Impact of Previous Occupational Exposure on Outcomes of Chronic Obstructive Pulmonary Disease
Abstract
1. Introduction
2. Methods and Materials
2.1. Study Design and Participants
2.2. Occupational Exposure
2.3. Spirometry and Six-Minute Walk Test
2.4. Outcomes
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics of the Study Population
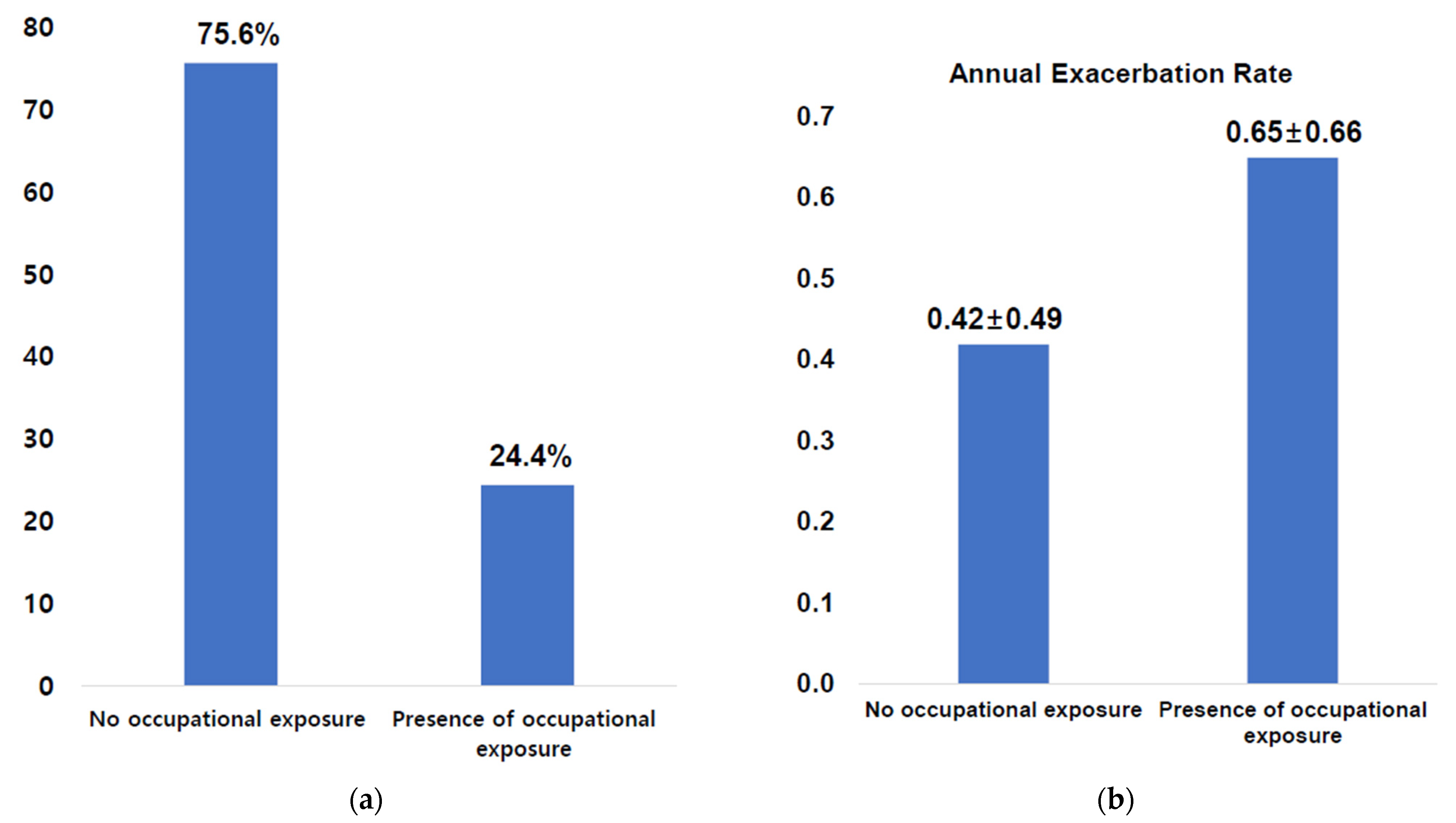
3.2. Occupational Exposure as a Risk Factor for Acute Exacerbation of COPD
3.3. Occupational Exposure as a Contributing Factor for Annual FEV1 Decline
3.4. Impact of Occupational Exposure on Quality of Life in COPD Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Materials | Number of Patients | % |
|---|---|---|
| Isocyanate, toluene di-isocyanate | 9 | 2.9 |
| Welding solvent | 5 | 1.6 |
| Wheat flour powder | 1 | 0.3 |
| Grain dust | 2 | 0.6 |
| Hair permanence drug | 1 | 0.3 |
| Other chemical material | 58 | 18.6 |
| Not exposed | 236 | 75.6 |
References
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. 2020 Report. Available online: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf (accessed on 20 November 2021).
- Decramer, M.; Janssens, W.; Miravitlles, M. Chronic obstructive pulmonary disease. Lancet 2012, 379, 1341–1351. [Google Scholar] [CrossRef]
- Zuo, L.; He, F.; Sergakis, G.G.; Koozehchian, M.S.; Stimpfl, J.N.; Rong, Y.; Diaz, P.T.; Best, T.M. Interrelated role of cigarette smoking, oxidative stress, and immune response in COPD and corresponding treatments. Am. J. Physiol. Lung Cell Mol. Physiol. 2014, 307, L205–L218. [Google Scholar] [CrossRef]
- Becklake, M.R. Occupational exposures: Evidence for a causal association with chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1989, 140 Pt 2, S85–S91. [Google Scholar] [CrossRef]
- Hnizdo, E.; Sullivan, P.A.; Bang, K.M.; Wagner, G. Airflow obstruction attributable to work in industry and occupation among U.S. race/ethnic groups: A study of NHANES III data. Am. J. Ind. Med. 2004, 46, 126–135. [Google Scholar] [CrossRef]
- Harber, P.; Tashkin, D.P.; Simmons, M.; Crawford, L.; Hnizdo, E.; Connett, J. Effect of occupational exposures on decline of lung function in early chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2007, 176, 994–1000. [Google Scholar] [CrossRef]
- Pallasaho, P.; Kainu, A.; Sovijarvi, A.; Lindqvist, A.; Piirila, P.L. Combined effect of smoking and occupational exposure to dusts, gases or fumes on the incidence of COPD. COPD 2014, 11, 88–95. [Google Scholar]
- Mehta, A.J.; Miedinger, D.; Keidel, D.; Bettschart, R.; Bircher, A.; Bridevaux, P.O.; Curjuric, I.; Kromhout, H.; Rochat, T.; Rothe, T.; et al. Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults. Am. J. Respir. Crit. Care Med. 2012, 185, 1292–1300. [Google Scholar] [CrossRef]
- Blanc, P.D.; Iribarren, C.; Trupin, L.; Earnest, G.; Katz, P.P.; Balmes, J.; Sidney, S.; Eisner, M.D. Occupational exposures and the risk of COPD: Dusty trades revisited. Thorax 2009, 64, 6–12. [Google Scholar]
- Boggia, B.; Farinaro, E.; Grieco, L.; Lucariello, A.; Carbone, U. Burden of smoking and occupational exposure on etiology of chronic obstructive pulmonary disease in workers of Southern Italy. J. Occup. Environ. Med. 2008, 50, 366–370. [Google Scholar]
- Balmes, J.; Becklake, M.; Blanc, P.; Henneberger, P.; Kreiss, K.; Mapp, C.; Milton, D.; Schwartz, D.; Toren, K.; Viegi, G.; et al. American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am. J. Respir. Crit. Care Med. 2003, 167, 787–797. [Google Scholar]
- Trupin, L.; Earnest, G.; San Pedro, M.; Balmes, J.R.; Eisner, M.D.; Yelin, E.; Katz, P.P.; Blanc, P.D. The occupational burden of chronic obstructive pulmonary disease. Eur. Respir. J. 2003, 22, 462–469. [Google Scholar] [CrossRef]
- Matheson, M.C.; Benke, G.; Raven, J.; Sim, M.R.; Kromhout, H.; Vermeulen, R.; Johns, D.P.; Walters, E.H.; Abramson, M.J. Biological dust exposure in the workplace is a risk factor for chronic obstructive pulmonary disease. Thorax 2005, 60, 645–651. [Google Scholar] [CrossRef]
- Balmes, J.R. Occupational contribution to the burden of chronic obstructive pulmonary disease. J. Occup. Environ. Med. 2005, 47, 154–160. [Google Scholar] [CrossRef]
- Park, T.S.; Lee, J.S.; Seo, J.B.; Hong, Y.; Yoo, J.W.; Kang, B.J.; Lee, S.W.; Oh, Y.-M.; Lee, S.D.; KOLD Study Group. Study Design and Outcomes of Korean Obstructive Lung Disease (KOLD) Cohort Study. Tuberc. Respir. Dis. 2014, 76, 169–174. [Google Scholar] [CrossRef]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef]
- Jones, P.W. ST George’s Respiratory Questionnaire for COPD Patients (SGRQ-C) Manual. 2016. Available online: https://www.sgul.ac.uk/research/research-operations/research-administration/st-georges-respiratory-questionnaire/docs/sgrq-c-manual-april-2012.pdf (accessed on 23 March 2018).
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef]
- Sundararajan, V.; Henderson, T.; Perry, C.; Muggivan, A.; Quan, H.; Ghali, W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004, 57, 1288–1294. [Google Scholar]
- Celli, B.R.; Cote, C.G.; Marin, J.M.; Casanova, C.; Montes de Oca, M.; Mendez, R.A.; Plata, V.P.; Cabral, H.J. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 2004, 350, 1005–1012. [Google Scholar] [CrossRef]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; van der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar]
- Choi, J.K.; Paek, D.; Lee, J.O. Normal predictive values of spirometry in Korean population. Tuberc. Respir. Dis. 2005, 58, 230–242. [Google Scholar] [CrossRef]
- Macintyre, N.; Crapo, R.O.; Viegi, G.; Johnson, D.C.; van der Grinten, C.P.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Enright, P.; et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur. Respir. J. 2005, 26, 720–735. [Google Scholar] [CrossRef] [PubMed]
- Park, J.O.; Choi, I.S.; Park, K.O. Normal predicted standards of single breath carbon monoxide diffusing capacity of lung in healthy nonsmoking adults. Korean J. Med. 1985, 28, 176–183. [Google Scholar]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Vestbo, J.; Hurd, S.S.; Agusti, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2013, 187, 347–365. [Google Scholar] [PubMed]
- Lamprecht, B.; McBurnie, M.A.; Vollmer, W.M.; Gudmundsson, G.; Welte, T.; Nizankowska-Mogilnicka, E.; Studnicka, M.; Bateman, E.; Anto, J.M.; Burney, P.; et al. COPD in never smokers: Results from the population-based burden of obstructive lung disease study. Chest 2011, 139, 752–763. [Google Scholar] [CrossRef]
- Jo, Y.S. Long-term outcome of chronic obstructive pulmonary disease: A review. Tuberc. Respir. Dis. 2022. Epub ahead of print. [Google Scholar] [CrossRef]
- Hnizdo, E.; Sullivan, P.A.; Bang, K.M.; Wagner, G. Association between chronic obstructive pulmonary disease and employment by industry and occupation in the US population: A study of data from the Third National Health and Nutrition Examination Survey. Am. J. Epidemiol. 2002, 156, 738–746. [Google Scholar] [CrossRef]
- Sadhra, S.; Kurmi, O.P.; Sadhra, S.S.; Lam, K.B.; Ayres, J.G. Occupational COPD and job exposure matrices: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 725–734. [Google Scholar] [CrossRef]
- Lopez-Campos, J.L.; Calero-Acuna, C.; Marquez-Martin, E. Frequent or Persistent Exacerbations: Identifying The Real Problem. Arch. Bronconeumol. 2016, 52, 577–578. [Google Scholar]
- Wedzicha, J.A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet 2007, 370, 786–796. [Google Scholar] [CrossRef]
- Paulin, L.M.; Diette, G.B.; Blanc, P.D.; Putcha, N.; Eisner, M.D.; Kanner, R.E.; Belli, A.J.; Christenson, S.; Tashkin, D.P.; Han, M.; et al. Occupational exposures are associated with worse morbidity in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2015, 191, 557–565. [Google Scholar] [PubMed]
- Skaaby, S.; Flachs, E.M.; Lange, P.; Schlunssen, V.; Marott, J.L.; Brauer, C.; Nordestgaard, B.G.; Sadhra, S.; Kurmi, O.; Bonde, J.P.E. Occupational exposures and exacerbations of asthma and COPD-A general population study. PLoS ONE 2020, 15, e0243826. [Google Scholar]
- Murgia, N.; Gambelunghe, A. Occupational COPD-The most under-recognized occupational lung disease? Respirology 2022, 27, 399–410. [Google Scholar] [PubMed]
- Kim, W.D. Phenotype of Chronic Obstructive Pulmonary Disease Based on Computed Tomography-Defined Underlying Pathology. Tuberc. Respir. Dis. 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, J.; Meng, Y.; Adcock, I.M.; Yao, X. Role of inflammatory cells in airway remodeling in COPD. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3341–3348. [Google Scholar]
- Donaldson, G.C.; Seemungal, T.A.; Patel, I.S.; Bhowmik, A.; Wilkinson, T.M.; Hurst, J.R.; Maccallum, P.K.; Wedzicha, J.A. Airway and systemic inflammation and decline in lung function in patients with COPD. Chest 2005, 128, 1995–2004. [Google Scholar]
- Snoeck-Stroband, J.B.; Postma, D.S.; Lapperre, T.S.; Gosman, M.M.; Thiadens, H.A.; Kauffman, H.F.; Sont, J.K.; Jansen, D.F.; Sterk, P.J. Airway inflammation contributes to health status in COPD: A cross-sectional study. Respir. Res. 2006, 7, 140. [Google Scholar]
- Kwon, H.Y.; Kim, E. Factors contributing to quality of life in COPD patients in South Korea. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 103–109. [Google Scholar] [CrossRef]
- Santos, N.C.D.; Miravitlles, M.; Camelier, A.A.; Almeida, V.D.C.; Maciel, R.; Camelier, F.W.R. Prevalence and Impact of Comorbidities in Individuals with Chronic Obstructive Pulmonary Disease: A Systematic Review. Tuberc. Respir. Dis. 2022, 85, 205–220. [Google Scholar] [CrossRef]
| Variable | Patients with Occupational Exposure (n = 76) | Patients without Occupational Exposure (n = 236) | p-Value * |
|---|---|---|---|
| Age, year | 65.6 ± 7.6 | 67.0 ± 7.5 | 0.184 |
| Female sex | 2 (2.6) | 8 (3.4) | 0.740 |
| BMI, kg/m2 | 22.6 ± 3.3 | 23.2 ± 3.28 | 0.183 |
| mMRC dyspnea grade | 1.84 ± 1.0 | 1.61 ± 1.0 | 0.105 |
| Current smoker | 24 (32.0) | 76 (33.3) | 0.539 |
| Education level, college or more | 8 (10.5) | 54 (22.9) | 0.012 |
| Quality of life | |||
| CAT score, total | 17.4 ± 8.6 | 14.6 ± 8.9 | 0.316 |
| SGRQ-c total | 39.7 ± 18.8 | 33.1 ± 17.6 | 0.005 |
| 6MWD, m | 419.9 ± 85.4 | 436.6 ± 86.8 | 0.132 |
| BODE index | 2.43 ± 2.2 | 2.15 ± 1.9 | 0.275 |
| mCCI | 0.36 ± 0.7 | 0.29 ± 0.5 | 0.398 |
| Post-BD spirometric values | |||
| FVC, L | 3.45 ± 0.78 | 3.47 ± 0.79 | 0.844 |
| FVC, % of predicted value | 89.8 ± 18.4 | 91.8 ± 18.1 | 0.403 |
| FEV1, L | 1.61 ± 0.62 | 1.62 ± 0.53 | 0.901 |
| FEV1, % of predicted value | 59.0 ± 19.7 | 60.9 ± 18.4 | 0.440 |
| FEV1/FVC ratio (%) | 46.4 ± 12.4 | 46.8 ± 10.6 | 0.832 |
| DLCO, % predicted | 74.5 ± 22.8 | 79.6 ± 24.8 | 0.117 |
| Emphysema index | 25.1 ± 16.3 | 22.7 ± 15.4 | 0.335 |
| Acute exacerbation | |||
| Exacerbations in the previous year ≥ 1 | 23 (30.3) | 41 (17.5) | 0.017 |
| Follow-up period after register, month | 54.2 ± 22.5 | 56.5 ± 24.5 | 0.482 |
| Presence of exacerbation during the follow-up period | 48 (69.6) | 148 (67.6) | 0.758 |
| Model 1 * | Model 2 † | |||||
|---|---|---|---|---|---|---|
| Factor | OR ‡ | 95% CI | p Value | OR ‡ | 95% CI | p Value |
| Presence of occupational exposure | 1.714 | 1.253–2.346 | 0.001 | 1.418 | 1.027–1.956 | 0.033 |
| Sex (female for male) | 1.531 | 0.867–2.705 | 0.142 | 1.601 | 0.830–3.088 | 0.160 |
| Age, an increase by 1 | 0.998 | 0.977–1.019 | 0.888 | 0.995 | 0.974–1.017 | 0.696 |
| Smoking status (never or ex-smoking for current smoking) | 0.921 | 0.677–1.252 | 0.601 | 0.860 | 0.638–1.158 | 0.322 |
| BODE index, an increase by 1 | 1.147 | 1.065–1.235 | <0.001 | 1.031 | 0.966–1.775 | 0.476 |
| Acute exacerbation in the previous year | 1.495 | 1.093–2.045 | 0.012 | 1.309 | 0.966–1.775 | 0.082 |
| mCCI, an increase by 1 | - | - | - | 1.145 | 0.945–1.387 | 0.116 |
| SGRQ-c total score, an increase by 1 | - | - | - | 1.019 | 1.010–1.028 | <0.001 |
| Factor (Baseline) | Estimated β (SE) | p Value * |
|---|---|---|
| Occupational Exposure | −0.519 (0.199) | 0.009 |
| Sex (female) | −0.499 (0.094) | <0.001 |
| Age | −0.021 (0.002) | <0.001 |
| Current smoking | 0.006 (0.038) | 0.807 |
| Baseline postBD-FEV1 | 0.020 (0.001) | <0.001 |
| History of exacerbation in the previous year | −0.015 (0.044) | 0.736 |
| BMI | 0.009 (0.006) | 0.119 |
| Emphysema index | −0.003 (0.001) | 0.012 |
| 6MWD | 0.001 (0.001) | 0.092 |
| Factor (Baseline) | Estimated β (SE) | p Value * |
|---|---|---|
| Occupational Exposure | 1.986 (2.752) | 0.471 |
| Sex (female) | 9.047 (5.138) | 0.080 |
| Age | 0.147 (0.139) | 0.916 |
| Current smoking | 3.561 (2.088) | 0.090 |
| Baseline postBD-FEV1 | −0.169 (0.056) | 0.003 |
| History of exacerbation in the previous year | 5.586 (2.414) | 0.022 |
| BMI | 0.290 (0.342) | 0.397 |
| Emphysema index | 0.325 (0.075) | <0.001 |
| 6MWD | −0.058 (0.012) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Park, T.S.; Kim, T.-H.; Rhee, C.K.; Kim, C.; Lee, J.S.; Kim, W.J.; Lim, S.Y.; Park, Y.B.; Yoo, K.H.; et al. Impact of Previous Occupational Exposure on Outcomes of Chronic Obstructive Pulmonary Disease. J. Pers. Med. 2022, 12, 1592. https://doi.org/10.3390/jpm12101592
Kim Y, Park TS, Kim T-H, Rhee CK, Kim C, Lee JS, Kim WJ, Lim SY, Park YB, Yoo KH, et al. Impact of Previous Occupational Exposure on Outcomes of Chronic Obstructive Pulmonary Disease. Journal of Personalized Medicine. 2022; 12(10):1592. https://doi.org/10.3390/jpm12101592
Chicago/Turabian StyleKim, Youlim, Tai Sun Park, Tae-Hyung Kim, Chin Kook Rhee, Changhwan Kim, Jae Seung Lee, Woo Jin Kim, Seong Yong Lim, Yong Bum Park, Kwang Ha Yoo, and et al. 2022. "Impact of Previous Occupational Exposure on Outcomes of Chronic Obstructive Pulmonary Disease" Journal of Personalized Medicine 12, no. 10: 1592. https://doi.org/10.3390/jpm12101592
APA StyleKim, Y., Park, T. S., Kim, T.-H., Rhee, C. K., Kim, C., Lee, J. S., Kim, W. J., Lim, S. Y., Park, Y. B., Yoo, K. H., Lee, S.-D., Oh, Y.-M., & Moon, J.-Y. (2022). Impact of Previous Occupational Exposure on Outcomes of Chronic Obstructive Pulmonary Disease. Journal of Personalized Medicine, 12(10), 1592. https://doi.org/10.3390/jpm12101592







