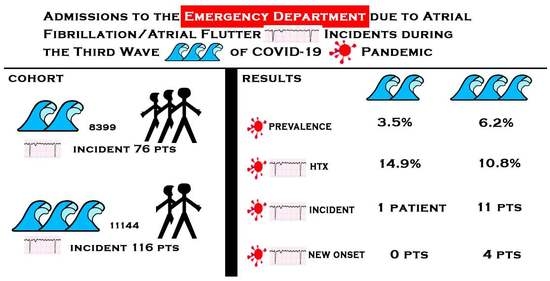
Admissions to the Emergency Department Due to Atrial Fibrillation/Atrial Flutter Incidents during the Third Wave of COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
The Vaccination Status of the Patients with AF/AFL Incident during Study Period
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Russo, V.; Navarin, S.; Zampini, G.; Magrini, L.; Mann, C.; Muiesan, M.L.S.; de Caterina, R.; Yilmaz, M.B.; Beton, O.; Monzani, V.; et al. Management of atrial fibrillation in the Emergency Department: Current approach and future expectations. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 3132–3147. [Google Scholar] [PubMed]
- Gulizia, M.M.; Cemin, R.; Colivicchi, F.; De Luca, L.; Di Lenarda, A.; Boriani, G.; di Pasquale, G.; Nardi, F.; Scherillo, M.; Lucci, D.; et al. Management of atrial fibrillation in the emergency room and in the cardiology ward: The BLITZ AF study. Europace 2019, 21, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Chourasia, G.; Sycz, W.K.; Wolniakowski, I.; Dudek, K.; Porębska, B.; Moczarska, J. Changes in the Visits to Emergency Department of Non-Infectious Hospital during the Early COVID-19 State of Epidemic. Emerg Med. Serv. 2020, 7, 99–102. [Google Scholar] [CrossRef]
- Bilaszewski, Ł.; Timler, W.; Budrewicz, K.; Marczak, M.; Kozłowski, R.; Wizowska, J.; Timler, M.; Jagielski, D.; Dudek, M.; Rasmus, P.; et al. The Impact of COVID-19 on Admissions and Management of Patients with Atrial Fibrillation Episodes in the Emergency Department. Int. J. Environ. Res. Public Health 2021, 18, 6048. [Google Scholar] [CrossRef] [PubMed]
- Schnaubelt, S.; Domanovits, H.; Niederdoeckl, J.; Schuetz, N.; Cacioppo, F.; Oppenauer, J.; Spiel, A.O.; Laggner, A.N. The Impact of the COVID-19 Pandemic on Incidences of Atrial Fibrillation and Electrical Cardioversion at a Tertiary Care Emergency Department: An Inter- and Intra-year Analysis. Front. Med. 2020, 7, 595881. [Google Scholar] [CrossRef] [PubMed]
- Ueberham, L.; König, S.; Pellissier, V.; Hohenstein, S.; Meier-Hellmann, A.; Kuhlen, R.; Hindricks, G.; Bollmann, A. Admission rates and care pathways in patients with atrial fibrillation during the COVID-19 pandemic-insights from the German-wide Helios hospital network. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Hwang, Y.M.; Cho, Y.; Oh, I.Y. Prognostic impact of atrial fibrillation in patients with severe acute respiratory syndrome coronavirus 2 infection. Medicine 2021, 100, e26993. [Google Scholar] [CrossRef] [PubMed]
- Romiti, G.F.; Corica, B.; Lip, G.Y.H.; Proietti, M. Prevalence and Impact of Atrial Fibrillation in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 2490. [Google Scholar] [CrossRef] [PubMed]
- Gawałko, M.; Kapłon-Cieślicka, A.; Hohl, M.; Dobrev, D.; Linz, D. COVID-19 associated atrial fibrillation: Incidence, putative mechanisms and potential clinical implications. Int. J. Cardiol. Heart Vasc. 2020, 30, 100631. [Google Scholar] [CrossRef] [PubMed]
- Stone, E.; Kiat, H.; McLachlan, C.S. Atrial fibrillation in COVID-19: A review of possible mechanisms. FASEB J. 2020, 34, 11347–11354. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, B.; Brady, W.J.; Bridwell, R.E.; Ramzy, M.; Montrief, T.; Singh, M.; Gottlieb, M. Electrocardiographic manifestations of COVID-19. Am. J. Emerg. Med. 2021, 41, 96–103. [Google Scholar] [CrossRef] [PubMed]
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 25 September 2021).
- Denegri, A.; Pezzuto, G.; D’Arienzo, M.; Morelli, M.; Savorani, F.; Cappello, C.G.; Luciani, A.; Boriani, G. Clinical and electrocardiographic characteristics at admission of COVID-19/SARS-CoV2 pneumonia infection. Intern. Emerg. Med. 2021, 16, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Lanza, G.A.; De Vita, A.; Ravenna, S.E.; D’Aiello, A.; Covino, M.; Franceschi, F. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace 2021, 23, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Russo, V.; Di Maio, M.; Mottola, F.F.; Pagnano, G.; Attena, E.; Verde, N.; Di Micco, P.; Silverio, A.; Scudiero, F.; Nunziata, L.; et al. Clinical characteristics and prognosis of hospitalized COVID-19 patients with incident sustained tachyarrhythmias: A multicenter observational study. Eur. J. Clin. Investig. 2020, 50, e13387. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.F.; Cheng, W.H.; Hung, Y.; Lin, W.Y.; Chao, T.F.; Liao, J.N.; Lin, Y.J.; Lin, W.S.; Chen, Y.J.; Chen, S.A. Management of Atrial Fibrillation in COVID-19 Pandemic. Circ. J. 2020, 84, 1679–1685. [Google Scholar] [CrossRef] [PubMed]
- Chahal, A.A.; Anesi, G.; Denduluri, S.; Domenico, C.M.; Arkles, J.; Abella, B.S.; Bullinga, J.R.; Callans, D.J.; Dixit, S. COVID-19 and cardiac arrhythmias. Heart Rhythm 2020, 17, 1439–1444. [Google Scholar] [CrossRef]
- Sowa, P.; Kiszkiel, Ł.; Laskowski, P.P.; Alimowski, M.; Szczerbiński, Ł.; Paniczko, M.; Moniuszko-Malinowska, A.; Kamiński, K. COVID-19 Vaccine Hesitancy in Poland-Multifactorial Impact Trajectories. Vaccines 2021, 9, 876. [Google Scholar] [CrossRef] [PubMed]
- Klugar, M.; Riad, A.; Mekhemar, M.; Conrad, J.; Buchbender, M.; Howaldt, H.P.; Attia, S. Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology 2021, 10, 752. [Google Scholar] [CrossRef] [PubMed]
| Study Period AF/AFL (+) N = 116 | Reference Period AF/AFL (+) N = 76 | p | |
|---|---|---|---|
| Age.; mean (SD) | 72.3 (12.1) | 71.2 (14.9) | 0.581 |
| Male sex.; n (%) | 52 (46.6) | 45 (59.2) | 0.051 |
| AF/AFL duration.; h.; median (IQR)/# of known | 9 (5–48)/82 | 10 (4–60)/48 | 0.341 |
| Unknown or unrecorded duration of AF.; n (%) | 34 (29.;3) | 28 (36.8) | 0.275 |
| Sinus rhythm restoration before the ED admission n (%) | 11 (9.5) | 4 (5.3) | 0.287 |
| Sinus rhythm at the ED discharge | 57 (51.1) | 37 (48.7) | 0.951 |
| Hospital admission n (%) | 28 (24.1) | 12 (15.8) | 0.164 |
| New onset n (%) | 11 (9.5) | 7 (9.2) | 0.950 |
| Rate control strategy at the ED n (%) | 35 (30.2) | 30 (39.5) | 0.183 |
| Phenazoline.; n (%) | 24 (20.7) | 24 (32.0) | 0.089 |
| Amiodarone.; n (%) | 13 (11.2) | 7 (9.3) | 0.658 |
| Beta-blocker.; n (%) | 31 (26.7) | 13 (17.3) | 0.121 |
| Rytmonorm n (%) | 5 (4.3) | 3 (4.0) | 0.902 |
| Electrocardioversion.; n (%) | 7 (6.0) | 8 (10.7) | 0.257 |
| SARS-CoV-2-positive n (%) | 11 (9.5) | 1 (1.3) | 0.047 |
| Brought to the ED by EMS n (%) | 57 (67.8) | 54 (71.1) | 0.002 |
| Duration of the stay in the ED (min) median (IQR) | 413.0 (283.5–564.0) | 435.5 (297.5–634.0) | 0.436 |
| SARS-CoV-2 (+) AFL/AF (-) (1) N = 681 | SARS CoV-2 (+) AFL/AF (+) (2) N = 11 | SARS CoV-2 (-) AFL/AF (+) (3) N = 105 | p (1) vs. (2) | p (1) vs. (3) | p (2) vs. (3) | |
|---|---|---|---|---|---|---|
| Age.; years.; mean (SD) | 60.6 (18.1) | 76.3 (13.2) | 71.8 (12.6) | 0.001 | 0.001 | 0.001 |
| Male gender.; n (%) | 353 (51.8) | 2 (18.2) | 50 (47.6) | 0.053 | 0.389 | 0.121 |
| Palpitations.; n (%) | 5 (0.7) | 5 (45.5) | 93 (88.6) | <0.001 | <0.001 | <0.001 |
| Fever.; n (%) | 247 (36.3) | 0 (0) | 0 (0) | 0.030 | 0.001 | 0.968 |
| Altered mental status.; n (%) | 111 (16.3) | 0 (0) | 6 (5.7) | 0.295 | 0.005 | 0.921 |
| Dyspnea.; n (%) | 389 (56.3) | 6 (54.4) | 18 (17.1) | 0.868 | <0.001 | 0.012 |
| Cough.; n (%) | 182 (26.7) | 0 (0) | 0 (0) | 0.099 | <0.001 | 0.999 |
| Gastrointestinal problems.; n (%) | 97 (14.3) | 0 (0) | 4 (3.8) | 0.362 | 0.005 | 0.834 |
| Chest pain.; n (%) | 40 (5.9) | 3 (27.3) | 13 (12.4) | 0.034 | 0.013 | 0.366 |
| New onset AF.; n (%) | 4 (0.6) | 4 (36.4) | 7 (6.7) | 0.001 | 0.002 | 0.008 |
| Full vaccination at least 14 days before positive SARS-CoV-2 test n (%)/N N-the number of patients with known vaccination history | 18 (3.7)/490 | 0 (0)/11 | 27 (25.7)/105 | 0.517 | <0.001 | 0.123 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chourasia, G.; Zyśko, D.; Wizowska, J.; Wróblewski, P.; Madziarska, K.; Wróbel, K.; Timler, W.; Kozłowski, R.; Marczak, M.; Timler, D. Admissions to the Emergency Department Due to Atrial Fibrillation/Atrial Flutter Incidents during the Third Wave of COVID-19 Pandemic. J. Pers. Med. 2022, 12, 2003. https://doi.org/10.3390/jpm12122003
Chourasia G, Zyśko D, Wizowska J, Wróblewski P, Madziarska K, Wróbel K, Timler W, Kozłowski R, Marczak M, Timler D. Admissions to the Emergency Department Due to Atrial Fibrillation/Atrial Flutter Incidents during the Third Wave of COVID-19 Pandemic. Journal of Personalized Medicine. 2022; 12(12):2003. https://doi.org/10.3390/jpm12122003
Chicago/Turabian StyleChourasia, Goutam, Dorota Zyśko, Joanna Wizowska, Paweł Wróblewski, Katarzyna Madziarska, Kacper Wróbel, Wojciech Timler, Remigiusz Kozłowski, Michał Marczak, and Dariusz Timler. 2022. "Admissions to the Emergency Department Due to Atrial Fibrillation/Atrial Flutter Incidents during the Third Wave of COVID-19 Pandemic" Journal of Personalized Medicine 12, no. 12: 2003. https://doi.org/10.3390/jpm12122003
APA StyleChourasia, G., Zyśko, D., Wizowska, J., Wróblewski, P., Madziarska, K., Wróbel, K., Timler, W., Kozłowski, R., Marczak, M., & Timler, D. (2022). Admissions to the Emergency Department Due to Atrial Fibrillation/Atrial Flutter Incidents during the Third Wave of COVID-19 Pandemic. Journal of Personalized Medicine, 12(12), 2003. https://doi.org/10.3390/jpm12122003