The Influence of the CES1 Genotype on the Pharmacokinetics of Enalapril in Patients with Arterial Hypertension
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Pharmacokinetic Study Design and Determination of Drug Concentrations
2.3. DNA Extraction
2.4. CES1 Genotyping
2.5. Statistical Analysis
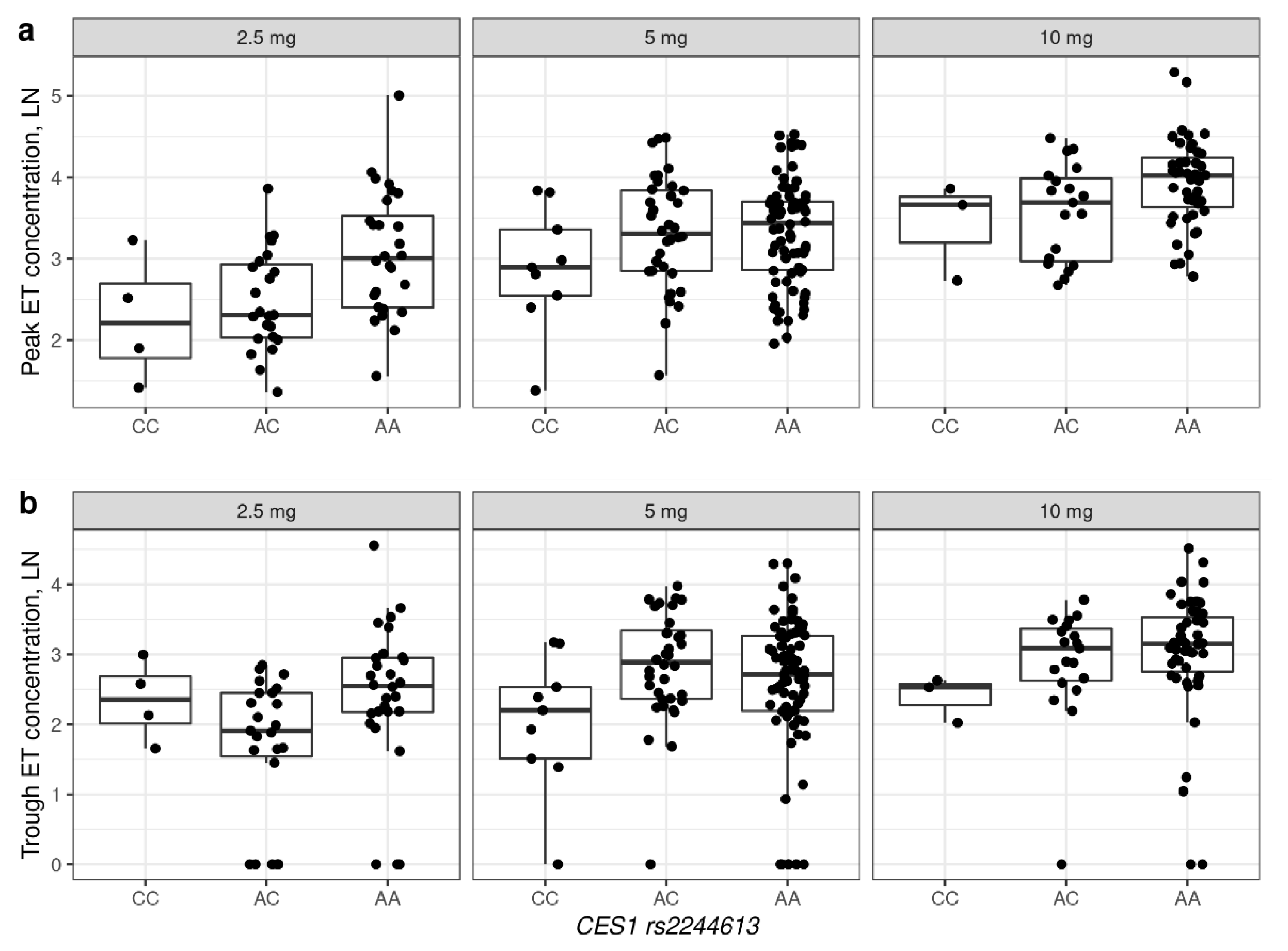
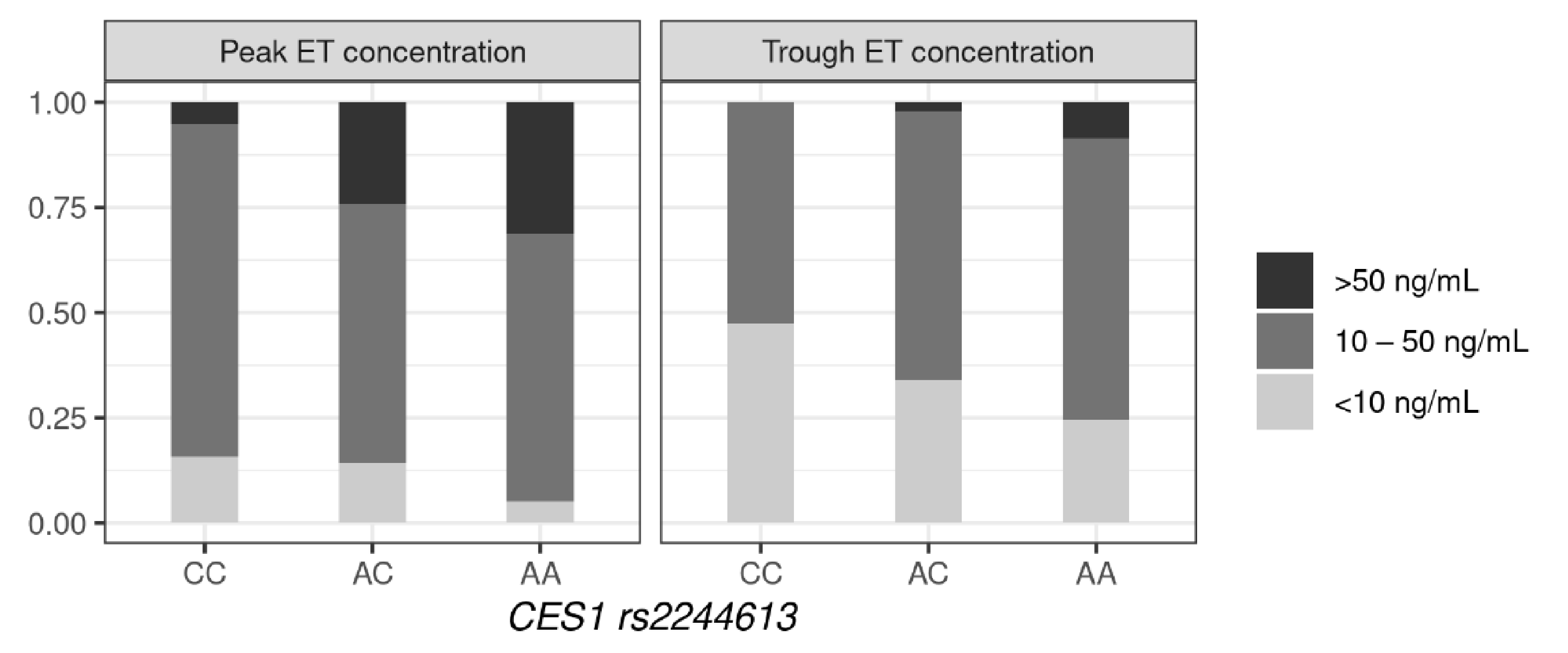
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. List of Co-Medications Taken by Patients, n (%)
- Calcium channel blockers—120 (42%)
- Loop diuretics—42 (14.7%)
- Potassium-sparing diuretics—45 (15.7%)
- Thiazides and thiazide-like diuretics—94 (32.9%)
- Losartan—18 (6.3%)
- Digoxin—20 (7%)
- β-blockers—232 (81.1%)
- Statins—217 (75.9%)
- Aspirin—119 (41.6%)
- Warfarin—28 (9.8%)
- Rivaroxaban—45 (15.7%)
- Dabigatran—12 (4.2%)
- Metformin—54 (18.9%)
- Other glucose-lowering drugs—38 (13.3%)
- Proton-pump inhibitors (PPIs)—57 (19.9%)
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Thomsen, R.; Rasmussen, H.B.; Linnet, K.; The INDICES Consortium. In Vitro Drug Metabolism by Human Carboxylesterase 1: Focus on Angiotensin-Converting Enzyme Inhibitors. Drug Metab. Dispos. 2013, 42, 126–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Wang, G.; Shi, J.; Aa, J.; Comas, R.; Liang, Y.; Zhu, H.-J. CES1 genetic variation affects the activation of angiotensin-converting enzyme inhibitors. Pharmacogenomics J. 2015, 16, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Tarkiainen, E.K.; Tornio, A.; Holmberg, M.T.; Launiainen, T.; Neuvonen, P.J.; Backman, J.T.; Niemi, M. Effect of carboxylesterase 1 c.428G > A single nucleotide variation on the pharmacokinetics of quinapril and enalapril. Br. J. Clin. Pharmacol. 2015, 80, 1131–1138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Her, L.H.; Wang, X.; Shi, J.; Choi, H.J.; Jung, S.M.; Smith, L.S.; Wu, A.H.; Bleske, B.E.; Zhu, H. Effect of CES1 genetic variation on enalapril steady-state pharmacokinetics and pharmacodynamics in healthy subjects. Br. J. Clin. Pharmacol. 2021, 87, 4691–4700. [Google Scholar] [CrossRef] [PubMed]
- Stage, C.; Jürgens, G.; Guski, L.S.; Thomsen, R.; Bjerre, D.; Ferrero-Miliani, L.; Lyauk, Y.K.; Rasmussen, H.B.; Dalhoff, K.; The INDICES Consortium (for members of this consortium-see Supplementum). The Pharmacokinetics of Enalapril in Relation to CES1 Genotype in Healthy Danish Volunteers. Basic Clin. Pharmacol. Toxicol. 2017, 121, 487–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, J.P.; Horenstein, R.B.; Ryan, K.; O’Connell, J.R.; Gibson, Q.; Mitchell, B.; Tanner, K.; Chai, S.; Bliden, K.P.; Tantry, U.S.; et al. The functional G143E variant of carboxylesterase 1 is associated with increased clopidogrel active metabolite levels and greater clopidogrel response. Pharmacogenetics Genom. 2013, 23, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Tarkiainen, E.K.; Holmberg, M.T.; Tornio, A.; Neuvonen, M.; Neuvonen, P.; Backman, J.T.; Niemi, M. Carboxylesterase 1 c.428G>A single nucleotide variation increases the antiplatelet effects of clopidogrel by reducing its hydrolysis in humans. Clin. Pharmacol. Ther. 2015, 97, 650–658. [Google Scholar] [CrossRef]
- Zhu, H.-J.; Wang, X.; Gawronski, B.E.; Brinda, B.J.; Angiolillo, D.J.; Markowitz, J.S. Carboxylesterase 1 as a Determinant of Clopidogrel Metabolism and Activation. J. Pharmacol. Exp. Ther. 2012, 344, 665–672. [Google Scholar] [CrossRef] [Green Version]
- Sychev, D.A.; Levanov, A.N.; Shelekhova, T.V.; Bochkov, P.O.; Denisenko, N.P.; Ryzhikova, K.A.; Mirzaev, K.B.; Grishina, E.A.; Gavrilov, M.A.; Ramenskaya, G.V.; et al. The impact of ABCB1 (rs1045642 and rs4148738) and CES1 (rs2244613) gene polymorphisms on dabigatran equilibrium peak concentration in patients after total knee arthroplasty. Pharmacogenomics Pers. Med. 2018, 11, 127–137. [Google Scholar] [CrossRef] [Green Version]
- Sychev, D.; Skripka, A.; Ryzhikova, K.; Bochkov, P.; Shevchenko, R.; Krupenin, P.; Ivashchenko, D.; Kogay, V.; Listratov, A.; Krainyaya, A.; et al. Effect of CES1 and ABCB1 genotypes on the pharmacokinetics and clinical outcomes of dabigatran etexilate in patients with atrial fibrillation and chronic kidney disease. Drug Metab. Pers. Ther. 2020, 35. [Google Scholar] [CrossRef]
- Dimatteo, C.; D’Andrea, G.; Vecchione, G.; Paoletti, O.; Cappucci, F.; Tiscia, G.L.; Buono, M.; Grandone, E.; Testa, S.; Margaglione, M. Pharmacogenetics of dabigatran etexilate interindividual variability. Thromb. Res. 2016, 144, 1–5. [Google Scholar] [CrossRef]
- Paré, G.; Eriksson, N.; Lehr, T.; Connolly, S.; Eikelboom, J.; Ezekowitz, M.D.; Axelsson, T.; Haertter, S.; Oldgren, J.; Reilly, P.; et al. Genetic determinants of dabigatran plasma levels and their relation to bleeding. Circulation 2013, 127, 1404–1412. [Google Scholar] [CrossRef] [Green Version]
- Shi, J.; Wang, X.; Nguyen, J.H.; Bleske, B.E.; Liang, Y.; Liu, L.; Zhu, H.-J. Dabigatran etexilate activation is affected by the CES1 genetic polymorphism G143E (rs71647871) and gender. Biochem. Pharmacol. 2016, 119, 76–84. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Yang, C.; Qi, W.; Pei, Z.; Xue, W.; Zhu, H.; Dong, M.; Guo, Y.; Cong, D.; Wang, F. The Impact of ABCB1 and CES1 Polymorphisms on Dabigatran Pharmacokinetics in Healthy Chinese Subjects. Pharmacogenomics Pers. Med. 2021, 14, 477–485. [Google Scholar] [CrossRef]
- Stage, C.; Jürgens, G.; Guski, L.S.; Thomsen, R.; Bjerre, D.; Ferrero-Miliani, L.; Lyauk, Y.K.; Rasmussen, H.B.; Dalhoff, K.; The INDICES Consortium. The impact of CES1 genotypes on the pharmacokinetics of methylphenidate in healthy Danish subjects. Br. J. Clin. Pharmacol. 2017, 83, 1506–1514. [Google Scholar] [CrossRef] [Green Version]
- Stage, C.; Dalhoff, K.; Rasmussen, H.B.; Guski, L.S.; Thomsen, R.; Bjerre, D.; Ferrero-Miliani, L.; Madsen, M.B.; Jürgens, G. The impact of human CES1 genetic variation on enzyme activity assessed by ritalinic acid/methylphenidate ratios. Basic Clin. Pharmacol. Toxicol. 2019, 125, 54–61. [Google Scholar] [CrossRef]
- Shi, J.; Wang, X.; Eyler, R.F.; Liang, Y.; Liu, L.; Mueller, B.A.; Zhu, H.-J. Association of Oseltamivir Activation with Gender and Carboxylesterase 1 Genetic Polymorphisms. Basic Clin. Pharmacol. Toxicol. 2016, 119, 555–561. [Google Scholar] [CrossRef] [Green Version]
- Tarkiainen, E.K.; Backman, J.T.; Neuvonen, M.; Neuvonen, P.J.; Schwab, M.; Niemi, M. Carboxylesterase 1 polymorphism impairs oseltamivir bioactivation in humans. Clin. Pharmacol. Ther. 2012, 92, 68–71. [Google Scholar] [CrossRef]
- Oh, J.; Lee, S.; Lee, H.; Cho, J.-Y.; Yoon, S.H.; Jang, I.-J.; Yu, K.-S.; Lim, K.S. The novel carboxylesterase 1 variant c.662A>G may decrease the bioactivation of oseltamivir in humans. PLoS ONE 2017, 12, e0176320. [Google Scholar] [CrossRef]
- Liu, D.; Li, X.; Li, X.; Wang, H.; Dong, M. Carboxylesterase 1 polymorphisms are associated with clinical outcomes in gastroenteric cancer patients treated with capecitabine. Cancer Chemother. Pharmacol. 2021, 87, 681–687. [Google Scholar] [CrossRef]
- Hamzic, S.; Kummer, D.; Milesi, S.; Mueller, D.; Joerger, M.; Aebi, S.; Amstutz, U.; Largiader, C. Novel Genetic Variants in Carboxylesterase 1 Predict Severe Early-Onset Capecitabine-Related Toxicity. Clin. Pharmacol. Ther. 2017, 102, 796–804. [Google Scholar] [CrossRef]
- Yamada, S.; Richardson, K.; Tang, M.; Halaschek-Wiener, J.; Cook, V.J.; Fitzgerald, J.M.; Elwood, K.; Marra, F.; Brooks-Wilson, A. Genetic variation in carboxylesterase genes and susceptibility to isoniazid-induced hepatotoxicity. Pharm. J. 2010, 10, 524–536. [Google Scholar] [CrossRef] [Green Version]
- Ji, Q.; Zhang, C.; Xu, Q.; Wang, Z.; Li, X.; Lv, Q. The impact of ABCB1 and CES1 polymorphisms on dabigatran pharmacokinetics and pharmacodynamics in patients with atrial fibrillation. Br. J. Clin. Pharmacol. 2020, 87, 2247–2255. [Google Scholar] [CrossRef]
- Mirzaev, K.B.; Osipova, D.V.; Kitaeva, E.J.; Shprakh, V.V.; Abdullaev, S.; Andreev, D.; Mumladze, R.B.; Sychev, D.A. Effects of the rs2244613 polymorphism of the CES1 gene on the antiplatelet effect of the receptor P2Y12 blocker clopidogrel. Drug Metab. Pers. Ther. 2019, 34. [Google Scholar] [CrossRef]
- Tanimoto, K.; Kaneyasu, M.; Shimokuni, T.; Hiyama, K.; Nishiyama, M. Human carboxylesterase 1A2 expressed from carboxylesterase 1A1 and 1A2 genes is a potent predictor of CPT-11 cytotoxicity in vitro. Pharmacogenetics Genom. 2007, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Kurella Tamura, M.; Feldman, H.I. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodina, T.A.; Melnikov, E.S.; Belkov, S.A.; Sokolov, A.V.; Prokofiev, A.B.; Sivkov, A.S. Express method for determination of en-alapril and enalaprilat in human serum BY HPLC-MS/MS. Drug Dev. Regist. 2016, 4, 184–189. (In Russian) [Google Scholar]
- Ferrero-Miliani, L.; Bjerre, D.; Stage, C.; Madsen, M.B.; Jűrgens, G.; Dalhoff, K.P.; Rasmussen, H.B. Reappraisal of the genetic diversity and pharmacogenetic assessment of CES1. Pharmacogenomics 2017, 18, 1241–1257. [Google Scholar] [CrossRef] [PubMed]
- Ikonnikova, A.Y.; Filippova, M.A.; Surzhikov, S.A.; Pozhitnova, V.O.; Kazakov, R.E.; Lisitsa, T.S.; Belkov, S.A.; Nasedkina, T.V. Biochip-based approach for comprehensive pharmacogenetic testing. Drug Metab. Pers. Ther. 2020, 36, 33–40. [Google Scholar] [CrossRef]
- Shershov, V.E.; Ikonnikova, A.Y.; Vasiliskov, V.A.; Lapa, S.A.; Miftakhov, R.A.; Kuznetsova, V.E.; Chudinov, A.V.; Nasedkina, T.V. The Efficiency of DNA Labeling with Near-Infrared Fluorescent Dyes. Biophysics 2020, 65, 736–741. [Google Scholar] [CrossRef]
- Solé, X.; Guinó, E.; Valls, J.; Iniesta, R.; Moreno, V. SNPStats: A web tool for the analysis of association studies. Bioinformatics 2006, 22, 1928–1929. [Google Scholar] [CrossRef] [Green Version]
- Bjerre, D.; Rasmussen, H.B.; The INDICES Consortium. Novel approach for CES1 genotyping: Integrating single nucleotide variants and structural variation. Pharmacogenomics 2018, 19, 349–359. [Google Scholar] [CrossRef]
- Schulz, M.; Iwersen-Bergmann, S.; Andresen, H.; Schmoldt, A. Therapeutic and toxic blood concentrations of nearly 1,000 drugs and other xenobiotics. Crit. Care 2012, 16, R136. [Google Scholar] [CrossRef] [Green Version]
- Nelveg-Kristensen, K.E.; Bie, P.; Ferrero, L.; Bjerre, D.; Bruun, N.E.; Egfjord, M.; Rasmussen, H.B.; Hansen, P.R.; INDICES Consortium. Pharmacodynamic Impact of Carboxylesterase 1 Gene Variants in Patients with Congestive Heart Failure Treated with Angiotensin-Converting Enzyme Inhibitors. PLoS ONE 2016, 11, e0163341. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | All Patients (n = 286) |
|---|---|
| Gender, n (%) | |
| women | 186 (65%) |
| men | 100 (35%) |
| Age, years (mean ± sd) | 67.22 ± 10.13 |
| Weight, kg (mean ± sd) | 84.6 ± 18.95 |
| BMI (mean ± sd) | 30.89 ± 6.15 |
| GFR, mL/min (mean ± sd) | 72.09 ± 20.08 |
| Grade of arterial hypertension, n (%) | |
| 1 | 10 (3.5%) |
| 2 | 46 (16.1%) |
| 3 | 230 (80.4%) |
| CAD, n (%) | 140 (49%) |
| CHF, n (%) | 110 (38.5%) |
| AF, n (%) | 97 (33.9%) |
| DM type 2, n (%) | 93 (32.5%) |
| Dislipidemia, n (%) | 128 (44.8%) |
| Single enalapril dose, n (%): | |
| 2.5 mg | 55 (19.2%) |
| 5 mg | 121 (42.3%) |
| 7.5 mg | 14 (4.9%) |
| 10 mg | 69 (24.1%) |
| 12.5 mg | 2 (0.7%) |
| 15 mg | 9 (3.1%) |
| 20 mg | 16 (5.6%) |
| Genopype | n, % | HWE χ2 p-Value |
|---|---|---|
| CES1A1c | ||
| wt | 197 (69%) | 0.42 |
| wt/CES1A1c | 83 (29%) | |
| CES1A1c/CES1A1c | 6 (2%) | |
| CES1 rs71647871 | ||
| GG | 279 (97.5%) | 0.83 |
| GA | 7 (2.5%) | |
| AA | 0 (0%) | |
| CES1 rs2244613 | ||
| AA | 176 (61.6%) | 0.13 |
| AC | 91 (31.8%) | |
| CC | 19 (6.6%) | |
| Coefficient | SE | p-Value | ||
|---|---|---|---|---|
| Intercept | 1.413 | 0.292 | 2.10 × 10−6 | *** |
| Age | 0.013 | 0.004 | 0.000756 | *** |
| Single dose, ln | 0.733 | 0.064 | <2 × 10−16 | *** |
| Gender_male | −0.192 | 0.08 | 0.016837 | * |
| CES1 rs2244613_AC | −0.181 | 0.081 | 0.026514 | * |
| CES1 rs2244613_CC | −0.435 | 0.153 | 0.004704 | ** |
| wt/CES1A1c | −0.003 | 0.083 | 0.97459 | |
| CES1A1c/CES1A1c | −0.492 | 0.262 | 0.061048 | . |
| Adjusted R-squared: 0.3679, p-value: <2.2 × 10−16 | ||||
| Coefficient | SE | p-Value | ||
|---|---|---|---|---|
| Intercept | 0.384 | 0.303 | 0.20680 | |
| Age | 0.023 | 0.004 | 1.17 × 10−8 | *** |
| Single dose, ln | 0.556 | 0.069 | 2.34 × 10−14 | *** |
| CES1 rs2244613_AC | −0.12 | 0.087 | 0.16724 | |
| CES1 rs2244613_CC | −0.49 | 0.161 | 0.00263 | ** |
| wt/CES1A1c | −0.111 | 0.088 | 0.20873 | |
| CES1A1c/CES1A1c | −0.605 | 0.294 | 0.04088 | * |
| Adjusted R-squared: 0.2957, p-value: <2.2 × 10−16 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ikonnikova, A.; Rodina, T.; Dmitriev, A.; Melnikov, E.; Kazakov, R.; Nasedkina, T. The Influence of the CES1 Genotype on the Pharmacokinetics of Enalapril in Patients with Arterial Hypertension. J. Pers. Med. 2022, 12, 580. https://doi.org/10.3390/jpm12040580
Ikonnikova A, Rodina T, Dmitriev A, Melnikov E, Kazakov R, Nasedkina T. The Influence of the CES1 Genotype on the Pharmacokinetics of Enalapril in Patients with Arterial Hypertension. Journal of Personalized Medicine. 2022; 12(4):580. https://doi.org/10.3390/jpm12040580
Chicago/Turabian StyleIkonnikova, Anna, Tatiana Rodina, Artem Dmitriev, Evgeniy Melnikov, Ruslan Kazakov, and Tatiana Nasedkina. 2022. "The Influence of the CES1 Genotype on the Pharmacokinetics of Enalapril in Patients with Arterial Hypertension" Journal of Personalized Medicine 12, no. 4: 580. https://doi.org/10.3390/jpm12040580
APA StyleIkonnikova, A., Rodina, T., Dmitriev, A., Melnikov, E., Kazakov, R., & Nasedkina, T. (2022). The Influence of the CES1 Genotype on the Pharmacokinetics of Enalapril in Patients with Arterial Hypertension. Journal of Personalized Medicine, 12(4), 580. https://doi.org/10.3390/jpm12040580






