Long COVID Syndrome Presenting as Neuropsychiatric Exacerbations in Autism Spectrum Disorder: Insights for Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Monocyte Cytokine Profiles
3. Results
3.1. Case Presentation
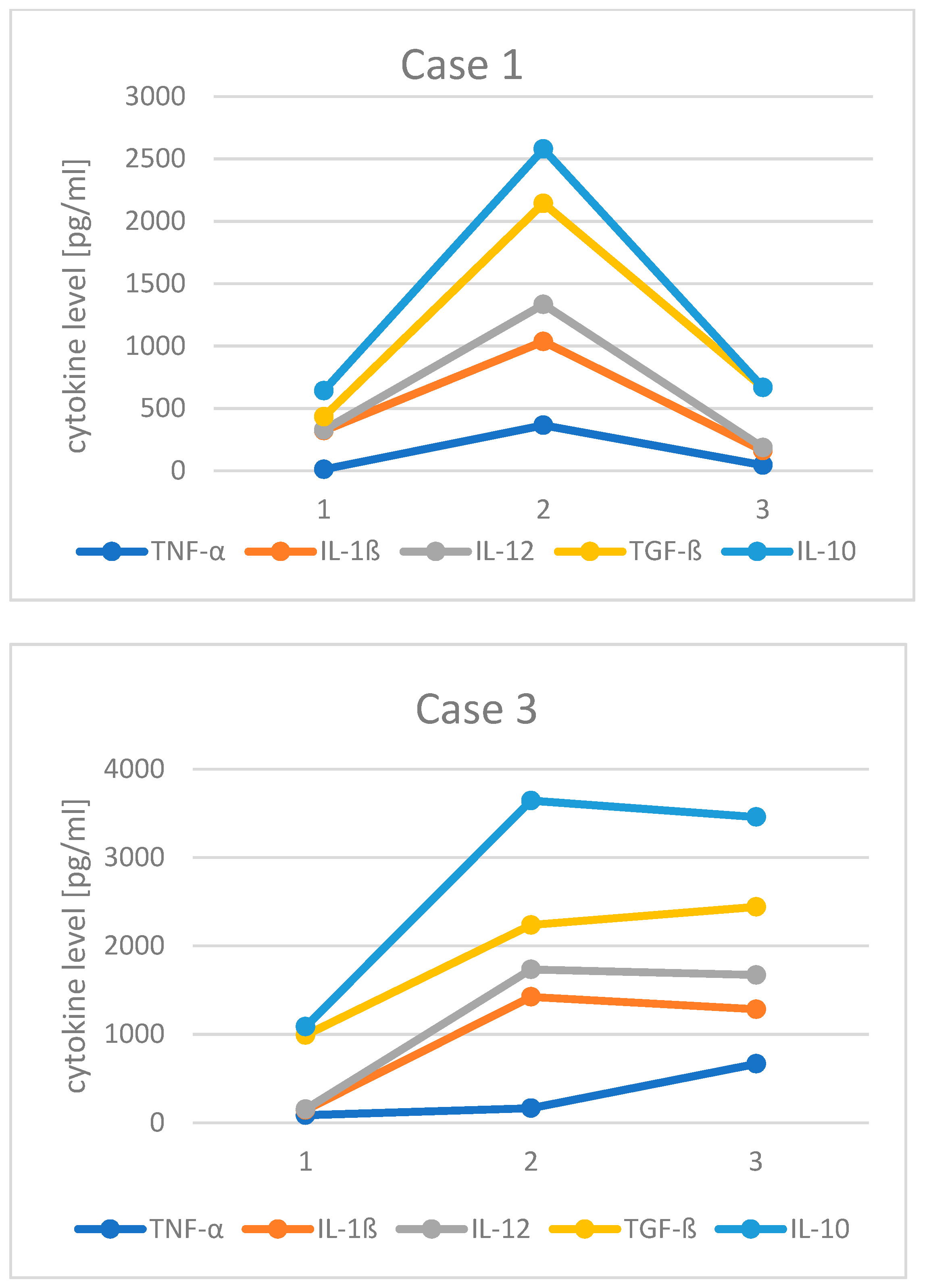
3.2. Changes in Monocyte Cytokine Profile before and after COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations Used:
| AE: | autoimmune encephalitis |
| AEDs: | anti-epileptic drugs |
| ASD: | autism spectrum disorders |
| CFS: | chronic fatigue syndrome |
| COVID-19: | coronavirus disease 2019 |
| CRCI: | cancer-therapy-related cognitive impairment |
| CVID: | common variable immunodeficiency |
| IDO: | indoleamine 2,3-dioxygenase |
| Ig: | immunoglobulin |
| IL: | interleukin |
| IVIg: | intravenous immunoglobulin |
| JAK: | Janus kinase |
| LPS: | lipopolysahhcaride |
| mTOR: | mammalian target of rapamycin |
| NSAIDs: | non-steroidal anti-inflammatory drugs |
| OCD: | obsessive compulsive disorder |
| PB Mo: | peripheral blood monocytes |
| QOL: | quality of life |
| SARS-CoV-2: | severe acute respiratory syndrome coronavirus 2 |
| SQ: | subcutaneous |
| SPUH: | Saint Peter’s University Hospital |
| TGF: | transforming growth factor |
| TNF: | tumor necrosis factor |
| WES: | whole exome sequencing |
| WGS: | whole genome sequencing |
References
- Brussow, H. COVID-19 and children: Medical impact and collateral damage. Microb. Biotechnol. 2022, 15, 1035–1049. [Google Scholar] [CrossRef]
- Lunsky, Y.; Jahoda, A.; Navas, P.; Campanella, S.; Havercamp, S.M. The mental health and well-being of adults with intellectual disability during the COVID-19 pandemic: A narrative review. J. Policy Pract. Intellect. Disabil. 2022, 19, 35–47. [Google Scholar] [CrossRef]
- Siberry, V.G.R.; Rowe, P.C. Pediatric long COVID and myalgic encephalomyelitis/chronic fatigue syndrome: Overlaps and opportunities. Pediatr. Infect. Dis. J. 2022, 41, 139–141. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, 102–107. [Google Scholar] [CrossRef]
- Zimmermann, P.; Pittet, L.F.; Curtis, N. How common is long COVID in children and adolescents? Pediatr. Infect. Dis. J. 2021, 40, 482–487. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta. Paediatr. 2021, 110, 914–921. [Google Scholar] [CrossRef]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Vincenzo, J.D.D.; Cao, B.; et al. Fatigue and cognitive impairment in post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef]
- Nasserie, T.; Hittle, M.; Goodman, S.N. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: A systematic review. JAMA. Netw. Open. 2021, 4, e2111417. [Google Scholar] [CrossRef]
- Gibson, E.M.; Monje, M. Microglia in cancer therapy-related cognitive impairment. Trends. Neurosci. 2021, 44, 441–451. [Google Scholar] [CrossRef]
- Wong, T.L.; Weitzer, D. Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology. Medicina 2021, 57, 418. [Google Scholar] [CrossRef]
- Gibson, E.M.; Monje, M. Emerging mechanistic underpinnings and therapeutic targets for chemotherapy-related cognitive impairment. Curr. Opin. Oncol. 2019, 31, 531–539. [Google Scholar] [CrossRef]
- Gibson, E.M.; Nagaraja, S.; Ocampo, A.; Tam, L.T.; Wood, L.S.; Pallegar, P.N.; Greene, J.J.; Geraghty, A.C.; Goldstein, A.K.; Ni, L.; et al. Methotrexate chemotherapy induces persistent tri-glial dysregulation that underlies chemotherapy-related cognitive impairment. Cell 2019, 176, 43–55.e13. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Ren, J.; Li, X.; Li, J.; Chen, S. Parents’ personality, parenting stress, and problem behaviors of children with special needs in China before and during the COVID-19 pandemic. Curr. Psychol. 2022, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Polónyiová, K.; Rašková, B.; Ostatníková, D. Changes in mental health during three waves of the COVID-19 pandemic in Slovakia: Neurotypical children versus children with autism spectrum disorder and their parents. Int. J. Environ. Res. Public Health. 2022, 19, 11849. [Google Scholar] [CrossRef] [PubMed]
- Rosen, N.E.; Lord, C.; Volkmar, F.R. The diagnosis of autism: From Kanner to DSM-III to DSM-5 and beyond. J. Autism Dev. Disord. 2021, 51, 4253–4270. [Google Scholar] [CrossRef] [PubMed]
- Jyonouchi, H.; Geng, L. Associations between monocyte and T cell cytokine profiles in autism spectrum disorders: Effects of dysregulated innate immune responses on adaptive responses to recall antigens in a subset of ASD children. Int. J. Mol. Sci. 2019, 20, 4731. [Google Scholar] [CrossRef]
- Eom, T.H.; Lee, H.S.; Jang, P.S.; Kim, Y.H. Valproate-induced panhypogammaglobulinemia. Neurol Sci. 2013, 34, 1003–1004. [Google Scholar] [CrossRef]
- Goldstein, H.E.; Hauptman, J.S. The putative role of mTOR inhibitors in non-tuberous sclerosis complex-related epilepsy. Front Neurol. 2021, 12, 639319. [Google Scholar] [CrossRef]
- Steinman, G.; Mankuta, D. Antepartum COVID-19 and postpartum autism. Austin J. Clin. Neurol. 2021, 8, 1149. [Google Scholar]
- Premraj, L.; Kannapadi, N.V.; Briggs, J.; Seal, S.M.; Battaglini, D.; Fanning, J.; Suen, J.; Robba, C.; Fraser, J.; Cho, S.M. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J. Neurol Sci. 2022, 434, 120162. [Google Scholar] [CrossRef]
- Savino, R.; Carotenuto, M.; Polito, A.N.; Noia, S.D.; Albenzio, M.; Scarinci, A.; Ambrosi, A.; Sessa, F.; Tartaglia, N.; Messina, G. Analyzing the potential biological determinants of autism spectrum disorder: From neuroinflammation to the kynurenine pathway. Brain. Sci. 2020, 10, 631. [Google Scholar] [CrossRef] [PubMed]
- Komada, M.; Nishimura, Y. Epigenetics and neuroinflammation associated with neurodevelopmental disorders: A microglial perspective. Front Cell Dev. Biol. 2022, 10, 852752. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Castaneda, A.; Lu, P.; Geraghty, A.C.; Song, E.; Lee, M.H.; Wood, J.; O’Dea, M.R.; Dutton, S.; Shamardani, K.; Nwangwu, K.; et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell 2022, 185, 2452–2468.e16. [Google Scholar] [CrossRef] [PubMed]
- Sefik, E.; Qu, R.; Junqueira, C.; Kaffe, E.; Mirza, H.; Zhao, J.; Brewer, J.R.; Han, A.; Steach, H.R.; Israelow, B.; et al. Inflammasome activation in infected macrophages drives COVID-19 pathology. Nature 2022, 606, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Ryan, F.J.; Hope, C.M.; Masavuli, M.G.; Lynn, M.A.; Mekonnen, Z.A.; Yeow, A.E.L.; Garcia-Valtanen, P.; Al-Delfi, Z.; Gummow, J.; Ferguson, C.; et al. Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection. BMC Med. 2022, 20, 26. [Google Scholar] [CrossRef]
- Mehandru, S.; Merad, M. Pathological sequelae of long-haul COVID. Nature Immunology. 2022, 23, 194–202. [Google Scholar] [CrossRef]
- Toro-Huamanchumo, C.J.; Benites-Meza, J.K.; Mamani-Garcia, C.S.; Bustamante-Paytan, D.; Garcia-Ramos, A.E.; Diaz-Vélez, C.; Baroza, J.J. Efficacy of colchicine in the treatment of COVID-19 patients: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 2615. [Google Scholar] [CrossRef]
- Bonaventura, A.; Vecchié, A.; Dagna, L.; Tangianu, F.; Abbate, A.; Dentali, F. Colchicine for COVID-19: Targeting NLRP3 inflammasome to blunt hyperinflammation. Inflamm. Res. 2022, 71, 293–307. [Google Scholar] [CrossRef]
- Mansouri, N.; Marjani, M.; Tabarsi, P.; von Garnier, C.; Mansouri, D. Successful treatment of Covid-19 associated cytokine release syndrome with colchicine. A case report and review of literature. Immunol. Investig. 2021, 50, 884–890. [Google Scholar] [CrossRef]
- Naik, R.R.; Shakya, A.K.; Aladwan, S.M.; Eltanani, M. Kinase inhibitors as potential therapeutic agents in the treatment of COVID-19. Front. Pharmacol. 2022, 13, 806568. [Google Scholar] [CrossRef]
- Chatterjee, B.; Thakur, S.S. Remdesivir and its combination with repurposed drugs as COVID-19 therapeutics. Front. Immunol. 2022, 13, 830990. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jyonouchi, H.; Geng, L.; Rossignol, D.A.; Frye, R.E. Long COVID Syndrome Presenting as Neuropsychiatric Exacerbations in Autism Spectrum Disorder: Insights for Treatment. J. Pers. Med. 2022, 12, 1815. https://doi.org/10.3390/jpm12111815
Jyonouchi H, Geng L, Rossignol DA, Frye RE. Long COVID Syndrome Presenting as Neuropsychiatric Exacerbations in Autism Spectrum Disorder: Insights for Treatment. Journal of Personalized Medicine. 2022; 12(11):1815. https://doi.org/10.3390/jpm12111815
Chicago/Turabian StyleJyonouchi, Harumi, Lee Geng, Daniel A. Rossignol, and Richard E. Frye. 2022. "Long COVID Syndrome Presenting as Neuropsychiatric Exacerbations in Autism Spectrum Disorder: Insights for Treatment" Journal of Personalized Medicine 12, no. 11: 1815. https://doi.org/10.3390/jpm12111815
APA StyleJyonouchi, H., Geng, L., Rossignol, D. A., & Frye, R. E. (2022). Long COVID Syndrome Presenting as Neuropsychiatric Exacerbations in Autism Spectrum Disorder: Insights for Treatment. Journal of Personalized Medicine, 12(11), 1815. https://doi.org/10.3390/jpm12111815






