed on 23 February 2022).
- Altmann, S.; Milsom, L.; Zillessen, H.; Blasone, R.; Gerdon, F.; Bach, R.; Kreuter, F.; Nosenzo, D.; Toussaert, S.; Abeler, J. Acceptability of app-based contact tracing for COVID-19: Cross-country survey study. JMIR mHealth uHealth 2020, 8, e19857. [Google Scholar] [CrossRef]
- Bachtiger, P.; Adamson, A.; Quint, J.K.; Peters, N.S. Belief of having had unconfirmed Covid-19 infection reduces willingness to participate in app-based contact tracing. NPJ Digit. Med. 2020, 3, 146. [Google Scholar] [CrossRef]
- Jansen-Kosterink, S.M.; Hurmuz, M.; Den Ouden, M.; Van Velsen, L. Predictors to use mobile apps for monitoring COVID-19 symptoms and contact tracing: A survey among Dutch citizens. JMIR Form Res. 2021, 5, e28416. [Google Scholar] [CrossRef]
- Jonker, M.; De Bekker-Grob, E.; Veldwijk, J.; Goossens, L.; Bour, S.; Rutten-Van Mölken, M. COVID-19 contact tracing apps: Predicted uptake in the Netherlands based on a discrete choice experiment. JMIR mHealth uHealth 2020, 8, e20741. [Google Scholar] [CrossRef]
- Kaspar, K. Motivations for social distancing and app use as complementary measures to combat the COVID-19 pandemic: Quantitative survey study. J. Med. Internet Res. 2020, 22, e21613. [Google Scholar] [CrossRef]
- O’Callaghan, M.E.; Buckley, J.; Fitzgerald, B.; Johnson, K.; Laffey, J.; McNicholas, B.; Nuseibeh, B.; O’Keeffe, D.; O’Keeffe, I.; Razzaq, A.; et al. A national survey of attitudes to COVID-19 digital contact tracing in the Republic of Ireland. Ir. J. Med. Sci. 2021, 190, 863–887. [Google Scholar] [CrossRef]
- Thomas, R.; Michaleff, Z.A.; Greenwood, H.; Abukmail, E.; Glasziou, P. Concerns and Misconceptions About the Australian Government’s COVIDSafe App: Cross-Sectional Survey Study. JMIR Public Health Surveill. 2020, 6, e23081. [Google Scholar] [CrossRef]
- Walrave, M.; Waeterloos, C.; Ponnet, K. Adoption of a Contact Tracing App for Containing COVID-19: A Health Belief Model Approach. JMIR Public Health Surveill. 2020, 6, e20572. [Google Scholar] [CrossRef]
- Kozyreva, A.; Lorenz-Spreen, P.; Lewandowsky, S.; Garrett, P.M.; Herzog, S.M.; Pachur, T.; Hertwig, R. Psychological factors shaping public responses to COVID-19 digital contact tracing technologies in Germany. Sci. Rep. 2021, 11, 1–19. [Google Scholar] [CrossRef]
- Singapore Government Agency. TraceTogether. Available online: https://www.tracetogether.gov.sg/ (accessed on 25 April 2022).
- Ontario Data Catalogue. COVID Alert Downloads—Canada. Available online: https://data.ontario.ca/fr/dataset/covid-alert-impact-data/resource/37cfeca2-059e-4a5f-a228-249f6ab1b771 (accessed on 13 January 2022).
- Sun, M.; Shaw, M.; Moodie, E.E.M.; Ruths, D. The epidemiological impact of the Canadian COVID Alert App. medRxiv 2022. [Google Scholar] [CrossRef]
- Digital Contact Tracing Can Slow or Even Stop Coronavirus Transmission and Ease Us Out of Lockdown. University of Oxford: Our Research. Available online: https://www.research.ox.ac.uk/Article/2020-04-16-digital-contact-tracing-can-slow-or-even-stop-coronavirus-transmission-and-ease-us-out-of-lockdown (accessed on 16 April 2021).
- O’Neill, P.H. No, Coronavirus Apps Don’t Need 60% Adoption to Be Effective. MIT Technology Review. Available online: https://www.technologyreview.com/2020/06/05/1002775/covid-apps-effective-at-less-than-60-percent-download/ (accessed on 16 December 2021).
- Wymant, C.; Ferretti, L.; Tsallis, D.; Charalambides, M.; Abeler-Dörner, L.; Bonsall, D.; Hinch, R.; Kendall, M.; Milsom, L.; Ayres, M.; et al. The epidemiological impact of the NHS COVID-19 app. Nature 2021, 594, 408–412. [Google Scholar] [CrossRef]
- Breton, M.; Hudon, C. La première vague de Covid-19 au Québec et les soins primaires. Rev. Med. Suisse. 2020, 16, 2131–2134. [Google Scholar] [CrossRef]
- Von Wyl, V.; Höglinger, M.; Sieber, C.; Kaufmann, M.; Moser, A.; Serra-Burriel, M.; Ballouz, T.; Menges, D.; Frei, A.; Puhan, M.A. Drivers of Acceptance of COVID-19 Proximity Tracing Apps in Switzerland: Panel Survey Analysis. JMIR Public Health Surveill. 2021, 7, e25701. [Google Scholar] [CrossRef]
- Horstmann, K.T.; Buecker, S.; Krasko, J.; Kritzler, S.; Terwiel, S. Who does or does not use the ‘Corona-Warn-App’ and why? Eur. J. Public Health 2021, 31, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES). Workshop Report on Biodiversity and Pandemics of the Intergovernmental Platform on Biodiversity and Ecosystem Services (IPBES); IPBES Secretariat: Bonn, Germany, 2020. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, J.; O’Keeffe, D.T. Contact Tracing for Covid-19—A Digital Inoculation against Future Pandemics. N. Engl. J. Med. 2021, 385, 484–487. [Google Scholar] [CrossRef]
- Government of Canada. Interim Report on Social and Economic Determinants of App Adoption, Retention and Use. Available online: https://www.ic.gc.ca/eic/site/icgc.nsf/vwapj/07716_en.pdf/$FILE/07716_en.pdf (accessed on 30 November 2021).
- Osmanlliu, E.; Rafie, E.; Bédard, S.; Paquette, J.; Gore, G.; Pomey, M.P. Considerations for the Design and Implementation of COVID-19 Contact Tracing Apps: Scoping Review. JMIR mHealth uHealth 2021, 9, e27102. [Google Scholar] [CrossRef] [PubMed]
- Gagnon, M.-P.; Desmartis, M.; Lepage-Savary, D.; Gagnon, J.; St-Pierre, M.; Rhainds, M.; Lemieux, R.; Gauvin, F.-P.; Pollender, H.; Légaré, F. Introducing patients’ and the public’s perspectives to health technology assessment: A systematic review of international experiences. Int. J. Technol. Assess. Health Care 2011, 27, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Grimshaw, J. SURGE (The SUrvey Reporting GuidelinE). In Guidelines for Reporting Health Research: A User’s Manual; Moher, D., Altman, D.G., Schulz, K.F., Simera, I., Wager, E., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Seto, E.; Challa, P.; Ware, P. Adoption of COVID-19 Contact Tracing Apps: A Balance Between Privacy and Effectiveness. J. Med. Internet Res. 2021, 23, e25726. [Google Scholar] [CrossRef]
- Government of Canada. Canada’s Health Care System. Available online: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html#a4 (accessed on 23 February 2022).
- Government of Canada. COVID-19 Daily Epidemiology Update. Available online: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed on 25 April 2022).
- Culnan, M.J.; Armstrong, P.K. Information privacy concerns, procedural fairness, and impersonal trust: An empirical investigation. Organ. Sci. 1999, 10, 104–115. [Google Scholar] [CrossRef]
- Mercure, P. Oui, Alerte COVID Existe Encore! La Presse. Available online: https://www.lapresse.ca/contexte/2022-01-16/l-edito-vous-repond/oui-alerte-covid-existe-encore.php (accessed on 23 February 2022).
- Montagni, I.; Roussel, N.; Thiébaut, R.; Tzourio, C. Health Care Students’ Knowledge of and Attitudes, Beliefs, and Practices Toward the French COVID-19 App: Cross-sectional Questionnaire Study. J. Med. Internet Res. 2021, 23, e26399. [Google Scholar] [CrossRef] [PubMed]
- Lewandowsky, S.; Dennis, S.; Perfors, A.; Kashima, Y.; White, J.P.; Garrett, P.; Little, D.; Yesilada, M. Public acceptance of privacy-encroaching policies to address the COVID-19 pandemic in the United Kingdom. PLoS ONE 2021, 16, e0245740. [Google Scholar] [CrossRef] [PubMed]
- Garrett, P.M.; Wang, Y.W.; White, J.P.; Kashima, Y.; Dennis, S.; Yang, C.T. High Acceptance of COVID-19 Tracing Technologies in Taiwan: A Nationally Representative Survey Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3323. [Google Scholar] [CrossRef]
- Abraham, C.; Sheeran, P. The health belief model. In Predicting Health Behaviour: Research and Practice with Social Cognition Models, 2nd ed.; Conner, M., Norman, P., Eds.; Open University Press: Buckingham, UK, 2005; pp. 30–55. [Google Scholar]
- Levine, D.M.; Lipsitz, S.R.; Linder, J.A. Trends in Seniors’ Use of Digital Health Technology in the United States, 2011–2014. JAMA 2016, 316, 538–540. [Google Scholar] [CrossRef] [Green Version]
- Anderson, M.; Perrin, A. Technology Use among Seniors. Pew Research Center. 2017. Available online: https://www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/ (accessed on 23 February 2022).
- Pandl, K.D.; Thiebes, S.; Schmidt-Kraepelin, M.; Sunyaev, A. How detection ranges and usage stops impact digital contact tracing effectiveness for COVID-19. Sci. Rep. 2021, 11, 9414. [Google Scholar] [CrossRef]
- Saint-Arnaud, P. Des Dépenses de 20 Millions pour des Résultats Pratiquement Inutiles. La Presse. Available online: https://www.lapresse.ca/covid-19/2021-07-05/application-alerte-covid/des-depenses-de-20-millions-pour-des-resultats-pratiquement-inutiles.php# (accessed on 15 December 2021).
- Government of Québec. Résultats de la Consultation Publique: Utilisation d’une Application Mobile de Notification d’exposition à la COVID-19. Available online: https://consultation.quebec.ca/uploads/decidim/attachment/file/9/COVID-Consultation_Publique-R%C3%A9sultats_publi%C3%A9s_V3.pdf (accessed on 30 November 2021).
- Colizza, V.; Grill, E.; Mikolajczyk, R.; Cattuto, C.; Kucharski, A.; Riley, S.; Kendall, M.; Lythgoe, K.; Bonsall, D.; Wymant, C.; et al. Time to evaluate COVID-19 contact-tracing apps. Nat. Med. 2021, 27, 361–362. [Google Scholar] [CrossRef]
- NWS Government. Create a COVID-19 Check-In Card. Available online: https://www.service.nsw.gov.au/transaction/create-covid-19-check-card (accessed on 30 November 2021).
- Lee, T.; Lee, H. Tracing surveillance and auto-regulation in Singapore: ‘Smart’ responses to COVID-19. Media Int. Aust. 2020, 177, 47–60. [Google Scholar] [CrossRef]
- Fraser Health. Patient Engagement Heard and Valued: A Handbook for Meaningful Engagement of Patients That Have Not Traditionally Been Heard in Healthcare Planning. Available online: https://www.cfhi-fcass.ca/docs/default-source/itr/pe-hub/awesome_handbook-fraserhealth.pdf (accessed on 19 January 2022).
| Demographic Characteristics of the COVID Alert Survey Respondents | n (% a) |
|---|---|
| Gender | |
| Male | 485 (50.6) |
| Female | 471 (49.1) |
| Gender diverse | 1 (0.1) |
| I prefer not to answer | 2 (0.2) |
| Age | |
| 18–24 years | 30 (3.1) |
| 25–34 years | 106 (11.1) |
| 35–44 years | 132 (13.8) |
| 45–54 years | 171 (17.8) |
| 55–64 years | 236 (24.6) |
| 65 years or older | 284 (29.6) |
| Region | |
| Greater Montréal Area | 479 (49.9) |
| Greater Québec Area | 122 (12.7) |
| Other regions of Québec | 353 (36.8) |
| Missing data | 5 (0.5) |
| Occupation | |
| Working | 520 (54.2) |
| Unemployed | 39 (4.1) |
| Retired | 335 (34.9) |
| Student | 34 (3.5) |
| Disability | 3 (0.3) |
| Other | 24 (2.5) |
| I prefer not to answer | 4 (0.4) |
| Education | |
| Without a university diploma | 603 (62.9) |
| With a university diploma | 351 (36.6) |
| Other | 2 (0.2) |
| I prefer not to answer | 3 (0.3) |
| First language | |
| French | 823 (85.8) |
| English | 103 (10.7) |
| Other | 33 (3.4) |
| Self-perceived risk of complications from COVID-19 | |
| No | 718 (74.9) |
| Yes | 223 (23.3) |
| I don’t know/I prefer not to answer | 18 (1.9) |
| Owns a smartphone | |
| Yes | 791 (82.5) |
| No | 168 (17.5) |
| Usage frequency of common mobile apps b | |
| Often (several times a week) | 651 (82.3) |
| Sometimes (a few times a month) | 117 (14.8) |
| Never | 16 (2.0) |
| I don’t know/I prefer not to answer | 7 (0.9) |
| Experience with and Perspectives on the COVID Alert App and the COVID-19 Pandemic a,b,c | % (95% CI) |
|---|---|
| Have downloaded the COVID Alert app | |
| Yes | 43.1 (39.0–47.0) |
| No | 52.7 (48.5–57.0) |
| Tried to but it didn’t work | 3.3 (2.2–5.0) |
| Don’t know/Prefer not to answer | 0.9 (0.2–4.0) |
| COVID Alert app is… | |
| Activated | 84.3 (79.5–88.0) |
| Not activated | 3.3 (1.9–6.0) |
| Uninstalled | 11.4 (8.1–16.0) |
| Don’t know/Prefer not to answer | 1.0 (0.03–3) |
| Have you tested positive for COVID-19? | |
| Yes | 3.9 (2.6–6.0) |
| No | 95.9 (94.1–97.0) |
| Don’t know/Prefer not to answer | 0.2 (0.05–1.0) |
| Did you report the positive result in the app? | |
| Yes | 62.1 (30.0–86.0) |
| No | 37.9 (13.5–7.0) |
| Don’t know/Prefer not to answer | 0.0 (0) |
| If you had received a positive test for COVID-19, would you have reported it in the app? | |
| Yes | 93.3 (88.0–96.0) |
| No | 2.7 (1.4–5.0) |
| Don’t know/Prefer not to answer | 4.0 (2.3–7.0) |
| Perceived risk of exposure to COVID-19 | |
| Low | 52.6 (48.8–56.0) |
| Moderate | 37.8 (34.2–42.0) |
| High | 8.2 (6.4–11.0) |
| Don’t know/Prefer not to answer | 1.4 (0.6–3.0) |
| Perceived knowledge of the COVID Alert app | |
| Low | 42.8 (39.0–47.0) |
| Average | 39.2 (35.5–43.0) |
| High | 14.1 (11.7–17.0) |
| Don’t know/Prefer not to answer | 3.9 (2.4–6.0) |
| Had concerns about this type of app | |
| Yes | 38.2 (34.5–42.0) |
| No | 53.3 (49.0–57.0) |
| Don’t know/Prefer not to answer | 8.51 (6.5–11.0) |
| The application can identify users | |
| Agree | 28.8 (25.4–32.0) |
| Disagree | 45.4 (41.7–49.0) |
| Don’t know/Prefer not to answer | 25.8 (22.6–29.0) |
| The application locates users by GPS | |
| Agree | 45.7 (41.9–50.0) |
| Disagree | 31.9 (28.4–35.0) |
| Don’t know/Prefer not to answer | 22.4 (19.5–26.0) |
| The app helps fight the COVID-19 pandemic | |
| Agree | 40.0 (36.3–44.0) |
| Disagree | 43.6 (39.8–47.0) |
| Don’t know/Prefer not to answer | 16.4 (13.8–19.0) |
| The app protects personal data adequately | |
| Agree | 36.6 (33.1–40.0) |
| Disagree | 33.1 (29.5–37.0) |
| Don’t know/Prefer not to answer | 30.3 (27.0–34.0) |
| The information collected by the app could be used to monitor the population | |
| Agree | 46.8 (43.0–51.0) |
| Disagree | 42.5 (38.7–46.0) |
| I don’t know/I prefer not to answer | 10.8 (8.7–13.0) |
| The app only collects the information users have consented to provide | |
| Agree | 56.6 (52.8–60.0) |
| Disagree | 23.6 (20.5–27.0) |
| I don’t know/I prefer not to answer | 19.7 (16.9–23.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osmanlliu, E.; Paquette, J.; Rodriguez Duarte, M.A.; Bédard, S.; de Marcellis-Warin, N.; Zhegu, M.; Régis, C.; Bouthillier, M.-E.; Grenier, A.-D.; Lewis, P.; et al. Public Perspectives on Exposure Notification Apps: A Patient and Citizen Co-Designed Study. J. Pers. Med. 2022, 12, 729. https://doi.org/10.3390/jpm12050729
Osmanlliu E, Paquette J, Rodriguez Duarte MA, Bédard S, de Marcellis-Warin N, Zhegu M, Régis C, Bouthillier M-E, Grenier A-D, Lewis P, et al. Public Perspectives on Exposure Notification Apps: A Patient and Citizen Co-Designed Study. Journal of Personalized Medicine. 2022; 12(5):729. https://doi.org/10.3390/jpm12050729
Chicago/Turabian StyleOsmanlliu, Esli, Jesseca Paquette, Maria Alejandra Rodriguez Duarte, Sylvain Bédard, Nathalie de Marcellis-Warin, Majlinda Zhegu, Catherine Régis, Marie-Eve Bouthillier, Annie-Danielle Grenier, Paul Lewis, and et al. 2022. "Public Perspectives on Exposure Notification Apps: A Patient and Citizen Co-Designed Study" Journal of Personalized Medicine 12, no. 5: 729. https://doi.org/10.3390/jpm12050729
APA StyleOsmanlliu, E., Paquette, J., Rodriguez Duarte, M. A., Bédard, S., de Marcellis-Warin, N., Zhegu, M., Régis, C., Bouthillier, M.-E., Grenier, A.-D., Lewis, P., & Pomey, M.-P. (2022). Public Perspectives on Exposure Notification Apps: A Patient and Citizen Co-Designed Study. Journal of Personalized Medicine, 12(5), 729. https://doi.org/10.3390/jpm12050729







