Ilizarov Bone Transfer for Treatment of Large Tibial Bone Defects: Clinical Results and Management of Complications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Technique
2.3. Statistical Analysis
3. Results
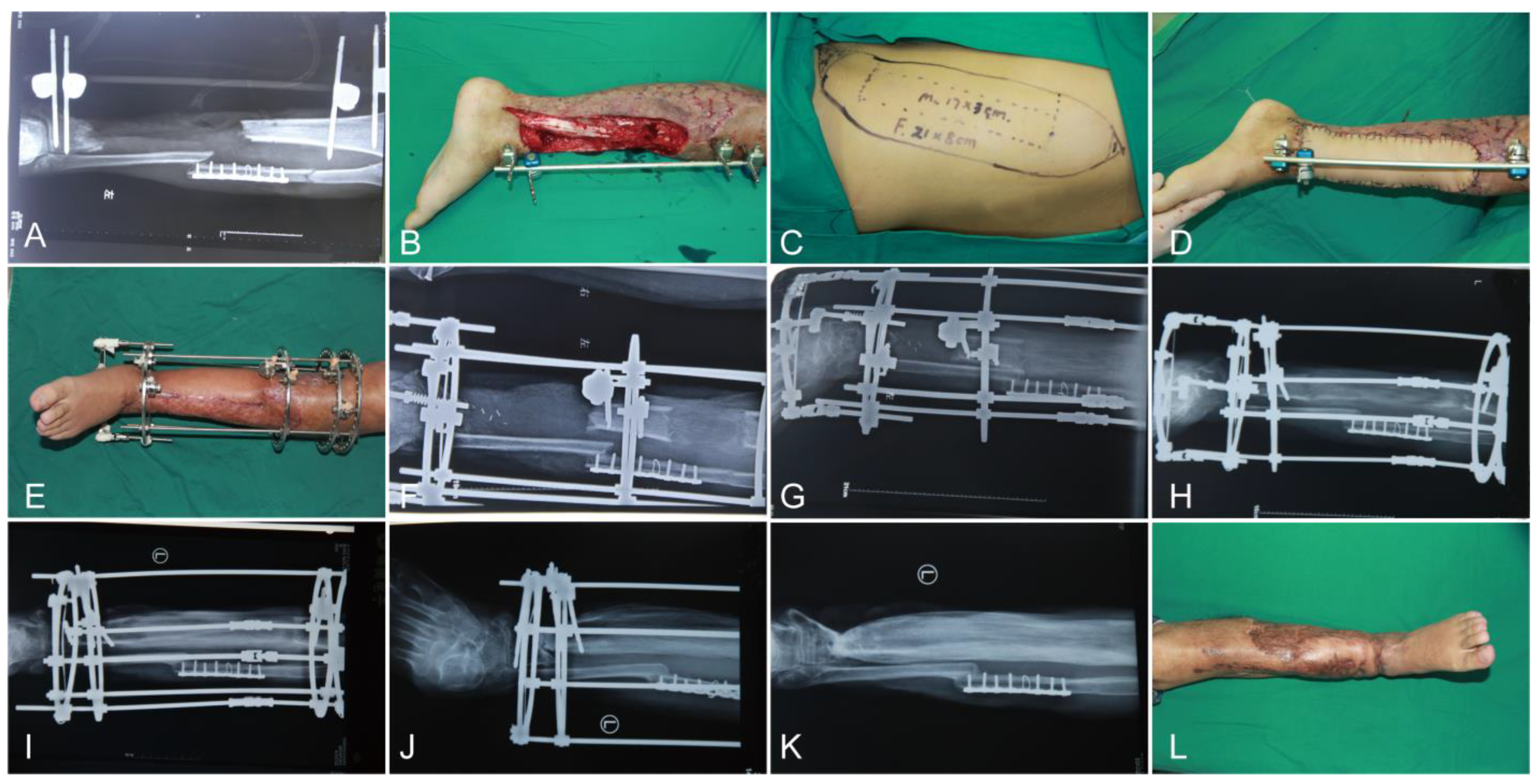
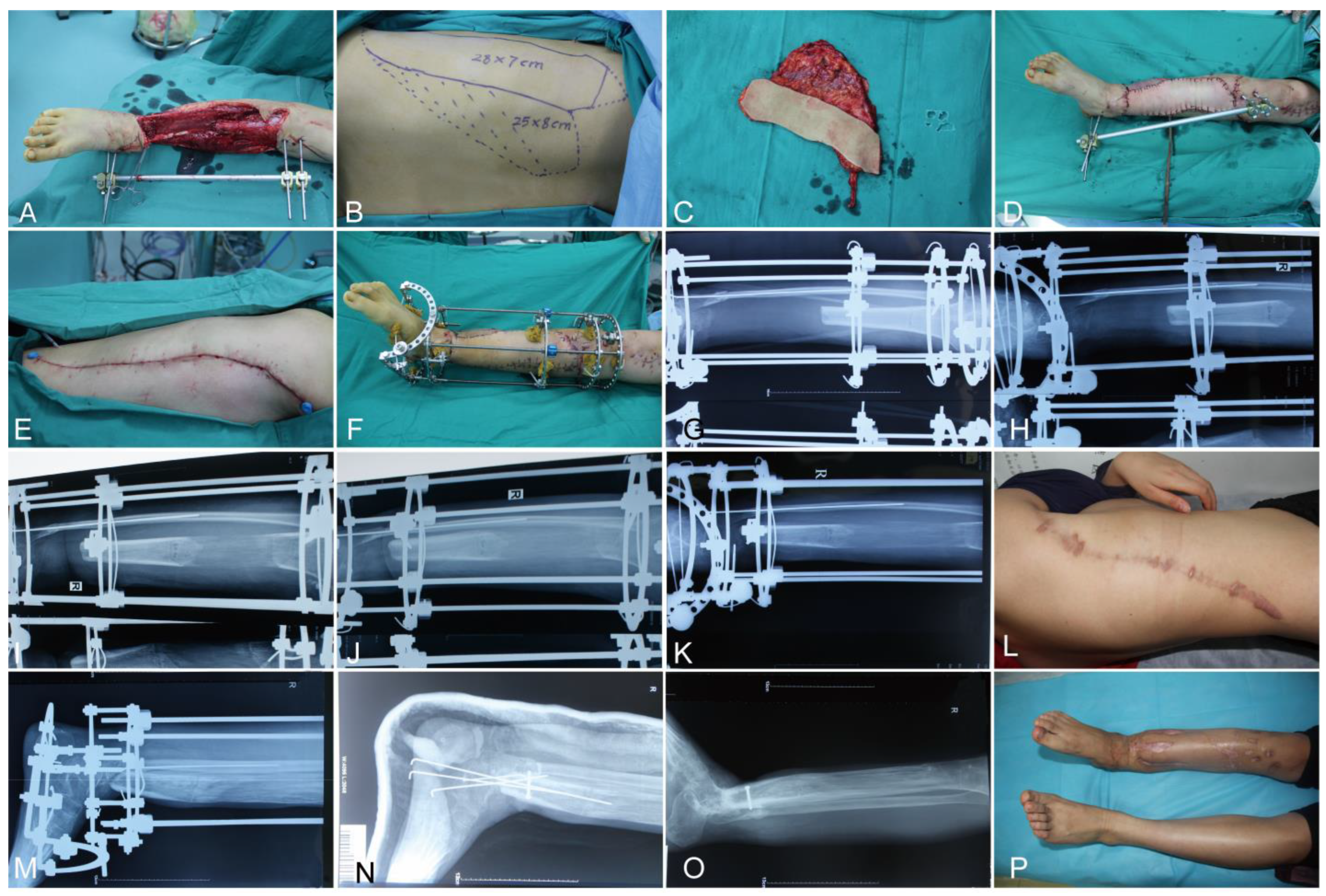
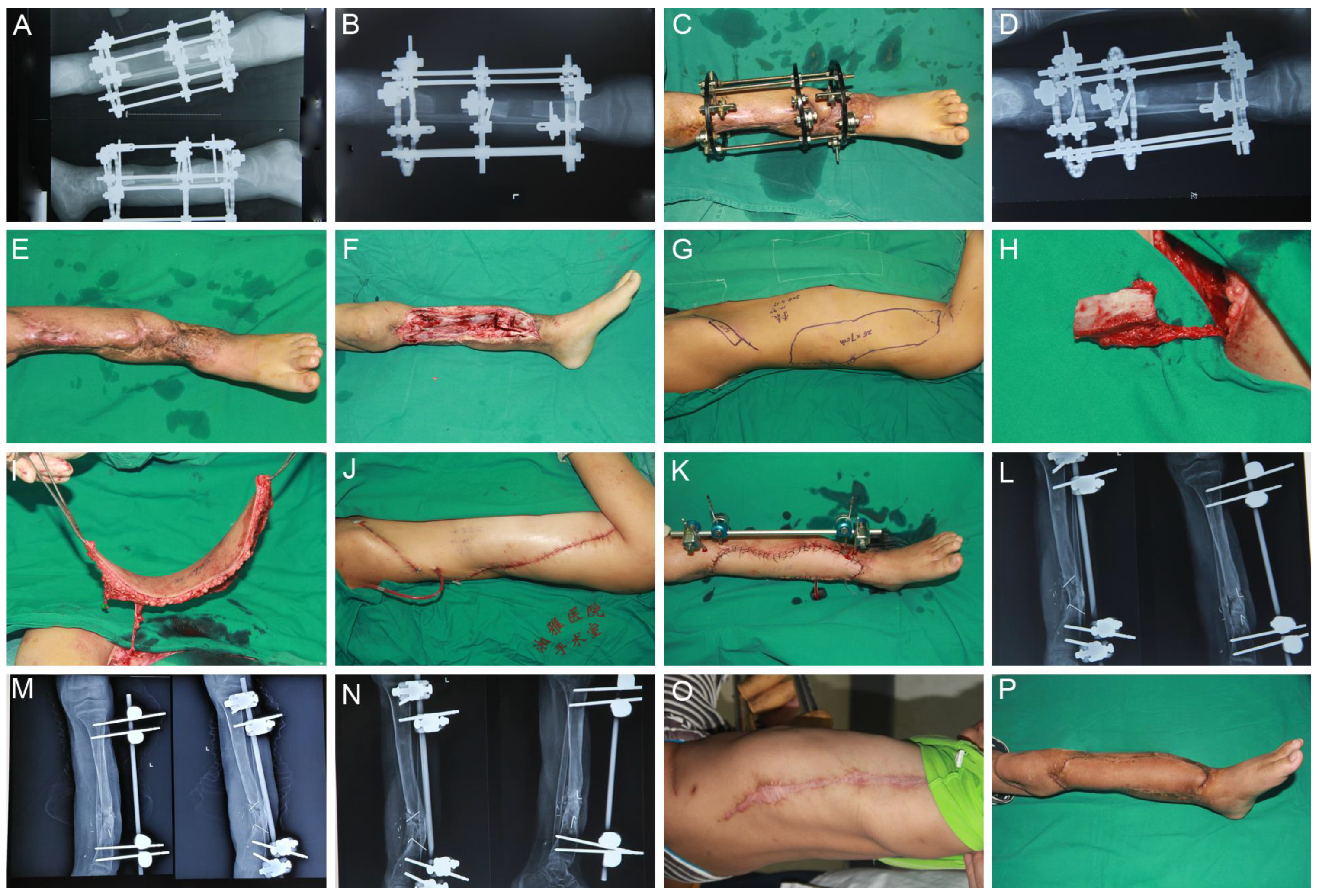
4. Case Report
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kadhim, M.; Holmes, L.; Gesheff, M.G.; Conway, J.D. Treatment Options for Nonunion with Segmental Bone Defects: Systematic Review and Quantitative Evidence Synthesis. J. Orthop. Trauma 2017, 31, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Bosse, M.J.; MacKenzie, E.J.; Kellam, J.F.; Burgess, A.R.; Webb, L.X.; Swiontkowski, M.F.; Sanders, R.W.; Jones, A.L.; McAndrew, M.P.; Patterson, B.M.; et al. An Analysis of Outcomes of Reconstruction or Amputation after Leg-Threatening Injuries. N. Engl. J. Med. 2002, 347, 1924–1931. [Google Scholar] [CrossRef] [PubMed]
- Pang, X.; Cao, Z.; Wu, P.; Tang, J.; Zhou, Z.; Yu, F.; Zeng, L.; Xiao, Y.; Pan, D.; Liu, R. Outcomes of free anterolateral thigh perforator flaps versus free modified latissimus dorsi myocutaneous flaps for Gustilo type IIIB open tibial fractures with necrosis and in-fection. Am. J. Transl Res. 2020, 12, 5836–5843. [Google Scholar] [PubMed]
- Hsieh, F.; Leow, O.Q.Y.; Cheong, C.-F.; Hung, S.-Y.; Tsao, C.-K. Musculoseptocutaneous Perforator of Anterolateral Thigh Flap: A Clinical Study. Plast. Reconstr. Surg. 2020, 147, 103e–110e. [Google Scholar] [CrossRef] [PubMed]
- Mericli, A.F.; Szpalski, C.; Schaverien, M.V.; Selber, J.C.; Adelman, D.M.; Garvey, P.B.; Villa, M.T.; Robb, G.; Baumann, D.P. The Latissimus Dorsi Myocutaneous Flap Is a Safe and Effective Method of Partial Breast Reconstruction in the Setting of Breast-Conserving Therapy. Plast. Reconstr. Surg. 2019, 143, 927e–935e. [Google Scholar] [CrossRef]
- Sanders, P.; Spierings, J.; Albergo, J.; Bus, M.; Fiocco, M.; Farfalli, G.; van de Sande, M.; Aponte-Tinao, L.; Dijkstra, P. Long-Term Clinical Outcomes of Intercalary Allograft Reconstruction for Lower-Extremity Bone Tumors. J. Bone Jt. Surg. 2020, 102, 1042–1049. [Google Scholar] [CrossRef]
- Myeroff, C.; Archdeacon, M. Autogenous Bone Graft: Donor Sites and Techniques. J. Bone Jt. Surg. 2011, 93, 2227–2236. [Google Scholar] [CrossRef]
- Li, Y.; Shao, Z.; Zhu, Y.; Liu, B.; Wu, T. Virtual Surgical Planning for Successful Second-Stage Mandibular Defect Reconstruction Using Vascularized Iliac Crest Bone Flap. Ann. Plast. Surg. 2020, 84, 183–187. [Google Scholar] [CrossRef]
- Khira, Y.M.; Badawy, H.A. Pedicled vascularized fibular graft with Ilizarov external fixator for reconstructing a large bone defect of the tibia after tumor resection. J. Orthop. Traumatol. 2013, 14, 91–100. [Google Scholar] [CrossRef] [Green Version]
- Eward, W.C.; Kontogeorgakos, V.; Levin, L.S.; Brigman, B.E. Free Vascularized Fibular Graft Reconstruction of Large Skeletal Defects after Tumor Resection. Clin. Orthop. Relat. Res. 2010, 468, 590–598. [Google Scholar] [CrossRef]
- Quinnan, S.M. Segmental Bone Loss Reconstruction Using Ring Fixation. J. Orthop. Trauma 2017, 31 (Suppl. 5), S42–S46. [Google Scholar] [CrossRef] [PubMed]
- Abdou, S.A.; Stranix, J.T.; Daar, D.A.; Mehta, D.D.; McLaurin, T.; Tejwani, N.; Saadeh, P.B.; Levine, J.P.; Leucht, P.; Thanik, V.D. Free Tissue Transfer with Distraction Osteogenesis and Masquelet Technique Is Effective for Limb Salvage in Patients with Gustilo Type IIIB Open Fractures. Plast. Reconstr. Surg. 2020, 145, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- Zhen, P.; Hu, Y.-Y.; Luo, Z.-J.; Liu, X.-Y.; Lu, H.; Li, X.-S. One-Stage Treatment and Reconstruction of Gustilo Type III Open Tibial Shaft Fractures with a Vascularized Fibular Osteoseptocutaneous Flap Graft. J. Orthop. Trauma 2010, 24, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Rozbruch, S.R.; Weitzman, A.M.; Watson, J.T.; Freudigman, P.; Katz, H.V.; Ilizarov, S. Simultaneous Treatment of Tibial Bone and Soft-tissue Defects with the Ilizarov Method. J. Orthop. Trauma 2006, 20, 194–202. [Google Scholar] [CrossRef]
- Li, R.; Zeng, C.; Yuan, S.; Chen, Y.; Zhao, S.; Ren, G.-H. Free flap transplantation combined with Ilizarov bone transport for the treatment of severe composite tibial and soft tissue defects. J. Int. Med Res. 2021, 49, 03000605211017618. [Google Scholar] [CrossRef]
- Hollenbeck, S.T.; Woo, S.; Ong, S.; Fitch, R.D.; Erdmann, D.; Levin, L.S. The Combined Use of the Ilizarov Method and Microsurgical Techniques for Limb Salvage. Ann. Plast. Surg. 2009, 62, 486–491. [Google Scholar] [CrossRef]
- Aktuglu, K.; Erol, K.; Vahabi, A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: A narrative review. J. Orthop. Traumatol. 2019, 20, 22. [Google Scholar] [CrossRef] [Green Version]
- Krappinger, D.; Irenberger, A.; Zegg, M.; Huber, B. Treatment of large posttraumatic tibial bone defects using the Ilizarov method: A subjective outcome assessment. Arch. Orthop. Trauma Surg. 2013, 133, 789–795. [Google Scholar] [CrossRef]
- Ilizarov, G.A.; Ledyaev, V.I. The replacement of long tubular bone defects by lengthening distraction osteotomy of one of the fragments. 1969. Clin. Orthop. Relat. Res. 1992, 280, 7–10. [Google Scholar] [CrossRef]
- El-Alfy, B.S.; Maaty, M.; Niazy, T. Reconstruction of infected nonunion of the distal humerus by Ilizarov external fixator. Injury 2020, 52, 1418–1422. [Google Scholar] [CrossRef]
- Paley, D.; Catagni, M.A.; Argnani, F.; Villa, A.; Benedetti, G.B.; Cattaneo, R. Ilizarov treatment of tibial nonunions with bone loss. Clin. Orthop. Relat. Res. 1989, 241, 146–165. [Google Scholar] [CrossRef]
- Qing, L.; Wu, P.; Yu, F.; Zhou, Z.; Tang, J. Use of a sequential chimeric perforator flap for one-stage reconstruction of complex soft tissue defects of the extremities. Microsurgery 2020, 40, 167–174. [Google Scholar] [CrossRef] [PubMed]
- van Dongen, T.T.; Huizinga, E.P.; de Kruijff, L.G.; van der Krans, A.C.; Hoogendoorn, J.M.; Leenen, L.P.; Hoencamp, R. Amputation: Not a failure for severe lower extremity combat injury. Injury 2017, 48, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Zheng, C.; Wang, B.; Qiu, Y.; Zhang, Z.; Li, H.; Wang, X. Reconstruction of complex soft-tissue defects in the extremities with chimeric anterolateral thigh perforator flap. Int. J. Surg. 2016, 26, 25–31. [Google Scholar] [CrossRef]
- Chai, Y.-M.; Wang, C.-Y.; Zeng, B.-F.; Chen, Z.-G.; Cai, P.-H.; Kang, Q.-L.; Ruan, H.-J. Peroneal artery perforator chimeric flap for reconstruction of composite defects in extremities. Microsurgery 2010, 30, 199–206. [Google Scholar] [CrossRef]
- Massarelli, O.; Gobbi, R.; Biglio, A.; Soma, D.; Tullio, A. Chimeric Lateral Supramalleolar Artery Perforator Fibula Free Flap in the Reconstruction of Composite Head and Neck Defects. Plast. Reconstr. Surg. 2014, 133, 130–136. [Google Scholar] [CrossRef]
- Hwang, J.H.; Kim, E.S.; Kim, K.S.; Kim, D.Y.; Lee, S.Y. Latissimus Dorsi Muscle and Its Short Perforator-Based Skin Compound Free Flap. Ann. Plast. Surg. 2007, 58, 381–387. [Google Scholar] [CrossRef]
- Tee, R.; Jeng, S.-F.; Chen, C.-C.; Shih, H.-S. The medial sural artery perforator pedicled propeller flap for coverage of middle-third leg defects. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1971–1978. [Google Scholar] [CrossRef]
- Nazerali, R.; Pu, L.L. Free Tissue Transfer to the Lower Extremity. Ann. Plast. Surg. 2013, 70, 419–422. [Google Scholar] [CrossRef] [Green Version]
- Testa, G.; Vescio, A.; Aloj, D.C.; Costa, D.; Papotto, G.; Gurrieri, L.; Sessa, G.; Pavone, V. Treatment of Infected Tibial Non-Unions with Ilizarov Technique: A Case Series. J. Clin. Med. 2020, 9, 1352. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Y.; Di, J.; Peng, A. Double-level bone transport for large post-traumatic tibial bone defects: A single centre experience of sixteen cases. Int. Orthop. 2018, 42, 1157–1164. [Google Scholar] [CrossRef] [PubMed]
- Yin, P.; Zhang, L.; Li, T.; Zhang, L.; Wang, G.; Li, J.; Liu, J.; Zhou, J.; Zhang, Q.; Tang, P. Infected nonunion of tibia and femur treated by bone transport. J. Orthop. Surg. Res. 2015, 10, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Cierny, G., 3rd; Zorn, K.E. Segmental tibial defects. Comparing conventional and Ilizarov methodologies. Clin. Orthop. Relat. Res. 1994, 301, 118–123. [Google Scholar]
- Li, R.; Zhu, G.; Chen, C.; Chen, Y.; Ren, G. Bone Transport for Treatment of Traumatic Composite Tibial Bone and Soft Tissue Defects: Any Specific Needs besides the Ilizarov Technique? BioMed Res. Int. 2020, 2020, 2716547. [Google Scholar] [CrossRef]
- Rosteius, T.; Pätzholz, S.; Rausch, V.; Lotzien, S.; Behr, B.; Lehnhardt, M.; Schildhauer, T.A.; Seybold, D.; Geßmann, J. Ilizarov bone transport using an intramedullary cable transportation system in the treatment of tibial bone defects. Injury 2021, 52, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shen, S.; Xiao, Q.; Wang, G.; Yang, H.; Zhao, H.; Shu, B.; Zhuo, N. Efficacy comparison of double-level and single-level bone transport with Orthofix fixator for treatment of tibia fracture with massive bone defects. Int. Orthop. 2020, 44, 957–963. [Google Scholar] [CrossRef]
- Borzunov, D.Y. Long bone reconstruction using multilevel lengthening of bone defect fragments. Int. Orthop. 2012, 36, 1695–1700. [Google Scholar] [CrossRef] [Green Version]
- Ju, J.; Li, L.; Zhou, R.; Hou, R. Combined application of latissimus dorsi myocutaneous flap and iliac bone flap in the treatment of chronic osteomyelitis of the lower extremity. J. Orthop. Surg. Res. 2018, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Kimata, Y.; Uchiyama, K.; Sakuraba, M.; Ebihara, S.; Hayashi, R.; Asakage, T.; Nakatsuka, T.; Harii, K. Deep circumflex iliac perforator flap with iliac crest for mandibular reconstruction. Br. J. Plast. Surg. 2001, 54, 487–490. [Google Scholar] [CrossRef]
- Taylor, G.I.; Watson, N. One-stage repair of compound leg defects with free, revascularized flaps of groin skin and iliac bone. Plast. Reconstr. Surg. 1978, 61, 494–506. [Google Scholar] [CrossRef]
- Lei, P.; Du, W.; Liu, H.; Wu, P.; Zhou, Z.; Yu, F.; Qing, L.; Pan, D.; Liu, R.; Zeng, L.; et al. Free vascularized iliac bone flap based on deep circumflex iliac vessels graft for the treatment of osteonecrosis of femoral head. J. Orthop. Surg. Res. 2019, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
| Variable | Ilizarov Group (N = 72) |
|---|---|
| Defect size (cm2) | 198.8 ± 50.8 |
| Flap size (cm2) | 209.4 ± 52.9 |
| Soft tissue repair | |
| ALTP | 24 |
| LD | 32 |
| Other * | 16 |
| Flap harvested time (min) | 74.0 ± 20.2 |
| Operative time (min) | 275.8 ± 55.1 |
| Flap complications | |
| Total flap necrosis Partial flap necrosis Subcutaneous ulcer | 2 5 2 |
| Factors of flap necrosis | |
| Vascular crisis | 5 |
| Infection | 2 |
| Hematoma | 2 |
| Donor site morbidity | |
| Delayed wound healing | 2 |
| Variable | Ilizarov Group (N = 72) |
|---|---|
| Operative time (min) | 60.6 ± 8.4 |
| Bone defect length (cm) | 10.6 ± 3.3 |
| External fixator carrying time (months) | 21.3 ± 5.6 |
| External fixation index (d/cm) | 62.4 ± 11.2 |
| Bone healing time (months) | 23.3 ± 5.6 |
| No longer tolerable | 21 |
| Deep pin tract infection | 3 |
| Reoperation | 13 |
| ASAMI functional results | |
| Excellent | 30 |
| Good | 21 |
| Fair | 14 |
| Poor | 7 |
| ASAMI bone results | |
| Excellent | 46 |
| Good | 19 |
| Fair | 2 |
| Poor | 5 |
| Cosmetic evaluation | |
| Subjectively a | |
| Excellent | 20 |
| Good | 31 |
| Moderate | 16 |
| Poor | 5 |
| Objectively b | |
| Excellent | 19 |
| Good | 30 |
| Moderate | 17 |
| Poor | 6 |
| Variable | No. of Patients (N = 72) | Bone Defect Length (cm)/p-Value | Bone Healing Time (Months)/p-Value |
|---|---|---|---|
| Age (years) | 0.001 | 0.001 | |
| <18 | 13 | 7.5 ± 1.8 | 17.7 ± 3.7 |
| ≥18 | 59 | 11.3 ± 3.1 | 24.5 ± 5.1 |
| Age (years) | - | 0.025 | |
| <18 | 13 | (5–10) | 17.7 ± 3.7 |
| ≥18 | 26 | (5–10) | 20.5 ± 3.5 |
| Gender | 0.225 | 0.092 | |
| Male | 63 | 10.8 ± 3.0 | 23.7 ± 5.2 |
| Female | 9 | 9.3 ± 4.7 | 20.3 ± 7.3 |
| BMI | 0.722 | 0.518 | |
| Normal | 44 | 10.5 ± 3.1 | 22.9 ± 5.2 |
| Abnormal | 28 | 10.8 ± 3.5 | 23.8 ± 6.1 |
| Smoking history | 0.447 | 0.194 | |
| No | 44 | 10.3 ± 3.6 | 22.6 ± 5.4 |
| Yes | 28 | 10.9 ± 2.7 | 24.3 ± 5.7 |
| Drinking history | 0.606 | 0.273 | |
| No | 49 | 10.4 ± 3.6 | 22.8 ± 5.4 |
| Yes | 23 | 10.9 ± 2.6 | 24.3 ± 6.5 |
| Bone defect length (cm) | 0.001 | 0.001 | |
| 4–8 | 18 | 6.7 ± 1.1 | 16.7 ± 2.9 |
| >8–12 | 29 | 9.7 ± 1.1 | 22.8 ± 2.6 |
| >12 | 25 | 14.4 ± 1.5 | 28.5 ± 4.1 |
| Soft tissue defect size (cm2) | 0.001 | 0.001 | |
| <180 | 25 | 7.8 ± 2.0 | 19.6 ± 5.0 |
| ≥180 | 47 | 12.0 ± 2.9 | 25.2 ± 4.9 |
| Postoperative complications | 0.030 | 0.001 | |
| No | 59 | 10.2 ± 3.1 | 21.8 ± 4.4 |
| Yes & | 13 | 12.3 ± 3.7 | 29.6 ± 5.8 |
| No | Age/Sex | Cause of Injury | Bone Defect Location/Length (cm) | Wound Coverage | Initial Treatment Time (Months) | Reasons for Reoperation | Treatment Measures | Bone Healing Time (Months) | Total Disease Duration (Months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 8/M | Traffic accident | Left leg/7 | ALTP (184 cm2) + Skin grafts | 18 | Scar hyperplasia contractures, nonunion of fracture, and intolerability | LD (175 cm2) + VIBF (5 cm) | 4 | 22 |
| 2 | 38/M | Traffic accident | Right leg/10 | LD (172 cm2) | 23 | Soft tissue incarceration and intolerability | ALTP (161.5 cm2) + VIBF (5 cm) | 6 | 29 |
| 3 | 51/M | Crush injury | Right leg/9 | ALTP (162.5 cm2) | 23 | Nonunion of fracture and intolerability | VIBF (5 cm) | 4 | 27 |
| 4 | 56/M | Traffic accident | Left leg/5 | ALTP (56 cm2) | 18 | Nonunion of fracture | SCIP (24 cm2) + VIBF (3 cm) | 7 | 23 |
| 5 | 34/F | Traffic accident | Right leg/15 | LD (180 cm2) + ALTP (126 cm2) | 31 | Soft tissue incarceration, pin loosening, and intolerability | Replace the nail, DIEP (60 cm2) + VIBF (4 cm) | 6 | 37 |
| 6 | 42/M | Traffic accident | Left leg/13.5 | LD (196 cm2) | 31 | Soft tissue incarceration and intolerability | VIBF (5 cm) | 5 | 36 |
| 7 | 28/M | Traffic accident | Right leg/14 | LD (160 cm2) + ALTP (133 cm2) | 30 | Soft tissue incarceration and intolerability | VIBF (5 cm) | 5 | 35 |
| 8 | 57/M | Agricultural accident | Right leg/13 | LD (161 cm2) | 25 | Nonunion of fracture and intolerability | VIBF (5 cm) | 7 | 32 |
| 9 | 20/M | Traffic accident | Left leg/18 | LD (189 cm2) + ALTP (184 cm2) | 30 | Deep pin tract infection, pin loosening, nonunion of fracture, and intolerability | Replace the nail, VIBF (5 cm) | 4 | 34 |
| 10 | 27/M | Traffic accident | Left leg/15 | LD (225 cm2) | 20 | Intolerability | VIBF (4 cm) | 5 | 25 |
| 11 | 16/M | Traffic accident | Left leg/11 | ALTP (192 cm2) | 18 | Intolerability | VIBF (5 cm) | 4 | 22 |
| 12 | 47/M | Traffic accident | Left leg/16 | LD (152 cm2) + ALTP (126 cm2) | 28 | Refracture | Cancellous bone graft of the iliac crest | 9 | 37 |
| 13 | 31/M | Crush injury | Right leg/14 | LD (208 cm2) + Skin grafts | - | Deep pin tract infection and pin loosening | Replace the nail | - | 26 |
| 14 | 18/M | Traffic accident | Right leg/12 | LD (204 cm2) | - | Deep pin tract infection | - | - | 23 |
| 15 | 23/F | Traffic accident | Left leg/15.5 | LD (218.5 cm2) + ALTP (147 cm2) | - | Deep pin tract infection | - | - | 27 |
| 16 | 26/M | Traffic accident | Right leg/12.5 | ALTP (212.5 cm2) | - | Deep pin tract infection | - | - | 25 |
| Variable | Soft Tissue Defect Size (cm2) | Complication Group & (N = 13) | Non-Complication Group (N = 59) | p-Value |
|---|---|---|---|---|
| Bone defect length (cm) 4–8 >8–12 >12 | 0.001 (150.8 ± 29.9) (193.1 ± 24.2) (239.8 ± 52.8) | 0.001 2/(22.5 ± 0.7) 3/(26.0 ± 3.6) 8/(32.8 ± 4.8) 13/(29.6 ± 5.8) | 0.001 16/(16.0 ± 2.1) 26/(22.4 ± 2.3) 17/(26.5 ± 1.3) 59/(21.8 ± 4.4) | 0.001 0.022 0.007 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, Z.; Zhang, Y.; Lipa, K.; Qing, L.; Wu, P.; Tang, J. Ilizarov Bone Transfer for Treatment of Large Tibial Bone Defects: Clinical Results and Management of Complications. J. Pers. Med. 2022, 12, 1774. https://doi.org/10.3390/jpm12111774
Cao Z, Zhang Y, Lipa K, Qing L, Wu P, Tang J. Ilizarov Bone Transfer for Treatment of Large Tibial Bone Defects: Clinical Results and Management of Complications. Journal of Personalized Medicine. 2022; 12(11):1774. https://doi.org/10.3390/jpm12111774
Chicago/Turabian StyleCao, Zheming, Yiqian Zhang, Katelyn Lipa, Liming Qing, Panfeng Wu, and Juyu Tang. 2022. "Ilizarov Bone Transfer for Treatment of Large Tibial Bone Defects: Clinical Results and Management of Complications" Journal of Personalized Medicine 12, no. 11: 1774. https://doi.org/10.3390/jpm12111774
APA StyleCao, Z., Zhang, Y., Lipa, K., Qing, L., Wu, P., & Tang, J. (2022). Ilizarov Bone Transfer for Treatment of Large Tibial Bone Defects: Clinical Results and Management of Complications. Journal of Personalized Medicine, 12(11), 1774. https://doi.org/10.3390/jpm12111774








