Risk Factors in Third and Fourth Degree Perineal Tears in Women in a Tertiary Centre: An Observational Ambispective Cohort Study
Abstract
:1. Introduction
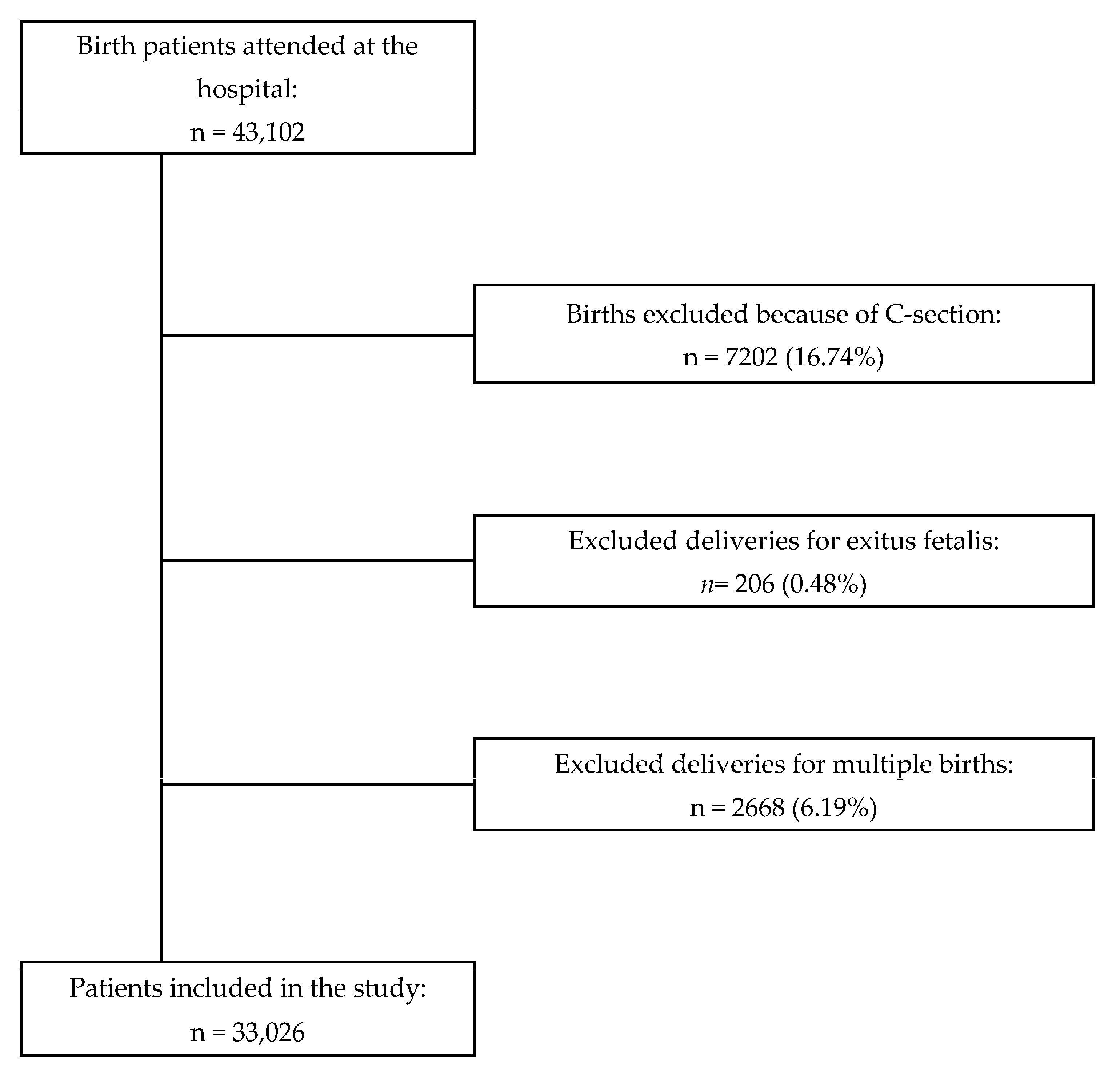
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OR | Odds ratio |
| C-Section | Caesarean birth |
| UI | Urinary incontinence |
| FI | Fecal incontinence |
| AI | Anal incontinence |
| pH | Hydrogen potential |
| CI | Confidence interval |
| I2 | I squared |
| PGE1 | Prostaglandin E1 |
| PGE2 | Prostaglandin E2 |
| WHO | World Health Organization |
| HGUGM | Gregorio Marañón General University Hospital in Madrid |
References
- Fenner, D.E.; Genberg, B.; Brahma, P.; Marek, L.; DeLancey, J.O. Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am. J. Obstet. Gynecol. 2003, 189, 1543–1549. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.G.; Leeman, L.M.; Borders, N.; Qualls, C.; Fullilove, A.M.; Teaf, D.; Hall, R.J.; Bedrick, E.; Albers, L.L. Contribution of the second stage of labour to pelvic floor dysfunction: A prospective cohort comparison of nulliparous women. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 1145–1153. [Google Scholar] [CrossRef]
- Hsieh, W.-C.; Liang, C.-C.; Wu, D.; Chang, S.-D.; Chueh, H.-Y.; Chao, A.-S. Prevalence and contributing factors of severe perineal damage following episiotomy-assisted vaginal delivery. Taiwan. J. Obstet. Gynecol. 2014, 53, 481–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blondel, B.; Alexander, S.; Bjarnadóttir, R.I.; Gissler, M.; Langhoff-Roos, J.; Novak-Antolič, Ž.; Prunet, C.; Zhang, W.-H.; Hindori-Mohangoo, A.D.; Zeitlin, J.; et al. Variations in rates of severe perineal tears and episiotomies in 20 European countries: A study based on routine national data in Euro-Peristat Project. Acta Obstet. Gynecol. Scand. 2016, 95, 746–754. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 165: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet. Gynecol. 2016, 128, e1–e15. [Google Scholar] [CrossRef]
- Lin, S.; Atan, I.K.; Dietz, H.P.; Herbison, P.; Wilson, P.D. Delivery mode, levator avulsion and obstetric anal sphincter injury: A cross-sectional study 20 years after childbirth. Aust. N. Z. J. Obstet. Gynaecol. 2019, 59, 590–596. [Google Scholar] [CrossRef] [Green Version]
- Abedzadeh-Kalahroudi, M.; Talebian, A.; Sadat, Z.; Mesdaghinia, E. Perineal trauma: Incidence and its risk factors. J. Obstet. Gynaecol. 2019, 39, 206–211. [Google Scholar] [CrossRef]
- Hawkins, J.L. Epidural analgesia for labor and delivery. N. Engl. J. Med. 2010, 362, 1503–1510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sng, B.L.; Leong, W.L.; Zeng, Y.; Siddiqui, F.J.; Assam, P.N.; Lim, Y.; Chan, E.S.; Sia, A.T. Early versus late initiation of epidural analgesia for labour. Cochrane Database Syst. Rev. 2014, 10, CD007238. [Google Scholar] [CrossRef] [Green Version]
- Anim-Somuah, M.; Smyth, R.M.; Cyna, A.M.; Cuthbert, A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst. Rev. 2018, 5, CD000331. [Google Scholar] [CrossRef]
- Gebuza, G.; Kaźmierczak, M.; Gdaniec, A.; Mieczkowska, E.; Gierszewska, M.; Dombrowska-Pali, A.; Banaszkiewicz, M.; Maleńczyk, M. Episiotomy and perineal tear risk factors in a group of 4493 women. Health Care Women Int. 2018, 39, 663–683. [Google Scholar] [CrossRef]
- Junior, M.D.C.; Júnior, R.P. Selective Episiotomy: Indications, Techinique, and Association with Severe Perineal Lacerations. Rev. Bras. Ginecol. Obstet. 2016, 38, 301–307. [Google Scholar] [CrossRef] [Green Version]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017, 2, CD000081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leombroni, M.; Buca, D.; Liberati, M.; Falò, E.; Rizzo, G.; Khalil, A.; Manzoli, L.; Flacco, M.E.; Santarelli, A.; Makatsariya, A.; et al. Post-partum pelvic floor dysfunction assessed on 3D rotational ultrasound: A prospective study on women with first- and second-degree perineal tears and episiotomy. J. Matern. Neonatal Med. 2021, 34, 445–455. [Google Scholar] [CrossRef]
- WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018.
- Mahgoub, S.; Piant, H.; Gaudineau, A.; Lefebvre, F.; Langer, B.; Koch, A. Risk factors for obstetric anal sphincter injuries (OASIS) and the role of episiotomy: A retrospective series of 496 cases. J. Gynecol. Obs. Hum. Reprod. 2019, 48, 657–662. [Google Scholar] [CrossRef]
- Wilson, A.N.; Homer, C.S. Third- and fourth-degree tears: A review of the current evidence for prevention and management. Aust. N. Z. J. Obstet. Gynaecol. 2020, 60, 175–182. [Google Scholar] [CrossRef]
- O’Mahony, F.; Hofmeyr, G.J.; Menon, V. Choice of instruments for assisted vaginal delivery. Cochrane Database Syst. Rev. 2010, 11, CD005455. [Google Scholar] [CrossRef]
- Gommesen, D.; Nohr, E.A.; Drue, H.C.; Qvist, N.; Rasch, V. Obstetric perineal tears: Risk factors, wound infection and dehiscence: A prospective cohort study. Arch. Gynecol. Obstet. 2019, 300, 67–77. [Google Scholar] [CrossRef]
- Anglim, B.; Kelly, L.; Fitzpatrick, M. Risk factors and outcome of repair of obstetric anal sphincter injuries as followed up in a dedicated perineal clinic. Int. Urogynecol. J. 2019, 30, 1649–1655. [Google Scholar] [CrossRef]
- Simic, M.; Cnattingius, S.; Petersson, G.; Sandström, A.; Stephansson, O. Duration of second stage of labor and instrumental delivery as risk factors for severe perineal lacerations: Population-based study. BMC Pregnancy Childbirth 2017, 17, 72. [Google Scholar] [CrossRef] [Green Version]
- Baghestan, E.; Irgens, L.M.; Børdahl, P.E.; Rasmussen, S. Trends in Risk Factors for Obstetric Anal Sphincter Injuries in Norway. Obstet. Gynecol. 2010, 116, 25–34. [Google Scholar] [CrossRef]
- Gurol-Urganci, I.; Cromwell, D.A.; Edozien, L.C.; Mahmood, T.A.; Adams, E.J.; Richmond, D.H.; Templeton, A.; Van Der Meulen, J.H. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: Time trends and risk factors. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 1516–1525. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, A.; Gabbay Benziv, R.; Hiersch, L.; Ashwal, E.; Aviram, R.; Yogev, Y.; Aviram, A. Episiotomy—Risk factors and outcomes. J. Matern. Fetal Neonatal Med. 2017, 30, 251–256. [Google Scholar] [CrossRef]
- Leeman, L.; Rogers, R.; Borders, N.; Teaf, D.; Qualls, C. The Effect of Perineal Lacerations on Pelvic Floor Function and Anatomy at 6 Months Postpartum in a Prospective Cohort of Nulliparous Women. Birth 2016, 43, 293–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellussi, F.; Montaguti, E.; Youssef, A.; Salsi, G.; Ghi, T.; Pilu, G. Dynamic 2-dimensional transperineal ultrasound evaluation in labor room as a screening tool for anal sphincter injuries and anal incontinence in primiparous women. Am. J. Obs. Gynecol. MFM 2019, 1, 100037. [Google Scholar] [CrossRef] [PubMed]
| Overall n = 33,026 | Group I n = 301 | Group II n = 32,725 | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| n (%) | n (%) | n (%) | p | ||||
| Maternal age at birth (Years) | 32 | ±5.74 | 32.36 | ±5.57 | 32.22 | ±5.79 | <0.001 |
| Groups | 0.483 | ||||||
| Under 25 | 3855 (11.7) | 27 (9.0) | 3828 (11.7) | ||||
| 25 to 30 | 5743 (17.4) | 57 (18.9) | 5686 (17.4) | ||||
| 30 to 35 | 11,335 (34.3) | 112 (37.2) | 11,223 (34.3) | ||||
| 35 to 40 | 9700 (29.4) | 84 (27.9) | 9616 (29.4) | ||||
| >40 | 2327 (7.0) | 21 (7.0) | 2306 (7.0) | ||||
| N/A | 66 (0.2) | 0 (0) | 66 (0.2) | ||||
| Nulliparity | 16,019 (52.3) | 238 (79.1) | 15,781 (48,2) | <0.001 | |||
| Gestational age at delivery | 39.01 | ±1.78 | 38.99 | ±1.60 | 38.58 | ±2.42 | <0.001 |
| Induced delivery | 7088 (23.1) | 84 (27.9) | 7004 (21.4) | 0.046 | |||
| Type of anaesthesia | 0.003 | ||||||
| None | 2428 (7.3) | 8 (2.7) | 2420 (7.4) | ||||
| Perineal | 2875 (8,7) | 32 (10.6) | 2843 (8.7) | ||||
| Epidural and/or spinal | 25,319 (76.7) | 258 (85.7) | 25,061 (76,6) | ||||
| General | 2404 (7.3) | 3 (1.0) | 2401 (7.3) | ||||
| Instrumental delivery | 6643 (21.7) | 158 (52.5) | 6485 (19.8) | <0.001 | |||
| Episiotomy procedure at delivery | 18,025 (59.0) | 248 (82.4) | 17,777 (54.3) | <0.001 | |||
| Cord blood pH after delivery | 7.28 | ±0.76 | 7.29 | ±0.07 | 7.28 | ±0.08 | <0.001 |
| Weight of newborn | 3237 | ±483.94 | 3,259 | ±471.82 | 3,130 | ±609.87 | <0.001 |
| Test Apgar 1 (1 min.) | 8.75 | ±0.09 | 8.85 | ±0.92 | 8.55 | ±1.21 | <0.001 |
| Test Apgar 2 (5 min.) | 9.68 | ±0.65 | 9.73 | ±0.80 | 9.55 | ±0.97 | <0.001 |
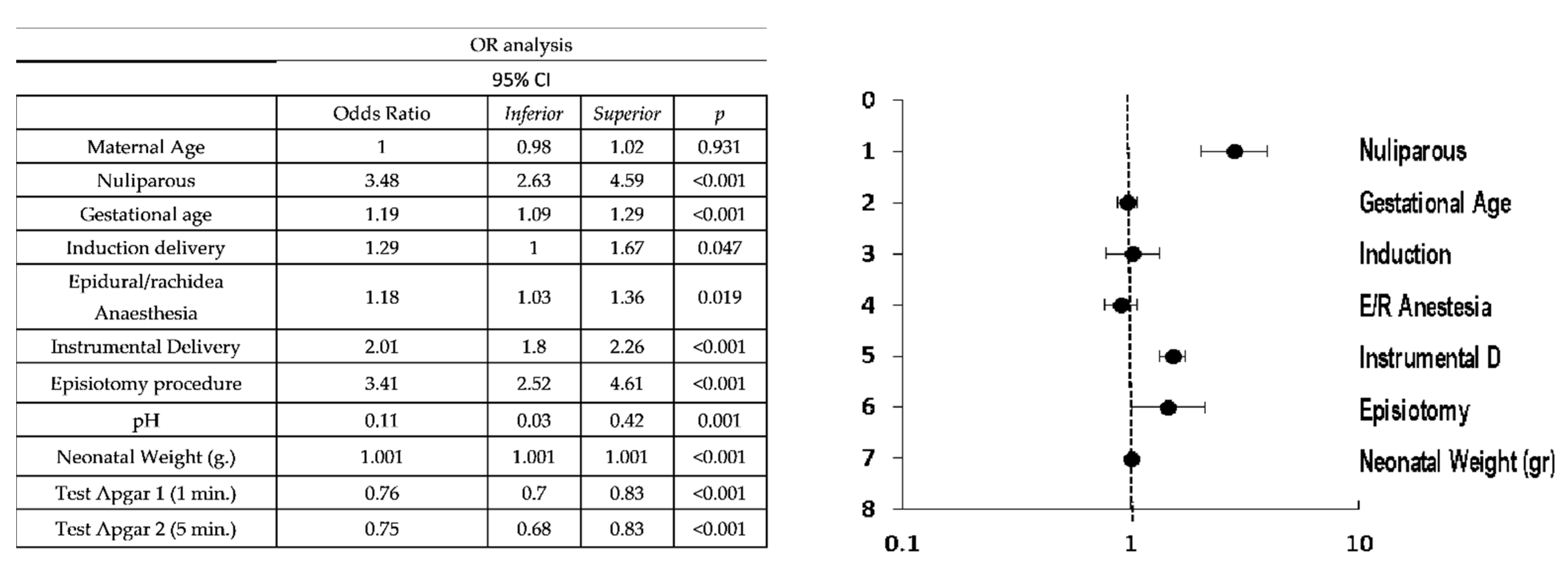
| 95% CI | ||||
|---|---|---|---|---|
| Odds Ratio | Inferior | Superior | p | |
| Maternal Age | ||||
| Nuliparous | 2.82 | 2.02 | 3.94 | <0.001 |
| Gestational age | 0.97 | 0.88 | 1.07 | 0.542 |
| Induction delivery | 1.02 | 0.78 | 1.33 | 0.895 |
| Epidural/rachidea Anaesthesia | 0.91 | 0.77 | 1.06 | 0.216 |
| Instrumental Delivery | 1.52 | 1.33 | 1.74 | <0.001 |
| Episiotomy procedure | 1.46 | 1.01 | 2.11 | 0.045 |
| pH | 1.77 | 0.35 | 9.01 | 0.491 |
| Neonatal Weight (g.) | 1.001 | 1.001 | 1.001 | <0.001 |
| Test Apgar 1 (1 min.) | 0.92 | 0.79 | 1.07 | 0.299 |
| Test Apgar 2 (5 min.) | 0.84 | 0.68 | 1.02 | 0.083 |
| 95% CI | ||||
|---|---|---|---|---|
| Odds Ratio | Inferior | Superior | p | |
| Nulliparity | 3.48 | 2.65 | 4.62 | <0.001 |
| Gestation at term (>38 weeks) | 2.11 | 1.32 | 3.36 | 0.002 |
| Induction delivery | 1.29 | 1 | 1.67 | 0.047 |
| Instrumental Delivery | ||||
| Forceps | 4.51 | 3.57 | 5.7 | <0.001 |
| Vacuum | 1.41 | 0.69 | 2.88 | 0.345 |
| Spatula | 4.35 | 2.02 | 9.37 | <0.001 |
| Eutocic Delivery | ||||
| Episiotomy procedure | 1.98 | 1.4 | 2.79 | <0.001 |
| Episiotomy procedure | ||||
| Instrumental delivery | 3.11 | 2.40 | 4.02 | <0.001 |
| Fetal Weight | ||||
| >3000 g | 2.41 | 1.73 | 3.37 | <0.001 |
| >3500 g | 1.97 | 1.56 | 2.47 | <0.001 |
| >4000 g | 2.17 | 1.46 | 3.24 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barca, J.A.; Bravo, C.; Pintado-Recarte, M.P.; Cueto-Hernández, I.; Ruiz-Labarta, J.; Cuñarro, Y.; Buján, J.; Alvarez-Mon, M.; Ortega, M.A.; De León-Luis, J.A. Risk Factors in Third and Fourth Degree Perineal Tears in Women in a Tertiary Centre: An Observational Ambispective Cohort Study. J. Pers. Med. 2021, 11, 685. https://doi.org/10.3390/jpm11080685
Barca JA, Bravo C, Pintado-Recarte MP, Cueto-Hernández I, Ruiz-Labarta J, Cuñarro Y, Buján J, Alvarez-Mon M, Ortega MA, De León-Luis JA. Risk Factors in Third and Fourth Degree Perineal Tears in Women in a Tertiary Centre: An Observational Ambispective Cohort Study. Journal of Personalized Medicine. 2021; 11(8):685. https://doi.org/10.3390/jpm11080685
Chicago/Turabian StyleBarca, Juan A., Coral Bravo, Maria P. Pintado-Recarte, Ignacio Cueto-Hernández, Javier Ruiz-Labarta, Yolanda Cuñarro, Julia Buján, Melchor Alvarez-Mon, Miguel A. Ortega, and Juan A. De León-Luis. 2021. "Risk Factors in Third and Fourth Degree Perineal Tears in Women in a Tertiary Centre: An Observational Ambispective Cohort Study" Journal of Personalized Medicine 11, no. 8: 685. https://doi.org/10.3390/jpm11080685
APA StyleBarca, J. A., Bravo, C., Pintado-Recarte, M. P., Cueto-Hernández, I., Ruiz-Labarta, J., Cuñarro, Y., Buján, J., Alvarez-Mon, M., Ortega, M. A., & De León-Luis, J. A. (2021). Risk Factors in Third and Fourth Degree Perineal Tears in Women in a Tertiary Centre: An Observational Ambispective Cohort Study. Journal of Personalized Medicine, 11(8), 685. https://doi.org/10.3390/jpm11080685










