Decrease in Sleep Duration and Poor Sleep Quality over Time Is Associated with an Increased Risk of Incident Non-Alcoholic Fatty Liver Disease
Abstract
:1. Introduction
2. Methods
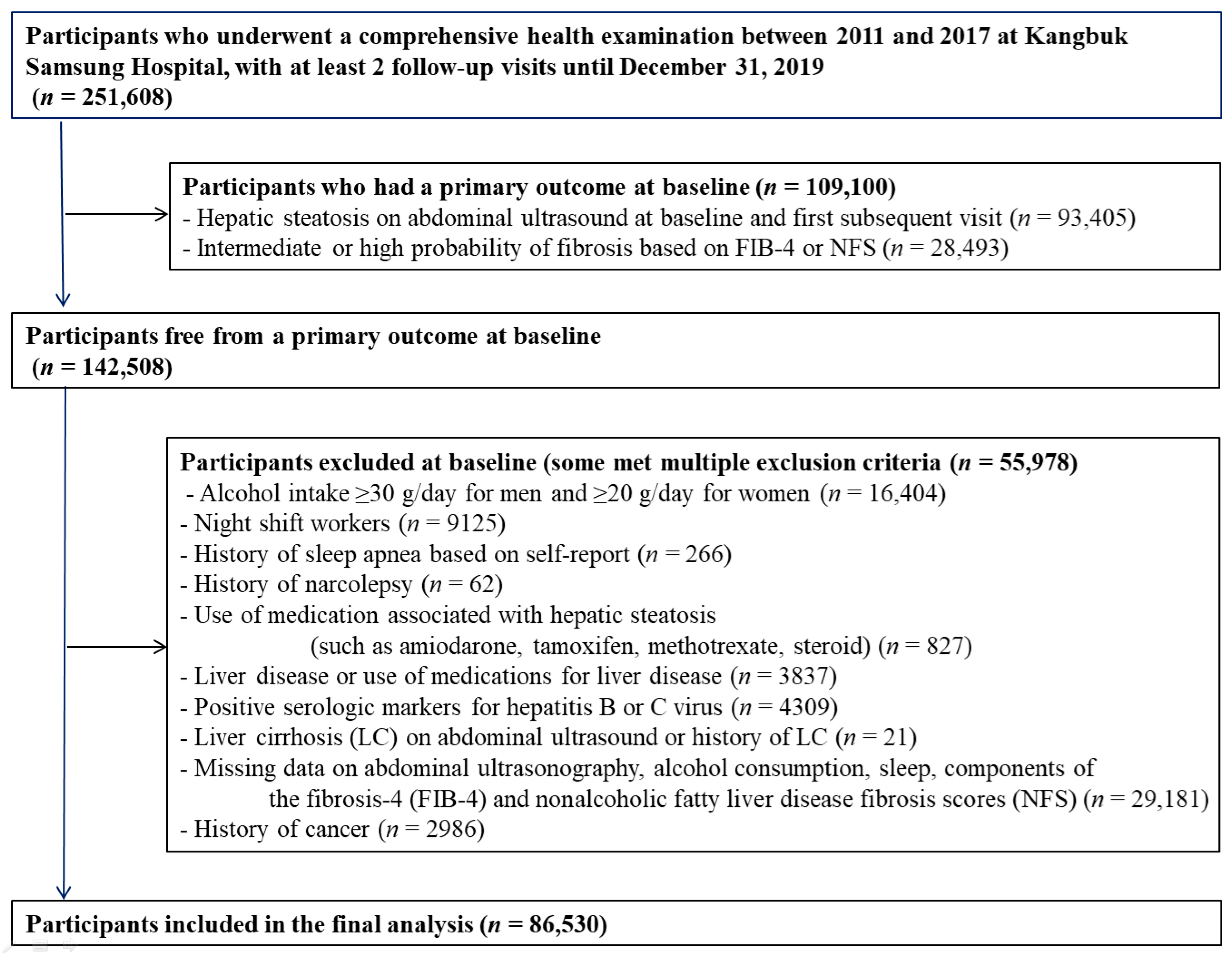
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
6.1. Key Points
6.1.1. Question
6.1.2. Findings
6.1.3. Meaning
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALT | alanine aminotransferase |
| AST | aspartate aminotransferase |
| BMI | body mass index |
| CES-D | Center for Epidemiologic Studies Depression |
| CI | confidence interval |
| HOMA-IR | homeostasis model assessment of insulin resistance |
| HR | hazard ratio |
| HDL-C | high-density lipoprotein cholesterol |
| HPA | hypothalamic–pituitary–adrenal |
| hsCRP | high sensitivity C-reactive protein |
| LDL-C | low-density lipoprotein cholesterol |
| NAFLD | nonalcoholic fatty liver disease |
| PSQI | Pittsburgh Sleep Quality Index |
References
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [Green Version]
- Adams, L.A.; Anstee, Q.M.; Tilg, H.; Targher, G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut 2017, 66, 1138–1153. [Google Scholar] [CrossRef] [Green Version]
- Younossi, Z.M. Non-alcoholic fatty liver disease—A global public health perspective. J. Hepatol. 2019, 70, 531–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Umbro, I.; Baratta, F.; Angelico, F.; Del Ben, M. Nonalcoholic fatty liver disease and the kidney: A review. Biomedicines 2021, 9, 1370. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- Dyson, J.K.; Anstee, Q.M.; McPherson, S. Non-alcoholic fatty liver disease: A practical approach to treatment. Frontline Gastroenterol. 2014, 5, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep disturbance, sleep duration, and inflammation: A Systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grandner, M.A.; Sands-Lincoln, M.R.; Pak, V.M.; Garland, S.N. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat. Sci. Sleep 2013, 5, 93–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation's sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, C.M.; Frochen, S.E.; Walsemann, K.M.; Ailshire, J.A. Are U.S. adults reporting less sleep?: Findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep 2019, 42, zsy221. [Google Scholar] [CrossRef]
- Xi, B.; He, D.; Zhang, M.; Xue, J.; Zhou, D. Short sleep duration predicts risk of metabolic syndrome: A systematic review and meta-analysis. Sleep Med. Rev. 2014, 18, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Kaneita, Y.; Tokiya, M.; Jike, M.; Murata, A.; Nakagome, S.; Otsuka, Y.; Ohida, T. Short sleep duration, shift work, and actual days taken off work are predictive life-style risk factors for new-onset metabolic syndrome: A seven-year cohort study of 40,000 male workers. Sleep Med. 2017, 39, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E. Nonalcoholic fatty liver disease: A systematic review. JAMA 2015, 313, 2263–2273. [Google Scholar] [CrossRef]
- Wijarnpreecha, K.; Thongprayoon, C.; Panjawatanan, P.; Ungprasert, P. Short sleep duration and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2016, 31, 1802–1807. [Google Scholar] [CrossRef]
- Shen, N.; Wang, P.; Yan, W. Sleep duration and the risk of fatty liver disease: A Systematic review and meta-analysis. Sci. Rep. 2016, 6, 31956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirshkowitz, M. Normal human sleep: An overview. Med. Clin. N. Am. 2004, 88, 551–565. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef]
- Dillon, H.R.; Lichstein, K.L.; Dautovich, N.D.; Taylor, D.J.; Riedel, B.W.; Bush, A.J. Variability in self-reported normal sleep across the adult age span. J. Gerontol. B Psychol. Sci. Soc. Sci. 2015, 70, 46–56. [Google Scholar] [CrossRef] [Green Version]
- Van Cauter, E.; Spiegel, K.; Tasali, E.; Leproult, R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008, 9, S23–S28. [Google Scholar] [CrossRef] [Green Version]
- Shockey, T.M.; Wheaton, A.G. Short sleep duration by occupation group–29 States, 2013–2014. MMWR 2017, 66, 207–213. [Google Scholar] [CrossRef]
- Song, Q.; Liu, X.; Zhou, W.; Wang, X.; Wu, S. Changes in sleep duration and risk of metabolic syndrome: The Kailuan prospective study. Sci. Rep. 2016, 6, 36861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrie, J.E.; Kivimaki, M.; Akbaraly, T.N.; Tabak, A.; Abell, J.; Davey Smith, G.; Virtanen, M.; Kumari, M.; Shipley, M.J. Change in sleep duration and type 2 diabetes: The Whitehall II Study. Diabetes Care 2015, 38, 1467–1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrie, J.E.; Shipley, M.J.; Cappuccio, F.P.; Brunner, E.; Miller, M.A.; Kumari, M.; Marmot, M.G. A prospective study of change in sleep duration: Associations with mortality in the Whitehall II cohort. Sleep 2007, 30, 1659–1666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Um, Y.J.; Chang, Y.; Jung, H.S.; Cho, I.Y.; Shin, J.H.; Shin, H.; Wild, S.H.; Byrne, C.D.; Ryu, S. Sleep duration, sleep quality, and the development of nonalcoholic fatty liver disease: A Cohort Study. Clin. Transl. Gastroenterol. 2021, 12, e00417. [Google Scholar] [CrossRef]
- Chang, Y.; Ryu, S.; Choi, Y.; Zhang, Y.; Cho, J.; Kwon, M.J.; Hyun, Y.Y.; Lee, K.B.; Kim, H.; Jung, H.S.; et al. Metabolically healthy obesity and development of chronic kidney disease: A cohort study. Ann. Intern. Med. 2016, 164, 305–312. [Google Scholar] [CrossRef]
- Chang, Y.; Ryu, S.; Sung, K.C.; Cho, Y.K.; Sung, E.; Kim, H.N.; Jung, H.S.; Yun, K.E.; Ahn, J.; Shin, H.; et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: Evidence from the Kangbuk Samsung Health Study. Gut 2019, 68, 1667–1675. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Cho, M.J.; Kim, K.H. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III R major depression. J. Korean Neuropsychiatr. Assoc. 1993, 32, 381–399. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Mathiesen, U.L.; Franzen, L.E.; Aselius, H.; Resjo, M.; Jacobsson, L.; Foberg, U.; Fryden, A.; Bodemar, G. Increased liver echogenicity at ultrasound examination reflects degree of steatosis but not of fibrosis in asymptomatic patients with mild/moderate abnormalities of liver transaminases. Dig. Liver Dis. 2002, 34, 516–522. [Google Scholar] [CrossRef]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J.; Nash Clinical Research, N. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckley, T.M.; Schatzberg, A.F. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J. Clin. Endocrinol. Metab. 2005, 90, 3106–3114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slavish, D.C.; Taylor, D.J.; Lichstein, K.L. Intraindividual variability in sleep and comorbid medical and mental health conditions. Sleep 2019, 42, zsz052. [Google Scholar] [CrossRef] [PubMed]
- Bose, M.; Olivan, B.; Laferrere, B. Stress and obesity: The role of the hypothalamic-pituitary-adrenal axis in metabolic disease. Curr. Opin. Endocrinol. Diabetes Obes. 2009, 16, 340–346. [Google Scholar] [CrossRef] [Green Version]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morselli, L.; Leproult, R.; Balbo, M.; Spiegel, K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best Pr. Res. Clin. Endocrinol. Metab. 2010, 24, 687–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheka, A.C.; Adeyi, O.; Thompson, J.; Hameed, B.; Crawford, P.A.; Ikramuddin, S. Nonalcoholic Steatohepatitis: A Review. JAMA 2020, 323, 1175–1183. [Google Scholar] [CrossRef]
- Briancon-Marjollet, A.; Weiszenstein, M.; Henri, M.; Thomas, A.; Godin-Ribuot, D.; Polak, J. The impact of sleep disorders on glucose metabolism: Endocrine and molecular mechanisms. Diabetol. Metab. Syndr. 2015, 7, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, S.R.; Zhu, X.; Storfer-Isser, A.; Mehra, R.; Jenny, N.S.; Tracy, R.; Redline, S. Sleep duration and biomarkers of inflammation. Sleep 2009, 32, 200–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, H.; Huang, F.F.; Qu, S. Melatonin: A potential intervention for hepatic steatosis. Lipids Health Dis. 2015, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Lockley, S.W.; Skene, D.J.; Arendt, J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J. Sleep Res. 1999, 8, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Liu, K.; Rathouz, P.J. Self-reported and measured sleep duration: How similar are they? Epidemiology 2008, 19, 838–845. [Google Scholar] [CrossRef] [Green Version]
- Hernaez, R.; Lazo, M.; Bonekamp, S.; Kamel, I.; Brancati, F.L.; Guallar, E.; Clark, J.M. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology 2011, 54, 1082–1090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popa, A.; Bende, F.; Sirli, R.; Popescu, A.; Baldea, V.; Lup.pusoru, R.; Cotrau, R.; Fofiu, R.; Foncea, C.; Sporea, I. Quantification of liver fibrosis, steatosis, and viscosity using multiparametric ultrasound in patients with non-alcoholic liver disease: A "real-life" cohort study. Diagnostics 2021, 11, 783. [Google Scholar] [CrossRef]
- Sugimoto, K.; Moriyasu, F.; Oshiro, H.; Takeuchi, H.; Abe, M.; Yoshimasu, Y.; Kasai, Y.; Sakamaki, K.; Hara, T.; Itoi, T. The role of multiparametric us of the liver for the evaluation of nonalcoholic steatohepatitis. Radiology 2020, 296, 532–540. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall | Sleep Duration Change Category (Hours) | ||||
|---|---|---|---|---|---|---|
| <−1 | −1 | 0 | 1 | >1 | ||
| Number | 86,530 | 5991 | 19,112 | 37,981 | 18,091 | 5355 |
| Age (years) a | 36.5 (6.0) | 35.5 (5.5) | 36.6 (5.9) | 37.0 (6.1) | 36.1 (5.9) | 35.1 (5.7) |
| Men (%) | 38.7 | 23.4 | 37.7 | 44.0 | 38.1 | 23.4 |
| Obesity (%) | 9.6 | 8.6 | 10.0 | 10.0 | 9.0 | 8.2 |
| Current smoker (%) | 13.3 | 9.4 | 13.4 | 14.7 | 13.0 | 8.6 |
| Alcohol intake (%) c | 23.5 | 18.2 | 23.0 | 24.9 | 23.7 | 19.1 |
| HEPA (%) | 13.8 | 13.6 | 14.3 | 13.9 | 13.4 | 12.6 |
| High education (%) d | 88.9 | 86.5 | 88.3 | 89.4 | 89.5 | 88.0 |
| Married (%) | 80.5 | 85.8 | 82.0 | 79.8 | 78.5 | 81.0 |
| Depression (%) | 11.2 | 13.7 | 10.4 | 10.1 | 11.8 | 17.6 |
| Hypertension | 3.8 | 2.7 | 3.7 | 4.2 | 3.7 | 2.5 |
| Diabetes | 0.6 | 0.5 | 0.6 | 0.6 | 0.5 | 0.4 |
| History of CVD | 0.7 | 0.4 | 0.7 | 0.8 | 0.6 | 0.5 |
| BMI (kg/m2) | 21.6 (2.5) | 21.4 (2.5) | 21.6 (2.6) | 21.7 (2.5) | 21.6 (2.5) | 21.3 (2.5) |
| Systolic BP (mmHg) a | 104.4 (11.6) | 102.5 (11.3) | 104.5 (11.7) | 105.1 (11.7) | 104.2 (11.5) | 101.9 (10.8) |
| Diastolic BP (mmHg) a | 66.7 (8.8) | 65.5 (8.6) | 66.8 (8.8) | 67.2 (8.9) | 66.5 (8.7) | 65.2 (8.2) |
| Glucose (mg/dL) a | 91.2 (8.8) | 90.5 (8.1) | 91.4 (8.9) | 91.5 (8.8) | 91.0 (8.9) | 90.0 (8.4) |
| Total cholesterol (mg/dl) a | 186.4 (31.1) | 184.9 (31.4) | 186.5 (31.4) | 187.0 (31.1) | 186.2 (30.9) | 183.7 (30.4) |
| LDL-C (mg/dL) a | 111.8 (28.8) | 109.6 (28.2) | 111.8 (28.9) | 112.8 (29.2) | 111.7 (28.7) | 108.3 (27.9) |
| HDL-C (mg/dL) a | 63.2 (14.6) | 64.0 (14.6) | 63.1 (14.5) | 62.8 (14.5) | 63.5 (14.6) | 64.6 (14.6) |
| Triglycerides (mg/dl) b | 73 (56–100) | 72 (55–97) | 73 (56–100) | 75 (57–102) | 73 (56–98) | 69 (54–93) |
| ALT (U/L) b | 14 (11–19) | 13 (10–18) | 14 (11–19) | 15 (11–20) | 14 (11–19) | 13 (11–18) |
| GGT (U/L) b | 15 (11–22) | 13 (10–19) | 15 (11–22) | 16 (11–23) | 15 (11–22) | 13 (10–19) |
| HOMA-IR b | 1.00 (0.68–1.41) | 1.01 (0.68–1.45) | 1.01 (0.68–1.42) | 0.99 (0.67–1.41) | 0.99 (0.68–1.42) | 0.98 (0.65–1.40) |
| hsCRP (mg/L) b | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) |
| Total energy intake b,e | 1487 (1137–1863) | 1469 (1109–1839) | 1493 (1144–1868) | 1500 (1155–1867) | 1469 (1114–1851) | 1463 (1104–1898) |
| Poor sleep quality | 19.3 | 18.8 | 16.0 | 16.0 | 23.5 | 39.9 |
| Person-Years (PY) | Incident Cases | Incidence Rate (/1000 PY) | Age and Sex-Adjusted HR (95% CI) | Multivariable-Adjusted HR a (95% CI) | ||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| Sleep Duration Change Category | ||||||
| <−1 h | 21,758.4 | 760 | 34.9 | 1.13 (1.05–1.22) | 1.24 (1.15–1.35) | 1.14 (1.06–1.24) |
| −1 h | 69,109.2 | 2788 | 40.3 | 1.07 (1.02–1.12) | 1.12 (1.06–1.17) | 1.07 (1.02–1.12) |
| 0 h | 134,225.6 | 5519 | 41.1 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 h | 62,399.4 | 2453 | 39.3 | 1.05 (1.00–1.10) | 1.00 (0.95–1.05) | 1.02 (0.97–1.07) |
| >1 h | 18,340.3 | 607 | 33.1 | 1.09 (1.00–1.19) | 0.99 (0.91–1.08) | 1.03 (0.94–1.12) |
| P for trend | 0.195 | < 0.001 | 0.015 | |||
| P for quadratic term | 0.003 | < 0.001 | 0.018 | |||
| Sleep quality change category | ||||||
| Persistent good quality | 218,435.7 | 9076 | 41.5 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Developed poor quality | 29,805.7 | 1038 | 34.8 | 1.02 (0.95–1.09) | 1.00 (0.94–1.07) | 1.02 (0.95–1.08) |
| Resolved poor quality | 29,182.2 | 987 | 33.8 | 1.00 (0.93–1.06) | 0.96 (0.90–1.02) | 1.00 (0.93–1.07) |
| Persistent poor quality | 28,409.4 | 1026 | 36.1 | 1.10 (1.03–1.17) | 1.05 (0.98–1.12) | 1.13 (1.05–1.20) |
| . | Person-Years (PY) | Incident Cases | Incidence Rate (/1000 PY) | Age and Sex-Adjusted HR (95% CI) | Multivariable-Adjusted HR a (95% CI) | |
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| Sleep Duration Change Category | ||||||
| <−1 h | 23,439.9 | 36 | 1.54 | 1.37 (0.96–1.94) | 1.58 (1.10–2.29) | 1.45 (1.004–2.10) |
| −1 h | 75,475.2 | 130 | 1.72 | 1.09 (0.89–1.35) | 1.16 (0.94–1.44) | 1.11 (0.90–1.38) |
| 0 h | 146,570.2 | 268 | 1.83 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 h | 67,695.1 | 104 | 1.54 | 1.03 (0.82–1.29) | 0.98 (0.77–1.23) | 0.99 (0.79–1.25) |
| >1 h | 19,605.6 | 21 | 1.07 | 1.00 (0.64–1.56) | 0.89 (0.56–1.42) | 0.93 (0.58–1.49) |
| P for trend | 0.197 | 0.028 | 0.104 | |||
| P for quadratic term | 0.509 | 0.381 | 0.543 | |||
| Sleep quality change category | ||||||
| Persistent good quality | 238,838 | 429 | 1.8 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Developed poor quality | 32,044.1 | 46 | 1.4 | 1.13 (0.83–1.53) | 1.11 (0.82–1.51) | 1.13 (0.83–1.53) |
| Resolved poor quality | 31,347 | 39 | 1.2 | 0.97 (0.70–1.35) | 0.92 (0.66–1.29) | 0.96 (0.69–1.34) |
| Persistent poor quality | 30,556.8 | 45 | 1.5 | 1.17 (0.86–1.59) | 1.09 (0.79–1.49) | 1.18 (0.86–1.62) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Um, Y.J.; Chang, Y.; Jung, H.-S.; Cho, I.Y.; Shin, J.H.; Shin, H.; Wild, S.H.; Byrne, C.D.; Ryu, S. Decrease in Sleep Duration and Poor Sleep Quality over Time Is Associated with an Increased Risk of Incident Non-Alcoholic Fatty Liver Disease. J. Pers. Med. 2022, 12, 92. https://doi.org/10.3390/jpm12010092
Um YJ, Chang Y, Jung H-S, Cho IY, Shin JH, Shin H, Wild SH, Byrne CD, Ryu S. Decrease in Sleep Duration and Poor Sleep Quality over Time Is Associated with an Increased Risk of Incident Non-Alcoholic Fatty Liver Disease. Journal of Personalized Medicine. 2022; 12(1):92. https://doi.org/10.3390/jpm12010092
Chicago/Turabian StyleUm, Yoo Jin, Yoosoo Chang, Hyun-Suk Jung, In Young Cho, Jun Ho Shin, Hocheol Shin, Sarah H. Wild, Christopher D Byrne, and Seungho Ryu. 2022. "Decrease in Sleep Duration and Poor Sleep Quality over Time Is Associated with an Increased Risk of Incident Non-Alcoholic Fatty Liver Disease" Journal of Personalized Medicine 12, no. 1: 92. https://doi.org/10.3390/jpm12010092
APA StyleUm, Y. J., Chang, Y., Jung, H.-S., Cho, I. Y., Shin, J. H., Shin, H., Wild, S. H., Byrne, C. D., & Ryu, S. (2022). Decrease in Sleep Duration and Poor Sleep Quality over Time Is Associated with an Increased Risk of Incident Non-Alcoholic Fatty Liver Disease. Journal of Personalized Medicine, 12(1), 92. https://doi.org/10.3390/jpm12010092






