Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?—A Systematic Review of the Literature
Abstract
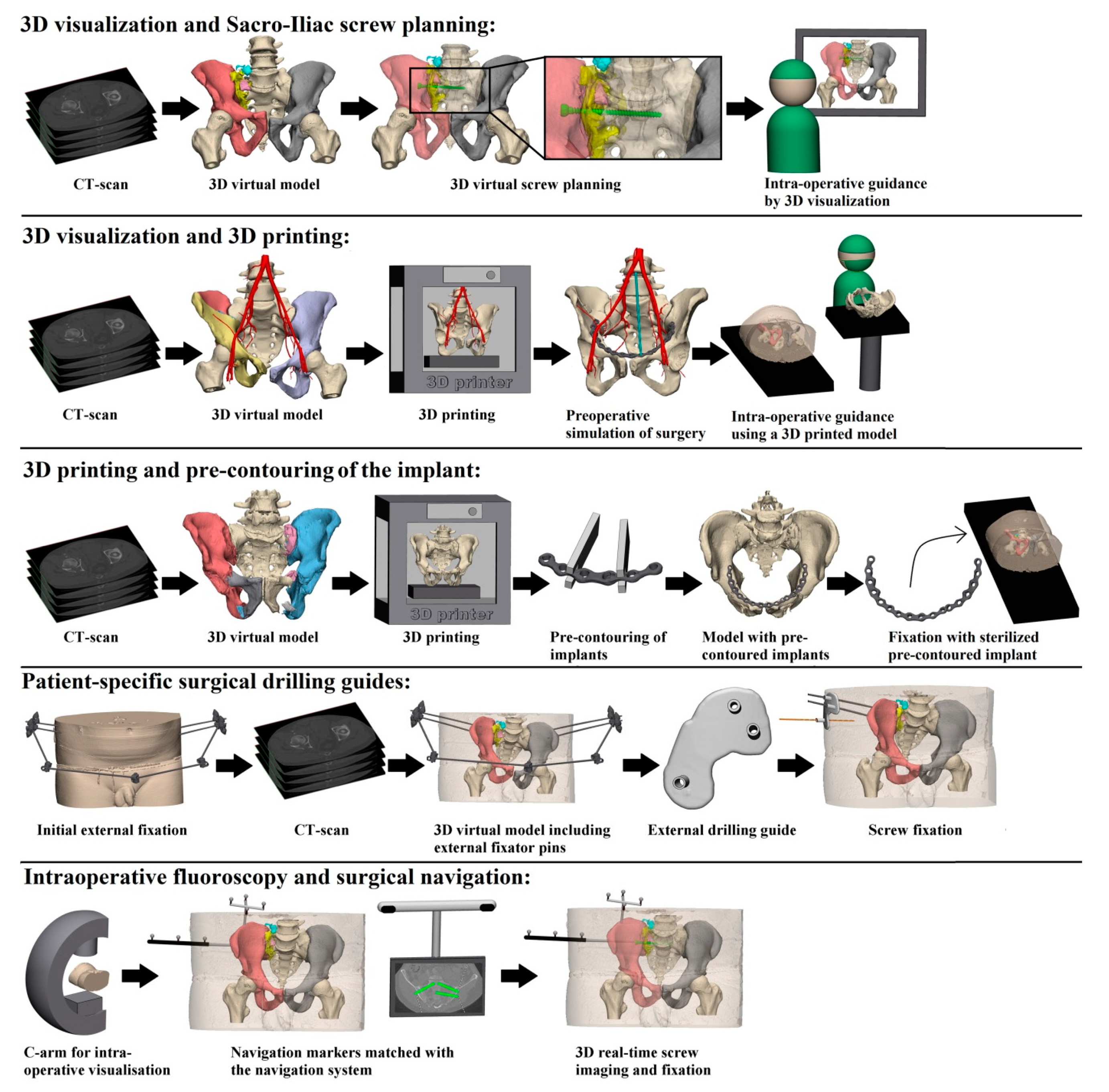
:1. Introduction
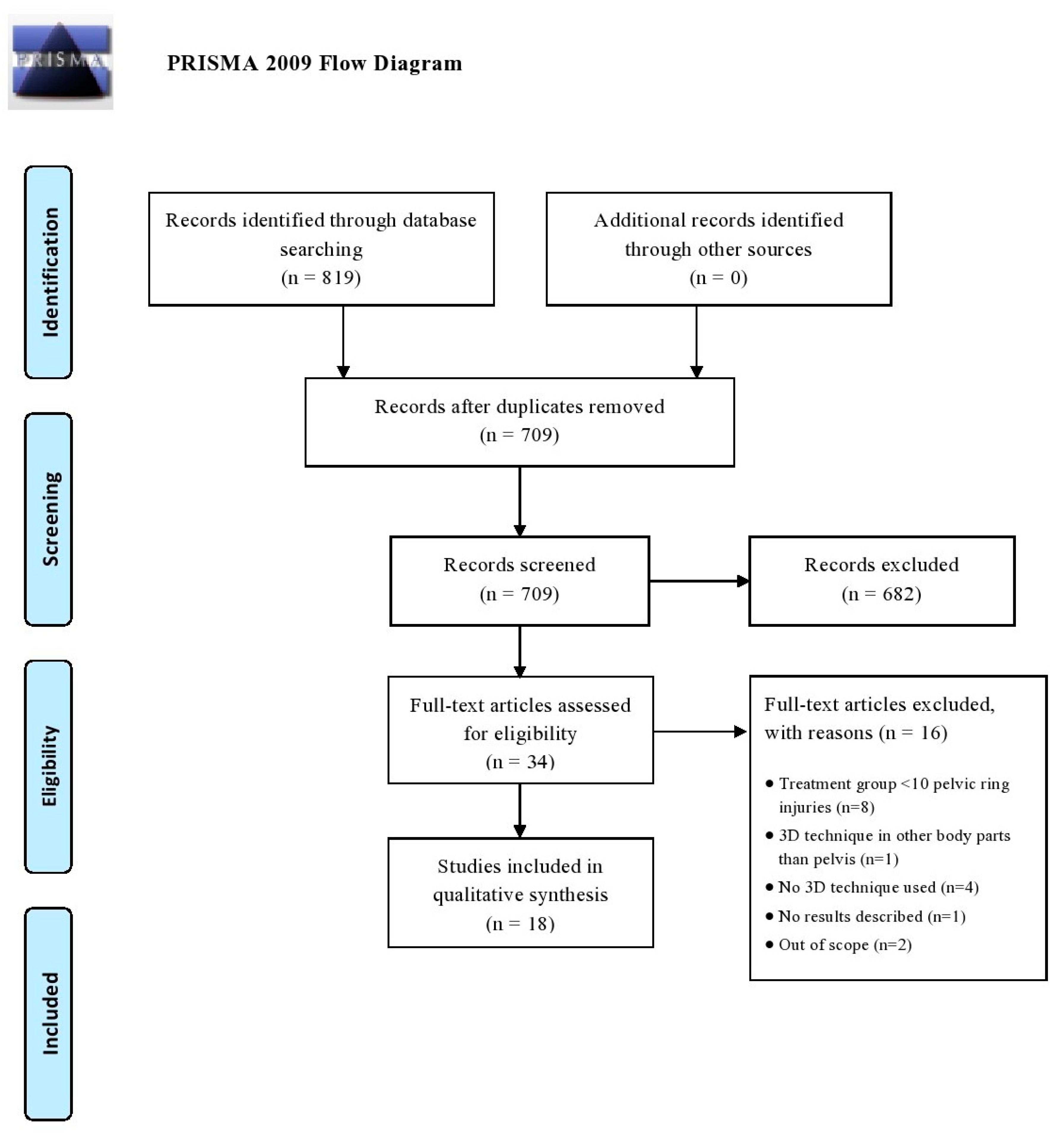
2. Methods
2.1. Identification of Studies: Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Assessment of Methodological Quality
2.6. Outcomes
2.7. Patient and Injury Characteristics
2.8. Strategy for Data Synthesis and Statistical Analysis
3. Results
3.1. Intra-Operative Results
3.1.1. Operation Time per Screw and Overall Operation Time
3.1.2. Blood Loss
3.1.3. Fluoroscopy Dose, Time and Frequency
3.2. Post-Operative Results
3.2.1. Screw Malposition
3.2.2. Post-Operative Reduction Score
3.2.3. Functional Outcome
3.3. Best-Evidence Synthesis
3.3.1. Intra-Operative Results
3.3.2. Post-Operative Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Pohlemann, T.; Tosounidis, G.; Bircher, M.; Giannoudis, P.; Culemann, U. The German multicentre pelvis registry: A template for an European expert network? Injury 2007, 38, 416–423. [Google Scholar] [CrossRef]
- Verbeek, D.O.; Ponsen, K.J.; Fiocco, M.; Amodio, S.; Leenen, L.P.H.; Goslings, J.C. Pelvic fractures in the Netherlands: Epidemiology, characteristics and risk factors for in-hospital mortality in the older and younger population. Eur. J. Orthop. Surg. Traumatol. 2017, 28, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-C.; Li, Y.T.; Chou, Y.-C.; Chen, J.-E.; Wu, C.-C.; Shen, H.-C.; Yeh, T.-T. Conventional plate fixation method versus pre-operative virtual simulation and three-dimensional printing-assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int. Orthop. 2019, 43, 425–431. [Google Scholar] [CrossRef]
- Cai, L.; Zhang, Y.; Chen, C.; Lou, Y.; Guo, X.; Wang, J. 3D printing-based minimally invasive cannulated screw treatment of unstable pelvic fracture. J. Orthop. Surg. Res. 2018, 13, 71. [Google Scholar] [CrossRef] [PubMed]
- Gras, F.; Marintschev, I.; Wilharm, A.; Klos, K.; Mückley, T.; O Hofmann, G. 2D-fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries—a case series. BMC Musculoskelet. Disord. 2010, 11, 153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balling, H. 3D image-guided surgery for fragility fractures of the sacrum. Oper. Orthop. Traumatol. 2019, 31, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Zwingmann, J.; Konrad, G.; Kotter, E.; Südkamp, N.P.; Oberst, M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin. Orthop. Relat. Res. 2009, 467, 1833–1838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-Analyses: The prisma Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Banierink, H.; Duis, K.T.; Wendt, K.; Heineman, E.; Ijpma, F.; Reininga, I. Patient-reported physical functioning and quality of life after pelvic ring injury: A systematic review of the literature. PLoS ONE 2020, 15, e0233226. [Google Scholar] [CrossRef]
- Zwingmann, J.; Hauschild, O.; Bode, G.; Südkamp, N.P.; Schmal, H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2013, 133, 1257–1265. [Google Scholar] [CrossRef]
- Pastor, T.; Tiziani, S.; Kasper, C.D.; Pape, H.-C.; Osterhoff, G. Quality of reduction correlates with clinical outcome in pelvic ring fractures. Injury 2019, 50, 1223–1226. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Law, M.; Stewart, D.; Pollock, N.; Letts, L.; Bosch, J.; Westmoreland, M. Guidelines for Critical Review Form-Quantitative Studies [Internet] Quantitative Review Form-Guidelines. 1998. Available online: https://healthsci.mcmaster.ca/docs/librariesprovider130/default-document-library/guidelines-for-critical-review-form-quantiative-studies-english.pdf?sfvrsn=ee9f6c19_2 (accessed on 1 July 2021).
- Berger-Groch, J.; Lueers, M.; Rueger, J.M.; Lehmann, W.; Thiesen, D.; Kolb, J.P.; Hartel, M.J.; Grossterlinden, L.G. Accuracy of navigated and conventional iliosacral screw placement in B- and C-type pelvic ring fractures. Eur. J. Trauma Emerg. Surg. 2018, 46, 107–113. [Google Scholar] [CrossRef]
- Takao, M.; Hamada, H.; Sakai, T.; Sugano, N. Factors influencing the accuracy of iliosacral screw insertion using 3D fluoroscopic navigation. Arch. Orthop. Trauma Surg. 2018, 139, 189–195. [Google Scholar] [CrossRef]
- Yang, F.; Yao, S.; Chen, K.-F.; Zhu, F.-Z.; Xiong, Z.-K.; Ji, Y.-H.; Sun, T.-F.; Guo, X.-D. A novel patient-specific three-dimensional-printed external template to guide iliosacral screw insertion: A retrospective study. BMC Musculoskelet. Disord. 2018, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; He, J.; Zhu, Z.; Zhou, N.; Hao, Z.; Wang, Y.; Li, Q. Comparison of 3D C-arm fluoroscopy and 3D image-guided navigation for minimally invasive pelvic surgery. Int. J. Comput. Assist. Radiol. Surg. 2015, 10, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- Teo, A.Q.A.; Yik, J.H.; Keat, S.N.J.; Murphy, D.P.; O’Neill, G.K. Accuracy of sacroiliac screw placement with and without intraoperative navigation and clinical application of the sacral dysmorphism score. Injury 2018, 49, 1302–1306. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Chen, B.; Zhang, Y.; Wang, X.; Wang, F.; Xia, H.; Yin, Q. Comparative use of the computer-aided angiography and rapid prototyping technology versus conventional imaging in the management of the tile C pelvic fractures. Int. Orthop. 2015, 40, 161–166. [Google Scholar] [CrossRef]
- Takeba, J.; Umakoshi, K.; Kikuchi, S.; Matsumoto, H.; Annen, S.; Moriyama, N.; Nakabayashi, Y.; Sato, N.; Aibiki, M. Accuracy of screw fixation using the O-arm® and StealthStation® navigation system for unstable pelvic ring fractures. Eur. J. Orthop. Surg. Traumatol. 2017, 28, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Pieske, O.; Landersdorfer, C.; Trumm, C.; Greiner, A.; Wallmichrath, J.; Gottschalk, O.; Rubenbauer, B. CT-guided sacroiliac percutaneous screw placement in unstable posterior pelvic ring injuries: Accuracy of screw position, injury reduction and complications in 71 patients with 136 screws. Injury 2015, 46, 333–339. [Google Scholar] [CrossRef]
- Beck, M.; Kröber, M.; Mittlmeier, T. Intraoperative three-dimensional fluoroscopy assessment of iliosacral screws and lumbopelvic implants stabilizing fractures of the os sacrum. Arch. Orthop. Trauma Surg. 2010, 130, 1363–1369. [Google Scholar] [CrossRef]
- Chen, K.; Yao, S.; Yang, F.; Drepaul, D.; Telemacque, D.; Zhu, F.; Zeng, L.; Xiong, Z.; Sun, T.; Guo, X. Minimally invasive screw fixation of unstable pelvic fractures using the “Blunt End” kirschner wire technique assisted by 3D printed external template. BioMed Res. Int. 2019, 2019, 1524908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, H.; Luo, C.-F.; Hu, C.-F.; Zhang, C.-Q.; Zeng, B.-F. Minimally Invasive Fluoro-Navigation Screw Fixation for the Treatment of Pelvic Ring Injuries. Surg. Innov. 2011, 18, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Ghisla, S.; Napoli, F.; Lehoczky, G.; Delcogliano, M.; Habib, N.; Arigoni, M.; Filardo, G.; Candrian, C. Posterior pelvic ring fractures: Intraoperative 3D-CT guided navigation for accurate positioning of sacro-iliac screws. Orthop. Traumatol. Surg. Res. 2018, 104, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-W.; Oh, C.-W.; Lee, H.-J.; Min, W.-K.; Kyung, H.-S.; Yoon, S.-H.; Mun, J.-U.; Oh, J.-K. Percutaneous iliosacral screwing in pelvic ring injury using three-dimensional fluoroscopy. J. Orthop. Sci. 2013, 18, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Nie, W.B.; Ye, F.G.; Ma, J.L.; Yu, J.P.; Wang, M.X.; Zhang, Z.H.; Sun, F.J. Three-dimensional (3D) printing technology assisted by minimally invasive surgery for pubic rami fractures. Curr. Med. Sci. 2018, 38, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Privalov, M.; Beisemann, N.; Swartman, B.; Vetter, S.Y.; Grützner, P.A.; Franke, J.; Keil, H. First experiences with intraoperative CT in navigated sacroiliac (SI) instrumentation: An analysis of 25 cases and comparison with conventional intraoperative 2D and 3D imaging. Injury 2020. [Google Scholar] [CrossRef]
- Tornetta, P.; Matta, J.M. Outcome of Operatively Treated Unstable Posterior Pelvic Ring Disruptions. Clin. Orthop. Relat. Res. 1996, 329, 186–193. [Google Scholar] [CrossRef]
- AO/OTA Classification. Available online: https://www.aofoundation.org/Structure/Pages/default.aspx (accessed on 1 July 2021).
- van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L. Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003, 28, 1290–1299. [Google Scholar] [CrossRef] [Green Version]
- Treadwell, J.R.; Singh, S.; Talati, R.; McPheeters, M.L.; Reston, J.T. A framework for best evidence approaches can improve the transparency of systematic reviews. J. Clin. Epidemiol. 2012, 65, 1159–1162. [Google Scholar] [CrossRef]
- Zhang, Y.D.; Wu, R.Y.; Xie, D.D.; Zhang, L.; He, Y.; Zhang, H. Effect of 3D printing technology on pelvic fractures:A meta-analysis. Zhongguo Gu Shang = China J. Orthop. Traumatol. 2018, 31, 465–471. [Google Scholar]
- Lefaivre, K.A.; Blachut, P.A.; Starr, A.J.; Slobogean, G.P.; O’Brien, P.J. Radiographic Displacement in Pelvic Ring Disruption. J. Orthop. Trauma 2014, 28, 160–166. [Google Scholar] [CrossRef] [PubMed]
| Database | Search String |
|---|---|
| MEDLINE-PubMed | (((“Pelvis”[Mesh] OR pelvic ring[tiab]) AND (“Wounds and Injuries”[Mesh] OR “injuries” [Subheading] OR injur*[tiab] OR fractur*[tiab]))) AND ((3D[tiab] OR three dimension*[tiab] OR 3 dimension*[tiab] OR “Printing, Three-Dimensional”[Mesh] OR “Imaging, Three-Dimensional”[Mesh] OR navigation[tiab])) AND 2010:2020[dp] |
| Ovid-EMBASE | (‘pelvis’/exp OR ‘pelvis surgery’/exp OR ‘pelvic ring’:ti,ab) AND (‘bone injury’/exp OR injur*:ti,ab OR fractur*:ti,ab) AND (‘three dimensional printing’/exp OR ‘three-dimensional imaging’/exp OR 3d:ti,ab OR ‘three dimension*’:ti,ab OR ‘3 dimension*’:ti,ab OR navigation:ti,ab) AND [embase]/lim AND (2010–2020)/py |
| − | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Total | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Citation | Study Purpose | Literature Review | Sample | Outcomes | Intervention | Results | Conclusion and Clinical Implications | ||||||||
| Berger-Groch et al. [14] | + | + | + | + | − | + | + | + | + | + | + | + | + | 12/13 | 92 |
| Takao et al. [15] | + | + | + | + | − | + | + | + | + | + | + | − | + | 11/13 | 85 |
| Yang et al. [16] | + | + | + | + | − | + | + | + | + | + | + | − | + | 11/13 | 85 |
| Hung et al. [3] | + | + | + | + | − | + | − | + | + | + | + | − | + | 10/13 | 76 |
| Li. et al. [17] | + | + | + | + | − | + | − | + | + | + | + | − | + | 10/13 | 76 |
| Teo et al. [18] | + | + | + | + | − | + | + | + | + | − | + | − | + | 10/13 | 76 |
| Cai et al. [4] | + | + | + | + | − | − | − | + | + | + | + | − | + | 9/13 | 69 |
| Li et al. [19] | + | + | + | + | − | − | − | + | + | + | + | − | + | 9/13 | 69 |
| Balling [6] | + | + | + | + | − | + | + | + | − | − | + | − | − | 8/13 | 62 |
| Takeba et al. [20] | + | + | + | + | − | + | + | + | − | − | + | − | − | 8/13 | 62 |
| Pieske et al. [21] | + | + | + | + | − | − | − | + | + | − | + | − | − | 7/13 | 54 |
| Beck et al. [22] | + | + | + | + | − | − | − | + | − | − | + | − | − | 6/13 | 46 |
| Chen et al. [23] | + | + | + | + | − | − | − | + | − | − | + | − | − | 6/13 | 46 |
| Gao et al. [24] | + | + | + | + | − | − | − | + | − | − | + | − | − | 6/13 | 46 |
| Ghisla et al. [25] | + | + | + | + | − | − | − | + | − | − | + | − | − | 6/13 | 46 |
| Kim et al. [26] | + | + | + | + | − | − | − | + | − | − | + | − | − | 6/13 | 46 |
| Nie et al. [27] | + | − | + | + | − | − | − | + | + | − | + | − | − | 6/13 | 46 |
| Privalov et al. [28] | + | + | + | − | − | − | − | + | + | − | + | − | − | 6/13 | 46 |
| No. | Study | Year | N | Method * | Study Period | Injury Type | Intervention |
|---|---|---|---|---|---|---|---|
| 1 | Balling [6] | 2019 | 52 | CSS | 2011–2016 | Sacral FFPs® | 3D image guided sacral screw fixation via single-sided minimally invasive transgluteal approach |
| 2 | Beck et al. [22] | 2010 | 26 | CCS | 2008–2009 | AO/Tile B, C | S: intra-operative 3D fluoroscopy of iliosacral screws and lumbopelvic implants (N = 14) C: iliosacral screws and lumbopelvic implants without intra-operative 3D (N = 12) |
| 3 | Berger-Groch et al. [14] | 2018 | 136 | CCS | 2004–2014 | AO/Tile B, C | S: 3D navigated iliosacral screw placement (N = 100) C: conventional iliosacral screw placement (N = 36) |
| 4 | Cai et al. [4] | 2018 | 137 | CCS | 2014–2016 | AO/Tile B, C | S: 3D printing-based minimally invasive cannulated screw treatment (N = 65) C: conventional surgery without 3D printing (N = 72) |
| 5 | Chen et al. [23] | 2019 | 28 | PCS | 2016–2018 | AO/Tile B, C | Minimally invasive screw fixation using the “Blunt End” Kirschner wire technique assisted by 3D printed external template |
| 6 | Gao et al. [24] | 2011 | 22 | CSS | 2006–2008 | AO/Tile B, C | Minimally invasive fluoro-navigation screw fixation |
| 7 | Ghisla et al. [25] | 2018 | 21 | CSS | 2008–2017 | Posterior pelvic ring | Intra-operative 3D-CT guided navigation for iliosacral screws |
| 8 | Hung et al. [3] | 2018 | 30 | CCS | 2012–2017 | AO/Tile A, B, C | S: ORIF with pre-operative virtual simulation and 3D- printing-assisted contoured plate (N = 16) C: ORIF with conventional plate fixation (N = 14) |
| 9 | Kim et al. [26] | 2013 | 29 | CSS | 2010 | AO/Tile A, B | Percutaneous iliosacral screwing using 3D-fluoroscopy |
| 10 | Li et al. [19] | 2015 | 157 | CCS | 2009–2014 | AO/Tile C | S: computer-aided angiography and rapid prototyping technology (N = 81) C: conventional imaging (N = 76) |
| 11 | Li. et al. [17] | 2015 | 81 | CCS | 2005–2011 | AO/Tile B, C | S: 3D C-arm fluoroscopy navigation (N = 43) C: C-arm fluoroscopy (N = 38) |
| 12 | Nie et al. [27] | 2018 | 30 | CSS | 2015–2017 | AO/Tile B, C | 3D printing assisted by minimally invasive surgery for pubic rami fractures |
| 13 | Pieske et al. [21] | 2015 | 71 | CSS | Unknown | AO/Tile B, C | CT-guided sacroiliac percutaneous screw placement |
| 14 | Privalov et al. [28] | 2020 | 53 | CCS | 2017–2018 | Posterior pelvic ring | S: intra-operative CT in navigated sacroiliac instrumentation (N = 25) C1: navigated surgery with intra-operative 3D-C-Arm (N = 15) C2: conventional surgery with intra-operative control by 3D-C-Arm (N = 9) C3: conventional surgery with intra-operative control by 2D fluoroscopy (N = 4) |
| 15 | Takao et al. [15] | 2019 | 27 | CSS | 2011–2016 | AO/Tile B, C | 3D fluoroscopic navigation of iliosacral screw insertion |
| 16 | Takeba et al. [20] | 2018 | 10 | CSS | 2013–2017 | AO/Tile B, C | O-arm and stealth station navigation for screw fixation |
| 17 | Teo et al. [18] | 2018 | 36 | CCS | 2011–2016 | AO/Tile B, C | S: sacroiliac screw placement with intra-operative navigation C: sacroiliac screw placement without intra-operative navigation |
| 18 | Yang et al. [16] | 2018 | 40 | CCS | 2016–2017 | AO/Tile B, C | S: 3D printed external template to guide iliosacral screw insertion (N = 22) C: conventional without external template (N = 18) |
| Best-Evidence Synthesis | |
|---|---|
| Strong evidence | Consistent findings among multiple high-quality studies |
| Moderate evidence | Consistent findings in multiple low-quality studies and/or one high-quality study |
| Limited evidence | Consistent findings in at least one low-quality study |
| Conflicting evidence | Inconsistent findings among multiple studies (high- and/or low-quality studies) |
| No evidence | Findings of eligible studies do not meet the criteria for one of the levels of evidence stated above, or there are no eligible studies available |
| Measure | Study | 3D Technology | Groups (N) | Outcomes | |||
|---|---|---|---|---|---|---|---|
| 3D | Conventional | 3D | Conventional | p-Value | |||
| Intra-Operative Results | |||||||
| Operation time per screw (min) Mean ± std or Mean ± (range) | Berger-Groch et al. [14] | 3D navigated iliosacral screw placement | 100 | 36 | 48 ± 25 | 50 ± 29 | 0.74 |
| Chen et al. [23] | Minimally invasive screw fixation using the “Blunt End” kirschner wire technique assisted by 3D printed external template | 28 | - | 21 ± 3 | - | - | |
| Gao et al. [24] | Minimally invasive fluoro-navigation screw fixation | 22 | - | 24 (16–45) | - | - | |
| Kim et al. [26] | Percutaneous iliosacral screwing using 3D-fluoroscopy | 29 | - | 36 (18–83) | - | - | |
| Li. et al. [17] | Percutaneous screw fixation using three-dimensional (ISO-C3D) navigation | 43 | 38 | 14 ± 1 | 19 ± 1 | <0.001 | |
| Pieske et al. [21] | CT-guided sacroiliac percutaneous screw placement | 71 | - | 63 ± 39 | - | - | |
| Takeba et al. [20] | O-arm and stealthstation navigation for screw fixation | 10 | - | 39 (25–68) | - | - | |
| Yang et al. [16] | 3D printed external template to guide iliosacral screw insertion | 22 | 18 | 18 ± 5 | 40 ± 11 | <0.001 | |
| Operation time overall (min) Mean ± std | Cai et al. [4] | 3D printing-based minimally invasive cannulated screw treatment | 65 | 72 | 59 ± 13 | 72 ± 13 | <0.001 |
| Chen et al. [23] | Minimally invasive screw fixation using the “Blunt End” kirschner wire technique assisted by 3D printed external template | 28 | - | 85 (60–150) | - | - | |
| Hung et al. [3] | Pre-operative virtual simulation and 3D printing-assisted contoured plate | 16 | 14 | 206 ± 70 | 276 ± 90 | 0.023 | |
| Li et al. [19] | Computer-aided angiography and rapid prototyping technology | 81 | 76 | 105 ± 19 | 122 ± 23 | 0.035 | |
| Privalov et al. [28] | Intra-operative CT in navigated sacroiliac instrumentation | 25 | 28 | 189 ± 89 | C1: 153 ± 68 C2: 201 ± 100 C3: 127 ± 70 | 0.31 0.70 0.14 | |
| Blood loss (mL)Mean ± std or Mean (range) | Hung et al. [3] | pre-operative virtual simulation and 3D printing-assisted contoured plate | 16 | 14 | 275 ± 197 | 549 ± 404 | 0.023 |
| Nie et al. [27] | 3D printing assisted by minimally invasive surgery | 30 | - | 31 ± 11 | - | - | |
| Takeba et al. [20] | O-arm and stealthstation navigation for screw fixation | 10 | - | 12 (0–120) | - | - | |
| Fluoroscopy Dose mean ± SD or mean (range) presented in the given unit | Balling [6] | 3D image guided sacral screw fixation via single-sided minimally invasive transgluteal approach | 52 | - | 788 ± 632mGy/cm | - | - |
| Beck et al. [22] | Intra-operative 3D fluoroscopy of iliosacral screws and lumbopelvic implants | 14 | 12 | 181 cGy/cm2 (90–424) | 1376 cGy/cm2 (485–2) | NA | |
| Ghisla et al. [25] | Intra-operative 3D-CT guided navigation for sacro-iliac screws | 21 | - | 1918 mGy/cm | - | - | |
| Pieske et al. [21] | CT-guided sacroiliac percutaneous screw placement | 71 | - | Male: 6 ± 3 msV, range: 2–17; Female: 9 ± 3 msV, range: 1–28 | - | - | |
| Yang et al. [16] | 3D printed external template to guide iliosacral screw insertion | 22 | 18 | 743 ± 231 cGy/cm2 | 1904 ± 845 cGy/cm2 | <0.001 | |
| Fluoroscopy time (sec) mean ± SD or mean (range) | Beck et al. [22] | Intra-operative 3D fluoroscopy of iliosacral screws and lumbopelvic implants | 14 | 12 | 64 (60–71) | 181 (54–340) | NA |
| Berger-Groch et al. [14] | 3D navigated iliosacral screw placement | 100 | 36 | 99 ± 812 | 164 ± 166 | 0.02 | |
| Gao et al. [24] | Minimally invasive fluoro-navigation screw fixation | 22 | - | 22 (10–46) | - | - | |
| Kim et al. [26] | Percutaneous iliosacral screwing using 3D-fluoroscopy | 29 | - | 84 (22–160) | |||
| Li. et al. [17] | Percutaneous screw fixation using three-dimensional (ISO-C3D) navigation | 43 | 38 | 34 ± 2 | 58 ± 5 | <0.001 | |
| Privalov et al. [28] | Intra-operative CT in navigated sacroiliac instrumentation | 25 | 28 | 82 ± 97 | C1: 299 ± 374 C2: 243 ± 92 C3: 248 ± 191 | 0.03 0.00 0.02 | |
| Fluoroscopy frequency number of times in mean ± SD or mean (range) | Cai et al. [4] | 3D printing-based minimally invasive cannulated screw treatment | 65 | 72 | 29 ± 4 | 37 ± 3 | <0.001 |
| Chen et al. [23] | Minimally invasive screw fixation using the “Blunt End” kirschner wire technique assisted by 3D printed external template | 28 | - | 35 (28–60) | - | - | |
| Post-Operative Results | |||||||
| Screw malposition rate (%) | Beck et al. [22] | Intra-operative 3D fluoroscopy of iliosacral screws and lumbopelvic implants | 14 | 12 | 7 | 6 | NA |
| Gao et al. [24] | Minimally invasive fluoro-navigation screw fixation | 22 | - | 2 | - | - | |
| Ghisla et al. [25] | Intra-operative 3D-CT guided navigation for sacro-iliac screws | 21 | - | 3 | - | - | |
| Kim et al. [26] | Percutaneous iliosacral screwing using 3D-fluoroscopy | 29 | - | 23 | - | - | |
| Li. et al. [17] | Percutaneous screw fixation using three-dimensional (ISO-C3D) navigation | 43 | 38 | 5 | 24 | 0.015 | |
| Pieske et al. [21] | CT-guided sacroiliac percutaneous screw placement | 71 | - | 1 | - | - | |
| Takao et al. [15] | 3D fluoroscopic navigation of iliosacra screw insertion | 27 | - | 7 | - | - | |
| Takeba et al. [20] | O-arm and stealthstation navigation for screw fixation | 10 | - | 0 | - | - | |
| Teo et al. [18] | Sacroiliac screw placement with and without intra-operative navigation | 17 | 19 | 12 | 5 | 0.48 | |
| Yang et al. [16] | 3D printed external template to guide iliosacral screw insertion | 22 | 18 | 3 | 14 | <0.001 | |
| Berger-Groch et al. [14] | 3D navigated iliosacral screw placement | 100 | 36 | 14 | 21 | 0.09 | |
| Reduction according to Matta (excellent + good in %) | Cai et al. [4] | 3D printing-based minimally invasive cannulated screw treatment | 65 | 72 | 79 | 81 | 0.762 |
| Chen et al. [23] | Minimally invasive screw fixation using the “Blunt End” kirschner wire technique assisted by 3D printed external template | 28 | - | 89 | - | - | |
| Nie et al. [27] | 3D printing assisted by minimally invasive surgery for pubic rami fractures | 30 | - | 100 | - | - | |
| Yang et al. [16] | 3D printed external template to guide iliosacral screw insertion | 22 | 18 | 86 | 89 | 1.000 | |
| Functional outcome (Majeed excellent + good rate in %) | Cai et al. [4] | 3D printing-based minimally invasive cannulated screw treatment | 65 | 72 | 82 | 81 | 0.884 |
| Chen et al. [23] | Minimally invasive screw fixation using the “Blunt End” kirschner wire technique assisted by 3D printed external template | 28 | - | 82 | - | - | |
| Li. et al. [17] | Percutaneous screw fixation using three-dimensional (ISO-C3D) navigation | 43 | 38 | 92 | 89 | 0.637 | |
| Nie et al. [27] | 3D printing assisted by minimally invasive surgery for pubic rami fractures | 30 | - | 100 | - | - | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banierink, H.; Meesters, A.M.L.; ten Duis, K.; Doornberg, J.N.; El Moumni, M.; Heineman, E.; Reininga, I.H.F.; IJpma, F.F.A. Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?—A Systematic Review of the Literature. J. Pers. Med. 2021, 11, 930. https://doi.org/10.3390/jpm11090930
Banierink H, Meesters AML, ten Duis K, Doornberg JN, El Moumni M, Heineman E, Reininga IHF, IJpma FFA. Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?—A Systematic Review of the Literature. Journal of Personalized Medicine. 2021; 11(9):930. https://doi.org/10.3390/jpm11090930
Chicago/Turabian StyleBanierink, Hester, Anne M. L. Meesters, Kaj ten Duis, Job N. Doornberg, Mostafa El Moumni, Erik Heineman, Inge H. F. Reininga, and Frank F. A. IJpma. 2021. "Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?—A Systematic Review of the Literature" Journal of Personalized Medicine 11, no. 9: 930. https://doi.org/10.3390/jpm11090930
APA StyleBanierink, H., Meesters, A. M. L., ten Duis, K., Doornberg, J. N., El Moumni, M., Heineman, E., Reininga, I. H. F., & IJpma, F. F. A. (2021). Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?—A Systematic Review of the Literature. Journal of Personalized Medicine, 11(9), 930. https://doi.org/10.3390/jpm11090930






