COVID-19 Vaccination Intention Associated with Behaviors towards Protection and Perceptions Regarding the Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Instruments
2.4. Data Analysis
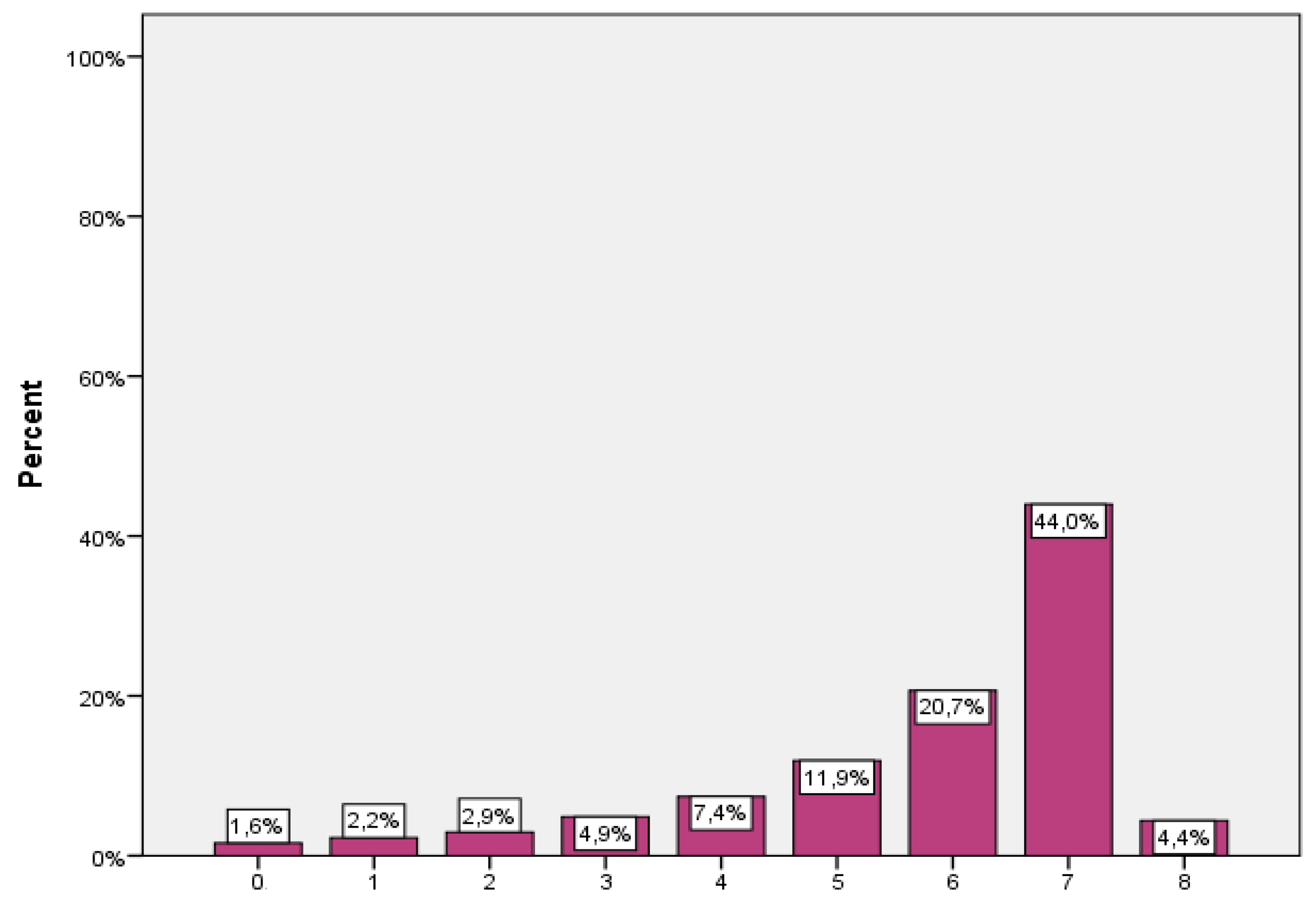
3. Results
3.1. Demographic Characteristics
3.2. Perceptions toward Protection and COVID-19 Vaccination Intention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report—66. 2019. Available online: https://www.who.int/docs/default-source/coronavirus/situation-reports/20200326-sitrep-66-covid-19.pdf?sfvrsn=9e5b8b48_2 (accessed on 26 March 2020).
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Barsade, S.G.; Coutifaris, C.G.; Pillemer, J. Emotional contagion in organizational life. Res. Organ. Behav. 2018, 38, 137–151. [Google Scholar] [CrossRef]
- Frijda, N.H. Impulsive action and motivation. Biol. Psychol. 2010, 84, 570–579. [Google Scholar] [CrossRef] [PubMed]
- de Vignemont, F.; Singer, T. The empathic brain: How, when and why? Trends Cogn. Sci. 2006, 10, 435–441. [Google Scholar] [CrossRef]
- EMA COVID-19 Vaccine Janssen: EMA Finds Possible Link to very Rare Cases of Unusual Blood Clots with Low Blood Platelets. Available online: https://www.ema.europa.eu/en/news/covid-19-vaccine-janssen-ema-finds-possible-link-very-rare-cases-unusual-blood-clots-low-blood (accessed on 8 February 2022).
- Cavaleri, M.; Sweeney, F.; Gonzalez-Quevedo, R.; Carr, M. Shaping EU Medicines Regulation in the Post COVID-19 Era; The Lancet Regional Health-Europe: Munich, Germany, 2021; Volume 9, p. 100192. ISSN 2666–7762. [Google Scholar] [CrossRef]
- Schaffer DeRoo, S.; Pudalov, N.J.; Fu, L.Y. Planning for a COVID-19 Vaccination Program. JAMA 2020, 323, 2458–2459. [Google Scholar] [CrossRef] [PubMed]
- Zampetakis, L.A.; Melas, C. The health belief model predicts vaccination intentions against COVID-19: A survey experiment approach. Appl. Psychol. Health Well Being 2021, 13, 469–484. [Google Scholar] [CrossRef] [PubMed]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccin Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Seale, H.; McLaws, M.-L.; Heywood, A.E.; Ward, K.F.; Lowbridge, C.P.; Van, D.; Gralton, J.; MacIntyre, C.R. The community’s attitude towards swine flu and pandemic influenza. Med. J. Aust. 2009, 191, 267–269. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Krumbholz, B.; Mavrouli, M.; Tseroni, M.; Gamaletsou, M.N.; Botsa, E.; Anastassopoulou, C.; Gikas, A.; Fournarakou, E.; Kavieri, M.; et al. A study of the evolution of the third COVID-19 pandemic wave in the Athens metropolitan area, Greece, through two cross-sectional seroepidemiological surveys: March, June 2021. J. Med. Virol. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dafogianni, C.; Pappa, D.; Koutelekos, I.; Mangoulia, P.; Ferentinou, E.; Margari, N. Stress, anxiety, and depression in nurses during COVID-19 pandemic: Evaluation of coping strategies. Int. J. Nurs. 2021, 8, 1–10. [Google Scholar]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/?gclid=EAIaIQobChMI2_CM6eDZ6gIVghh9Ch3nDQm1EAAYASAAEgLqwPD_BwE (accessed on 20 May 2021).
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 20 May 2021).
- Lurie, N.; Saville, M.; Hatchett, R.; Halton, J. Developing COVID-19 Vaccines at Pandemic Speed. N. Engl. J. Med. 2020, 382, 1969–1973. [Google Scholar] [CrossRef]
- Yang, Y.; Peng, F.; Wang, R.; Guan, K.; Jiang, T.; Xu, G.; Sun, J.; Chang, C. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020, 109, 102434. [Google Scholar] [CrossRef]
- World Health Organization. DRAFT Landscape of COVID-19 Candidate Vaccines—28 May 2021. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 28 May 2021).
- Eastwood, K.; Durrheim, D.N.; Jones, A.; Butler, M. Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Australian public. Med. J. Aust. 2010, 192, 33–36. [Google Scholar] [CrossRef]
- Maurer, J.; Harris, K.M.; Parker, A.M.; Lurie, N. Does receipt of seasonal influenza vaccine predict intention to receive novel H1N1 vaccine: Evidence from a nationally representative survey of U.S. adults. Vaccine 2009, 27, 5732–5734. [Google Scholar] [CrossRef][Green Version]
- Schwarzinger, M.; Flicoteaux, R.; Cortarenoda, S.; Obadia, Y.; Moatti, J.P. Low acceptability of A/H1N1 pandemic vaccination in French adult population: Did public health policy fuel public dissonance? PLoS ONE 2010, 5, e10199. [Google Scholar] [CrossRef]
- Maurer, J.; Uscher-Pines, L.; Harris, K.M. Perceived seriousness of seasonal and A(H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among U.S. adults: Does the source of information matter? Prev. Med. 2010, 51, 185–187. [Google Scholar] [CrossRef]
- Sypsa, V.; Livanios, T.; Psichogiou, M.; Malliori, M.; Tsiodras, S.; Nikolakopoulos, I.; Hatzakis, A.A. Public perceptions in relation to intention to receive pandemic influenza vaccination in a random population sample: Evidence from a cross-sectional telephone survey. Eur. Surveill. 2009, 14, 19437. [Google Scholar] [CrossRef]
- Raude, J.; Caille-Brillet, A.L.; Setbon, M. The 2009 pandemic H1N1 influenza vaccination in France: Who accepted to receive the vaccine and why? PLoS Curr. 2010, 2, RRN1188. [Google Scholar] [CrossRef] [PubMed]
- Rubin, G.J.; Potts, H.; Michie, S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: Results from 36 national telephone surveys in the UK. Health Technol. Assess. 2010, 14, 183–266. [Google Scholar] [CrossRef] [PubMed]
- Seale, H.; Heywood, A.E.; McLaws, M.L.; Ward, K.F.; Lowbridge, C.P.; Van, D.; MacIntyre, C.R. Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect. Dis. 2010, 10, 99. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Henningsen, K.H.; Brehaut, J.C.; Hoe, E.; Wilson, K. Acceptance of a pandemic influenza vaccine: A systematic review of surveys of the general public. Infect. Drug Resist. 2011, 4, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Henrich, N.; Holmes, B. The public’s acceptance of novel vaccines during a pandemic: A focus group study and its application to influenza H1N1. Emerg Health Threat J. 2009, 2, e8. [Google Scholar] [CrossRef]
- Lau, J.T.F.; Yeung, N.C.; Choi, K.C.; Cheng, M.Y.; Tsui, H.; Griffiths, S. Factors in association with acceptability of A/H1N1 vaccination during the influenza A/H1N1 pandemic phase in the Hong Kong general population. Vaccine 2010, 28, 4632–4637. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Reuters. China to Provide COVID-19 Vaccines Free of Charge–Official. Available online: https://www.reuters.com/article/uk-health-coronavirus-china-vaccine-idUKKBN29E04Z (accessed on 10 December 2021).
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Determann, D.; de Bekker-Grob, E.W.; French, J.; Voeten, H.A.; Richardus, J.H.; Das, E.; Korfage, I.J. Future pandemics and vaccination: Public opinion and attitudes across three European countries. Vaccine 2016, 34, 803–808. [Google Scholar] [CrossRef]
- Chirico, F.; Nucera, G.; Magnavita, N. COVID-19: Protecting healthcare workers is a priority. Infect. Control Hosp. Epidemiol. 2020, 41, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Dedoukou, X.; Tseroni, M.; Tsonou, P.; Raftopoulos, V.; Papadima, K.; Mouratidou, E.; Poufta, S.; Panagiotakopoulos, G.; Hatzigeorgiou, D.; et al. SARS-CoV-2 infection in healthcare personnel with high-risk occupational exposure: Evaluation of seven-day exclusion from work policy. Clin Infect Dis. 2020, 71, ciaa888. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross-sectional survey. J. Hosp. Infect. 2020, 108, 168–173. [Google Scholar] [CrossRef]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; El-Fatah Abdo, S.A. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.L.; Gerolamo, A.M.; Marino, M.A.; Hanson-Zalot, M.E.; Pogorzelska-Maziarz, M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs. Outlokk. 2021, 69, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Earnshaw, V.A.; Eaton, L.A.; Kalichman, S.C.; Brousseau, N.M.; Hill, E.C.; Fox, A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Trans. Behav. Med. 2020, 10, 850–856. [Google Scholar] [CrossRef]
- Neuman-Böhme, S.; Varghese, N.E.; Sabat, I. Once we have it, it will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High rates of CVID-19 vaccine hesitancy and its association with conspiracy beliefs: A study in Jordan and Kuwait among other Arab countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Chevallier, C.; Hacquin, A.S.; Mercier, H. COVID-19 vaccine hesitancy: Shortening the last mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef] [PubMed]
| n (%) | ||
|---|---|---|
| Gender | Male | 1193 (32.3) |
| Female | 2498 (67.7) | |
| Age, mean (SD) | 29.4 (12.6) | |
| Nationality | Greek | 3566 (96.5) |
| Other | 110 (3.0) | |
| Prefer not to say | 18 (0.5) | |
| Religion | Christian Orthodox | 2821 (76.8) |
| No religion | 329 (9.0) | |
| Other | 90 (2.4) | |
| Don’t know | 1 (0.0) | |
| Prefer not to say | 432 (11.8) | |
| Educational level | Primary school | 1 (0.0) |
| High school | 1802 (48.8) | |
| University | 1155 (31.3) | |
| MSc degree | 661 (17.9) | |
| Prefer not to say | 70 (1.9) | |
| Key worker | 1395 (37.7) | |
| Annual income | EUR ≤ 10,000 | 869 (24.1) |
| EUR 10,001–20,000 | 783 (21.7) | |
| EUR 20,001–30,000 | 240 (6.6) | |
| EUR 30,001–40,000 | 104 (2.9) | |
| EUR 40,001–50,000 | 55 (1.5) | |
| EUR 50,001–75,000 | 35 (1) | |
| >75,000 | 28 (0.8) | |
| Don’t know | 723 (20.0) | |
| Prefer not to say | 776 (21.5) | |
| Number of people in household | 1 | 377 (10.2) |
| 2 | 684 (18.6) | |
| 3–4 | 2114 (57.4) | |
| 5–6 | 428 (11.6) | |
| >7 | 37 (1) | |
| Prefer not to say | 43 (1.2) | |
| Residence | Athens/Attica | 2569 (70.3) |
| Outside Athens | 1036 (28.4) | |
| Abroad | 48 (1.3) | |
| Flu vaccination last winter | No | 2665 (72.2) |
| Yes | 909 (24.6) | |
| Don’t know | 104 (2.8) | |
| Prefer not to say | 15 (0.4) | |
| Item | Level | n (%) |
|---|---|---|
| To what extent do you think COVID-19 poses a risk to people in Greece? | Major risk | 1090 (29.5) |
| Significant risk | 1601 (43.3) | |
| Moderate risk | 733 (19.8) | |
| Minor risk | 220 (6.0) | |
| No risk at all | 26 (0.7) | |
| Don’t know | 25 (0.7) | |
| To what extent do you think COVID-19 poses a risk to you personally? | Major risk | 525 (14.2) |
| Significant risk | 884 (23.9) | |
| Moderate risk | 1022 (27.7) | |
| Minor risk | 997 (27.0) | |
| No risk at all | 231 (6.3) | |
| Don’t know | 37 (1.0) | |
| Do you believe you have had, or currently have, COVID-19? * | Definitely | 99 (2.7) |
| Probably | 269 (7.3) | |
| Probably not | 1371 (37.1) | |
| Definitely not | 1448 (39.2) | |
| Don’t know | 504 (13.6) | |
| Prefer not to say | 5 (0.1) | |
| Do you personally know anyone (excluding yourself) who has had COVID-19? | No | 1076 (29.2) |
| Yes | 2608 (70.6) | |
| Prefer not to say | 9 (0.2) | |
| As far as you know, would your employer want you to have the COVID-19 vaccination? * | No | 184 (5.1) |
| Yes | 1315 (36.4) | |
| Don’t know | 1634 (45.3) | |
| Prefer not to say | 477 (13.2) | |
| As far as you know, is there currently a widely available vaccination to protect against COVID-19? * | No | 1550 (42.3) |
| Yes | 1180 (32.2) | |
| Don’t know | 829 (22.6) | |
| Prefer not to say | 107 (2.9) |
| n (%) | |
|---|---|
| Washed my hands with soap and water more often than usual | 3112 (84.2) |
| Used alcoholic hand gel more than usual | 3013 (81.6) |
| Increased the amount I clean or disinfect things that I might touch, such as door knobs | 2645 (71.6) |
| Kept away from crowded places generally | 3343 (90.5) |
| Reduced the amount I use public transport | 3180 (86.1) |
| Deliberately cancelled or postponed a social event, such as meeting friends, eating out, or going to a sports event | 2893 (78.3) |
| Reduced the amount I go into shops | 2980 (80.7) |
| Kept one or more of my children out of school or preschool | 226 (42.6) |
| Undertook ≥ 1 behavioral change due to the COVID-19 pandemic | 3637 (98.4) |
| Number of behavioral changes due to the COVID-19 pandemic, mean (SD) | 5.9 (1.7) |
| Unstandardized Coefficient β | Standardized Coefficient β | 99% CI for β | p Value | |
|---|---|---|---|---|
| Gender (reference: Men) | 0.20 | 0.05 | 0.05 to 0.36 | 0.001 * |
| Age | 0.01 | 0.07 | 0.00 to 0.02 | 0.001 * |
| Nationality (reference: Greek) | −0.79 | −0.07 | −1.23 to −0.34 | <0.001 ** |
| Key worker | −0.02 | −0.01 | −0.18 to 0.14 | 0.738 |
| Religion (reference: No religion) | ||||
| Christian Orthodox | −0.09 | −0.02 | −0.32 to 0.15 | 0.343 |
| Other | −0.01 | 0.00 | −0.51 to 0.48 | 0.940 |
| Number of people in household | 0.09 | 0.05 | 0.01 to 0.18 | 0.005 * |
| Residence (reference: Athens/Attica) | ||||
| Outside Athens | 0.07 | 0.02 | −0.09 to 0.23 | 0.267 |
| Abroad | −0.64 | −0.04 | −1.26 to −0.02 | 0.008 * |
| Flu vaccination last winter (reference: No) | 0.10 | 0.03 | −0.07 to 0.28 | 0.129 |
| To what extent do you think COVID-19 poses a risk to people in Greece? (reference: Major risk) | ||||
| No risk at all/minor risk | −2.39 | −0.34 | −2.75 to −2.03 | <0.001 ** |
| Moderate risk | −1.09 | −0.25 | −1.35 to −0.83 | <0.001 ** |
| Significant risk | −0.33 | −0.09 | −0.52 to −0.13 | <0.001 ** |
| To what extent do you think COVID-19 poses a risk to you personally? (reference: Major risk) | ||||
| No risk at all/minor risk | −0.57 | −0.15 | −0.87 to −0.27 | <0.001 ** |
| Moderate risk | −0.09 | −0.02 | −0.36 to 0.18 | 0.382 |
| Significant risk | 0.06 | 0.02 | −0.18 to 0.31 | 0.495 |
| Do you personally know anyone (excluding yourself) who has had COVID-19? (reference: No) | 0.24 | 0.06 | 0.08 to 0.40 | <0.001 ** |
| Unstandardized Coefficient β | Standardized Coefficient β | 99% CI for β | p Value | |
|---|---|---|---|---|
| Gender (reference: Men) | −0.55 | −0.07 | −0.88 to −0.23 | <0.001 ** |
| Age | −0.01 | −0.02 | −0.02 to 0.01 | 0.294 |
| Nationality (reference: Greek) | 0.71 | 0.03 | −0.22 to 1.63 | 0.050 |
| Key worker | −0.06 | −0.01 | −0.39 to 0.26 | 0.616 |
| Religion (reference: No religion | ||||
| Christian Orthodox | −1.35 | −0.13 | −1.83 to −0.86 | <0.001 ** |
| Other | −0.58 | −0.03 | −1.6 to 0.44 | 0.141 |
| Number of people in household | −0.01 | 0.00 | −0.19 to 0.17 | 0.914 |
| Residence (reference: Athens / Attica) | ||||
| Outside Athens | 0.36 | 0.05 | 0.03 to 0.69 | 0.005 * |
| Abroad | 0.28 | 0.01 | −1.01 to 1.57 | 0.576 |
| Flu vaccination last winter (reference: No) | 1.17 | 0.14 | 0.81 to 1.53 | <0.001 ** |
| To what extent do you think COVID-19 poses a risk to people in Greece? (reference: Major risk) | ||||
| No risk at all/minor risk | −4.96 | −0.34 | −5.72 to −4.2 | <0.001 ** |
| Moderate risk | −3.14 | −0.34 | −3.67 to −2.6 | <0.001 ** |
| Significant risk | −1.48 | −0.20 | −1.88 to −1.07 | <0.001 ** |
| To what extent do you think COVID-19 poses a risk to you personally? (reference: Major risk) | ||||
| No risk at all/minor risk | −1.04 | −0.13 | −1.66 to −0.42 | <0.001 ** |
| Moderate risk | −0.80 | −0.10 | −1.36 to −0.24 | <0.001 ** |
| Significant risk | −0.44 | −0.05 | −0.95 to 0.07 | 0.025 |
| Do you personally know anyone (excluding yourself) who has had COVID-19? (reference: No) | 0.44 | 0.05 | 0.1 to 0.78 | 0.001 * |
| Have undertaken at least one behavioral change due to COVID-19 | 1.39 | 0.05 | 0.11 to 2.68 | 0.005 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dafogianni, C.; Mangoulia, P.; Pappa, D.; Xanthopoulou, P.; Koutelekos, I.; Zografakis-Sfakianakis, M.; Ferentinou, E.; Fountouki, A.; Drakopoulou, M.; Giga, A.; et al. COVID-19 Vaccination Intention Associated with Behaviors towards Protection and Perceptions Regarding the Pandemic. J. Pers. Med. 2022, 12, 295. https://doi.org/10.3390/jpm12020295
Dafogianni C, Mangoulia P, Pappa D, Xanthopoulou P, Koutelekos I, Zografakis-Sfakianakis M, Ferentinou E, Fountouki A, Drakopoulou M, Giga A, et al. COVID-19 Vaccination Intention Associated with Behaviors towards Protection and Perceptions Regarding the Pandemic. Journal of Personalized Medicine. 2022; 12(2):295. https://doi.org/10.3390/jpm12020295
Chicago/Turabian StyleDafogianni, Chrysoula, Polyxeni Mangoulia, Despoina Pappa, Panagiota Xanthopoulou, Ioannis Koutelekos, Mixalis Zografakis-Sfakianakis, Eftychia Ferentinou, Antigoni Fountouki, Marianna Drakopoulou, Anna Giga, and et al. 2022. "COVID-19 Vaccination Intention Associated with Behaviors towards Protection and Perceptions Regarding the Pandemic" Journal of Personalized Medicine 12, no. 2: 295. https://doi.org/10.3390/jpm12020295
APA StyleDafogianni, C., Mangoulia, P., Pappa, D., Xanthopoulou, P., Koutelekos, I., Zografakis-Sfakianakis, M., Ferentinou, E., Fountouki, A., Drakopoulou, M., Giga, A., Anastasiou, N., Margari, N., & Fasoi, G. (2022). COVID-19 Vaccination Intention Associated with Behaviors towards Protection and Perceptions Regarding the Pandemic. Journal of Personalized Medicine, 12(2), 295. https://doi.org/10.3390/jpm12020295








