Acceptance and Factors Influencing Acceptance of COVID-19 Vaccine in a Romanian Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Survey Instrument
2.3. Quality Control
2.4. Ethics Considerations
2.5. Statistical Analyses
3. Results
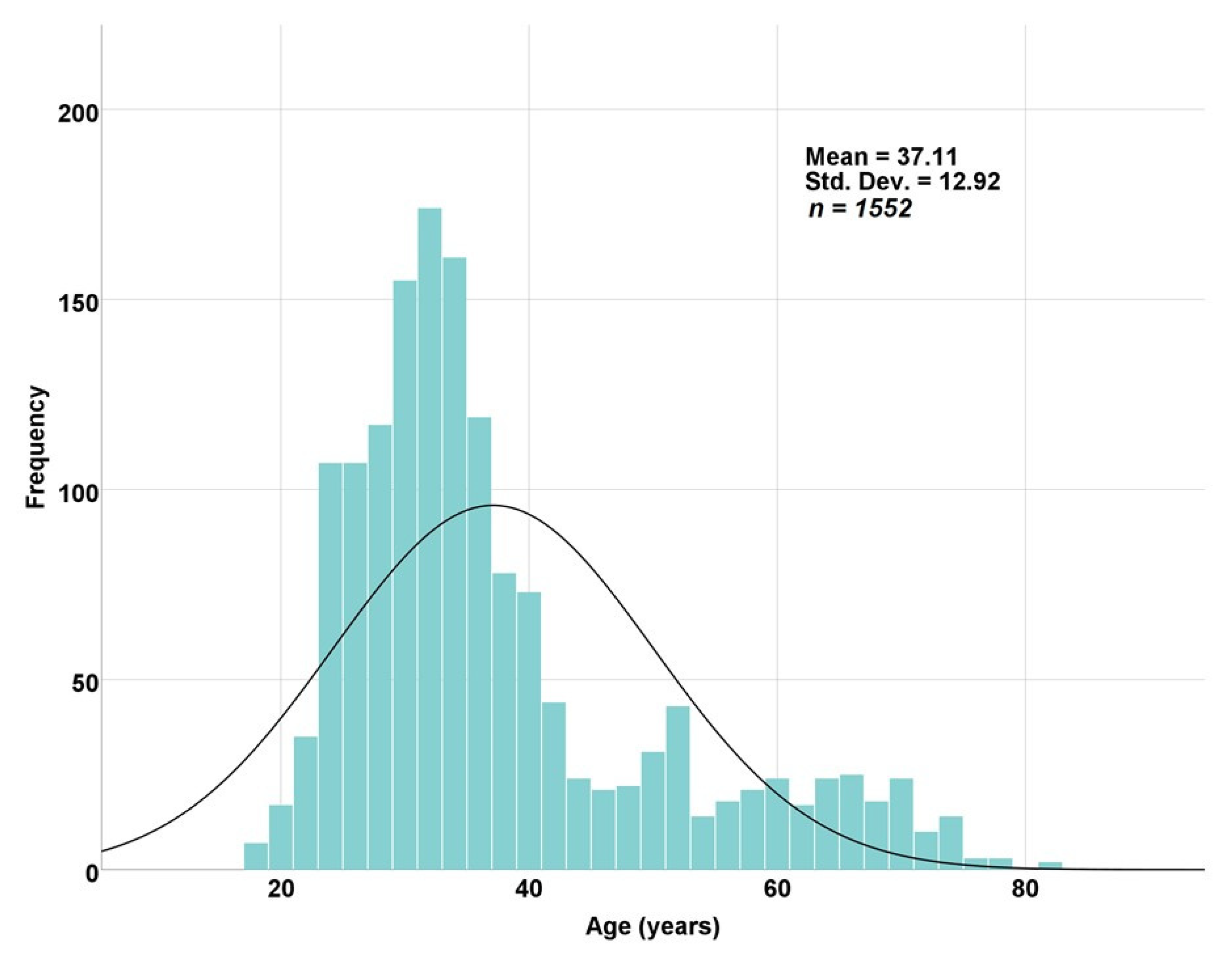
3.1. Socio-Demographic Characteristics
3.2. Medical and Psychiatric Comorbidities
3.3. Lifestyle-Related Characteristics
3.4. Anxiety Levels
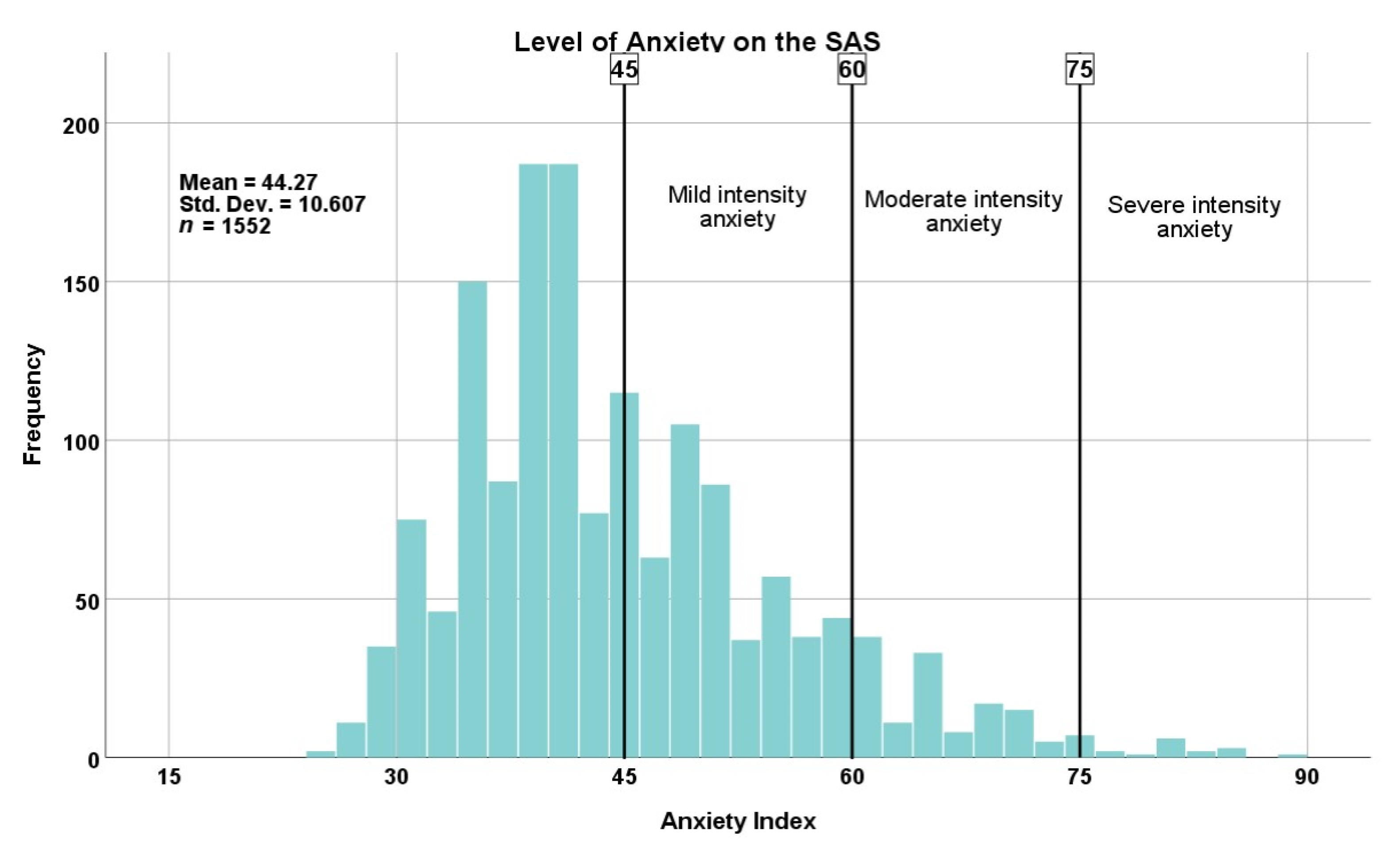
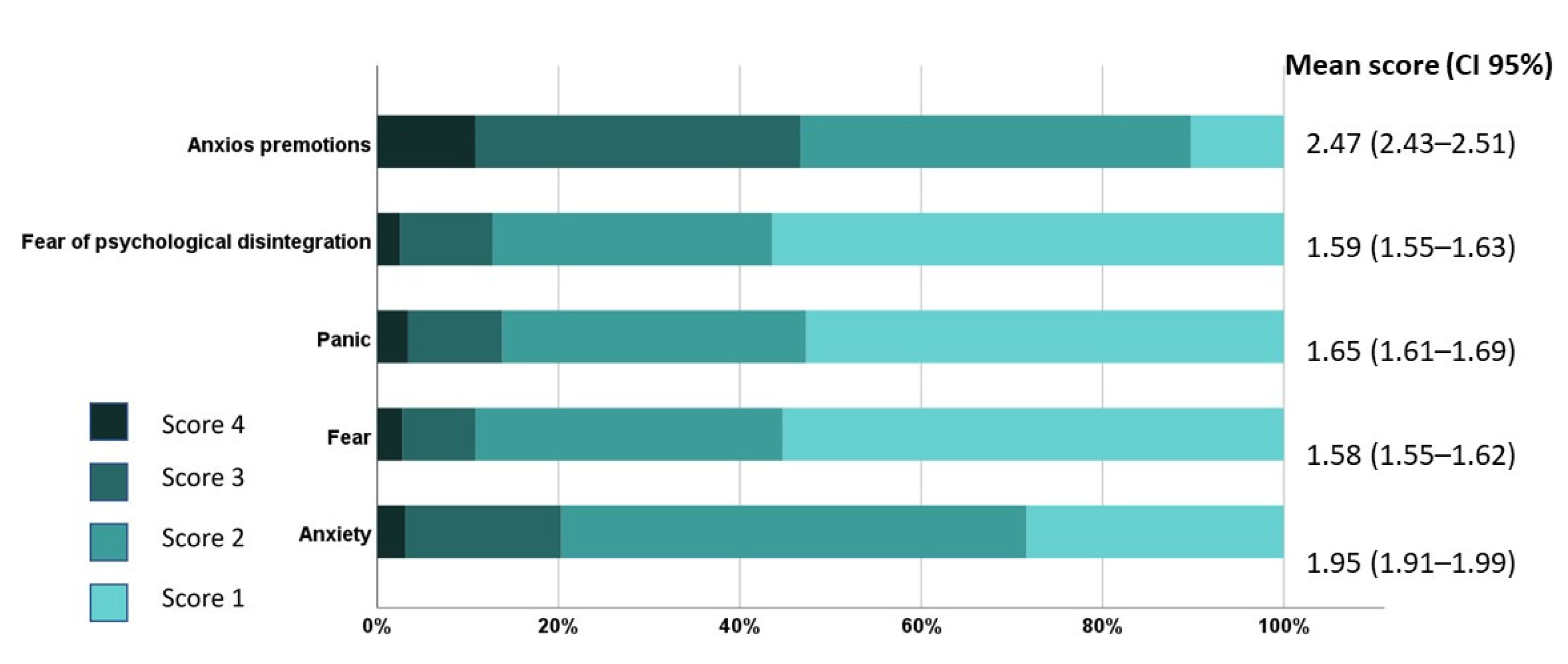
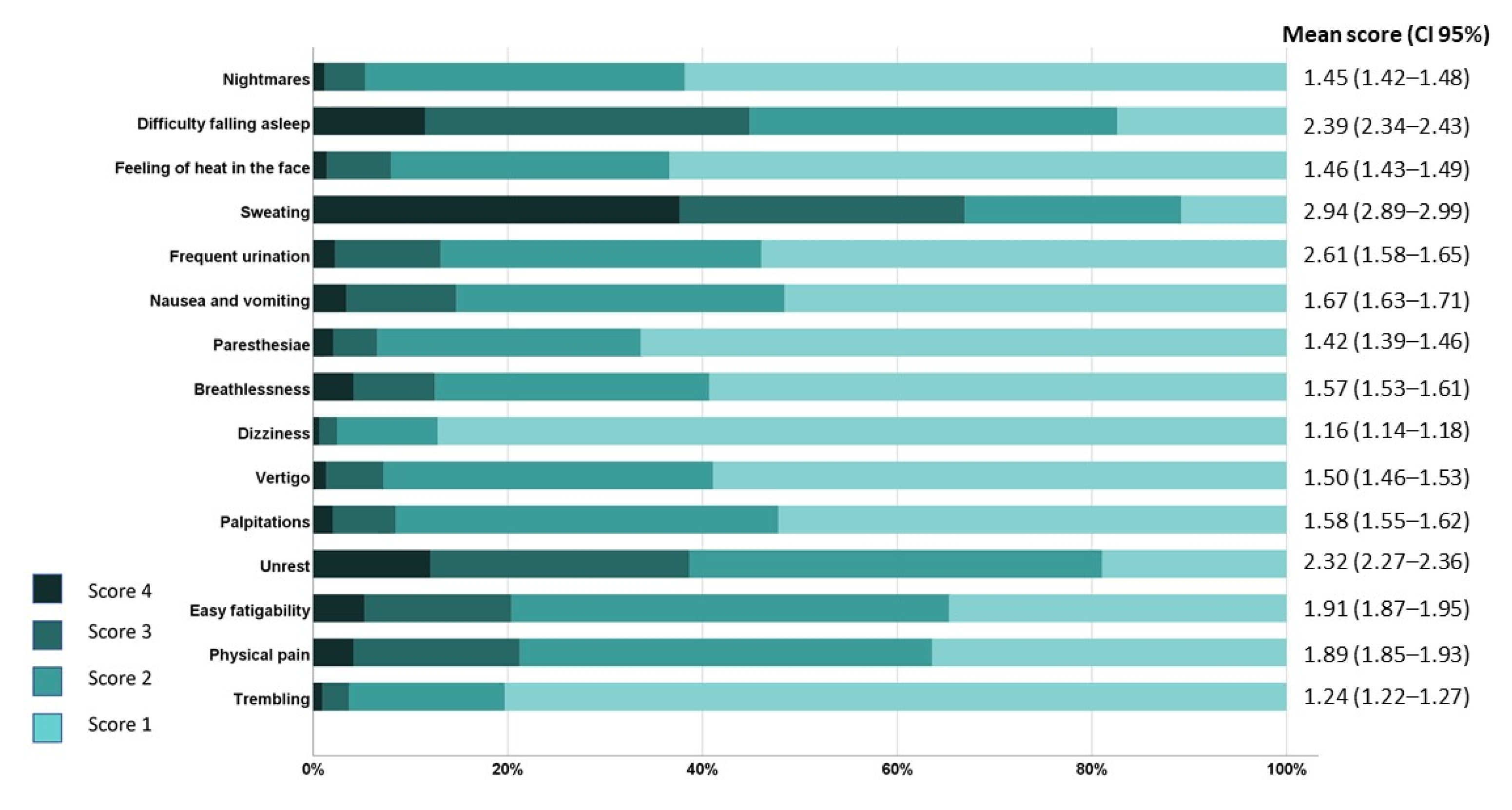
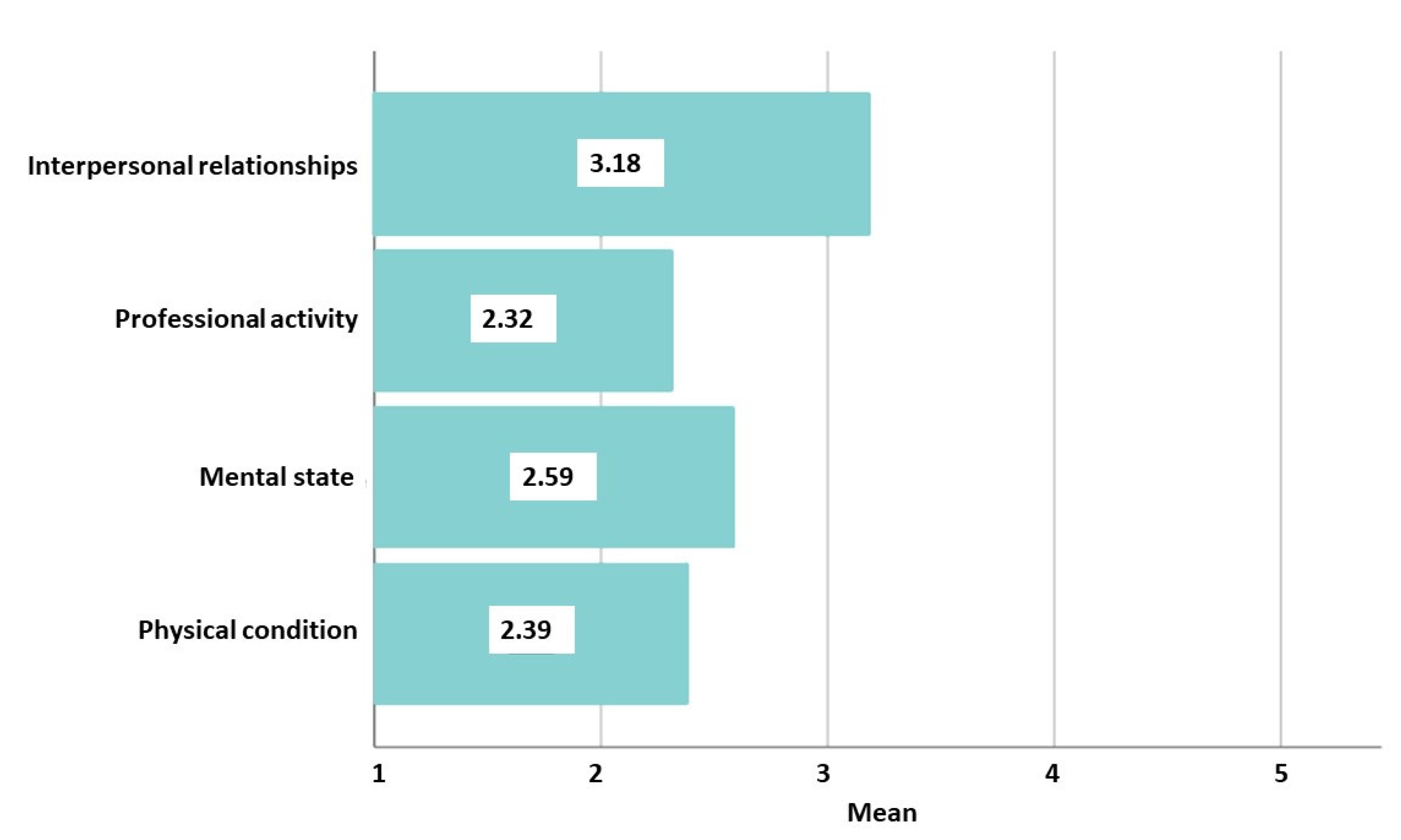
3.5. COVID-19 Pandemic Impact
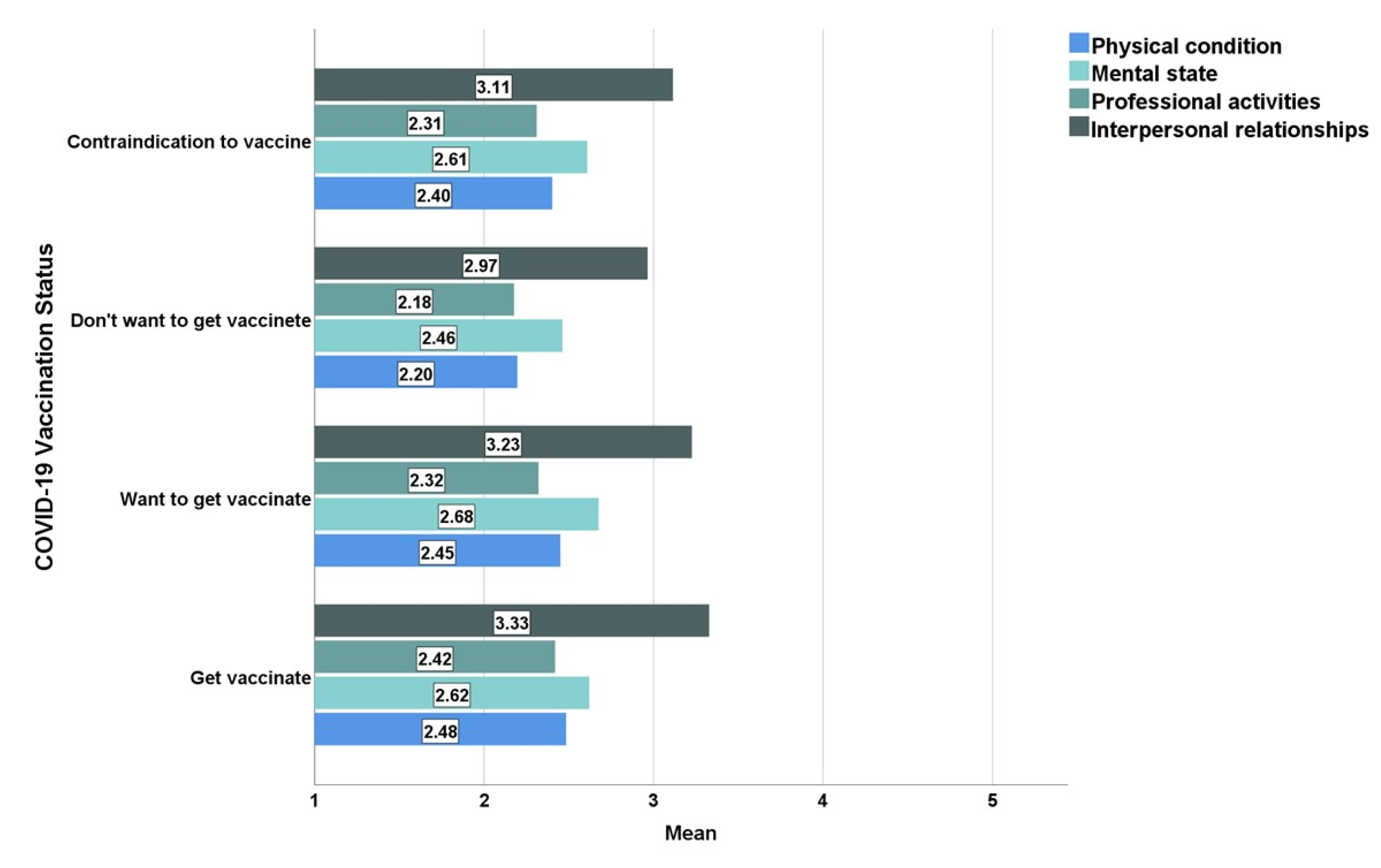
3.6. Results on COVID-19 Vaccination Acceptance
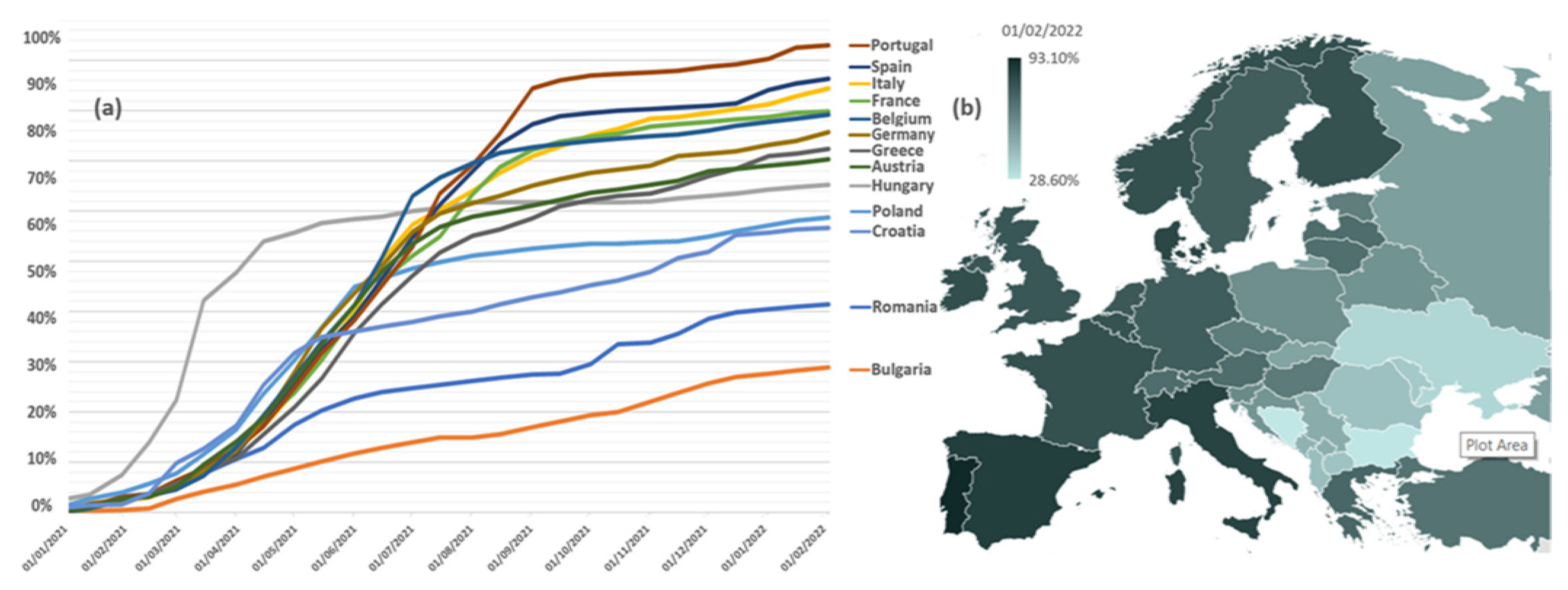
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables | Total (%) n = 1552 | |
|---|---|---|
| Gender | Female | 1217 (78.4) |
| Male | 335 (21.6) | |
| Residency | Urban | 1197 (77.1) |
| Peri-urban | 118 (7.6) | |
| Rural | 237 (15.3) | |
| Marital status | Single | 139 (9) |
| Married | 1049 (67.6) | |
| In relationship | 288 (18.6) | |
| Widow | 25 (1.6) | |
| Divorced | 66 (4.3) | |
| Household size and composition | Living alone | 198 (12.8) |
| Living with partner | 1164 (75.0) | |
| Living with children | 786 (50.6) | |
| Living with parents | 187 (12.0) | |
| Living with siblings | 57 (3.7) | |
| Others | 50 (3.2) | |
| Number of children | 0 | 411 (26.5) |
| 1 | 645 (41.6) | |
| 2 | 427 (27.5) | |
| ≥3 | 69 (4.4) | |
| Educational level | Secondary school | 30 (1.9) |
| Highschool | 426 (27.4) | |
| University graduate | 583 (37.6) | |
| Master graduate | 411 (26.5) | |
| Doctoral degree | 100 (6.4) | |
| Mother’s educational level | No formal education | 6 (0.4) |
| Secondary school | 312 (20.1) | |
| Highschool | 816 (52.6) | |
| University degree | 383 (24.7) | |
| Don’t know | 34 (2.2) | |
| Father’s educational level | No formal education | 9 (0.6) |
| Primary school | 276 (17.8) | |
| Highschool | 811 (52.3) | |
| University degree | 407 (26.2) | |
| Don’t know | 48 (3.1) | |
| Occupational status | Unemployed | 395 (25.4) |
| Student | 149 (9.6) | |
| Employed | 766 (49.4) | |
| Freelance | 113 (20.4) | |
| Retired | 128 (8.2) | |
| Revenues (with comparison to the pre-pandemic period) | Significantly decreased | 87 (5.6) |
| Decreased | 322 (20.7) | |
| Stagnated | 967 (62.3) | |
| Increased | 151 (9.7) | |
| Significantly increased | 25 (1.6) | |
| Religious self-perception | Unreligious | 539 (34.7) |
| Religious | 1013 (65.3) | |
| Any Comorbid Physical Condition(s) %, (n) | ||
|---|---|---|
| Yes | 29.4 | (456) |
| No | 70.6 | (1096) |
| Physical condition(s), %, (n) | ||
| Endocrine and metabolic | 7.8 | (121) |
| Cardiovascular | 7.1 | (110) |
| Rheumatic and musculoskeletal | 3.0 | (46) |
| Hepatic | 2.7 | (42) |
| Neurological | 1.6 | (25) |
| Dermatological | 1.5 | (24) |
| Gynaecological | 1.5 | (23) |
| Pulmonary | 1.2 | (19) |
| Others | 3.8 | (59) |
| Any comorbid mental condition(s) %, (n) | ||
| Yes | 5.6 | (87) |
| No | 94.4 | (1465) |
| Mental condition(s), %, (n) | ||
| Major depression disorder | 3.0 | (47) |
| Anxiety disorder | 1.9 | (30) |
| Others | 0.7 | (10) |
| |||||
| Classification of BMI (kg/m2) According to WHO | |||||
|---|---|---|---|---|---|
| Category | BMI | % | n | ||
| Underweight (Severe thinness) | <16.0 | 0.3 | (4) | ||
| Underweight (Moderate thinness) | 16.0–16.9 | 1.4 | (22) | ||
| Underweight (Mild thinness) | 17.0–18.4 | 4.6 | (72) | ||
| Normal range | 18.5–24.9 | 52.8 | (819) | ||
| Overweight (Pre-obese) | 25.0–29.9 | 27.2 | (422) | ||
| Obese (Class I) | 30.0–34.9 | 10.2 | (158) | ||
| Obese (Class II) | 35.0–39.9 | 2.4 | (37) | ||
| Obese (Class III) | ≥40.0 | 1.2 | (18) | ||
| Self-assessment on weight, %, (n) | |||||
| Very underweight | 16 | (1.0) | |||
| Slightly underweight | 103 | (6.6) | |||
| About right | 786 | (50.7) | |||
| Slightly overweight | 545 | (35.1) | |||
| Very overweight | 102 | (6.6) | |||
| Desire to lose weight, %, (n) | |||||
| Yes | 64.5 | (1001) | |||
| No | 35.5 | (551) | |||
| Dieting to lose weight, %, (n) | |||||
| Yes | 15.7 | (244) | |||
| No | 84.3 | (1308) | |||
| |||||
| Physical activity over the past 2 weeks? | What physical activity? | ||||
| Yes No | % 58.6 41.4 | n (909) (643) |
| % | n |
| 14.0 | (218) | |||
| 13.1 | (204) | |||
| 10.4 | (161) | |||
| 7.9 | (123) | |||
| 3.5 | (54) | |||
| 3.7 | (59) | |||
| Desire to increase physical activity | |||||
| Yes | 82.5 | (1280) | |||
| No | 17.5 | (271) | |||
| |||||
| 23.4 | (363) | |||
| 64.6 | (1003) | |||
| 12.0 | (186) | |||
| Demographic Variables | Anxiety Index (SAS) | |||||
|---|---|---|---|---|---|---|
| Median | Mean | 95.0% Lower CL for Mean | 95.0% Upper CL for Mean | p Value | ||
| Gender | Female | 43 | 45.21 | 44.6 | 45.81 | |
| Male | 39 | 40.89 | 39.91 | 41.86 | <0.001 ** | |
| Age groups | <25 | 46 | 48.33 | 46.42 | 50.24 | |
| 25–34 | 43 | 44.66 | 43.88 | 45.44 | ||
| 35–44 | 40 | 42.78 | 41.75 | 43.82 | ||
| 45–54 | 41 | 43.73 | 41.69 | 45.78 | ||
| 55–64 | 41 | 42.87 | 41.28 | 44.45 | ||
| >65 | 41 | 41.98 | 40.26 | 43.7 | <0.001 ** | |
| Residency | Urban | 41 | 43.94 | 43.34 | 44.53 | |
| Rural | 41 | 44.85 | 42.78 | 46.92 | ||
| Educational level | Secondary school | 55 | 54.33 | 49.6 | 59.07 | |
| Highschool | 45 | 46.32 | 45.24 | 47.4 | ||
| University graduate | 41 | 43.65 | 42.81 | 44.49 | ||
| Master graduate | 40 | 42.43 | 41.51 | 43.35 | ||
| Doctoral degree | 42 | 43.91 | 41.93 | 45.89 | =0.001 ** | |
| Occupational status | Employed | 41 | 43.69 | 42.97 | 44.42 | |
| Student | 46 | 47.34 | 45.38 | 49.29 | ||
| Retired | 41 | 42.55 | 41.05 | 44.05 | ||
| Unemployment | 50 | 49.97 | 47.14 | 52.8 | ||
| Freelancer | 39 | 42.21 | 40.09 | 44.33 | =0.168 | |
| Being parents | No | 44 | 45.72 | 44.59 | 46.86 | |
| Yes | 41 | 43.76 | 43.17 | 44.34 | =0.007 ** | |
| Number of children | 0 | 44 | 45.73 | 44.6 | 46.86 | |
| 1 | 41 | 43.75 | 42.96 | 44.54 | ||
| 2 | 41 | 43.99 | 43.02 | 44.96 | ||
| ≥3 | 40 | 42.92 | 40.25 | 45.6 | =0.016 * | |
| Revenues | Significantly decreased | 48 | 48.99 | 46.16 | 51.82 | |
| Decreased | 45 | 46.87 | 45.57 | 48.17 | ||
| Stagnated | 41 | 43.22 | 42.61 | 43.83 | ||
| Increased | 41 | 42.89 | 41.34 | 44.45 | ||
| Significantly increased | 38 | 43.44 | 38.51 | 48.37 | <0.001 ** | |
| Family background | Wealthy | 37 | 40.50 | 35.71 | 45.29 | <0.001 ** |
| Quite well off | 40 | 42.38 | 41.68 | 43.07 | ||
| Not very well off | 44 | 46.06 | 45.28 | 46.84 | ||
| Quite poor | 48 | 46.93 | 41.45 | 52.42 | ||
| Satisfied with their own lives | Extremely satisfied | 38 | 38.64 | 37.76 | 39.52 | |
| Moderately satisfied | 41 | 44.03 | 43.43 | 44.62 | ||
| Neither satisfied nor dissatisfied | 50 | 51.31 | 49.68 | 52.94 | ||
| Moderately dissatisfied | 56 | 56.67 | 53.13 | 60.22 | ||
| Extremely dissatisfied | 61 | 61.82 | 51.36 | 72.28 | <0.001 ** | |
References
- Eurosurveillance Editorial Team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Eurosurveillance 2020, 25, 200131e. [Google Scholar] [CrossRef]
- Zanke, A.A.; Thenge, R.R.; Adhao, V.S. A Pandemic Declare by World Health Organization: COVID-19. IP Int. J. Compr. Adv. Pharmacol. 2021, 5, 449–457. [Google Scholar] [CrossRef]
- Ghebreyesus, T. WHO Director-General Opening Remarks at the Member State Briefing on the COVID-19 Pandemic Evaluation. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 10 February 2022).
- Mo, P.K.-H.; Luo, S.; Wang, S.; Zhao, J.; Zhang, G.; Li, L.; Li, L.; Xie, L.; Lau, J.T. Intention to receive the COVID-19 vaccination in China: Application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines 2021, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Randolph, H.E.; Barreiro, L.B. Herd immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
- Chen, Y.-T. The effect of vaccination rates on the infection of COVID-19 under the vaccination rate below the herd immunity threshold. Int. J. Environ. Res. Public Health 2021, 18, 7491. [Google Scholar] [CrossRef]
- Dascalu, S.; Geambasu, O.; Covaciu, O.; Chereches, R.M.; Diaconu, G.; Dumitra, G.G.; Gheorghita, V.; Popovici, E.D. Prospects of COVID-19 Vaccination in Romania: Challenges and Potential Solutions. Front. Public Health 2021, 9, 90. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Ruiz, J.B.; Bell, R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef]
- Haynes, B.F.; Corey, L.; Fernandes, P.; Gilbert, P.B.; Hotez, P.J.; Rao, S.; Santos, M.R.; Schuitemaker, H.; Watson, M.; Arvin, A. Prospects for a safe COVID-19 vaccine. Sci. Transl. Med. 2020, 12, eabe0948. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.; Shevlin, M.; McBride, O.; Hartman, T. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Haque, A.; Pant, A.B. Efforts at COVID-19 vaccine development: Challenges and successes. Vaccines 2020, 8, 739. [Google Scholar] [CrossRef] [PubMed]
- Domnich, A.; Grassi, R.; Fallani, E.; Ciccone, R.; Bruzzone, B.; Panatto, D.; Ferrari, A.; Salvatore, M.; Cambiaggi, M.; Vasco, A.; et al. Acceptance of COVID-19 and Influenza Vaccine Co-Administration: Insights from a Representative Italian Survey. J. Pers. Med. 2022, 12, 139. [Google Scholar] [CrossRef]
- Eibensteiner, F.; Ritschl, V.; Nawaz, F.A.; Fazel, S.S.; Tsagkaris, C.; Kulnik, S.T.; Crutzen, R.; Klager, E.; Völkl-Kernstock, S.; Schaden, E.; et al. People’s Willingness to Vaccinate against COVID-19 Despite Their Safety Concerns: Twitter Poll Analysis. J. Med. Internet Res. 2021, 23, e28973. [Google Scholar] [CrossRef]
- Maturkanič, P.; Čergeťová, I.T.; Králik, R.; Hlad, Ľ.; Roubalová, M.; Martin, J.G.; Judák, V.; Akimjak, A.; Petrikovičová, L. The Phenomenon of Social and Pastoral Service in Eastern Slovakia and Northwestern Czech Republic during the COVID-19 Pandemic: Comparison of Two Selected Units of Former Czechoslovakia in the Context of the Perspective of Positive Solutions. Int. J. Environ. Res. Public Health 2022, 19, 2480. [Google Scholar] [CrossRef]
- An, L.; Russell, D.M.; Mihalcea, R.; Bacon, E.; Huffman, S.; Resnicow, K. Online Search Behavior Related to COVID-19 Vaccines: Infodemiology Study. JMIR Infodemiol. 2021, 1, e32127. [Google Scholar] [CrossRef]
- Johns Hopkins University of Medicine. Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/region/romania (accessed on 12 February 2022).
- OECD. State of Health in the EU Romania Country Health Profile; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- Dima, A.; Jurcut, C.; Balaban, D.V.; Gheorghita, V.; Jurcut, R.; Dima, A.C.; Jinga, M. Physicians’ Experience with COVID-19 Vaccination: A Survey Study. Healthcare 2021, 9, 1746. [Google Scholar] [CrossRef]
- Dascalu, S. The successes and failures of the initial COVID-19 pandemic response in Romania. Front. Public Health 2020, 8, 344. [Google Scholar] [CrossRef]
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Chivu, R.D. Early COVID-19 Vaccination of Romanian Medical and Social Personnel. Vaccines 2021, 9, 1127. [Google Scholar] [CrossRef]
- Dascalu, S.; Geambasu, O.; Raiu, C.V.; Azoicai, D.; Popovici, E.D.; Apetrei, C. COVID-19 in Romania: What Went Wrong? Front. Public Health 2021, 9, 813941. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Wardle, J. The european health and behaviour survey the development of an international study in health psychology. Psychol. Health 1996, 11, 49–73. [Google Scholar] [CrossRef]
- Zung, W.W. A rating instrument for anxiety disorders. Psychosomatics 1971, 12, 371–379. [Google Scholar] [CrossRef]
- Ionescu, T.C.; Fetecau, B.I.; Boscaiu, V.; Tudose, C. Anxiety, Perceived Stress, and Resilience during the COVID-19 Pandemic: Population Estimates of Persons Presenting to a General Practitioner in Romania. Brain Sci. 2021, 11, 1541. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef]
- Robinson, E.; Jones, A.; Daly, M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 2021, 39, 2024–2034. [Google Scholar] [CrossRef]
- Palamenghi, L.; Barello, S.; Boccia, S.; Graffigna, G. Mistrust in biomedical research and vaccine hesitancy: The forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020, 35, 785–788. [Google Scholar] [CrossRef]
- Mouliou, D.S.; Pantazopoulos, I.; Gourgoulianis, K.I. Social Response to the Vaccine against COVID-19: The Underrated Power of Influence. J. Pers. Med. 2022, 12, 15. [Google Scholar] [CrossRef]
- Sonmezer, M.C.; Sahin, T.K.; Erul, E.; Ceylan, F.S.; Hamurcu, M.Y.; Morova, N.; Al, I.R.; Unal, S. Knowledge, Attitudes, and Perception towards COVID-19 Vaccination among the Adult Population: A Cross-Sectional Study in Turkey. Vaccines 2022, 10, 278. [Google Scholar] [CrossRef]
- Chaudhuri, K.; Chakrabarti, A.; Chandan, J.S.; Bandyopadhyay, S. COVID-19 vaccine hesitancy in the UK: A longitudinal household cross-sectional study. BMC Public Health 2022, 22, 104. [Google Scholar] [CrossRef]
- Petrovič, F.; Murgaš, F.; Králik, R. Happiness in Czechia during the COVID-19 Pandemic. Sustainability 2021, 13, 10826. [Google Scholar] [CrossRef]
- Mattia, G.; Anna, I.; Alice, B.; Riccardo, M.; Stefania, C.; Alessandra, G. Who Is Willing to Get Vaccinated? A Study into the Psychological, Socio-Demographic, and Cultural Determinants of COVID-19 Vaccination Intentions. Vaccines 2021, 9, 810. [Google Scholar] [CrossRef]
- Maciuszek, J.; Polak, M.; Stasiuk, K. Declared Intention (Not) to Be Vaccinated against COVID-19, and Actual Behavior—The Longitudinal Study in the Polish Sample. Vaccines 2022, 10, 147. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, D.; Malli, F.; Gourgoulianis, K.I. Registry Systems for COVID-19 Vaccines and Rate of Acceptability for Vaccination Before and After Availability of Vaccines in 12 Countries: A Narrative Review. Infect. Dis. Rep. 2022, 14, 121–133. [Google Scholar] [CrossRef]
- Dohle, S.; Wingen, T.; Schreiber, M. Acceptance and adoption of protective measures during the COVID-19 pandemic: The role of trust in politics and trust in science. Soc. Psychol. Bull. 2020, 15, 1–23. [Google Scholar] [CrossRef]
- Giambi, C.; Fabiani, M.; D’Ancona, F.; Ferrara, L.; Fiacchini, D.; Gallo, T.; Martinelli, D.; Pascucci, M.G.; Prato, R.; Filia, A. Parental vaccine hesitancy in Italy—Results from a national survey. Vaccine 2018, 36, 779–787. [Google Scholar] [CrossRef]
- Hromatko, I.; Tonković, M.; Vranic, A. Trust in Science, Perceived Vulnerability to Disease, and Adherence to Pharmacological and Non-pharmacological COVID-19 Recommendations. Front. Psychol. 2021, 12, 1425. [Google Scholar] [CrossRef]
- Kerr, J.R.; Schneider, C.R.; Recchia, G.; Dryhurst, S.; Sahlin, U.; Dufouil, C.; Arwidson, P.; Freeman, A.L.; van der Linden, S. Correlates of intended COVID-19 vaccine acceptance across time and countries: Results from a series of cross-sectional surveys. BMJ Open 2021, 11, e048025. [Google Scholar] [CrossRef]
- Plohl, N.; Musil, B. Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychol. Health Med. 2021, 26, 1–12. [Google Scholar] [CrossRef]
- Viswanath, K.; Bekalu, M.; Dhawan, D.; Pinnamaneni, R.; Lang, J.; McLoud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 2021, 21, 818. [Google Scholar] [CrossRef]
- Kosarkova, A.; Malinakova, K.; van Dijk, J.P.; Tavel, P. Vaccine Refusal in the Czech Republic Is Associated with Being Spiritual but Not Religiously Affiliated. Vaccines 2021, 9, 1157. [Google Scholar] [CrossRef] [PubMed]
- Gusar, I.; Konjevoda, S.; Babić, G.; Hnatešen, D.; Čebohin, M.; Orlandini, R.; Dželalija, B. Pre-Vaccination COVID-19 Vaccine Literacy in a Croatian Adult Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 7073. [Google Scholar] [CrossRef] [PubMed]
- Petravić, L.; Arh, R.; Gabrovec, T.; Jazbec, L.; Rupčić, N.; Starešinič, N.; Zorman, L.; Pretnar, A.; Srakar, A.; Zwitter, M.; et al. Factors Affecting Attitudes towards COVID-19 Vaccination: An Online Survey in Slovenia. Vaccines 2021, 9, 247. [Google Scholar] [CrossRef]
- Šiđanin, I.; Njegovan, B.R.; Sokolović, B. Students’ Views on Vaccination against COVID-19 Virus and Trust in Media Information about the Vaccine: The Case of Serbia. Vaccines 2021, 9, 1430. [Google Scholar] [CrossRef]
- European Commission. EU Digital COVID Certificate. Available online: https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/safe-covid-19-vaccines-europeans/eu-digital-covid-certificate_en (accessed on 12 February 2022).
- Matichescu, M.L.; Dragan, A.; Lucheș, D. Channels to West: Exploring the Migration Routes between Romania and France. Sustainability 2017, 9, 1861. [Google Scholar] [CrossRef] [Green Version]
- OECD. International Migration Outlook. 2020. Romania. Available online: https://www.oecd-ilibrary.org/sites/89085e47-en/index.html?itemId=/content/component/89085e47-en (accessed on 12 February 2022).
- Mocanu, I.; Mitrică, B.; Damian, N.; Popovici, A.; Persu, M.; Grigorescu, I.; Săgeată, R. Territorial characteristics of the vaccination process in Romania. evidence at a local level. Chem. Life Sci. Geosci. 2021, 23, 153–161. [Google Scholar]
- Wiemken, T.L.; Ramirez, J.A.; Carrico, R.M. Reasons for vaccine declination in healthy individuals attending an international vaccine and travel clinic. J. Refug. Glob. Health 2019, 2, 2. [Google Scholar]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. J. Refug. Glob. Health 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Zakar, R.; ul Momina, A.; Shahzad, S.; Hayee, M.; Shahzad, R.; Zakar, M.Z. COVID-19 Vaccination Hesitancy or Acceptance and Its Associated Factors: Findings from Post-Vaccination Cross-Sectional Survey from Punjab Pakistan. Int. J. Environ. Res. Public Health 2022, 19, 1305. [Google Scholar] [CrossRef]
- Berghea, F.; Berghea, C.E.; Abobului, M.; Vlad, V.M. Willingness to pay for a for a potential vaccine against SARS-CoV-2/COVID-19 among adult persons. Res. Square 2020, preprint. [Google Scholar] [CrossRef]
- Padureanu, V.; Bogdan, M.; Subtirelu, M.-S.; Padureanu, R.; Turcu-Stiolica, A.; Petrescu, F.; Dumitrescu, F.; Mititelu-Tartau, L. Perceptions of COVID-19 vaccination among healthcare professionals in Romania. Vaccines 2020, 22, 1204. [Google Scholar] [CrossRef]


| Main Concerns Associated with the Pandemic Context | n | Responses (%) | Respondents (%) |
|---|---|---|---|
| Fear of illness | 522 | 10.8% | 33.6% |
| Fear of death | 275 | 5.7% | 17.7% |
| Fear of illness of close people | 980 | 20.3% | 63.1% |
| Fear of death of close people | 747 | 15.5% | 48.1% |
| Concerns regarding the capacity of the health system | 836 | 17.3% | 53.9% |
| Fear that the basic protective measures (mask, disinfection of hands) are not enough | 256 | 5.3% | 16.5% |
| Concerns regarding the risk of becoming unemployed/economic impact | 330 | 6.8% | 21.3% |
| Social isolation | 689 | 14.3% | 44.4% |
| Social stigma associated with COVID-19 infection | 156 | 3.2% | 10.1% |
| Family conflicts | 32 | 0.7% | 2.1% |
| Total | 4823 | 100.0% |
| Sources of Information | n | Responses (%) | Respondents (%) |
|---|---|---|---|
| Traditional media (television, newspapers, and radio broadcasting) | 751 | 24.4% | 48.4% |
| The internet (blogs, news websites, and social media) | 923 | 30.0% | 59.5% |
| Friends, co-workers, and family members | 479 | 15.6% | 30.9% |
| Medical staff | 924 | 30.0% | 59.5% |
| Total | 3077 | 100.0% |
| The Main Reason for Refusal Is the Following | Responses (%) | Respondents (%) |
|---|---|---|
| I’m not afraid to get infected | 7.3% | 7.8% |
| There is not enough evidence of vaccine safety | 84.4% | 90.5% |
| I don’t think the COVID-19 disease exists | 5.9% | 6.3% |
| Others | 2.4% | 2.6% |
| Total | 100.0% | 107.2% |
| Socio-Demographic Characteristics | COVID-19 Vaccination Status % (n) | p Value | ||||
|---|---|---|---|---|---|---|
| Got Vaccinated | Want to Get Vaccinated | Don’t Want to Get Vaccinated | Contraindication to Vaccine | |||
| Gender | Female | 34.18% (416) | 27.36% (333) | 32.29% (393) | 6.16% (75) | <0.001 ** |
| Male | 57.61% (193) | 19.4% (65) | 19.4% (65) | 3.58% (12) | ||
| Age Groups | <25 | 49.4% (82) | 19.28% (32) | 27.11% (45) | 4.22% (7) | <0.001 ** |
| 25–34 | 28.85% (206) | 30.53% (218) | 33.75% (241) | 6.86% (49) | ||
| 35–44 | 36.98% (125) | 28.99% (98) | 28.99% (98) | 5.03% (17) | ||
| 45–54 | 47.33% (62) | 20.61% (27) | 26.72% (35) | 5.34% (7) | ||
| 55–64 | 54.81% (57) | 18.27% (19) | 23.08% (24) | 3.85% (4) | ||
| >65 | 77.78% (77) | 4.04% (4) | 15.15% (15) | 3.03% (3) | ||
| Educational level | Secondary school | 6.67% (2) | 40.00% (12) | 53.33% (16) | 0.00% (0) | <0.001 ** |
| Highschool | 30.05% (128) | 21.13% (90) | 43.43% (185) | 5.4% (23) | ||
| University graduate | 43.22% (252) | 26.07% (152) | 25.04% (146) | 5.66% (33) | ||
| Master graduate | 41.36% (170) | 29.2% (120) | 23.11% (95) | 6.33% (26) | ||
| Doctoral degree | 57.00% (57) | 23.00% (23) | 15.00% (15) | 5.00% (5) | ||
| Occupational status | Unemployed | 18.98% (75) | 31.40% (124) | 40.76% (161) | 8.86% (35) | <0.001 ** |
| Employed | 38.64% (296) | 26.89% (206) | 29.5% (226) | 4.96% (38) | ||
| Student | 70.47% (105) | 18.12% (27) | 8.05% (12) | 3.36% (5) | ||
| Retired | 71.09% (91) | 8.59% (11) | 16.41% (21) | 3.91% (5) | ||
| Freelancer | 37.17% (42) | 26.55% (30) | 33.63% (38) | 2.65% (3) | ||
| Family background | Wealthy | 68.18% (15) | 22.73% (5) | 4.55% (1) | 4.55% (1) | <0.001 ** |
| Quite well off | 43.39 (315) | 23.14% (168) | 27.82% (202) | 5.65% (41) | ||
| Not very well off | 35.19% (272) | 27.55% (213) | 31.57% (244) | 5.69% (44) | ||
| Quite poor | 23.33% (7) | 36.67% (11) | 36.67% (11) | 3.33% (1) | ||
| Being single | No | 37.65% (532) | 25.83% (365) | 30.64% (433) | 5.87% (83) | <0.001 ** |
| Yes | 55.4% (77) | 23.74% (33) | 17.99% (25) | 2.88% (4) | ||
| Living alone | No | 38.4% (520) | 25.33% (343) | 30.35% (411) | 5.91% (80) | =0.014 * |
| Yes | 44.95% (89) | 27.78% (55) | 23.74% (47) | 3.54% (7) | ||
| Being parents | No | 51.59% (211) | 23.96% (98) | 20.54% (84) | 3.91% (16) | <0.001 ** |
| Yes | 34.82% (398) | 26.25% (300) | 32.72% (374) | 6.21% (71) | ||
| Religious self-perception | Unreligious | 48.05% (259) | 27.27% (147) | 21.15% (114) | 3.53% (19) | <0.001 ** |
| Religious | 34.55% (350) | 24.78% (251) | 33.96% (344) | 6.71% (68) | ||
| Physical comorbidities(s) | No | 33.76% (370) | 28.38% (311) | 32.66% (358) | 5.2% (57) | <0.001 ** |
| Yes | 52.41% (239) | 19.08% (87) | 21.93% (100) | 6.58% (30) | ||
| Cardiovascular condition | No | 37.17% (536) | 26.63% (384) | 30.44% (439) | 5.76% (83) | <0.001 ** |
| Yes | 66.36% (73) | 12.73% (14) | 17.27% (19) | 3.64% (4) | ||
| Metabolic condition | No | 38.11% (574) | 26.29% (396) | 29.95% (451) | 5.64% (85) | <0.001 ** |
| Yes | 76.09% (35) | 4.35% (2) | 15.22% (7) | 4.35% (2) | ||
| Revenues (compared to pre pandemic period) | Significantly decreased | 18.39% (16) | 35.63% (31) | 39.08% (34) | 6.9% (6) | <0.001 ** |
| Decreased | 32.92% (106) | 26.4% (85) | 34.47% (111) | 6.21% (20) | ||
| Stagnated | 41.99% (406) | 24.61% (238) | 27.82% (269) | 5.58% (54) | ||
| Increased | 44.37% (67) | 25.83% (39) | 25.83% (39) | 3.97% (6) | ||
| Significantly Increased | 56.00% (14) | 20.00% (5) | 20.00% (5) | 4.00% (1) | ||
| Knowing someone with the COVID-19 infection | No | 28.79% (114) | 22.22% (88) | 40.91% (162) | 8.08% (32) | |
| Yes | 42.82% (495) | 26.82% (310) | 25.61% (296) | 4.76% (55) | <0.001 ** | |
| Lifestyle-Related Characteristics | COVID-19 Vaccination Status % (n) | p Value | ||||
|---|---|---|---|---|---|---|
| Got Vaccinated | Want to Get Vaccinated | Don’t Want to Get Vaccinated | Contraindication to Vaccine | |||
| BMI (kg/m2) | Underweight | 26.09% (24) | 28.26% (26) | 39.13% (36) | 6.52% (6) | =0.012 * |
| Normal range | 37.65% (305) | 26.54% (215) | 29.88% (242) | 5.93% (48) | ||
| Overweight | 42.04% (177) | 25.65% (108) | 28.50% (120) | 3.80% (16) | ||
| Obese | 44.60% (95) | 21.60% (46) | 26.29% (56) | 7.51% (16) | ||
| Self-assessment on weight | Very underweight | 50.00% (51) | 22.55% (23) | 21.57% (22) | 5.88% (6) | =0.009 * |
| Slightly underweight | 41.65% (227) | 24.77% (135) | 27.52% (150) | 6.06% (33) | ||
| About right | 38.04 (299) | 25.06% (197) | 31.42% (247) | 5.47% (43) | ||
| Slightly overweight | 27.18 (28) | 36.89% (38) | 31.07% (32) | 4.85% (5) | ||
| Very overweight | 26.67% (4) | 26.67% (4) | 46.67% (7) | 0.00% (0) | ||
| Desire to lose weight | No | 34.30% (189) | 25.95% (143) | 33.39% (184) | 6.35% (35) | =0.002 * |
| Yes | 41.96% (420) | 25.47% (255) | 27.37% (274) | 5.19% (52) | ||
| Dieting to lose weight | No | 37.77% (494) | 25.54% (334) | 30.89% (404) | 5.81% (76) | =0.002 * |
| Yes | 47.13% (115) | 26.23% (64) | 22.13% (54) | 4.51% (11) | ||
| Desire to increase physical activity | No | 30.26% (82) | 21.77% (59) | 41.33% (112) | 6.64% (18) | <0.001 ** |
| Yes | 41.17% (527) | 26.48% (339) | 27.03% (346) | 5.31% (68) | ||
| Duration of sleep in 24 h period | <7 h | 39.78% (144) | 27.07% (98) | 28.45% (103) | 4.70% (17) | <0.001 ** |
| 7–8 h | 41.82% (419) | 25.25% (253) | 27.84% (279) | 5.09% (51) | ||
| >8 h | 25.14% (45) | 24.02% (43) | 40.78% (73) | 10.06% (18) | ||
| Main Concerns Associated with the Pandemic Context | COVID-19 Vaccination Status % (n) | p Value | ||||
|---|---|---|---|---|---|---|
| Got Vaccinated | Want to Get Vaccinated | Don’t Want to Get Vaccinated | Contraindication to Vaccine | |||
| Fear of illness | No | 37.14% (384) | 22.92% (237) | 34.53% (357) | 5.42% (56) | <0.0001 ** |
| Yes | 43.44% (225) | 31.08% (161) | 19.50% (101) | 5.98% (31) | ||
| Fear of death | No | 38.49% (493) | 24.59% (315) | 31.69% (406) | 5.23% (67) | =0.050 * |
| Yes | 42.80% (116) | 30.63% (83) | 19.19% (52) | 7.38% (20) | ||
| Fear of illness of close people | No | 31.37% (181) | 20.62% (119) | 42.11% (243) | 5.89% (34) | <0.0001 ** |
| Yes | 43.90% (428) | 28.62% (279) | 22.05% (215) | 5.44% (53) | ||
| Fear of death of close people | No | 33.99% (275) | 21.38% (173) | 38.32% (310) | 6.30% (51) | <0.0001 ** |
| Yes | 44.95% (334) | 30.28% (225) | 19.92% (148) | 4.85% (36) | ||
| Concerns regarding the capacity of the health system | No | 35.97% (259) | 23.89% (172) | 35.00% (252) | 5.14% (37) | =0.0003 * |
| Yes | 42.07% (350) | 27.16% (226) | 24.76% (206) | 6.01% (50) | ||
| Fear that the basic protective measures are not enough | No | 38.80% (504) | 24.71% (321) | 31.25% (406) | 5.23% (68) | =0.177 |
| Yes | 41.50% (105) | 30.43% (77) | 20.55% (52) | 7.51% (19) | ||
| Concerns regarding the risk of becoming unemployed/ economic impact | No | 41.58% (509) | 24.75% (303) | 28.27% (346) | 5.39% (66) | =0.0001 ** |
| Yes | 30.49% (100) | 28.96% (95) | 34.15% (112) | 6.40% (21) | ||
| Social isolation | No | 39.54% (342) | 26.01% (225) | 29.02% (251) | 5.43% (47) | =0.599 |
| Yes | 38.86% (267) | 25.18% (173) | 30.13% (207) | 5.82% (40) | ||
| Social stigma associated with COVID-19 infection | No | 40.13% (561) | 24.75% (346) | 29.90% (418) | 5.22% (73) | =0.115 |
| Yes | 31.17% (48) | 33.77% (52) | 25.97% (40) | 9.09% (14) | ||
| Family conflicts | No | 39.67% (603) | 25.46% (387) | 29.34% (446) | 5.53% (84) | =0.031 * |
| Yes | 18.75% (6) | 34.38% (11) | 37.50% (12) | 9.38% (3) | ||
| Main Information Sources | COVID-19 Vaccination Status % (n) | Pearson’s r, p Value | ||||
|---|---|---|---|---|---|---|
| Got Vaccinated | Want to Get Vaccinated | Don’t Want to Get Vaccinated | Contraindication to Vaccine | |||
| Traditional media | No | 53.5% (326) | 47.7% (190) | 53.1% (243) | 50.6% (44) | 0.009, 0.714 |
| Yes | 46.5% (283) | 52.3% (208) | 46.9% (215) | 49.4% (43) | ||
| The internet | No | 40.9% (249) | 44.0% (175) | 37.3% (171) | 44.8% (39) | 0.013, 0.612 |
| Yes | 59.1% (360) | 56.0% (223) | 62.7% (287) | 55.2% (48) | ||
| Friends, co-workers, family members | No | 74.4% (453) | 64.1% (255) | 67.7% (310) | 66.7% (58) | 0.063 *, 0.013 |
| Yes | 25.6% (156) | 35.9% (143) | 32.3% (148) | 33.3% (29) | ||
| Medical staff | No | 28.2% (172) | 42.5% (169) | 57.9% (265) | 29.9% (26) | −0.186 **, 0.000 |
| Yes | 71.8% (437) | 57.5% (229) | 42.1% (193) | 70.1% (61) | ||
| COVID-19 Symptoms | Correlations | Anxiety Index | Psychological Symptoms of Anxiety | Somatic Symptoms of Anxiety |
|---|---|---|---|---|
| Dyspnoea | Pearson correlation | 0.205 ** | 0.127 * | 0.220 ** |
| Sig. (2-tailed) | 0.000 | 0.025 | 0.000 | |
| Fever | Pearson correlation | 0.044 | −0.008 | 0.065 |
| Sig. (2-tailed) | 0.441 | 0.894 | 0.255 | |
| Headaches | Pearson correlation | 0.146 ** | 0.120 * | 0.144 * |
| Sig. (2-tailed) | 0.009 | 0.034 | 0.011 | |
| Muscle aches | Pearson correlation | 0.126 * | 0.108 | 0.121 * |
| Sig. (2-tailed) | 0.026 | 0.057 | 0.033 | |
| Sore throats | Pearson correlation | 0.060 | −0.006 | 0.084 |
| Sig. (2-tailed) | 0.291 | 0.909 | 0.138 | |
| Loss of taste | Pearson correlation | 0.016 | 0.041 | 0.005 |
| Sig. (2-tailed) | 0.772 | 0.468 | 0.926 | |
| Loss of smell | Pearson correlation | −0.005 | −0.001 | −0.006 |
| Sig. (2-tailed) | 0.930 | 0.992 | 0.921 | |
| Fatigue | Pearson correlation | 0.165 ** | 0.148 ** | 0.160 ** |
| Sig. (2-tailed) | 0.003 | 0.009 | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ionescu, T.C.; Fetecau, B.I.; Giurgiuca, A.; Tudose, C. Acceptance and Factors Influencing Acceptance of COVID-19 Vaccine in a Romanian Population. J. Pers. Med. 2022, 12, 452. https://doi.org/10.3390/jpm12030452
Ionescu TC, Fetecau BI, Giurgiuca A, Tudose C. Acceptance and Factors Influencing Acceptance of COVID-19 Vaccine in a Romanian Population. Journal of Personalized Medicine. 2022; 12(3):452. https://doi.org/10.3390/jpm12030452
Chicago/Turabian StyleIonescu, Tiberiu Constantin, Bogdana Ioana Fetecau, Ana Giurgiuca, and Catalina Tudose. 2022. "Acceptance and Factors Influencing Acceptance of COVID-19 Vaccine in a Romanian Population" Journal of Personalized Medicine 12, no. 3: 452. https://doi.org/10.3390/jpm12030452
APA StyleIonescu, T. C., Fetecau, B. I., Giurgiuca, A., & Tudose, C. (2022). Acceptance and Factors Influencing Acceptance of COVID-19 Vaccine in a Romanian Population. Journal of Personalized Medicine, 12(3), 452. https://doi.org/10.3390/jpm12030452






