Evaluation of Internet-Connected Real-Time Remote Auscultation: An Open-Label Randomized Controlled Pilot Trial
Abstract
1. Introduction
2. Materials and Methods
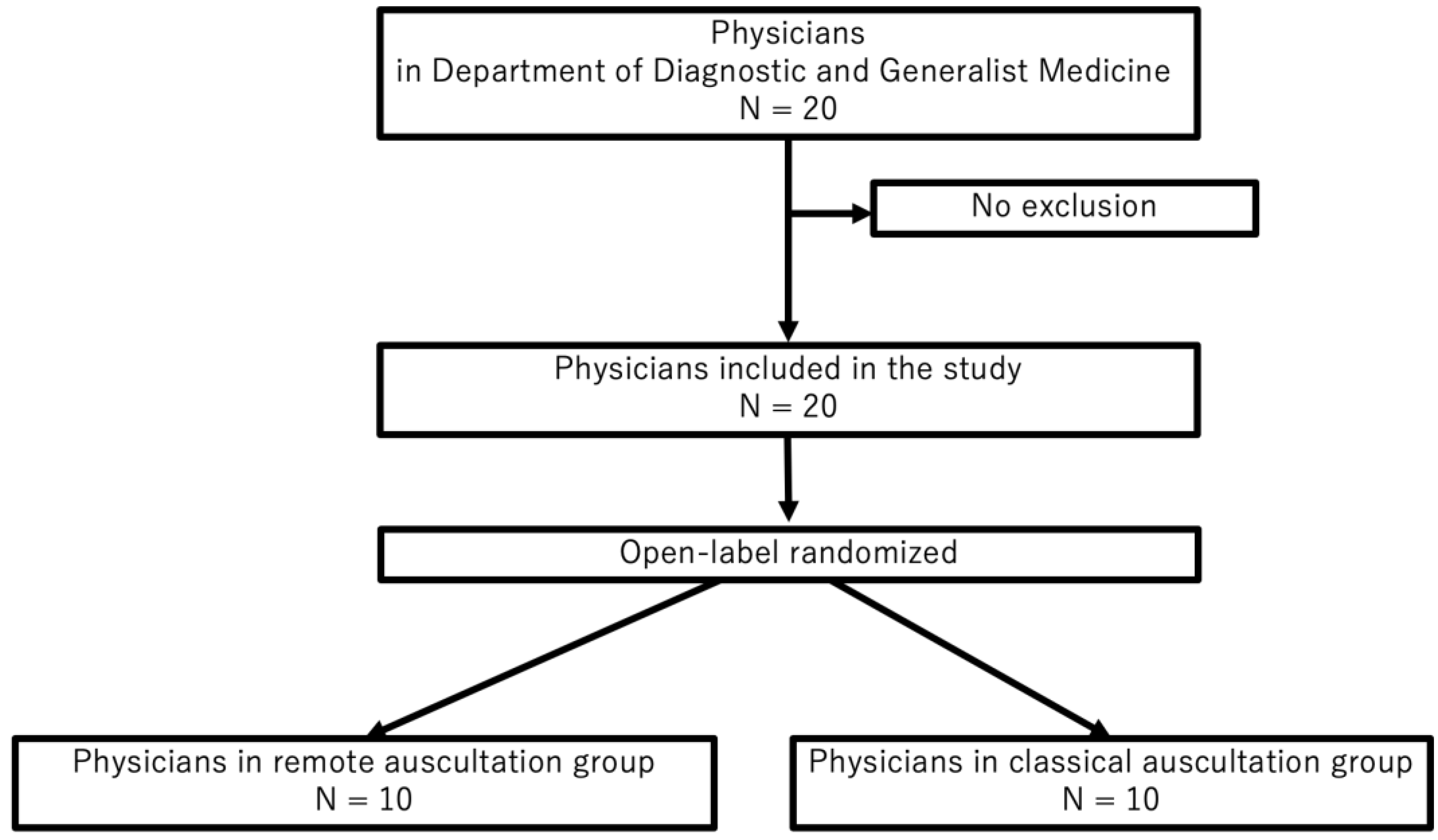
2.1. Study Design, Setting, and Participants
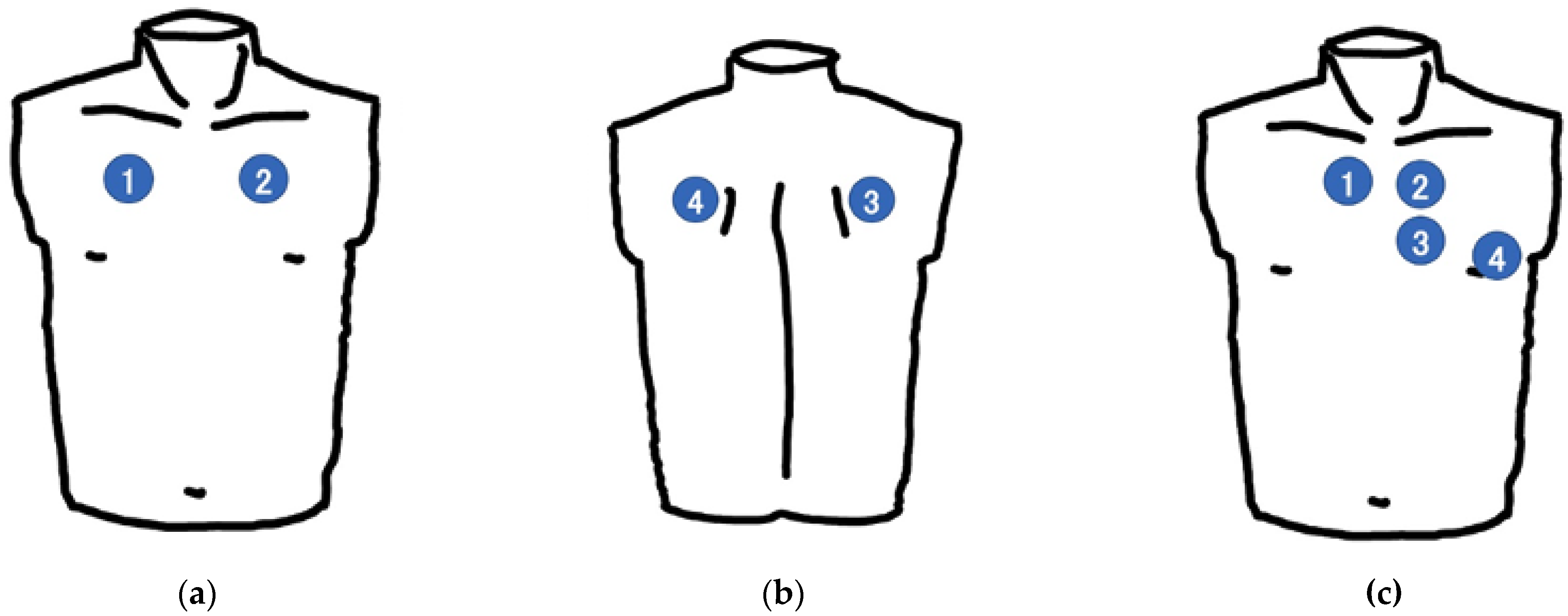
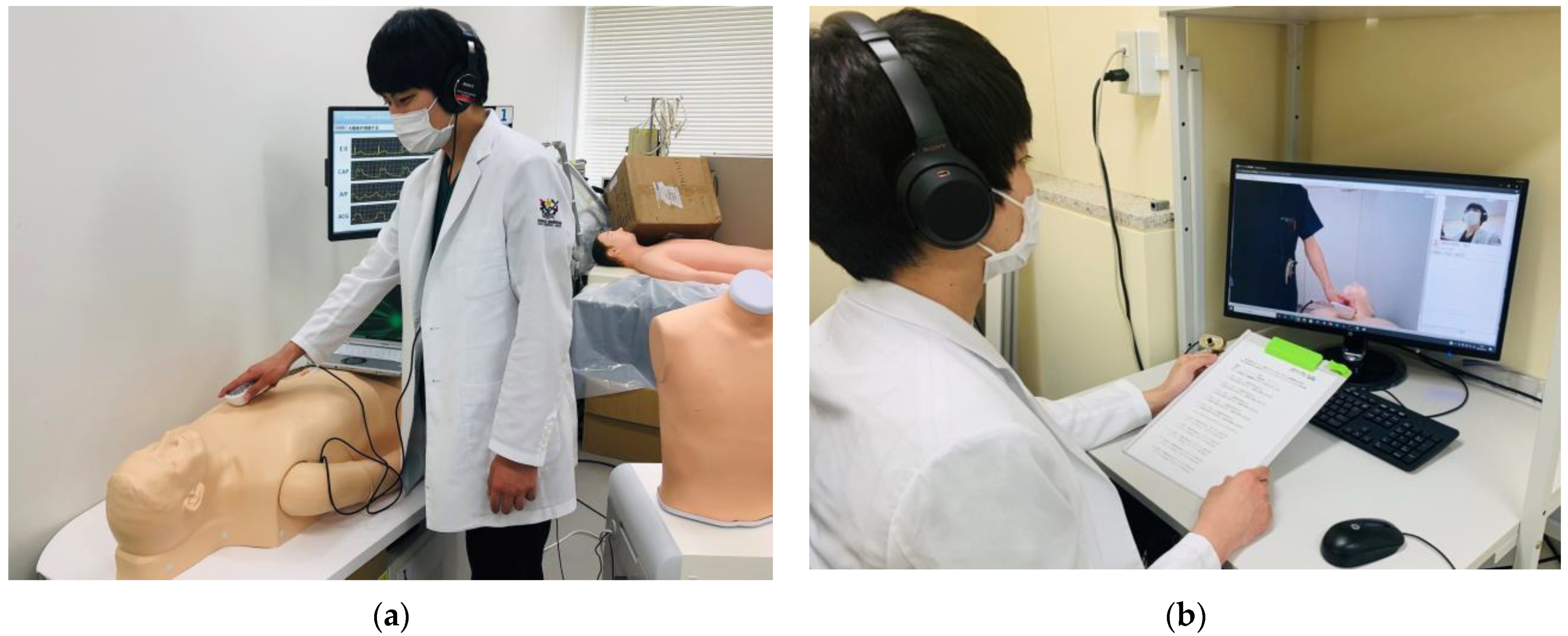
2.2. Procedures
2.2.1. Study Flow and Randomization
2.2.2. Training Session
2.2.3. Test Session
2.2.4. Simulator
2.2.5. Real-Time Remote Auscultation
2.3. Data Collection and Outcome Measures
2.4. Statistical Analysis
3. Results
3.1. Participants’ Profiles
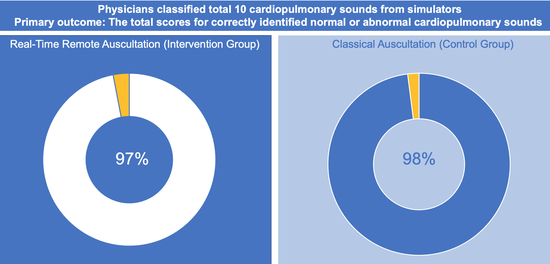
3.2. Diagnostic Performance
3.2.1. Diagnostic Performance for Lung Sounds
3.2.2. Diagnostic Performance for Cardiac Sounds
4. Discussion
4.1. Principal Results
4.2. Strengths
4.3. Limitations
4.4. Comparions with Our Prior Work
4.5. Other Remote Auscultation Systems
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wijesooriya, N.R.; Mishra, V.; Brand, P.L.P.; Rubin, B.K. COVID-19 and telehealth, education, and research adaptations. Paediatr. Respir. Rev. 2020, 35, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Omboni, S. Telemedicine During The COVID-19 in Italy: A Missed Opportunity? Telemed. J. E Health 2020, 26, 973–975. [Google Scholar] [CrossRef] [PubMed]
- Pereira, D.; Castro, A.; Gomes, P.; Areias, J.C.N.C.; Reis, Z.S.N.; Coimbra, M.T.; Cruz-Correia, R. Digital Auscultation. In Encyclopedia of E-Health and Telemedicine; IGI Global: Hershey, PA, USA, 2016; pp. 910–927. [Google Scholar]
- Leng, S.; Tan, R.S.; Chai, K.T.; Wang, C.; Ghista, D.; Zhong, L. The electronic stethoscope. Biomed. Eng. Online 2015, 14, 66. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, O.J.; Persaud, Y.; Kimball, A.B. Telehealth Systems; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Marani, R.; Gelao, G.; Perri, A.G. High quality heart and lung auscultation system for diagnostic use on remote patients in real time. Open Biomed. Eng. J. 2010, 4, 250–256. [Google Scholar]
- Fan, M.; Wang, Q.; Liu, J.; Su, L.; Wang, B.; Xu, H.; Li, Q.; Zhang, Z. Real-world evaluation of the Stemoscope electronic tele-auscultation system. Biomed. Eng. Online 2022, 21, 63. [Google Scholar] [CrossRef]
- Fragasso, G.; Cuko, A.; Spoladore, R.; Montano, C.; Palloshi, A.; Silipigni, C.; Monti, G.; Castelli, A.; Padiglione, F.; Leonida, A.; et al. Validation of remote cardiopulmonary examination in patients with heart failure with a videophone-based system. J. Card. Fail. 2007, 13, 281–286. [Google Scholar] [CrossRef]
- Hirosawa, T.; Harada, Y.; Ikenoya, K.; Kakimoto, S.; Aizawa, Y.; Shimizu, T. The Utility of Real-Time Remote Auscultation Using a Bluetooth-Connected Electronic Stethoscope: Open-Label Randomized Controlled Pilot Trial. JMIR Mhealth Uhealth 2021, 9, e23109. [Google Scholar] [CrossRef]
- Bernardi, S.; Giudici, F.; Leone, M.F.; Zuolo, G.; Furlotti, S.; Carretta, R.; Fabris, B. A prospective study on the efficacy of patient simulation in heart and lung auscultation. BMC Med. Educ. 2019, 19, 275. [Google Scholar] [CrossRef] [PubMed]
- Vukanovic-Criley, J.M.; Criley, S.; Warde, C.M.; Boker, J.R.; Guevara-Matheus, L.; Churchill, W.H.; Nelson, W.P.; Criley, J.M. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: A multicenter study. Arch. Intern. Med. 2006, 166, 610–616. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic, S. Updated nomenclature for membership reaction. ATS NEWS 1977, 3, 5–6. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Bohadana, A.; Izbicki, G.; Kraman, S.S. Fundamentals of lung auscultation. N. Engl. J. Med. 2014, 370, 744–751. [Google Scholar] [CrossRef]
- Nobuoka, S.; Kamegai, M.; Nakamura, T. Assessment of Cardiac Auscultatory Events in Outpatients in General Internal Medicine: Teaching Suggestions for Education on Cardiac Auscultatory Skills in Primary Care. Gen. Med. 2006, 7, 25–28. [Google Scholar] [CrossRef]
- Chen, C.H.; Huang, W.T.; Tan, T.H.; Chang, C.C.; Chang, Y.J. Using K-Nearest Neighbor Classification to Diagnose Abnormal Lung Sounds. Sensors 2015, 15, 13132–13158. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Andrès, E.; Hajjam, A.; Brandt, C. Advances and innovations in the field of auscultation, with a special focus on the development of new intelligent communicating stethoscope systems. Health Technol. 2012, 2, 5–16. [Google Scholar] [CrossRef]
- Kalinauskienė, E.; Razvadauskas, H.; Morse, D.J.; Maxey, G.E.; Naudžiūnas, A. A Comparison of Electronic and Traditional Stethoscopes in the Heart Auscultation of Obese Patients. Medicina 2019, 55, 94. [Google Scholar] [CrossRef]
- Behere, S.; Baffa, J.M.; Penfil, S.; Slamon, N. Real-World Evaluation of the Eko Electronic Teleauscultation System. Pediatr. Cardiol. 2018, 40, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Ghanayim, T.; Lupu, L.; Naveh, S.; Bachner-Hinenzon, N.; Adler, D.; Adawi, S.; Banai, S.; Shiran, A. Artificial Intelligence-Based Stethoscope for the Diagnosis of Aortic Stenosis. Am. J. Med. 2022, 135, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Belmont, J.M.; Mattioli, L.F. Accuracy of analog telephonic stethoscopy for pediatric telecardiology. Pediatrics 2003, 112, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Noda, A.; Saraya, T.; Morita, K.; Saito, M.; Shimasaki, T.; Kurai, D.; Nakamoto, K.; Ishii, H. Evidence of the Sequential Changes of Lung Sounds in COVID-19 Pneumonia Using a Novel Wireless Stethoscope with the Telemedicine System. Intern. Med. 2020, 59, 3213–3216. [Google Scholar] [CrossRef] [PubMed]
- Zenk, B.M.; Bratton, R.L.; Flipse, T.R.; Page, E.E. Accuracy of detecting irregular cardiac rhythms via telemedicine. J. Telemed. Telecare 2004, 10, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, L.; Goertz, K.; Ardinger, R.; Belmont, J.; Cox, R.; Thomas, C. Pediatric cardiology: Auscultation from 280 miles away. Kans. Med. 1992, 93, 326, 347–350. [Google Scholar] [PubMed]
- Hedayioglu, F.L.; Mattos, S.S.; Moser, L.; de Lima, M.E. Development of a tele-stethoscope and its application in pediatric cardiology. Indian J. Exp. Biol. 2007, 45, 86–92. [Google Scholar]
- Klum, M.; Urban, M.; Tigges, T.; Pielmus, A.-G.; Feldheiser, A.; Schmitt, T.; Orglmeister, R. Wearable Cardiorespiratory Monitoring Employing a Multimodal Digital Patch Stethoscope: Estimation of ECG, PEP, LVET and Respiration Using a 55 mm Single-Lead ECG and Phonocardiogram. Sensors 2020, 20, 2033. [Google Scholar] [CrossRef]
- Thompson, W.R.; Reinisch, A.J.; Unterberger, M.J.; Schriefl, A.J. Artificial Intelligence-Assisted Auscultation of Heart Murmurs: Validation by Virtual Clinical Trial. Pediatr. Cardiol. 2019, 40, 623–629. [Google Scholar] [CrossRef]

| Variable | Remote Auscultation (N = 10) | Classical Auscultation (N = 10) | p Value |
|---|---|---|---|
| Age (years), mean ± SD | 31.6 ± 4 | 32.6 ± 5.1 | 0.63 1 |
| No. of men, n (%) | 9 (90) | 6 (60) | 0.15 2 |
| Years after graduation (years), mean ± (SD) | 6.8 ± 4 | 8.1 ± 5.5 | 0.54 1 |
| Variable | Remote Auscultation (N = 10) | Classical Auscultation (N = 10) | p Value 1 |
|---|---|---|---|
| Total scores for correctly identified normal or abnormal cardiopulmonary sounds | 97/100 (97) | 98/100 (98) | >0.99 |
| Total lung sounds, n (%) | 43/50 (86) | 45/50 (90) | 0.54 |
| Normal | 10/10 (100) | 10/10 (100) | >0.99 |
| Wheeze | 10/10 (100) | 9/10 (90) | 0.99 |
| Rhonchi | 9/10 (90) | 9/10 (90) | >0.99 |
| Coarse crackles | 8/10 (80) | 9/10 (90) | 0.54 |
| Fine crackles | 6/10 (60) | 8/10 (80) | 0.34 |
| Total cardiac sounds, n (%) | 36/50 (72) | 47/50 (94) | <0.05 |
| Normal | 9/10 (90) | 10/10 (100) | 0.99 |
| S3 gallop | 8/10 (80) | 10/10 (100) | 0.99 |
| Aortic stenosis | 5/10 (50) | 9/10 (90) | 0.07 |
| Aortic regurgitation | 7/10 (70) | 9/10 (90) | 0.28 |
| Mitral regurgitation | 7/10 (70) | 9/10 (90) | 0.28 |
| Participants’ Responses in the Remote Auscultation Group | |||||
| Normal | Wheeze | Rhonchi | Coarse Crackles | Fine Crackles | |
| Correct Answer | |||||
| Normal | 10/10 | 0 | 0 | 0 | 0 |
| Wheeze | 0 | 10/10 | 0 | 0 | 0 |
| Rhonchi | 0 | 0 | 9/10 | 0 | 1/10 |
| Coarse crackles | 0 | 0 | 0 | 8/10 | 2/10 |
| Fine crackles | 0 | 0 | 1/10 | 3/10 | 6/10 |
| Participants’ Responses in the Classical Auscultation Group | |||||
| Normal | Wheeze | Rhonchi | Coarse Crackles | Fine Crackles | |
| Correct Answer | |||||
| Normal | 10/10 | 0 | 0 | 0 | 0 |
| Wheezes | 0 | 9/10 | 1/10 | 0 | 0 |
| Rhonchi | 0 | 1/10 | 9/10 | 0 | 0 |
| Coarse crackles | 0 | 0 | 0 | 9/10 | 1/10 |
| Fine crackles | 1/10 | 0 | 0 | 1/10 | 8/10 |
| Participants’ Responses in the Remote Auscultation Group | |||||
| Normal | S3 gallop | Aortic stenosis | Aortic regurgitation | Mitral Regurgitation | |
| Correct Answer | |||||
| Normal | 9/10 | 1/10 | 0 | 0 | 0 |
| S3 gallop | 2/10 | 8/10 | 0 | 0 | 0 |
| Aortic stenosis | 0 | 0 | 5/10 | 3/10 | 2/10 |
| Aortic regurgitation | 0 | 1/10 | 2/10 | 7/10 | 0 |
| Mitral regurgitation | 0 | 0 | 3/10 | 0 | 7/10 |
| Participants’ Responses in the Classical Auscultation Group | |||||
| Normal | S3 Gallop | Aortic Stenosis | Aortic Regurgitation | Mitral Regurgitation | |
| Correct Answer | |||||
| Normal | 10/10 | 0 | 0 | 0 | 0 |
| S3 gallop | 0 | 10/10 | 0 | 0 | 0 |
| Aortic stenosis | 0 | 0 | 9/10 | 1/10 | 0 |
| Aortic regurgitation | 0 | 0 | 1/10 | 9/10 | 0 |
| Mitral regurgitation | 0 | 0 | 1/10 | 0 | 9/10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, T.; Hirosawa, T.; Harada, Y.; Kakimoto, S.; Shimizu, T. Evaluation of Internet-Connected Real-Time Remote Auscultation: An Open-Label Randomized Controlled Pilot Trial. J. Pers. Med. 2022, 12, 1950. https://doi.org/10.3390/jpm12121950
Ito T, Hirosawa T, Harada Y, Kakimoto S, Shimizu T. Evaluation of Internet-Connected Real-Time Remote Auscultation: An Open-Label Randomized Controlled Pilot Trial. Journal of Personalized Medicine. 2022; 12(12):1950. https://doi.org/10.3390/jpm12121950
Chicago/Turabian StyleIto, Takahiro, Takanobu Hirosawa, Yukinori Harada, Shintaro Kakimoto, and Taro Shimizu. 2022. "Evaluation of Internet-Connected Real-Time Remote Auscultation: An Open-Label Randomized Controlled Pilot Trial" Journal of Personalized Medicine 12, no. 12: 1950. https://doi.org/10.3390/jpm12121950
APA StyleIto, T., Hirosawa, T., Harada, Y., Kakimoto, S., & Shimizu, T. (2022). Evaluation of Internet-Connected Real-Time Remote Auscultation: An Open-Label Randomized Controlled Pilot Trial. Journal of Personalized Medicine, 12(12), 1950. https://doi.org/10.3390/jpm12121950