Abstract
Background: Lung ultrasound (LUS) is a useful imaging method for identifying COVID-19 pneumonia. The aim of this study was to explore the role of LUS in predicting the severity of the disease and fatality in patients with COVID-19. Methods: This was a single-center, follow-up study, conducted from 1 November 2020, to 22 March 2021. The LUS protocol was based on the assessment of 14 lung zones with a total score up to 42, which was compared to the disease severity and fatality. Results: A total of 133 patients with COVID-19 pneumonia confirmed by RT-PCR were enrolled, with a median time from hospital admission to lung ultrasound of one day. The LUS score was correlated with clinical severity at hospital admission (Spearman’s rho 0.40, 95% CI 0.24 to 0.53, p < 0.001). Patients with higher LUS scores were experiencing greater disease severity; a high flow nasal cannula had an odds ratio of 1.43 (5% CI 1.17–1.74) in patients with LUS score > 29; the same score also predicted the need for mechanical ventilation (1.25, [1.07–1.48]). An LUS score > 30 (1.41 [1.18–1.68]) and age over 68 (1.26 [1.11–1.43]) were significant predictors of fatality. Conclusions: LUS at hospital admission is shown to have a high predictive power of the severity and fatality of COVID-19 pneumonia.
1. Introduction
The coronavirus disease 2019 (COVID-19) is caused by a new strain of the virus discovered at the end of 2019 in China, which had not been detected in humans previously; the World Health Organization named it SARS-CoV-2, and it is the cause of a pandemic that continues to this day []. The symptoms of COVID-19 differ between individuals, varying from asymptomatic infection to severe respiratory failure. Common symptoms are a fever, cough, fatigue, slight dyspnea, sore throat, and headache. The vast majority of patients with symptoms and more severe clinical features had one or more comorbidities, for instance, obesity and cardiovascular conditions, with high case fatalities amongst elderly and frail patients [,].
Recognizing risk factors at admission which predict disease progression would help physicians to deliver appropriate and timely therapeutic interventions. Increasing age, medical comorbidities, lymphopenia, elevated serum ferritin, d-dimer, cardiac troponin I, C-reactive protein, lactate dehydrogenase, and IL-6 levels are associated with severe illness, poor prognosis, and increased mortality [,,].
COVID-19 pneumonia is radiologically characterized by bilateral pulmonary infiltrates with a propensity toward the lung periphery and a lack of associated pulmonary nodules, cavitation, adenopathy, or pleural effusions [].
CT is a gold standard for COVID-19 pneumonia imaging, and recent studies have suggested a potential role of CT severity scores in predicting outcomes for SARS-CoV-2 patients [,]. However, because CT scans are not readily available in pandemic situations, there is a need for a comparable imaging method. Lung ultrasound (LUS) is a useful noninvasive diagnostic procedure for identifying pleural and pulmonary lesions; it can be performed continuously at the bedside and with no radiation exposure, to assess disease progression and severity. LUS has been shown to be comparable to X-ray and CT scans in the diagnosis of pneumothorax, pleural effusion, and pneumonia, and identifying the signs of cardiac failure [,,,]. Recent studies have reported that findings on LUS associated with COVID-19 correlate well with CT scans [,,]. In addition, current research suggests the usability of lung ultrasounds for COVID-19 screening at hospital admission, showing a high negative predictive value for LUS [,].
Treatments for COVID-19 are mainly in the form of a certain degree of respiratory support with other adjunctive therapies. Supplemental oxygen is the primary step for addressing respiratory impairment, ranging from a low flow nasal cannula, and as the disease progresses, to the usage of masks with higher oxygen delivery, high-flow nasal cannula (HFNC) devices, noninvasive ventilation, and ultimately, to invasive mechanical ventilation []. Therefore, it is crucial to be able to predict the degree of oxygen support that patients presenting with COVID-19 pneumonia may need, enabling physicians to adjust other treatment modalities accordingly, such as corticosteroid therapy, or transferring patients to more specialized centers.
There have been some suggestions lately that LUS can predict outcomes in COVID-19; endpoints in most of studies were mortality and the need for invasive mechanical ventilation [,,,,,]. At the beginning of the COVID-19 pandemic, it was observed that LUS did not correlate much with oxygen need in patients at the time of admission to a hospital ward. For example, the patient could be on a low oxygen flow and clinically stable, although the LUS findings were disproportionally negative. Only after a few days would the patient’s clinical status deteriorate significantly, a realization that alerted us to the possible prognostic value of bedside lung ultrasound; therefore, this study explores the role of LUS in predicting the disease severity and mortality in patients with COVID-19.
2. Materials and Methods
2.1. Study Design
This was a single-center, follow-up study.
2.2. Inclusion and Exclusion Criteria
The study was based on a consecutive group of patients admitted with a diagnosis of COVID-19 pneumonia in the University Hospital Centre Split, Croatia, from 1 November 2020, to 22 March 2021. Inclusion criteria were the WHO diagnostic criteria for COVID-19 pneumonia, with SARS-CoV-2 infection confirmed by PCR or a rapid antigen test from a nasopharyngeal swab []. Exclusion criteria were pulmonary edema associated with heart failure; severe lung emphysema; chronic interstitial lung disease, severe hemodynamic instability and inability to change body position; severe chest deformity; extensive subcutaneous emphysema; any other pulmonary diseases impeding image acquisition (i.e., significant pleural effusion, previous pneumonectomy); and an inability to undergo LUS examination.
Outcomes
The study’s primary outcome was disease severity. We divided modalities into groups and graded them as follows: 0—no oxygen administration necessary; 1—0–10 L of oxygen nasally; 2—11–16 L of oxygen per bag mask; 3—HFNC (high-flow nasal cannula); and 4—MV (mechanical ventilation). A secondary outcome was fatality.
2.3. Data Extraction
Patient demographics, symptoms, laboratory tests, comorbidities, and treatment modalities were extracted from electronic medical records by the principal investigator (I.S.).
2.4. Acquisition Protocol
Lung ultrasound examinations were performed by two trained sonographers (I.S. and I.B.) using a Toshiba Nemio XG iSTYLE ultrasound system (Toshiba Medical Systems Corporation, Otawara, Japan) with a 1–6 MHz convex transducer. The transducer was in abdominal preset mode using a single focal point modality on the pleural line, a mechanical index starting from 0.7, depth from 10 to 15 cm, and gain was controlled to avoid over-saturation. The extent and severity of pulmonary infiltrations were described by a numerically repeatable LUS coefficient (Lung Ultrasound Score), proposed for COVID-19 pneumonia by Soldati et al. []. Fourteen areas (three posterior, two lateral, and two anterior for each lung) were examined completely intercostally to cover the widest possible area with a single scan. Changes were scored from 0 to 3, as presented in Table 1. For each patient, the stated scores in all fourteen zones were added together (ranging from 0 to 42) to obtain the total LUS score []. According to the part of the lung in which they were positioned, the 14 areas were grouped as apical, middle, and basal for further statistical analysis.

Table 1.
Lung ultrasound point scoring system.
2.5. Bias
The LUS examinations were performed simultaneously by two team members who were blinded to the patients’ clinical data (I.S. and I.B.), reaching immediate consensus about the lung ultrasound score, and minimizing the information bias or measurement errors. Potential confounders of negative outcomes (e.g., arterial hypertension, cardiovascular diseases, or malignancy) were stated in all of the subgroups, and only two patients were excluded due to illnesses directly influencing the LUS score.
2.6. Study Size
This was a convenience sample of consecutive patients during the peak period of the pandemic in Croatia. The study size was calculated to accommodate a statistical power (beta error) of 80%, requiring a minimum of 130 patients. This coincided with the end of the pandemic peak and the occurrence of new viral strains.
2.7. Statistical Analysis
Categorical data were presented by absolute and relative frequencies. The normality of the distribution of continuous variables was tested by the Shapiro–Wilk test. Continuous data were described by the median and the limits of the interquartile range (IQR). The Mann–Whitney U test was used to compare the median between two groups and the Kruskal–Wallis test (post hoc Conover) was used to compare the median between two groups, whereas the Fisher’s exact test was used to analyze the differences between proportions. Logistic regression analysis (multivariate—stepwise method) was used to analyze independent factors associated with any respiratory support or a negative outcome. The receiver operating curve (ROC) was used to determine the optimal threshold, the area under the curve (AUC), specificity, and sensitivity of the tested parameters. All p values were two-sided. The level of significance was set at Alpha = 0.05. The statistical analysis was performed using MedCalc® Statistical Software version 19.6 (MedCalc Software Ltd., Ostend, Belgium; https://www.medcalc.org; 2020, accessed on 20 April 2021.) and IBM SPSS Stat. 23 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY, USA).
2.8. Reporting
The study is reported in line with the STROBE reporting guideline for cohort studies; the STROBE checklist is available in Supplementary File S1.
3. Results
3.1. Patients and Characteristics
From 1 November 2020, to 22 March 2021, we admitted 445 patients confirmed with COVID-19 by RT-PCR, and 133 patients were enrolled in the study (Figure 1). Two patients were excluded because of severe emphysema and chronic hypersensitivity pneumonitis.
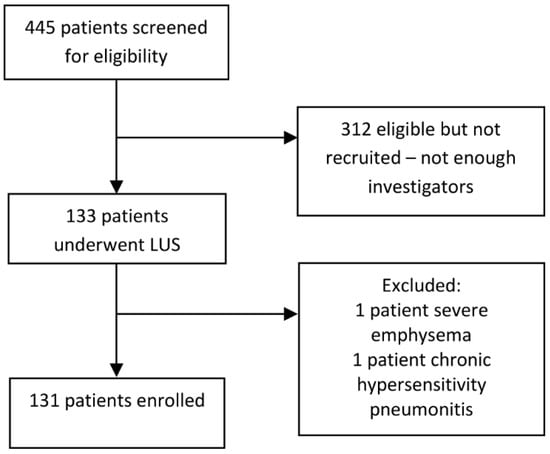
Figure 1.
Flowchart of the included patients.
The baseline characteristics of the included patients, including age, gender, day of illness, habits, comorbidities, and the respiratory support modality used, were comparable between the subgroups (Table 2).

Table 2.
Baseline characteristics of patients according to comorbidity and respiratory support modality used.
The biochemical indicators upon presentation were similar no matter the highest respiratory modality used, except for spO2 (Table 3).

Table 3.
Biochemical parameters according to the highest level of respiratory support used.
The severity of the ultrasonic parameters was also followed by the highest modality. The distribution of lung infiltrations was found to be lower in the upper regions of the lungs according to the LUS score (Friedman test, p < 0.001, Supplementary File S2).
We have shown that the LUS score is only weakly correlated with clinical severity at admission to the hospital (Spearman’s rho 0.396, 95%CI 0.240 to 0.531, p < 0.001); however, the correlation is significantly greater with the progression in disease severity (Spearman’s rho 0.750, 95%CI 0.664 to 0.817, p < 0.001).
The LUS score had a predictive value in fatality (Kruskal–Wallis test, p < 0.001; Table 4). D-dimer levels were significantly higher in deceased patients (Kruskal–Wallis test, p = 0.002; Table 4).

Table 4.
Differences in indicators according to mortality.
3.2. Impact of LUS Score on the Highest Respiratory Support Modality Used
Two independent predictors yielded statistically significant contributions to the regression model: the LUS score and the age of the patient. The model accurately classified 91.6% of cases (Table 5, Supplementary File S3).

Table 5.
Multivariate logistic regression analysis according to the highest respiratory support required (mechanical ventilation).
Patients with higher LUS scores were more likely to need more respiratory support, either the high-flow nasal cannula (HFNC) with an LUS score cut-off value of >29 (Supplementary File S3), or mechanical ventilation (MV) with a cut-off value of >30 (Table 5, Supplementary File S3).
The LUS score and age of the patient predicted the need for mechanical ventilation, as shown in Figure 2 and Supplementary File S4.
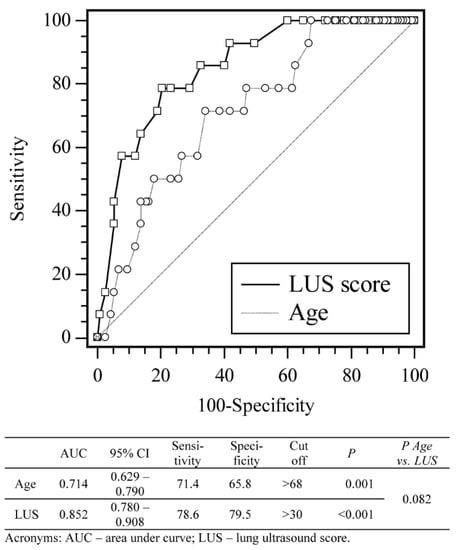
Figure 2.
Receiver operating curve analysis of sensitivity, specificity, and cut-off values for LUS score and age according to highest respiratory modality (mechanical ventilation).
3.3. Impact of LUS Score and Risk Factors on the Patient Mortality
Two independent predictors yielded significant contributions to the regression model: LUS score and age of the patient. The model accurately classified 95.4% of cases (Table 6, Supplementary File S5).

Table 6.
Multivariate logistic regression analysis according to mortality.
The LUS score and age of the patient were predictors of fatality, as shown in Figure 3 and Supplementary File S4.
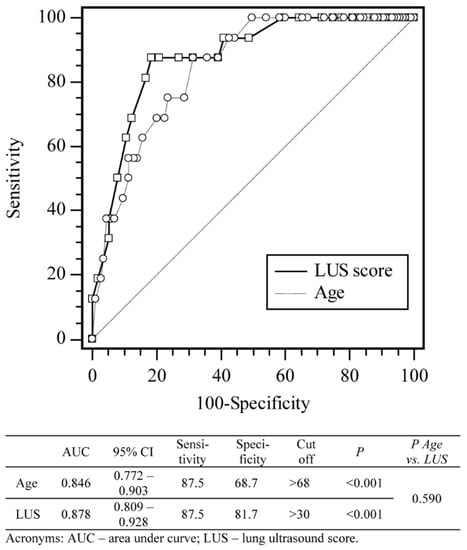
Figure 3.
Receiver operating curve analysis of sensitivity, specificity, and cut-off values for LUS score and age according to the probability of a negative outcome (death).
4. Discussion
LUS is very useful in the early diagnosis of COVID-19 pneumonia as a cheap, fast, radiation-free, and readily available method with sensitivity comparable to CT scans. This finding is even more important because obtaining computed tomography has proven to be a challenge in a pandemic setting [,].
Similar to earlier studies, the majority of patients in our study presented with bilateral interstitial changes in lung ultrasound examinations, such as B-lines, most frequently in posterior and basal zones of the lungs, where these changes were also of the highest intensity [,].
In previously published papers, LUS has been established as an excellent diagnostic technique in COVID 19 pneumonia, although there are limited data available concerning lung ultrasound as a prognostic tool for poor outcomes [,,,,,]. A study by Falgarone et al. even suggests that LUS has a better prognostic value for oxygen requirements than a chest CT scan, which is considered a gold standard for COVID-19 pneumonia [].
The ability to predict the highest level of oxygen treatment necessary is valuable information, because it can help clinicians in planning patient care, potentially making decisions on transferring a patient to a more specialized intensive care center, or even to adapt the usual therapy protocols enabling a more individualized treatment approach. Some recent evidence suggests that high-dose corticosteroid therapy can help in treating severe COVID-19 pneumonia, and perhaps the indication of a poor prognosis in patients could be used to start high doses earlier in the course of the disease, thus preventing the worst outcomes [,].
Our study showed age as a predictor with a cut-off value of >68, both for mechanical ventilation and death. Previous studies have also shown age to be a predictor of mortality and ICU admission. A systematic review of 88 studies by Katzenschlager et al. revealed that patients who required ICU admission had a median age of 65, and patients who died had a median age of 71 [].
According to our results, the LUS score showed a moderate correlation with oxygen requirements in patients at admission. We hypothesize that this discrepancy may be because interstitial changes, seen as B-lines, predate the later loss of aeration and progression to consolidation, as described in studies investigating ultrasound changes in ARDS [,]. Further studies are needed to explore the pathophysiology and development of ultrasound changes in COVID-19.
LUS was able to predict the need for HFNC or MV in COVID-19 patients. The cut-off values were similar, 29 and 30, respectively, suggesting that LUS cannot predict differentiations between these two groups. However, age was shown to only be predictive for MV in our population, which means that by combining it with a LUS score higher than 30, it can discriminate patients older than 68 who are more likely to need MV; those who are below that age who are more likely to need HFNC. To the best of our knowledge, this is the first study which has developed a model for predicting the need for HFNC in COVID-19 patients.
The AUC for LUS prediction of mortality in our study population was 0.87 at the cut-off value of LUS set to >30. The LUS score then yielded 81% specificity for mortality. Previous studies had slightly lower findings with AUC values of 0.72, 0.76, and 0.78, respectively, which could be attributed to fewer lung zones examined in the LUS protocols these earlier studies used, or the different patient populations [,,].
As opposed to some of the earlier studies, we did not find any predictive value of laboratory blood markers, such as LDH, CRP or the lymphocytic count. However, in our population, D-dimer levels were found to be significantly higher among deceased patients.
It has to be noted that in our study, only 3.8% of patients enrolled were active smokers, which is a surprising finding because more than one-third (35%) of the Croatian population are active smokers, the third highest prevalence in the European Union []. Several studies have confirmed a very low prevalence of smokers among hospitalized COVID-19 patients [,,]. It has been known for years that smokers are less likely to develop interstitial diseases such as sarcoidosis and hypersensitive pneumonitis, which is attributed to the possible protective effect of nicotine suppressing T-helper cell 1 immunity [,,,,]. Further multi-center prospective studies are needed to confirm the potential protective role of smoking in COVID-19 patients.
4.1. Strengths
The median time from disease onset to LUS examination was 10 days, and the median time from hospital admission to LUS examinations was one day, which was the main strength of our study: this suggests that it was unlikely that many patients were at the peak of their illness at the time of LUS examination. At the time of examination, the median respiratory support administered was 2 L/min of oxygen flow through a nasal cannula.
We chose an LUS examination protocol with 14 lung regions suggested by Soldati et al., which differs slightly from 10 and 12 lung region protocols used in other previously mentioned studies []. A study by Hernandez et al. suggests that the 14-lung-region protocol is superior to other protocols []. Although this might tend to require a more extensive patient workload, we have used this advantageously and noticed two things: (i) COVID19 pneumonia tends to be more severe if apical regions are affected; and (ii) infiltration of the middle regions seem to correlate with the highest respiratory modality used, even better than the whole LUS score (Supplementary File S6).
4.2. Limitations
Some limitations of our study should be highlighted. This study was performed in a single Clinical Medical Centre in Split, Croatia, with a relatively small number of patients. Not all patients admitted were included in this study due to the excessive workload and lack of resources and support staff.
Furthermore, we did not test interobserver variability because the two sonographers performed the examinations together due to time constraints as a result of the pandemic situation.
During this study, we noticed some limitations to the scoring system for the severity of pulmonary infiltrations proposed by Soldati et al., where consolidations and “white lung” were given the same score. Separating these two findings into different categories, as shown by Gutsche et al., should be considered, because consolidations are the most severe stage of COVID-19 pneumonia progression [,].
5. Conclusions
In our study, LUS at hospital admission was shown to be predictive of the need for HFNC, endotracheal intubation, and death. This finding can help in early risk stratification in COVID-19 patients, guiding further clinical and therapy decisions.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm11080757/s1, Supplementary File S1—STROBE Checklist; Supplementary File S2—Mean infiltration scores by regions of the lungs; Supplementary File S3—Logistic regression according to highest respiratory support (HFNC, MV); Supplementary File S4—Logistic regression according to mortality; Supplementary File S5—Logistic regression according to mortality; Supplementary File S6—Multivariate and ROC analysis when all ultrasonic parameters are included.
Author Contributions
Conceptualization, I.S., M.R., M.P.I.; methodology, I.S., M.R., M.P.I., K.D., O.P.; software, O.B.; validation, I.S., M.R., M.P.I., K.D.; formal analysis, O.B., O.P.; investigation, I.S., M.R., M.P.I., I.B.; resources, K.D.; data curation, I.S., O.B.; writing—original draft preparation, I.S., M.P.I., O.B., K.D., O.P.; writing—review and editing, I.S., M.P.I., O.B., K.D., I.B., O.P.; visualization, I.S., M.P.I., O.B., O.P.; supervision, M.R., O.P.; project administration, M.R., O.P.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University Hospital Centre Split, Croatia (Klasa: 500-03/21-01/01, Ur.br. 2181-147-01/06/M.S.-20-02, 29.1.2021).
Informed Consent Statement
Written informed consent was not required for participants with emerging infectious diseases. LUS is a standard of care in our center, and this study had no interventions.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank Ana Hecimovic for her kind assistance and advice during the writing of this article. We also express our gratitude to all medical staff of our COVID-19 department for their exemplary strength and endurance during this pandemic.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cascella, M.; Rajnik, M.; Cuomo, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus. In StatPearls; Uniformed Services University Of The Health Sciences: Treasure Island, FL, USA, 2020. [Google Scholar]
- Pascarella, G.; Strumia, A.; Piliego, C.; Bruno, F.; Del Buono, R.; Costa, F.; Scarlata, S.; Agro, F.E. COVID-19 diagnosis and management: A comprehensive review. J. Intern. Med. 2020, 288, 192–206. [Google Scholar] [CrossRef]
- Mohammad, S.; Aziz, R.; Al Mahri, S.; Malik, S.S.; Haji, E.; Khan, A.H.; Khatlani, T.S.; Bouchama, A. Obesity and COVID-19: What makes obese host so vulnerable? Immun. Ageing I A 2021, 18, 1. [Google Scholar] [CrossRef]
- Ji, D.; Zhang, D.; Xu, J.; Chen, Z.; Yang, T.; Zhao, P.; Chen, G.; Cheng, G.; Wang, Y.; Bi, J.; et al. Prediction for Progression Risk in Patients With COVID-19 Pneumonia: The CALL Score. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 1393–1399. [Google Scholar] [CrossRef] [Green Version]
- Huang, G.; Kovalic, A.J.; Graber, C.J. Prognostic Value of Leukocytosis and Lymphopenia for Coronavirus Disease Severity. Emerg. Infect. Dis. 2020, 26, 1839–1841. [Google Scholar] [CrossRef]
- Luo, X.; Zhou, W.; Yan, X.; Guo, T.; Wang, B.; Xia, H.; Ye, L.; Xiong, J.; Jiang, Z.; Liu, Y.; et al. Prognostic Value of C-Reactive Protein in Patients With Coronavirus 2019. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 2174–2179. [Google Scholar] [CrossRef]
- Kaufman, A.E.; Naidu, S.; Ramachandran, S.; Kaufman, D.S.; Fayad, Z.A.; Mani, V. Review of radiographic findings in COVID-19. World J. Radiol. 2020, 12, 142–155. [Google Scholar] [CrossRef]
- Khosravi, B.; Aghaghazvini, L.; Sorouri, M.; Naybandi Atashi, S.; Abdollahi, M.; Mojtabavi, H.; Khodabakhshi, M.; Motamedi, F.; Azizi, F.; Rajabi, Z.; et al. Predictive value of initial CT scan for various adverse outcomes in patients with COVID-19 pneumonia. Heart Lung J. Crit. Care 2021, 50, 13–20. [Google Scholar] [CrossRef]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef]
- Touw, H.R.; Tuinman, P.R.; Gelissen, H.P.; Lust, E.; Elbers, P.W. Lung ultrasound: Routine practice for the next generation of internists. Neth. J. Med. 2015, 73, 100–107. [Google Scholar]
- Jackson, K.; Butler, R.; Aujayeb, A. Lung ultrasound in the COVID-19 pandemic. Postgrad. Med. J. 2021, 97, 34–39. [Google Scholar] [CrossRef]
- Lieveld, A.W.E.; Kok, B.; Schuit, F.H.; Azijli, K.; Heijmans, J.; van Laarhoven, A.; Assman, N.L.; Kootte, R.S.; Olgers, T.J.; Nanayakkara, P.W.B.; et al. Diagnosing COVID-19 pneumonia in a pandemic setting: Lung Ultrasound versus CT (LUVCT)—A multicentre, prospective, observational study. ERJ Open Res. 2020, 6. [Google Scholar] [CrossRef]
- Ragnoli, B.; Malerba, M. Focus on the Potential Role of Lung Ultrasound in COVID-19 Pandemic: What More to Do? Int. J. Environ. Res. Public Health 2020, 17, 8398. [Google Scholar] [CrossRef]
- Ottaviani, S.; Franc, M.; Ebstein, E.; Demaria, L.; Lheure, C.; Debray, M.P.; Khalil, A.; Crestani, B.; Borie, R.; Dieude, P. Lung ultrasonography in patients with COVID-19: Comparison with CT. Clin. Radiol. 2020, 75, 877.e1–877.e6. [Google Scholar] [CrossRef]
- Lu, W.; Zhang, S.; Chen, B.; Chen, J.; Xian, J.; Lin, Y.; Shan, H.; Su, Z.Z. A Clinical Study of Noninvasive Assessment of Lung Lesions in Patients with Coronavirus Disease-19 (COVID-19) by Bedside Ultrasound. Ultraschall Der Med. 2020, 41, 300–307. [Google Scholar] [CrossRef]
- Nouvenne, A.; Zani, M.D.; Milanese, G.; Parise, A.; Baciarello, M.; Bignami, E.G.; Odone, A.; Sverzellati, N.; Meschi, T.; Ticinesi, A. Lung Ultrasound in COVID-19 Pneumonia: Correlations with Chest CT on Hospital admission. Respir. Int. Rev. Thorac. Dis. 2020, 99, 617–624. [Google Scholar] [CrossRef]
- Pivetta, E.; Goffi, A.; Tizzani, M.; Locatelli, S.M.; Porrino, G.; Losano, I.; Leone, D.; Calzolari, G.; Vesan, M.; Steri, F.; et al. Lung Ultrasonography for the Diagnosis of SARS-CoV-2 Pneumonia in the Emergency Department. Ann. Emerg. Med. 2021, 77, 385–394. [Google Scholar] [CrossRef]
- Gutsche, H.; Lesser, T.G.; Wolfram, F.; Doenst, T. Significance of Lung Ultrasound in Patients with Suspected COVID-19 Infection at Hospital Admission. Diagnostics 2021, 11, 921. [Google Scholar] [CrossRef]
- Ji, L.; Cao, C.; Gao, Y.; Zhang, W.; Xie, Y.; Duan, Y.; Kong, S.; You, M.; Ma, R.; Jiang, L.; et al. Prognostic value of bedside lung ultrasound score in patients with COVID-19. Crit. Care 2020, 24, 700. [Google Scholar] [CrossRef]
- Castelao, J.; Graziani, D.; Soriano, J.B.; Izquierdo, J.L. Findings and Prognostic Value of Lung Ultrasound in COVID-19 Pneumonia. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2020, 40, 1315–1324. [Google Scholar] [CrossRef]
- Lichter, Y.; Topilsky, Y.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; Gal Oz, A.; Vine, J.; Goren, O.; Cohen, B.; et al. Lung ultrasound predicts clinical course and outcomes in COVID-19 patients. Intensive Care Med. 2020, 46, 1873–1883. [Google Scholar] [CrossRef]
- Brahier, T.; Meuwly, J.Y.; Pantet, O.; Brochu Vez, M.J.; Gerhard Donnet, H.; Hartley, M.A.; Hugli, O.; Boillat-Blanco, N. Lung ultrasonography for risk stratification in patients with COVID-19: A prospective observational cohort study. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020. [Google Scholar] [CrossRef]
- de Alencar, J.C.G.; Marchini, J.F.M.; Marino, L.O.; da Costa Ribeiro, S.C.; Bueno, C.G.; da Cunha, V.P.; Lazar Neto, F.; Brandao Neto, R.A.; Souza, H.P.; Team, C.U.S.P.R. Lung ultrasound score predicts outcomes in COVID-19 patients admitted to the emergency department. Ann. Intensive Care 2021, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Ramos Hernandez, C.; Botana Rial, M.; Pazos Area, L.A.; Nunez Fernandez, M.; Perez Fernandez, S.; Rubianes Gonzalez, M.; Crespo Casal, M.; Fernandez Villar, A. Lung Ultrasound to Predict Unfavorable Progress in Patients Hospitalized for COVID-19. Arch. Bronconeumol. 2021, 57 (Suppl. S1), 47–54. [Google Scholar] [CrossRef]
- WHO. Diagnostic Testing for SARS-CoV-2. Available online: https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2 (accessed on 18 April 2021).
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Buonsenso, D.; Perrone, T.; Briganti, D.F.; Perlini, S.; Torri, E.; Mariani, A.; Mossolani, E.E.; et al. Proposal for International Standardization of the Use of Lung Ultrasound for Patients With COVID-19: A Simple, Quantitative, Reproducible Method. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2020, 39, 1413–1419. [Google Scholar] [CrossRef] [Green Version]
- Zanforlin, A.; Strapazzon, G.; Falk, M.; Gallina, V.; Viteritti, A.; Valzolgher, L.; La Guardia, M.; Ferro, F.; Pagani, L.; Vezzali, N. Lung Ultrasound in the Emergency Department for Early Identification of COVID-19 Pneumonia. Respir. Int. Rev. Thorac. Dis. 2021, 100, 145–153. [Google Scholar] [CrossRef]
- Smith, M.J.; Hayward, S.A.; Innes, S.M.; Miller, A.S.C. Point-of-care lung ultrasound in patients with COVID-19—A narrative review. Anaesthesia 2020, 75, 1096–1104. [Google Scholar] [CrossRef] [Green Version]
- Falgarone, G.; Pamoukdjian, F.; Cailhol, J.; Giocanti-Auregan, A.; Guis, S.; Bousquet, G.; Bouchaud, O.; Seror, O. Lung ultrasound is a reliable diagnostic technique to predict abnormal CT chest scan and to detect oxygen requirements in COVID-19 pneumonia. Aging 2020, 12, 19945–19953. [Google Scholar] [CrossRef]
- European Commission. Attitudes of Europeans towards Tobacco and Electronic cigarettes: Special Eurobarometer 458; European Commission: Brussels, Belgium, 2017. [Google Scholar] [CrossRef]
- Usman, M.S.; Siddiqi, T.J.; Khan, M.S.; Patel, U.K.; Shahid, I.; Ahmed, J.; Kalra, A.; Michos, E.D. Is there a smoker’s paradox in COVID-19? BMJ Evid. Based Med. 2020. [Google Scholar] [CrossRef]
- Gonzalez-Rubio, J.; Navarro-Lopez, C.; Lopez-Najera, E.; Lopez-Najera, A.; Jimenez-Diaz, L.; Navarro-Lopez, J.D.; Najera, A. A Systematic Review and Meta-Analysis of Hospitalised Current Smokers and COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 7394. [Google Scholar] [CrossRef]
- Farsalinos, K.; Bagos, P.G.; Giannouchos, T.; Niaura, R.; Barbouni, A.; Poulas, K. Smoking prevalence among hospitalized COVID-19 patients and its association with disease severity and mortality: An expanded re-analysis of a recent publication. Harm Reduct. J. 2021, 18, 9. [Google Scholar] [CrossRef]
- Strzelak, A.; Ratajczak, A.; Adamiec, A.; Feleszko, W. Tobacco Smoke Induces and Alters Immune Responses in the Lung Triggering Inflammation, Allergy, Asthma and Other Lung Diseases: A Mechanistic Review. Int. J. Environ. Res. Public Health 2018, 15, 1033. [Google Scholar] [CrossRef] [Green Version]
- Sopori, M. Effects of cigarette smoke on the immune system. Nat. Rev. Immunol. 2002, 2, 372–377. [Google Scholar] [CrossRef]
- Nizri, E.; Irony-Tur-Sinai, M.; Lory, O.; Orr-Urtreger, A.; Lavi, E.; Brenner, T. Activation of the cholinergic anti-inflammatory system by nicotine attenuates neuroinflammation via suppression of Th1 and Th17 responses. J. Immunol. 2009, 183, 6681–6688. [Google Scholar] [CrossRef] [Green Version]
- Arnson, Y.; Shoenfeld, Y.; Amital, H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J. Autoimmun. 2010, 34, J258–J265. [Google Scholar] [CrossRef]
- Margaritopoulos, G.A.; Vasarmidi, E.; Jacob, J.; Wells, A.U.; Antoniou, K.M. Smoking and interstitial lung diseases. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 2015, 24, 428–435. [Google Scholar] [CrossRef]
- Rojatti, M.; Regli, I.B.; Zanforlin, A.; Ferretti, E.; Falk, M.; Strapazzon, G.; Gamper, M.; Zanon, P.; Bock, M.; Rauch, S. Lung Ultrasound and Respiratory Pathophysiology in Mechanically Ventilated COVID-19 Patients-an Observational Trial. SN Compr. Clin. Med. 2020, 2, 1970–1977. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).