Clinical Utility and Validation of the Krakow DCM Risk Score—A Prognostic Model Dedicated to Dilated Cardiomyopathy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Clinical Follow-Up and Endpoint Definition
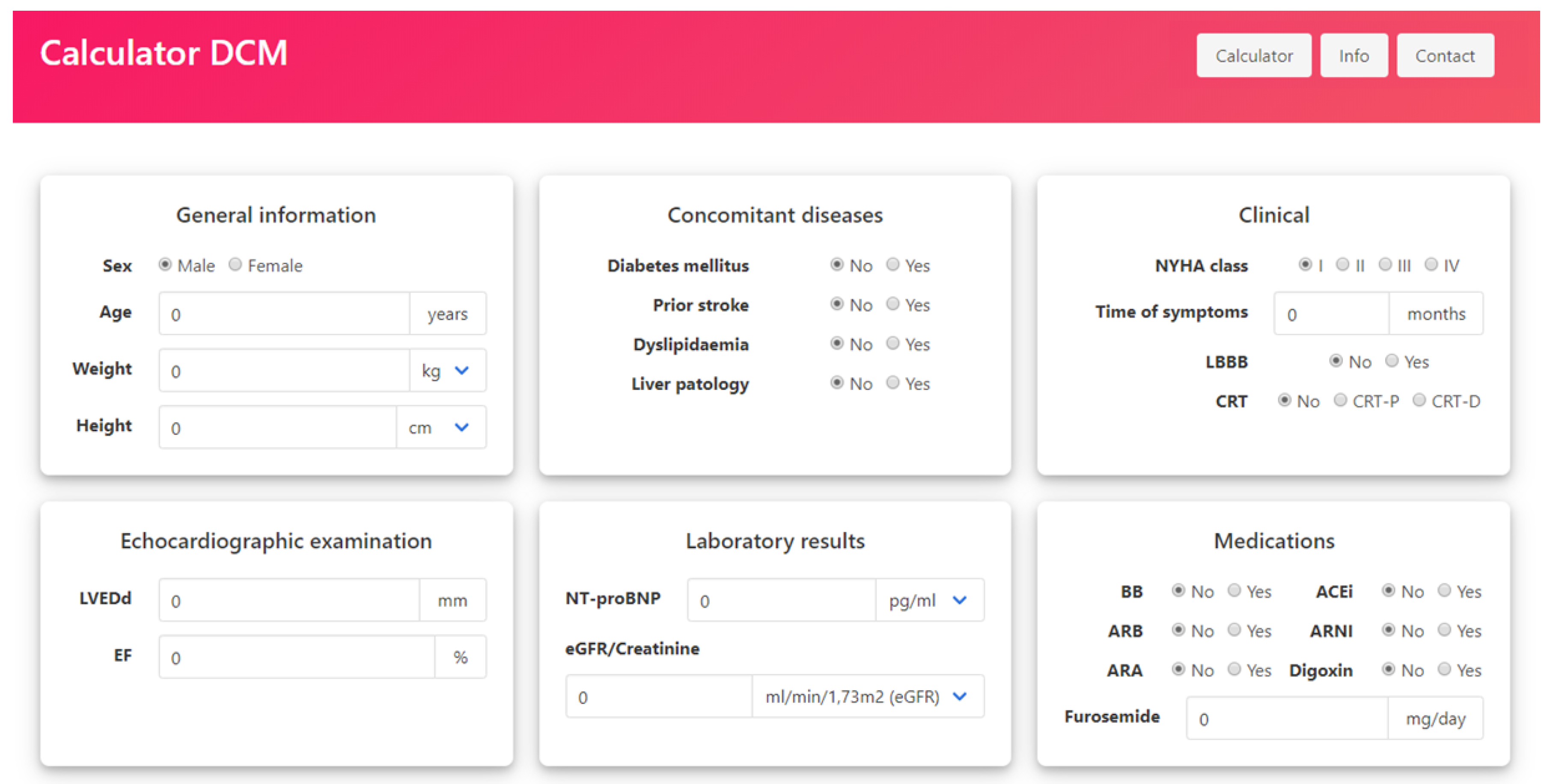
2.3. Structure of the Krakow DCM Risk Score
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Performance of Krakow DCM Risk Score
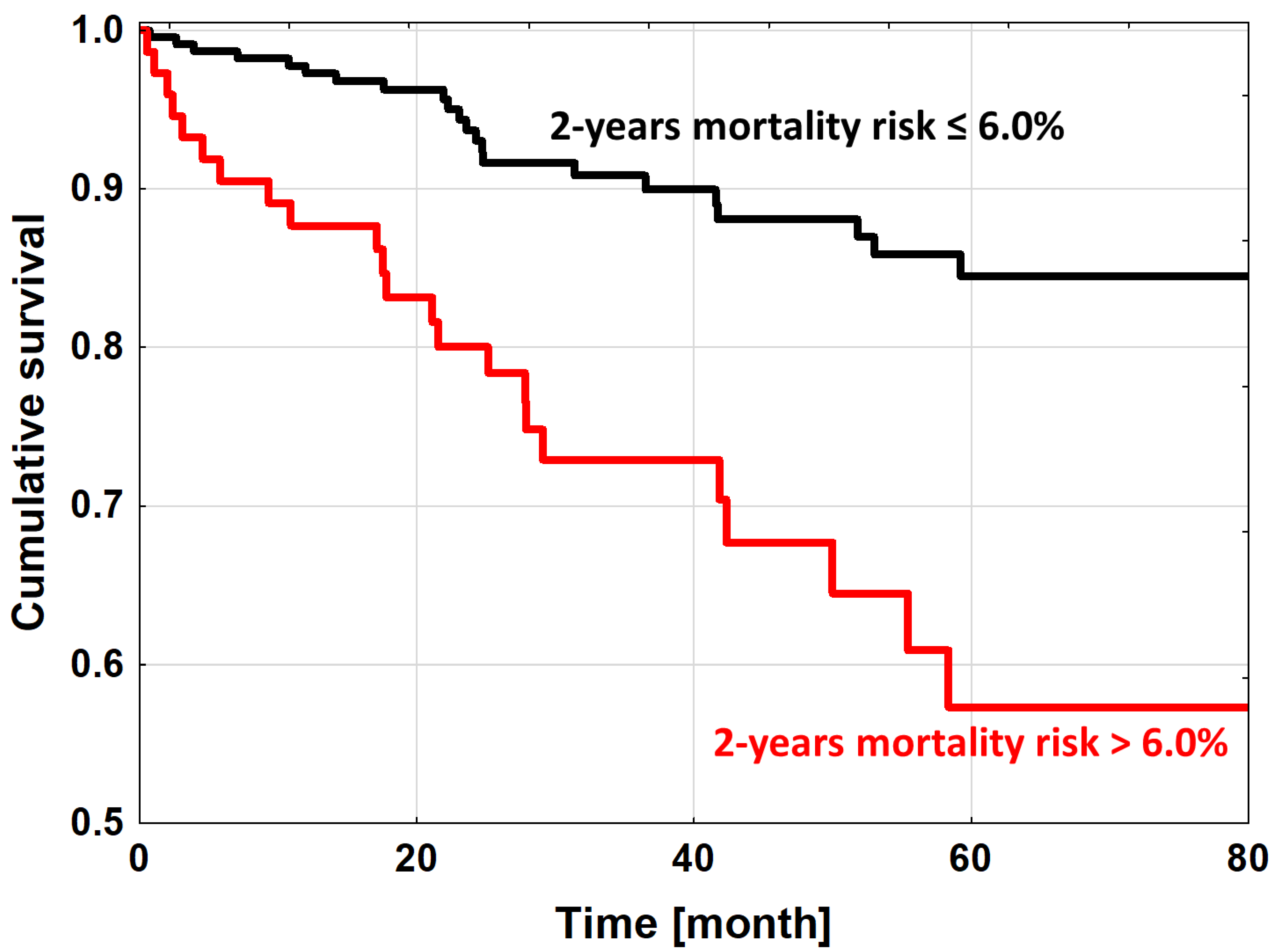
3.3. High Mortality Risk DCM Patients
4. Discussion
4.1. Prognostic Models in DCM
4.2. Krakow DCM Risk Score Performance
4.3. Identification of High Mortality DCM Patients
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Elliott, P.; Andersson, B.; Arbustini, E.; Bilinska, Z.; Cecchi, F.; Charron, P.; Dubourg, O.; Kühl, U.; Maisch, B.; McKenna, W.J.; et al. Classification of the cardiomyopathies: A position statement from the european society of cardiology working group on myocardial and pericardial diseases. Eur. Heart J. 2008, 29, 270–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinto, Y.M.; Elliott, P.M.; Arbustini, E.; Adler, Y.; Anastasakis, A.; Böhm, M.; Duboc, D.; Gimeno, J.; De Groote, P.; Imazio, M.; et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: A position statement of the ESC working group on myocardial and pericardial diseases. Eur. Heart J. 2016, 37, 1850–1858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Zschirnt, M.; Thul, J.; Akintürk, H.; Valeske, K.; Schranz, D.; Skrzypek, S.; Müller, M.; Jux, C.; Hahn, A.; Rupp, S. Aetiology and 30-Year Long-Term Outcome of Children with Cardiomyopathy Necessitating Heart Transplantation. J. Pers. Med. 2020, 10, 251. [Google Scholar] [CrossRef]
- Maron, B.J.; Towbin, J.A.; Thiene, G.; Antzelevitch, C.; Corrado, D.; Arnett, D.; Moss, A.J.; Seidman, C.E.; Young, J.B. Contemporary Definitions and Classification of the Cardiomyopathies: An American Heart Association Scientific Statement From the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functio. Circulation 2006, 113, 1807–1816. [Google Scholar] [CrossRef] [Green Version]
- 6. Lupón, J.; Simpson, J.; McMurray, J.J.; De Antonio, M.; Vila-Domènech, J.S.; Subirana, I.; Barallat, J.; Moliner, P.; Domingo, M.; Zamora, E.; et al. Barcelona Bio-HF Calculator Version 2.0: Incorporation of angiotensin II receptor blocker neprilysin inhibitor (ARNI) and risk for heart failure hospitalization. Eur. J. Heart Fail. 2017, 20, 938–940. [Google Scholar] [CrossRef]
- Pocock, S.J.; Wang, D.; Pfeffer, M.A.; Yusuf, S.; Mcmurray, J.; Swedberg, K.B.; Östergren, J.; Michelson, E.L.; Pieper, K.S.; Granger, C.B. Predictors of mortality and morbidity in patients with chronic heart failure. Eur. Heart J. 2005, 27, 65–75. [Google Scholar] [CrossRef] [Green Version]
- Pocock, S.J.; Ariti, C.A.; Mcmurray, J.; Maggioni, A.P.; Køber, L.; Squire, I.B.; Swedberg, K.; Dobson, J.; Poppe, K.K.; Whalley, G.; et al. Predicting survival in heart failure: A risk score based on 39 372 patients from 30 studies. Eur. Heart J. 2012, 34, 1404–1413. [Google Scholar] [CrossRef]
- Collier, T.J.; Pocock, S.J.; Mcmurray, J.; Zannad, F.; Krum, H.; Van Veldhuisen, D.J.; Swedberg, K.; Shi, H.; Vincent, J.; Pitt, B. The impact of eplerenone at different levels of risk in patients with systolic heart failure and mild symptoms: Insight from a novel risk score for prognosis derived from the EMPHASIS-HF trial. Eur. Heart J. 2013, 34, 2823–2829. [Google Scholar] [CrossRef] [Green Version]
- Levy, W.C.; Mozaffarian, D.; Linker, D.T.; Sutradhar, S.C.; Anker, S.D.; Cropp, A.B.; Anand, I.; Maggioni, A.P.; Burton, P.; Sullivan, M.D.; et al. The Seattle Heart Failure Model. Circulation 2006, 113, 1424–1433. [Google Scholar] [CrossRef]
- Vazquez, R.; Bayes-Genis, A.; Cygankiewicz, I.; Pascual-Figal, D.; Grigorian-Shamagian, L.; Pavon, R.; Gonzalez-Juanatey, J.R.; Cubero, J.M.; Pastor, L.; Ordonez-Llanos, J.; et al. The MUSIC Risk score: A simple method for predicting mortality in ambulatory patients with chronic heart failure. Eur. Heart J. 2009, 30, 1088–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miura, K.; Matsumori, A.; Nasermoaddeli, A.; Soyama, Y.; Morikawa, Y.; Sakurai, M.; Kitabatake, A.; Nagai, M.; Inaba, Y.; Nakagawa, H. Prognosis and Prognostic Factors in Patients With Idiopathic Dilated Cardiomyopathy in Japan Results From a Nationwide Study. Circ. J. 2008, 72, 343–348. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Marcus, P.; Núñez, J.; Núñez, E.; Sanchis, J.; Levy, W.C. Validity of the Seattle Heart Failure Model after heart failure hospitalization. ESC Heart Fail. 2019, 6, 509–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doumouras, B.S.; Lee, D.S.; Levy, W.C.; Alba, A.C. An Appraisal of Biomarker-Based Risk-Scoring Models in Chronic Heart Failure: Which One Is Best? Curr. Heart Fail. Rep. 2018, 15, 24–36. [Google Scholar] [CrossRef]
- Nguyen, L.S.; Coutance, G.; Ouldamar, S.; Zahr, N.; Brechot, N.; Galeone, A.; Bougle, A.; Lebreton, G.; Leprince, P.; Varnous, S. Performance of existing risk scores around heart transplantation: Validation study in a 4-year cohort. Transpl. Int. 2018, 31, 520–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iorio, A.; Senni, M.; Barbati, G.; Greene, S.J.; Poli, S.; Zambon, E.; Di Nora, C.; Cioffi, G.; Tarantini, L.; Gavazzi, A.; et al. Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: A community-based study. Eur. J. Heart Fail. 2018, 20, 1257–1266. [Google Scholar] [CrossRef] [Green Version]
- Dziewięcka, E.; Rubiś, P. Mortality risk assessment in dilated cardiomyopathy: The Krakow DCM Risk Score. Kardiol. Pol. 2021, 79, 215–216. [Google Scholar] [CrossRef]
- Dziewięcka, E.; Gliniak, M.; Winiarczyk, M.; Karapetyan, A.; Wiśniowska-Śmiałek, S.; Karabinowska, A.; Dziewięcki, M.; Podolec, P.; Rubiś, P. Mortality risk in dilated cardiomyopathy: The accuracy of heart failure prognostic models and dilated cardiomyopathy-tailored prognostic model. ESC Heart Fail. 2020, 7, 2455–2467. [Google Scholar] [CrossRef]
- Donal, E.; Delgado, V.; Bucciarelli-Ducci, C.; Galli, E.; Haugaa, K.H.; Charron, P.; Voigt, J.U.; Cardim, N.; Masci, P.G.; 2016–2018 EACVI Scientific Documents Committee; et al. Multimodality imaging in the diagnosis, risk stratification, and management of patients with dilated cardiomyopathies: An expert consensus document from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1075–1093. [Google Scholar] [CrossRef] [Green Version]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef]
- Rubiś, P. The Diagnostic Work-up of Genetic and Inflammatory Dilated Cardiomyopathy. E-J. Cardiol. Pract. 2015, 13, 19. [Google Scholar]
- 22. Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. -Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef] [PubMed]
- Halliday, B.P.; Gulati, A.; Ali, A.; Newsome, S.; Lota, A.; Tayal, U.; Vassiliou, V.S.; Arzanauskaite, M.; Izgi, C.; Krishnathasan, K.; et al. Sex- and age-based differences in the natural history and outcome of dilated cardiomyopathy. Eur. J. Heart Fail. 2018, 20, 1392–1400. [Google Scholar] [CrossRef] [Green Version]
- Karatolios, K.; Holzendorf, V.; Richter, A.; Schieffer, B.; Pankuweit, S.; Competence Network Heart Failure Germany. Long-term outcome and predictors of outcome in patients with non-ischemic dilated cardiomyopathy. Int. J. Cardiol. 2016, 220, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Gulati, A.; Ismail, T.F.; Jabbour, A.; Alpendurada, F.; Guha, K.; Ismail, N.A.; Raza, S.; Khwaja, J.; Brown, T.D.; Morarji, K.; et al. The Prevalence and Prognostic Significance of Right Ventricular Systolic Dysfunction in Nonischemic Dilated Cardiomyopathy. Circulation 2013, 128, 1623–1633. [Google Scholar] [CrossRef] [Green Version]
- Ertaş, G.; Kozdağ, G.; Emre, E.; Vural, A.; Akbulut, T.; Ural, D.; Göktekin, Ö. Renal function has an effect on cardiovascular mortality in patients with dilated cardiomyopathy. J. Cardiovasc. Med. 2012, 13, 554–558. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, Y.; Inomata, T.; Iida, Y.; Iwamoto-Ishida, M.; Nabeta, T.; Ishii, S.; Sato, T.; Yanagisawa, T.; Mizutani, T.; Naruke, T.; et al. Time course of left ventricular reverse remodeling in response to pharmacotherapy: Clinical implication for heart failure prognosis in patients with idiopathic dilated cardiomyopathy. Heart Vessel. 2015, 31, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Merlo, M.; Pyxaras, S.A.; Pinamonti, B.; Barbati, G.; Di Lenarda, A.; Sinagra, G. Prevalence and Prognostic Significance of Left Ventricular Reverse Remodeling in Dilated Cardiomyopathy Receiving Tailored Medical Treatment. J. Am. Coll. Cardiol. 2011, 57, 1468–1476. [Google Scholar] [CrossRef] [Green Version]
- Marume, K.; Noguchi, T.; Tateishi, E.; Morita, Y.; Kamakura, T.; Ishibashi, K.; Noda, T.; Miura, H.; Nishimura, K.; Nakai, M.; et al. Mortality and Sudden Cardiac Death Risk Stratification Using the Noninvasive Combination of Wide QRS Duration and Late Gadolinium Enhancement in Idiopathic Dilated Cardiomyopathy. Circ. Arrhythmia Electrophysiol. 2018, 11, e006233. [Google Scholar] [CrossRef]
- Sinagra, G.; Iorio, A.; Merlo, M.; Cannatà, A.; Stolfo, D.; Zambon, E.; Di Nora, C.; Paolillo, S.; Barbati, G.; Berton, E.; et al. Prognostic value of cardiopulmonary exercise testing in Idiopathic Dilated Cardiomyopathy. Int. J. Cardiol. 2016, 223, 596–603. [Google Scholar] [CrossRef]
- Dziewięcka, E.; Gliniak, M.; Winiarczyk, M.; Karapetyan, A.; Wiśniowska-Śmiałek, S.; Karabinowska, A.; Holcman, K.; Kostkiewicz, M.; Hlawaty, M.; Leśniak-Sobelga, A.; et al. The burden of atrial fibrillation and its prognostic value in patients with dilated cardiomyopathy. Kardiol. Pol. 2020, 78, 37–44. [Google Scholar] [CrossRef] [Green Version]
- Dziewięcka, E.; Wiśniowska-Śmiałek, S.; Karabinowska, A.; Holcman, K.; Gliniak, M.; Winiarczyk, M.; Karapetyan, A.; Kaciczak, M.; Podolec, P.; Kostkiewicz, M.; et al. Relationships between Pulmonary Hypertension Risk, Clinical Profiles, and Outcomes in Dilated Cardiomyopathy. J. Clin. Med. 2020, 9, 1660. [Google Scholar] [CrossRef] [PubMed]
- Zegkos, T.; Tziomalos, G.; Parcharidou, D.; Ntelios, D.; Papanastasiou, C.A.; Karagiannidis, E.; Gossios, T.; Rouskas, P.; Katranas, S.; Paraskevaidis, S.; et al. Validation of the new American College of Cardiology/American Heart Association Guidelines for the risk stratification of sudden cardiac death in a large Mediterranean cohort with Hypertrophic Cardiomyopathy. Hell. J. Cardiol. 2022, 63, 15–21. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, C.; Jichi, F.; Pavlou, M.; Monserrat, L.; Anastasakis, A.; Rapezzi, C.; Biagini, E.; Gimeno, J.R.; Limongelli, G.; McKenna, W.J.; et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM Risk-SCD). Eur. Heart J. 2013, 35, 2010–2020. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.A.A.; Lucas, J.E.; Pieper, K.S.; Bassand, J.-P.; Camm, J.; Fitzmaurice, D.A.; Goldhaber, S.Z.; Goto, S.; Haas, S.; Hacke, W.; et al. Improved risk stratification of patients with atrial fibrillation: An integrated GARFIELD-AF tool for the prediction of mortality, stroke and bleed in patients with and without anticoagulation. BMJ Open 2017, 7, e017157. [Google Scholar] [CrossRef] [Green Version]
- Vriesendorp, P.A.; Schinkel, A.F.; Liebregts, M.; Theuns, D.A.; van Cleemput, J.; Cate, F.J.T.; Willems, R.; Michels, M. Validation of the 2014 European Society of Cardiology Guidelines Risk Prediction Model for the Primary Prevention of Sudden Cardiac Death in Hypertrophic Cardiomyopathy. Circ. Arrhythm. Electrophysiol. 2015, 8, 829–835. [Google Scholar] [CrossRef] [Green Version]

| Parameters | All n = 329 | Alive n = 280 (85%) | Deceased n = 49 (15%) | p-Value |
|---|---|---|---|---|
| Clinical parameters | ||||
| Age (years) | 49.88 ± 10.71 | 49.31 ± 10.69 | 53.29 ± 10.66 | 0.006 |
| Male (n (%)) | 261 (79.3%) | 226 (80.7%) | 35 (71.4%) | 0.14 |
| Symptoms duration (months) | 21.3 ± 34.78 | 25.15 ± 89.865 | 28.63 ± 41.03 | 0.31 |
| BMI (kg/m2) | 29.39 ± 14.37 | 29.47 ± 16.162 | 29.16 ± 6.18 | 0.77 |
| NYHA class | 2.23 ± 0.77 | 2.14 ± 0.73 | 2.73 ± 0.8 | <0.0001 |
| NYHA III/IV | 89 (27.1%) | 63 (22.5%) | 26 (53.1%) | <0.0001 |
| Diabetes mellitus (n (%)) | 64 (19.5%) | 49 (17.5%) | 15 (30.6%) | 0.03 |
| Prior stroke (n (%)) | 13 (4%) | 11 (3.9%) | 2 (4.1%) | 0.96 |
| Liver diseases (n (%)) | 47 (14.3%) | 39 (13.9%) | 8 (16.3%) | 0.66 |
| Dyslipidaemia (n (%)) | 258 (78.4%) | 223 (79.6%) | 35 (71.4%) | 0.20 |
| COPD (n (%)) | 18 (5.5%) | 15 (5.4%) | 3 (6.1%) | 0.83 |
| Atrial fibrillation (n (%)) | 100 (30.4%) | 84 (30.0%) | 16 (32.7%) | 0.71 |
| Hypertension (n (%)) | 155 (47.1%) | 127 (45.4%) | 28 (57.1%) | 0.13 |
| SBP (mmHg) | 122.99 ± 20.55 | 123.97 ± 20.58 | 117.83 ± 19.94 | 0.09 |
| ECG findings | ||||
| HR (bpm) | 76.5 ± 16.62 | 75.76 ± 16.011 | 80.93 ± 19.75 | 0.07 |
| QRS (ms) | 105.59 ± 35.24 | 104.11 ± 34.077 | 114.49 ± 41.13 | 0.05 |
| LBBB (n (%)) | 74 (22.5%) | 62 (22.1%) | 12 (24.5%) | 0.72 |
| VT (0/1) | 88 (26.7%) | 74 (26.6%) | 14 (28.6%) | 0.81 |
| Echocardiographic findings | ||||
| LVEF (%) | 27.02 ± 9.96 | 27.73 ± 9.936 | 23.72 ± 9.55 | 0.01 |
| LVEDd (mm) | 65.08 ± 8.89 | 64.76 ± 8.64 | 66.46 ± 10.24 | 0.24 |
| IVS (mm) | 10 ± 1.98 | 10.06 ± 1.987 | 9.7 ± 1.91 | 0.33 |
| RVOT (mm) | 33.79 ± 6.61 | 33.4 ± 6.383 | 36.15 ± 7.41 | 0.008 |
| TAPSE (mm) | 19.14 ± 4.12 | 19.41 ± 4.118 | 17.77 ± 4.02 | 0.01 |
| LAA (cm2) | 28.97 ± 8.33 | 28.35 ± 7.813 | 32.04 ± 10.27 | 0.01 |
| RVSP (mmHg) | 25.46 ± 13.12 | 23.89 ± 11.886 | 33.46 ± 16.15 | 0.0001 |
| MR moderate/severe (n (%)) | 111 (33.7%) | 89 (31.8%) | 22 (44.9%) | 0.07 |
| TR moderate/severe (n (%)) | 66 (20.1%) | 44 (15.7%) | 22 (44.9%) | <0.0001 |
| Laboratory tests results | ||||
| Hb (g/dL) | 14.55 ± 1.66 | 14.67 ± 1.626 | 13.88 ± 1.78 | 0.002 |
| eGFR (ml/min/1.73 m2) | 83.5 ± 20.9 | 84.91 ± 20.411 | 75.67 ± 22.71 | 0.006 |
| NT-proBNP (pg/mL) | 2759.25 ± 3639.6 | 2297.9 ± 3131.6 | 4980.7 ± 4910.9 | <0.0001 |
| LDL (mmol/L) | 2.99 ± 0.98 | 2.99 ± 0.969 | 2.86 ± 1.04 | 0.36 |
| Heart failure therapy | ||||
| BB (n (%)) | 317 (96.4%) | 272 (97.1%) | 45 (91.8%) | 0.049 |
| ACEi/ARB/ARNI (n (%)) | 291 (88.4%) | 253 (90.4%) | 38 (77.6%) | 0.01 |
| MRA (n (%)) | 285 (86.6%) | 244 (87.1%) | 41 (83.7%) | 0.51 |
| Loop diuretics (mg/d) 1 | 44.47 ± 69.24 | 37.91 ± 56.42 | 80.16 ± 113.94 | 0.0003 |
| Furosemide (mg/d) | 25.7 ± 50.31 | 22.02 ± 44.717 | 45.57 ± 72 | 0.03 |
| Ivabradine (n (%)) | 53 (16.1%) | 41 (14.6%) | 12 (24.5%) | 0.08 |
| Digoxin (n (%)) | 52 (15.8%) | 38 (13.6%) | 14 (28.6%) | 0.008 |
| Statins (n (%)) | 148 (45%) | 124 (44.3%) | 24 (49.0%) | 0.54 |
| CRT (n (%)) | 11 (3.3%) | 6 (2.1%) | 5 (10.2%) | 0.004 |
| ICD (n (%)) | 30 (9.1%) | 23 (8.2%) | 7 (14.3%) | 0.17 |
| Follow-Up | Observed Mortality [%] (Kaplan–Meier Analysis) | Calculated Mortality Risk [%] | Krakow DCM Risk Score Discrimination | ||||
|---|---|---|---|---|---|---|---|
| All | Alive | Deceased | p-Value | AUC-ROC | p-Value | ||
| 1 year | 4.68 ± 0.02 | 3.52 ± 9.13 | 3.08 ± 8.41 | 11.2 ± 15.93 | 0.0006 | 0.765 [95%CI 0.628–0.902] | 0.0001 |
| 2 years | 9.96 ± 0.02 | 6.88 ± 14.21 | 5.96 ± 13.02 | 14.48 ± 20.16 | 0.0003 | 0.718 [95%CI 0.613–0.822] | <0.0001 |
| 3 years | 14.41 ± 0.02 | 10.37 ± 18.68 | 8.25 ± 15.4 | 18.91 ± 25.4 | 0.0002 | 0.706 [95%CI 0.608–0.805] | <0.0001 |
| 4 years | 17.60 ± 0.03 | 13.06 ± 21.32 | 10.32 ± 18.54 | 20.89 ± 26.19 | 0.0001 | 0.709 [95%CI 0.616–0.802] | <0.0001 |
| 5 years | 22.57 ± 0.03 | 15.78 ± 23.53 | 11.51 ± 19.85 | 23.49 ± 27.26 | 0.0002 | 0.704 [95%CI 0.609–0.798] | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dziewięcka, E.; Winiarczyk, M.; Wiśniowska-Śmiałek, S.; Karabinowska-Małocha, A.; Gliniak, M.; Robak, J.; Kaciczak, M.; Leszek, P.; Celińska-Spodar, M.; Dziewięcki, M.; et al. Clinical Utility and Validation of the Krakow DCM Risk Score—A Prognostic Model Dedicated to Dilated Cardiomyopathy. J. Pers. Med. 2022, 12, 236. https://doi.org/10.3390/jpm12020236
Dziewięcka E, Winiarczyk M, Wiśniowska-Śmiałek S, Karabinowska-Małocha A, Gliniak M, Robak J, Kaciczak M, Leszek P, Celińska-Spodar M, Dziewięcki M, et al. Clinical Utility and Validation of the Krakow DCM Risk Score—A Prognostic Model Dedicated to Dilated Cardiomyopathy. Journal of Personalized Medicine. 2022; 12(2):236. https://doi.org/10.3390/jpm12020236
Chicago/Turabian StyleDziewięcka, Ewa, Mateusz Winiarczyk, Sylwia Wiśniowska-Śmiałek, Aleksandra Karabinowska-Małocha, Matylda Gliniak, Jan Robak, Monika Kaciczak, Przemysław Leszek, Małgorzata Celińska-Spodar, Marcin Dziewięcki, and et al. 2022. "Clinical Utility and Validation of the Krakow DCM Risk Score—A Prognostic Model Dedicated to Dilated Cardiomyopathy" Journal of Personalized Medicine 12, no. 2: 236. https://doi.org/10.3390/jpm12020236
APA StyleDziewięcka, E., Winiarczyk, M., Wiśniowska-Śmiałek, S., Karabinowska-Małocha, A., Gliniak, M., Robak, J., Kaciczak, M., Leszek, P., Celińska-Spodar, M., Dziewięcki, M., & Rubiś, P. (2022). Clinical Utility and Validation of the Krakow DCM Risk Score—A Prognostic Model Dedicated to Dilated Cardiomyopathy. Journal of Personalized Medicine, 12(2), 236. https://doi.org/10.3390/jpm12020236








