Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis
Abstract
:1. Introduction
2. Materials and Methods
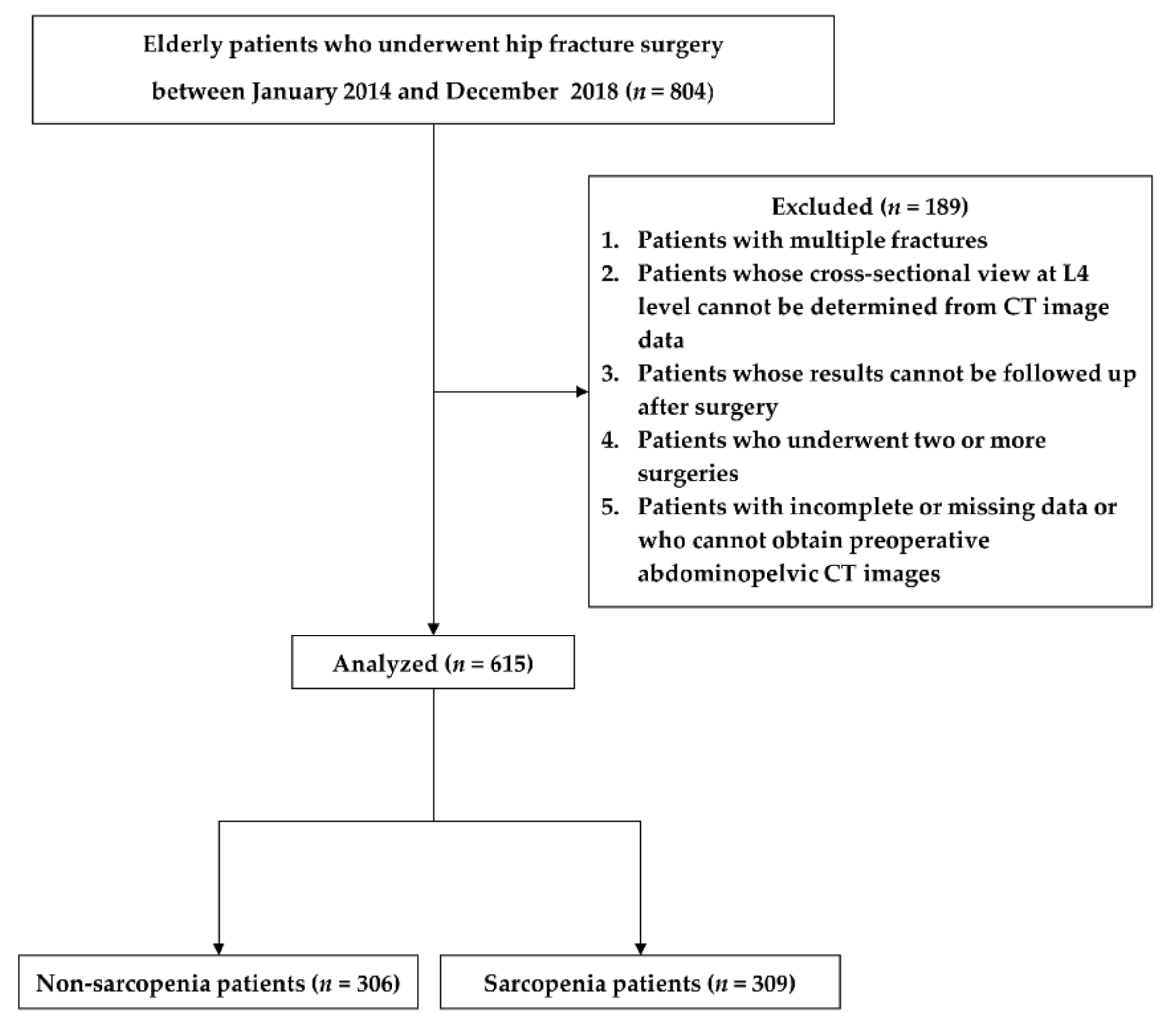
2.1. Study Design and Patients
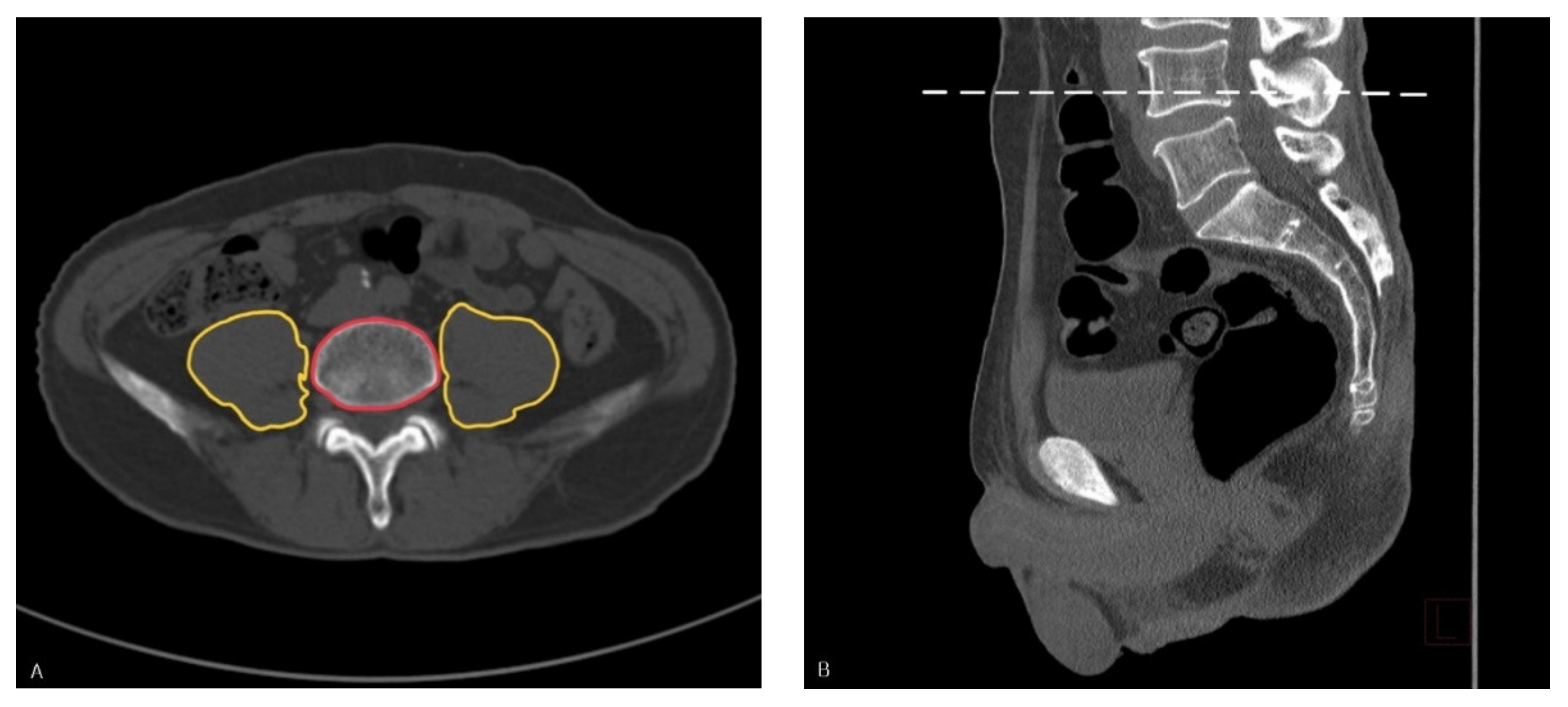
2.2. Measurements
2.3. Data Collection and Outcome Assessment
2.4. Statistical Analyses
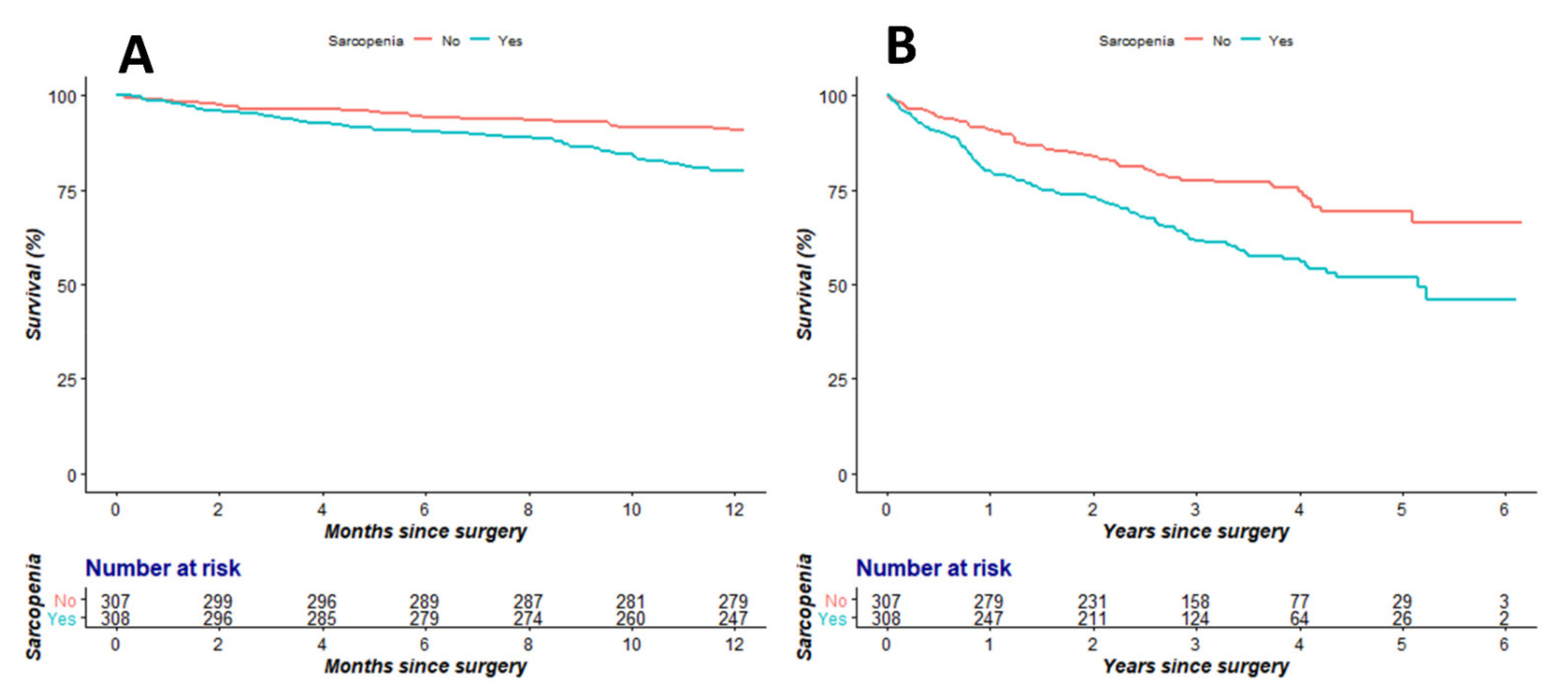
3. Results
Study Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Lin, K.B.; Yang, N.P.; Lee, Y.H.; Chan, C.L.; Wu, C.H.; Chen, H.C.; Chang, N.T. The incidence and factors of hip fractures and subsequent morbidity in Taiwan: An 11-Year Population-Based cohort study. PLoS ONE 2018, 13, e0192388. [Google Scholar] [CrossRef]
- Lewiecki, E.M.; Wright, N.C.; Curtis, J.R.; Siris, E.; Gagel, R.F.; Saag, K.G.; Singer, A.J.; Steven, P.M.; Adler, R.A. Hip fracture trends in the United States, 2002 to 2015. Osteoporos. Int. 2018, 29, 717–722. [Google Scholar] [CrossRef]
- Kannus, P.; Parkkari, J.; Sievänen, H.; Heinonen, A.; Vuori, I.; Järvinen, M. Epidemiology of hip fractures. Bone 1996, 18, s57–s63. [Google Scholar] [CrossRef]
- Huette, P.; Abou-Arab, O.; Djebara, A.E.; Terrasi, B.; Beyls, C.; Guinot, P.G.; Havet, E.; Dupont, H.; Lorne, E.; Ntouba, A.; et al. Risk factors and mortality of patients undergoing hip fracture surgery: A One-Year Follow-Up study. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.D.; Park, S.J.; Lee, D.H.; Jee, D.L. Risk factors of morbidity and mortality following hip fracture surgery. Korean J. Anesthesiol. 2013, 64, 505–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, S.J.G.; Frizelle, F.A.; Geddes, J.A.; Eglinton, T.W.; Hampton, M.B. Frailty in surgical patients. Int. J. Colorectal Dis. 2018, 33, 1657–1666. [Google Scholar] [CrossRef] [PubMed]
- Walston, J.; Hadley, E.C.; Ferrucci, L.; Guralnik, J.M.; Newman, A.B.; Studenski, S.A.; Ershler, W.B.; Harris, T.; Fried, L.P. Research agenda for frailty in older adults: Toward a better understanding of physiology and etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 991–1001. [Google Scholar] [CrossRef]
- Carneiro, J.A.; Cardoso, R.R.; Durães, M.S.; Guedes, M.C.A.; Santos, F.L.; Costa, F.M.D.; Caldeira, A.P. Frailty in the elderly: Prevalence and associated factors. Rev. Bras. Enferm. 2017, 70, 747–752. [Google Scholar] [CrossRef] [Green Version]
- Campbell, A.J.; Buchner, D.M. Unstable disability and the fluctuations of frailty. Age Ageing 1997, 26, 315–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Lee, J.S.-J.; He, K.; Harbaugh, C.M.; Schaubel, D.E.; Sonnenday, C.J.; Wang, S.C.; Englesbe, M.J.; Eliason, J.L. Michigan Analytic Morphomics Group. Frailty, core muscle size, and mortality in patients undergoing open abdominal aortic aneurysm repair. J. Vasc. Surg. 2011, 53, 912–917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moskven, E.; Bourassa-Moreau, E.; Charest-Morin, R.; Flexman, A.; Street, J. The impact of frailty and sarcopenia on postoperative outcomes in adult spine surgery. A systematic review of the literature. Spine J. 2018, 18, 2354–2369. [Google Scholar] [CrossRef] [PubMed]
- James, L.A.; Levin, M.A.; Lin, H.M.; Deiner, S.G. Association of Preoperative Frailty with Intraoperative Hemodynamic Instability and Postoperative Mortality. Anesth. Analg. 2019, 128, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Bautista, M.A.C.; Malhotra, R. Identification and Measurement of Frailty: A Scoping Review of Published Research from Singapore. Ann. Acad. Med. Singap. 2018, 47, 455–491. [Google Scholar] [PubMed]
- Walston, J.; Buta, B.; Xue, Q.L. Frailty Screening and Interventions: Considerations for Clinical Practice. Clin. Geriatr. Med. 2018, 34, 25–38. [Google Scholar] [CrossRef]
- Thompson, M.Q.; Yu, S.; Tucker, G.R.; Adams, R.J.; Cesari, M.; Theou, O.; Visvanathan, R. Frailty and sarcopenia in combination are more predictive of mortality than either condition alone. Maturitas 2021, 144, 102–107. [Google Scholar] [CrossRef]
- Ebbeling, L.; Grabo, D.J.; Shashaty, M.; Dua, R.; Sonnad, S.S.; Sims, C.A.; Pascual, J.L.; Schwab, C.W.; Holena, D.N. Psoas: Lumbar vertebra index: Central sarcopenia independently predicts morbidity in elderly trauma patients. Eur. J. Trauma Emerg. Surg. 2014, 40, 57–65. [Google Scholar] [CrossRef]
- Hawkins, R.B.; Mehaffey, J.H.; Charles, E.J.; Kern, J.A.; Lim, D.S.; Teman, N.R.; Ailawadi, G. Psoas Muscle Size Predicts Risk-Adjusted Outcomes After Surgical Aortic Valve Replacement. Ann. Thorac. Surg. 2018, 106, 39–45. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, P.M.; Collinge, C.A.; O’Neill, D.E.; Bible, J.E.; Mir, H.R. Sarcopenia is Predictive of 1-Year Mortality After Acetabular Fractures in Elderly Patients. J. Orthop. Trauma 2018, 32, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.I.; Doleman, B.; Scott, S.; Lund, J.N.; Williams, J.P. Simple psoas Cross-Sectional area measurement is a quick and easy method to assess sarcopenia and predicts major surgical complications. Colorectal Dis. 2015, 17, O20–O26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okamura, H.; Kimura, N.; Tanno, K.; Mieno, M.; Matsumoto, H.; Yamaguchi, A.; Adachi, H. The impact of preoperative sarcopenia, defined based on psoas muscle area, on Long-Term outcomes of heart valve surery. J. Thorac. Cardiovasc. Surg. 2019, 157, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Swanson, S.; Patterson, R.B. The correlation between the psoas muscle/vertebral body ratio and the severity of peripheral artery disease. Ann. Vasc. Surg. 2015, 29, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Newton, D.H.; Kim, C.; Lee, N.; Wolfe, L.; Pfeifer, J.; Amendola, M. Sarcopenia predicts poor Long-Term survival in patients undergoing endovascular aortic aneurysm repair. J. Vasc. Surg. 2018, 67, 453–459. [Google Scholar] [CrossRef]
- Liu, P.; Hao, Q.; Hai, S.; Wang, H.; Cao, L.; Dong, B. Sarcopenia as a predictor of All-Cause mortality among community-dwelling older people: A systematic review and Meta-Analysis. Maturitas 2017, 103, 16–22. [Google Scholar] [CrossRef]
- Hajibandeh, S.; Hajibandeh, S.; Jarvis, R.; Bhogal, T.; Dalmia, S. Meta-Analysis of the effect of sarcopenia in predicting postoperative mortality in emergency and elective abdominal surgery. Surgeon 2019, 17, 370–380. [Google Scholar] [CrossRef]
- Nascimento, C.M.; Ingles, M.; Salvador-Pascual, A.; Cominetti, M.R.; Gomez-Cabrera, M.C.; Viña, J. Sarcopenia, frailty and their prevention by exercise. Free Radic. Biol. Med. 2019, 132, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.A.; Zenilman, M.E. The impact of frailty in the elderly on the outcome of surgery in the aged. Adv. Surg. 2010, 44, 229–249. [Google Scholar] [CrossRef]
- Abraham, A.; Burrows, S.; Abraham, N.J.; Mandal, B. Modified frailty index and hypoalbuminemia as predictors of adverse outcomes in older adults presenting to acute general surgical unit. Rev. Esp. Geriatr. Gerontol. 2020, 55, 70–75. [Google Scholar] [CrossRef]
- Ryan, S.; Politzer, C.; Fletcher, A.; Bolognesi, M.; Seyler, T. Preoperative Hypoalbuminemia Predicts Poor Short-Term Outcomes for Hip Fracture Surgery. Orthopedics 2018, 41, e789–e796. [Google Scholar] [CrossRef]
- Kim, S.; McClave, S.A.; Martindale, R.G.; Miller, K.R.; Hurt, R.T. Hypoalbuminemia and Clinical Outcomes: What is the Mechanism behind the Relationship? Am. Surg. 2017, 83, 1220–1227. [Google Scholar] [CrossRef]
- Loftus, T.J.; Brown, M.P.; Slish, J.H.; Rosenthal, M.D. Serum Levels of Prealbumin and Albumin for Preoperative Risk Stratification. Nutr. Clin. Pract. 2019, 34, 340–348. [Google Scholar] [CrossRef]
- Sim, S.D.; Sim, Y.E.; Tay, K.; Howe, T.S.; Png, M.A.; Chang, C.C.P.; Abdullah, H.R.; Koh, J.S.B. Preoperative hypoalbuminemia: Poor functional outcomes and quality of life after hip fracture surgery. Bone 2021, 143, 115567. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Kiesswetter, E.; Drey, M.; Sieber, C.C. Nutrition, frailty, and sarcopenia. Aging Clin. Exp. Res. 2017, 29, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Kane, A.E.; Sinclair, D.A. Frailty biomarkers in humans and rodents: Current approaches and future advances. Mech. Ageing Dev. 2019, 180, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Nam, J.S.; Kim, W.J.; An, S.M.; Choi, D.K.; Chin, J.H.; Lee, E.H.; Choi, I.C. Age-Dependent relationship between preoperative serum aminotransferase and mortality after cardiovascular surgery. Aging 2019, 11, 9060–9074. [Google Scholar] [CrossRef] [PubMed]
- Al Saedi, A.; Feehan, J.; Phu, S.; Duque, G. Current and emerging biomarkers of frailty in the elderly. Clin. Interv. Aging 2019, 14, 389–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, H.B.; Yan, X.L.; Dong, W.X.; Yu, D.Y.; Zhang, F.M.; Zhou, L.P.; Shen, Z.L.; Cai, G.J.; Zhuang, C.L.; Yu, Z. Sarcopenia is a predictive factor of poor quality of life and prognosis in patients after radical gastrectomy. Eur. J. Surg. Oncol. 2021, 47, 1976–1984. [Google Scholar] [CrossRef]
| Study Population | ||||
|---|---|---|---|---|
| High PLVI | Low PLVI | Total | p-Value | |
| (n = 306) | (n = 309) | (n = 615) | ||
| Demographic variables | ||||
| Age, year | 79.24 ± 7.05 | 82.20 ± 7.97 | 80.73 ± 7.67 | <0.001 |
| Sex, male | 87 (28.4) | 88 (28.5) | 175 (28.5) | 0.990 |
| BMI, kg/m2 | 23.09 ± 3.55 | 21.08 ± 3.85 | 22.08 ± 3.84 | <0.001 |
| DM | 101 (33.0) | 87 (28.2) | 188 (30.6) | 0.192 |
| HTN | 185 (60.5) | 168 (54.4) | 353 (57.4) | 0.127 |
| CVA | 62 (20.3) | 67 (21.7) | 129 (21.0) | 0.665 |
| CVD | 98 (32.0) | 93 (30.1) | 191 (31.1) | 0.605 |
| Pulmonary disease | 64 (20.9) | 74 (23.9) | 138 (22.4) | 0.367 |
| Kidney disease | 39 (12.7) | 37 (12.0) | 76 (12.4) | 0.771 |
| Cognitive impairment | 36 (11.8) | 39 (12.6) | 75 (12.2) | 0.745 |
| ASA | 0.018 | |||
| 2 | 192 (62.7) | 169 (54.7) | 367 (59.7) | |
| 3 | 109 (35.6) | 139 (45.0) | 248 (40.3) | |
| 4 | 5 (1.6) | 1 (0.3) | 6 (1.0) | |
| PLVI | 0.65 ± 0.11 | 0.44 ± 0.09 | 0.55 ± 0.15 | <0.001 |
| Anesthesia type | ||||
| General | 118 (38.6) | 119 (38.5) | 237 (38.5) | 0.990 |
| Spinal | 188 (61.4) | 190 (61.5) | 378 (61.5) | |
| Operation timing | ||||
| Early (≤48 h) | 136 (44.4) | 98 (31.7) | 234 (38.5) | 0.001 |
| Late (>48 h) | 170 (55.6) | 211 (68.3) | 381 (62.0) | |
| Operation type | ||||
| Arthroplasty | 138 (45.1) | 117 (37.9) | 255 (41.5) | 0.069 |
| Osteosynthesis | 168 (54.9) | 192 (62.1) | 360 (58.5) | |
| Laboratory variables | ||||
| Hemoglobin, g/dL | 11.45 ± 1.84 | 10.84 ± 1.92 | 11.20 ± 1.91 | <0.001 |
| Platelet, 109/L | 204.25 ± 74.28 | 211.69 ± 78.18 | 200.00 ± 76.29 | 0.177 |
| WBC, 103/uL | 10.44 ± 3.82 | 9.67 ± 3.64 | 9.60 ± 3.75 | 0.002 |
| CRP, mg/dL | 1.99 ± 3.65 | 2.60 ± 3.89 | 0.640 ± 3.7824 | 0.003 |
| Albumin, g/dL | 3.44 ± 0.44 | 3.22 ± 0.52 | 3.400 ± 0.4933 | <0.001 |
| AST, IU/L | 27.85 ± 22.03 | 24.54 ± 11.00 | 22.00 ± 17.45 | 0.072 |
| ALT, IU/L | 18.02 ± 11.61 | 16.13 ± 9.59 | 15.00 ± 10.67 | 0.013 |
| Creatinine, mg/dL | 1.13 ± 1.25 | 1.04 ± 1.10 | 0.78 ± 1.18 | 0.489 |
| Surgical outcomes | ||||
| Hospital stay (days) | 7.00 (5.00, 10.75) | 7.00 (6.00, 10.00) | 7.00 (5.00, 10.00) | 0.672 |
| Delirium | 75 (24.5) | 84 (27.2) | 159 (25.9) | 0.449 |
| 1 year mortality | 28 (9.2) | 61 (19.7) | 89 (14.5) | <0.001 |
| Overall mortality | 75 (24.5) | 126 (40.8) | 201 (32.7) | <0.001 |
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Low PLVI | 2.26 | 1.45–3.54 | <0.001 | 1.87 | 1.18–2.96 | 0.008 |
| Age | 1.02 | 1.00–1.05 | 0.074 | 1.01 | 0.98–1.04 | 0.354 |
| Sex (male) | 2.02 | 1.33–3.08 | 0.001 | 1.67 | 1.08–2.59 | 0.021 |
| ASA | ||||||
| 2 | 1.00 | 1.00 | ||||
| 3/4 | 2.21 | 1.45–3.37 | <0.001 | 1.47 | 0.92–2.35 | 0.103 |
| BMI | 0.96 | 0.91–1.02 | 0.182 | |||
| DM | 1.79 | 1.18–2.73 | 0.006 | 1.57 | 0.99–2.50 | 0.057 |
| HTN | 1.42 | 0.92–2.20 | 0.111 | 1.15 | 0.72–1.85 | 0.561 |
| CVD | 1.48 | 0.97–2.27 | 0.070 | 1.09 | 0.69–1.73 | 0.698 |
| CVA | 1.47 | 0.92–2.34 | 0.108 | |||
| Cognitive impairment | 1.64 | 0.95–2.81 | 0.074 | 1.24 | 0.70–2.17 | 0.462 |
| Hypoalbuminemia (albumin < 3.5 g/dL) | 2.61 | 1.62–4.20 | <0.001 | 1.65 | 0.99–2.72 | 0.053 |
| Anemia (Hb < 12 g/dL) | 2.49 | 1.41–4.41 | 0.002 | 1.68 | 0.93–3.04 | 0.088 |
| Operation timing | ||||||
| Early (≤48 h) | 1.00 | 1.00 | ||||
| Late (>48 h) | 1.96 | 1.21–3.18 | 0.006 | 1.30 | 0.78–2.17 | 0.308 |
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Low PLVI | 1.84 | 1.38–2.45 | <0.001 | 1.51 | 1.12–2.03 | 0.006 |
| Age | 1.05 | 1.03–1.06 | <0.001 | 1.04 | 1.01–1.06 | 0.001 |
| Sex (male) | 2.16 | 1.63–2.86 | <0.001 | 1.67 | 1.24–2.26 | 0.001 |
| ASA | ||||||
| 2 | 1.00 | 1.00 | ||||
| 3 or 4 | 2.74 | 2.06, 3.64 | <0.001 | 1.78 | 1.30–2.45 | <0.001 |
| BMI | 0.92 | 0.89–0.96 | <0.001 | |||
| DM | 1.67 | 1.26–2.22 | <0.001 | 1.43 | 1.04–1.96 | 0.026 |
| HTN | 1.45 | 1.09–1.94 | 0.011 | 1.21 | 0.89–1.66 | 0.226 |
| CVD | 1.51 | 1.14–2.02 | 0.004 | 1.05 | 0.76–1.43 | 0.782 |
| CVA | 1.83 | 1.35–2.48 | <0.001 | 1.41 | 1.02–1.94 | 0.037 |
| Pulmonary disease | 1.56 | 1.14–2.12 | 0.005 | 0.99 | 0.70–1.41 | 0.971 |
| Kidney disease | 1.69 | 1.17–2.44 | 0.006 | 1.04 | 0.70–1.53 | 0.850 |
| Cognitive impairment | 1.91 | 1.33–2.73 | <0.001 | 1.21 | 0.89–1.66 | 0.226 |
| Anesthesia type | ||||||
| General | 1.00 | 1.00 | ||||
| Spinal | 1.06 | 0.79–1.41 | 0.713 | 1.04 | 0.77–1.41 | 0.802 |
| Hypoalbuminemia (albumin < 3.5 g/dL) | 2.73 | 2.01–3.73 | <0.001 | 1.72 | 1.21–2.44 | 0.002 |
| Anemia (Hb < 12 g/dL) | 2.16 | 1.52–3.05 | <0.001 | 1.42 | 0.97–2.07 | 0.069 |
| CRP | 1.09 | 1.06–1.12 | <0.001 | 1.03 | 1.00–1.07 | 0.045 |
| Operation timing | ||||||
| Early (≤48 h) | 1.00 | 1.00 | ||||
| Late (>48 h) | 1.59 | 1.18–2.14 | 0.003 | 0.93 | 0.66–1.30 | 0.652 |
| Operation type | ||||||
| Arthroplasty | 1.00 | 1.00 | ||||
| Osteosynthesis | 0.86 | 0.65–1.13 | 0.280 | 0.76 | 0.57–1.03 | 0.075 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sim, J.-H.; Lee, S.-H.; Kim, J.-W.; Koh, W.-U.; Kim, H.-T.; Ro, Y.-J.; Kim, H.-J. Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis. J. Pers. Med. 2021, 11, 673. https://doi.org/10.3390/jpm11070673
Sim J-H, Lee S-H, Kim J-W, Koh W-U, Kim H-T, Ro Y-J, Kim H-J. Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis. Journal of Personalized Medicine. 2021; 11(7):673. https://doi.org/10.3390/jpm11070673
Chicago/Turabian StyleSim, Ji-Hoon, Soo-Ho Lee, Ji-Wan Kim, Won-Uk Koh, Hyung-Tae Kim, Young-Jin Ro, and Ha-Jung Kim. 2021. "Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis" Journal of Personalized Medicine 11, no. 7: 673. https://doi.org/10.3390/jpm11070673
APA StyleSim, J.-H., Lee, S.-H., Kim, J.-W., Koh, W.-U., Kim, H.-T., Ro, Y.-J., & Kim, H.-J. (2021). Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis. Journal of Personalized Medicine, 11(7), 673. https://doi.org/10.3390/jpm11070673






