The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review
Abstract
1. Introduction
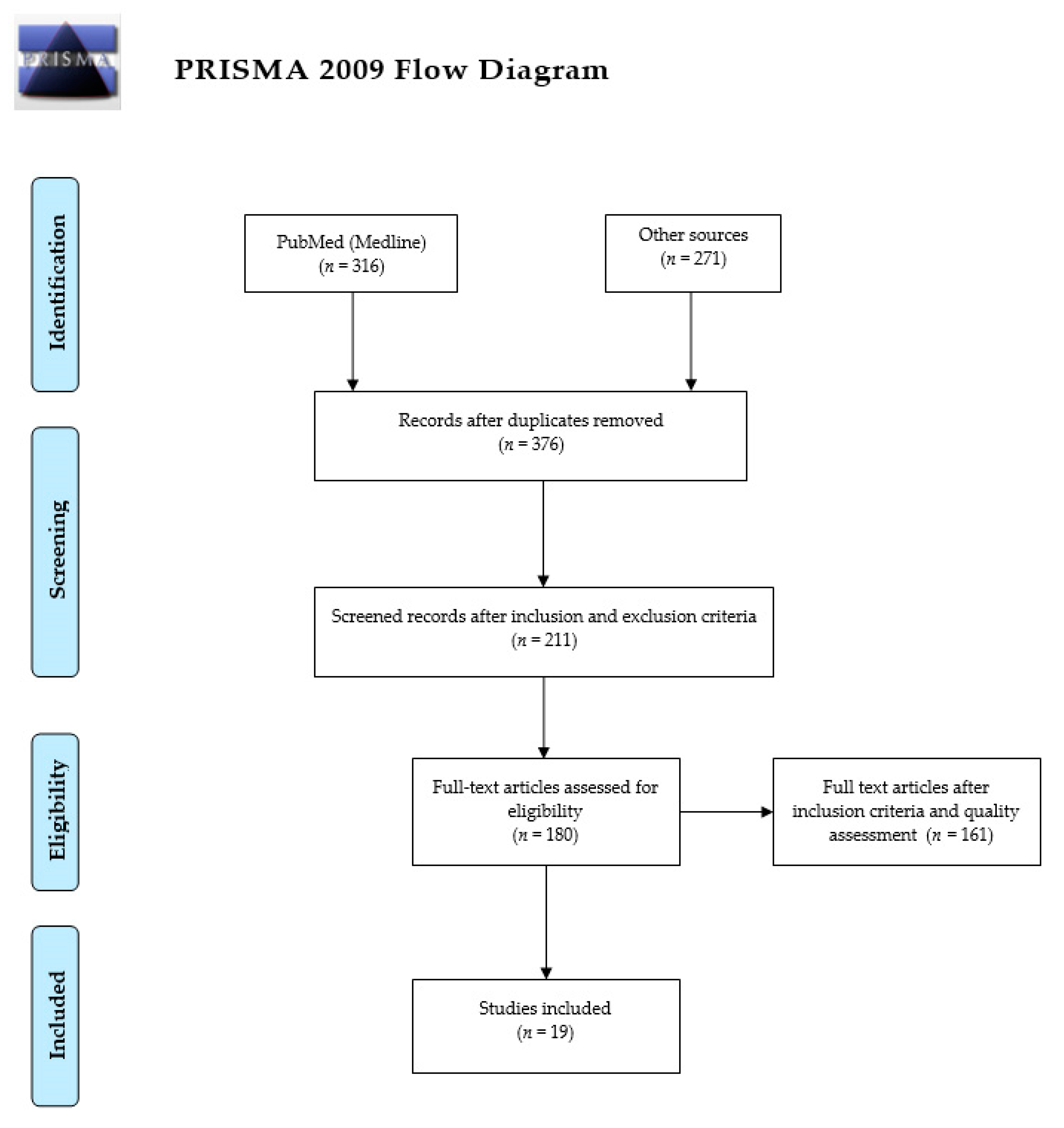
2. Methods
2.1. Data Source and Search Strategies
2.2. Inclusion and Exclusion Criteria
2.3. Quality Criteria
3. Results
3.1. Summary of the Main Findings
3.2. Study Characteristics
3.2.1. Telemedicine in CVD Treatment
Reduced Patient Exposure and Staff
Opportunities for Patient-Provider Information
Internet-Based Physical Activities for Cardiovascular Care and Cardiac Rehabilitation
Reduction in Specialist Shortages and Improvement of CVD Care Efficiency
3.2.2. Telemedicine in CVD Prevention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Currie, G.; Delles, C. Precision medicine and personalized medicine in cardiovascular disease. In Advances in Experimental Medicine and Biology; Springer New York LLC: New York, NY, USA, 2018; Volume 1065, pp. 589–605. [Google Scholar]
- Sagaro, G.G.; Battineni, G.; Amenta, F. Barriers to Sustainable Telemedicine Implementation in Ethiopia: A Systematic Review. Telemed. Rep. 2020, 1, 8–15. [Google Scholar]
- World Health Organization. A Health Telematics Policy in support of WHO´s Health-for-All Strategy for Global Health Development. In Proceedings of the WHO Group Consultation on Health Telematics, Geneva, Switzerland, 1–16 December 1997. [Google Scholar]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. e-Health 2020, 26, 1426–1427. [Google Scholar] [CrossRef]
- Sagaro, G.G.; Battineni, G.; Chintalapudi, N.; Di Canio, M.; Amenta, F. Telemedical assistance at sea in the time of COVID-19 pandemic. Int. Marit. Health 2020, 71, 229–236. [Google Scholar] [CrossRef]
- Brunetti, N.D.; Scalvini, S.; Acquistapace, F.; Parati, G.; Volterrani, M.; Fedele, F.; Molinari, G. Telemedicine for cardiovascular disease continuum: A position paper from the Italian society of cardiology working group on telecardiology and informatics. Int. J. Cardiol. 2015. [Google Scholar] [CrossRef]
- Do, A.W.; Hurst, R.T.; Gulati, M. Maintaining Cardiovascular Health While Practicing Social Distancing: Can Telemedicine Bridge the Gap? Am. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Cardiovascular Diseases (CVDs) Factsheet. Available online: http://www.who.int/mediacentre/factsheets/fs317/en/index.html (accessed on 23 May 2021).
- Sagaro, G.G.; Battineni, G.; Di Canio, M.; Amenta, F. Self-Reported Modifiable Risk Factors of Cardiovascular Disease among Seafarers: A Cross-Sectional Study of Prevalence and Clustering. J. Pers. Med. 2021, 11, 512. [Google Scholar] [CrossRef] [PubMed]
- Molinari, G.; Molinari, M.; Di Biase, M.; Brunetti, N.D. Telecardiology and its settings of application: An update. J. Telemed. Telecare 2018. [Google Scholar] [CrossRef] [PubMed]
- Bliziotis, I.A.; Destounis, A.; Stergiou, G.S. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: A systematic review and meta-analysis. J. Hypertens. 2012. [Google Scholar] [CrossRef]
- Fletcher, B.R.; Hartmann-Boyce, J.; Hinton, L.; Mcmanus, R.J. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: A systematic review and meta-analysis. Am. J. Hypertens. 2015. [Google Scholar] [CrossRef]
- Lo, C.K.L.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 2014. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018. [Google Scholar] [CrossRef]
- Batsis, J.A.; Pletcher, S.N.; Stahl, J.E. Telemedicine and primary care obesity management in rural areas - innovative approach for older adults? BMC Geriatr. 2017, 17, 6. [Google Scholar] [CrossRef] [PubMed]
- Vernooij, W.P.; Kaasjager, H.A.H.; Van Der Graaf, Y.; Wierdsma, J.; Grandjean, H.M.H.; Hovens, M.M.C.; De Wit, G.A.; Visseren, F.L.J. Internet based vascular risk factor management for patients with clinically manifest vascular disease: Randomised controlled trial. BMJ 2012. [Google Scholar] [CrossRef]
- Benson, G.A.; Sidebottom, A.; Sillah, A.; Boucher, J.L.; Miedema, M.D.; Knickelbine, T.; VanWormer, J.J. Reach and effectiveness of the HeartBeat Connections telemedicine pilot program. J. Telemed. Telecare 2018. [Google Scholar] [CrossRef] [PubMed]
- Bosworth, H.B.; Olsen, M.K.; McCant, F.; Stechuchak, K.M.; Danus, S.; Crowley, M.J.; Goldstein, K.M.; Zullig, L.L.; Oddone, E.Z. Telemedicine cardiovascular risk reduction in veterans: The CITIES trial. Am. Heart J. 2018. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Allison, T.G.; Lennon, R.; Lopez-Jimenez, F.; Lerman, L.O.; Lerman, A. Digital health intervention during cardiac rehabilitation: A randomized controlled trial. Am. Heart J. 2017. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, N.D.; Dellegrottaglie, G.; De Gennaro, L.; Di Biase, M. Telemedicine pre-hospital electrocardiogram for acute cardiovascular disease management in detainees: An update. Eur. Res. Telemed. 2015. [Google Scholar] [CrossRef]
- Zullig, L.L.; Oakes, M.M.; McCant, F.; Bosworth, H.B. Lessons learned from two randomized controlled trials: CITIES and STOP-DKD. Contemp. Clin. Trials Commun. 2020. [Google Scholar] [CrossRef]
- Khera, A.; Baum, S.J.; Gluckman, T.J.; Gulati, M.; Martin, S.S.; Michos, E.D.; Navar, A.M.; Taub, P.R.; Toth, P.P.; Virani, S.S.; et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: A scientific statement from the American Society for Preventive Cardiology. Am. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Coorey, G.; Peiris, D.; Neubeck, L.; Redfern, J. A realist evaluation approach to explaining the role of context in the impact of a complex eHealth intervention for improving prevention of cardiovascular disease. BMC Health Serv. Res. 2020. [Google Scholar] [CrossRef]
- Broekhuizen, K.; Van Poppel, M.N.; Koppes, L.L.; Brug, J.; Van Mechelen, W. A tailored lifestyle intervention to reduce the cardiovascular disease risk of individuals with Familial Hypercholesterolemia (FH): Design of the PRO-FIT randomised controlled trial. BMC Public Health 2010. [Google Scholar] [CrossRef]
- Broers, E.R.; Gavidia, G.; Wetzels, M.; Ribas, V.; Ayoola, I.; Piera-Jimenez, J.; Widdershoven, J.W.M.G.; Habibović, M. Usefulness of a Lifestyle Intervention in Patients With Cardiovascular Disease. Am. J. Cardiol. 2020. [Google Scholar] [CrossRef]
- Wienert, J.; Kuhlmann, T.; Storm, V.; Reinwand, D.; Lippke, S. Latent user groups of an eHealth physical activity behaviour change intervention for people interested in reducing their cardiovascular risk. Res. Sport. Med. 2019. [Google Scholar] [CrossRef] [PubMed]
- Joubert, J.; Nkomazana, O.; Mompati, K.; Joubert, L.; Preux, P.M.; La Croix, P.; Laing, J.; Korn, S.; Mbogwe, B.; Tsima, B.; et al. A community survey of cardiovascular risk factors in an urban population in Botswana exploring potential for telemedicine. Eur. Res. Telemed. 2014. [Google Scholar] [CrossRef]
- Agarwal, A.K.; Gaieski, D.F.; Perman, S.M.; Leary, M.; Delfin, G.; Abella, B.S.; Carr, B.G. Telemedicine REsuscitation and Arrest Trial (TREAT): A feasibility study of real-time provider-to-provider telemedicine for the care of critically ill patients. Heliyon 2016. [Google Scholar] [CrossRef] [PubMed]
- Coley, N.; Rosenberg, A.; van Middelaar, T.; Soulier, A.; Barbera, M.; Guillemont, J.; Steensma, J.; Igier, V.; Eskelinen, M.; Soininen, H.; et al. Older Adults’ Reasons for Participating in an eHealth Prevention Trial: A Cross-Country, Mixed-Methods Comparison. J. Am. Med. Dir. Assoc. 2019. [Google Scholar] [CrossRef]
- Van Dyck, W.; Vértes, G.; Palaniappan, M.; Gassull, D.; Jain, P.; Schulthess, D.; Tambuyzer, E.; Hudson, R.; Moran, N. Acute coronary syndrome: What is the cost-effectiveness of prevention, point-of-care technology and telemonitoring? Health Policy Technol. 2012. [Google Scholar] [CrossRef]
- Neubeck, L.; Coorey, G.; Peiris, D.; Mulley, J.; Heeley, E.; Hersch, F.; Redfern, J. Development of an integrated e-health tool for people with, or at high risk of, cardiovascular disease: The Consumer Navigation of Electronic Cardiovascular Tools (CONNECT) web application. Int. J. Med. Inform. 2016. [Google Scholar] [CrossRef]
- Zhou, R.; Cao, Y.; Zhao, R.; Zhou, Q.; Shen, J.; Zhou, Q.; Zhang, H. A novel cloud based auxiliary medical system for hypertension management. Appl. Comput. Informatics 2019. [Google Scholar] [CrossRef]
- Reid, R.D.; Morrin, L.I.; Beaton, L.J.; Papadakis, S.; Kocourek, J.; McDonnell, L.; D’Angelo, M.E.S.; Tulloch, H.; Suskin, N.; Unsworth, K.; et al. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur. J. Prev. Cardiol. 2012. [Google Scholar] [CrossRef]
- Tersalvi, G.; Winterton, D.; Cioffi, G.M.; Ghidini, S.; Roberto, M.; Biasco, L.; Pedrazzini, G.; Dauw, J.; Ameri, P.; Vicenzi, M. Telemedicine in Heart Failure During COVID-19: A Step Into the Future. Front. Cardiovasc. Med. 2020, 7, 612818. [Google Scholar] [CrossRef]
- Battineni, G.; Pallotta, G.; Nittari, G.; Amenta, F. Telemedicine framework to mitigate the impact of the COVID-19 pandemic. J. Taibah Univ. Med. Sci. 2021. [Google Scholar] [CrossRef]
- DeFilippis, E.M.; Reza, N.; Donald, E.; Givertz, M.M.; Lindenfeld, J.A.; Jessup, M. Considerations for Heart Failure Care During the COVID-19 Pandemic. JACC Hear. Fail. 2020, 8, 681–691. [Google Scholar] [CrossRef]
- Battineni, G.; Nittari, G.; Sirignano, A.; Amenta, F. Are telemedicine systems effective healthcare solutions during the COVID-19 pandemic? J. Taibah. Univ. Med. Sci. 2021, 16, 305–306. [Google Scholar]
- Santamore, W.P.; Homko, C.J.; Kashem, A.; McConnell, T.R.; Bove, A.A. Using a telemedicine system to decrease cardiovascular disease risk in an underserved population: Design, use, and interim results. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology, Loyn, France, 23–26 August 2007; Volume 2007, pp. 3701–3704. [Google Scholar]
- Flodgren, G.; Rachas, A.; Farmer, A.J.; Inzitari, M.; Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Abraham, W.T.; Adamson, P.B.; Bourge, R.C.; Aaron, M.F.; Costanzo, M.R.; Stevenson, L.W.; Strickland, W.; Neelagaru, S.; Raval, N.; Krueger, S.; et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: A randomised controlled trial. Lancet 2011, 377, 658–666. [Google Scholar] [CrossRef]
- Heron, N.; Kee, F.; Mant, J.; Cupples, M.E.; Donnelly, M. Rehabilitation of patients after transient ischaemic attack or minor stroke: Pilot feasibility randomised trial of a home-based prevention programme. Br. J. Gen. Pract. 2019, 69, E706–E714. [Google Scholar] [CrossRef] [PubMed]
- Fogliardi, R.; Frumento, E.; Rincón, D.; Viñas, M.Á.; Fregonara, M. Telecardiology: Results and perspectives of an operative experience. J. Telemed. Telecare 2000, 6. [Google Scholar] [CrossRef]
- Kendzerska, T.; Zhu, D.T.; Gershon, A.S.; Edwards, J.D.; Peixoto, C.; Robillard, R.; Kendall, C.E. The effects of the health system response to the COVID-19 pandemic on chronic disease management: A narrative review. Risk Manag. Healthc. Policy 2021, 14, 575–584. [Google Scholar] [CrossRef]
- Chen, C.; Li, X.; Sun, L.; Cao, S.; Kang, Y.; Hong, L.; Liang, Y.; You, G.; Zhang, Q. Post-discharge short message service improves short-term clinical outcome and self-care behaviour in chronic heart failure. ESC Hear. Fail. 2019, 6, 164–173. [Google Scholar] [CrossRef]
- Appel, L.J.; Clark, J.M.; Yeh, H.C.; Wang, N.Y.; Coughlin, J.W.; Daumit, G.; Miller, E.R., 3rd; Dalcin, A.; Jerome, G.J.; Geller, S.; et al. Comparative effectiveness of weight-loss interventions in clinical practice. N. Engl. J. Med. 2011, 365, 1959–1968. [Google Scholar] [CrossRef]
- Christopher, A.M.L.S. Telemonitoring Adherence to Medications in Heart Failure Patients (TEAM-HF): A Pilot Randomized Clinical Trial. Physiol. Behav. 2016, 176, 100–106. [Google Scholar]
- Boyne, J.J.J.; Vrijhoef, H.J.M.; Crijns, H.J.G.M.; De Weerd, G.; Kragten, J.; Gorgels, A.P.M. Tailored telemonitoring in patients with heart failure: Results of a multicentre randomized controlled trial. Eur. J. Heart Fail. 2012, 14, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Koehler, F.; Koehler, K.; Deckwart, O.; Prescher, S.; Wegscheider, K.; Kirwan, B.A.; Winkler, S.; Vettorazzi, E.; Bruch, L.; Oeff, M.; et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): A randomised, controlled, parallel-group, unmasked trial. Lancet 2018, 392, 1047–1057. [Google Scholar] [CrossRef]
- Marino, M.M.; Rienzo, M.; Serra, N.; Marino, N.; Ricciotti, R.; Mazzariello, L.; Leonetti, C.A.; Ceraldi, M.P.; Casamassimi, A.; Capocelli, F.; et al. Mobile Screening Units for the Early Detection of Breast Cancer and Cardiovascular Disease: A Pilot Telemedicine Study in Southern Italy. Telemed. e-Health 2020, 26, 286–293. [Google Scholar] [CrossRef]
- Dendale, P.; De Keulenaer, G.; Troisfontaines, P.; Weytjens, C.; Mullens, W.; Elegeert, I.; Ector, B.; Houbrechts, M.; Willekens, K.; Hansen, D. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: The TEMA-HF 1 (telemonitoring in the management of heart failure) study. Eur. J. Heart Fail. 2012, 14, 333–340. [Google Scholar] [CrossRef] [PubMed]
| Funding Source | Frequency (%) |
|---|---|
| Public bodies | 11 (57.89%) |
| Private bodies | 4 (21.05%) |
| No funding | 4 (21.05%) |
| Telemedicine in Personalized CVD | Frequency (%) |
|---|---|
| Obesity control | 5 (26.31%) |
| Transmission of electrocardiograms | 3 (15.78%) |
| Outpatient management | 4 (21.05%) |
| Control of cardiac arrest | 7 (36.84%) |
| Hypertension control | 6 (31.57%) |
| Cardiac rehabilitation | 4 (21.05%) |
| n | Name of Author (S) and Year | Number of Participants | Type of Study | Advantage | Outcome |
|---|---|---|---|---|---|
| 1 | Walter V.D. et al., 2012 [30] | - | Cost analysis model | Measuring the impact of cost involvement in treatment, the incremental net benefit, and the quality-adjusted life years | 15% decrease in emergency room visits, as well as changes in utilization costs among bypass (−17%), rehabilitation (−13%), catheterization (−59%), medication (−14%), and angioplasty (−59%). |
| 2 | Reid R.D. et al., 2012 [33] | 223 | RCT | Monitoring physical activity for patients with ACS | More effective in monitoring physical activity for patients with ACS than for patients who received usual care |
| 3 | Gallagher B.D. et al., 2017 [46] | 40 | RCT | Medication adherence in a patient with heart failure | Improved medication adherence |
| 4 | Abraham W.T. et al., 2011 [40] | 550 | RCT | Monitoring pulmonary artery hemodynamic data for a patient with heart failure to reduce hospitalization | Significant reduction in hospitalization for patients with heart failure. |
| 5 | Vernooij J.W.P. et al., 2012 [16] | 330 | RCT | Promoting self-management in reducing vascular risk factors | Effective in reducing vascular risk and risk factors for patients with vascular diseases |
| 6 | Chen et al., 2019 [44] | 767 | RCT | Reducing readmission and improving self-care of patients with chronic heart failure (CHF) | Improved self-care behavior and reduced days lost in readmission |
| 7 | Appel L.J. et al., 2011 [45] | 415 | RCT | Weight reduction intervention in obese participants. | Significant weight loss recorded by telemedicine compared to in-person coaching over 24 months. |
| 8 | Boyne J.J. et al., 2012 [47] | 870 | RCT | Monitoring to identify the early symptoms of patients with heart failure to reduce the readmission of rehospitalization | No significant result was found in reducing the rehospitalization |
| 9 | Marino M.M. et al., 2020 [49] | 430 | Cross-sectional | For screening and early detection programs in the prevention of CVD | Effective in screening, early detection, and cost reduction. |
| 10 | Dendale P. et al., 2012 [50] | 160 | RCT | Monitoring and following up patients with heart failure to reduce rehospitalization and mortality rate | Effective in collaboration with doctors to reduce death rate and several days lost due to hospitalization |
| 11 | Koehler F. et al., 2018 [48] | 1571 | RCT | Detecting early signs and symptoms of a patient with heart failure | Effective in detecting early signs and symptoms, as well as reducing days of unplanned readmission and causes of death |
| 12 | Benson G.A. et al., 2018 [17] | 1028 | Retrospective cohort study | For the intervention of main CV risk factors (dyslipidemia and hypertension) | Significant improvement in the prevention of dyslipidemia and hypertension (CV risk factors) among patients at high risk for developing CVD |
| 13 | Widmer R.J. et al., 2017 [19] | 64 | RCT | Cardiac rehabilitation and rehospitalization of patients after PCI for ACS | Significantly reduced CV-related emergency department visits and rehospitalization in patients after ACS |
| 14 | Heron N. et al., 2019 [41] | 40 | RCT | Improving home-based prevention program of patients with a transient ischemic attack | Improved secondary prevention after a transient ischemic attack |
| 15 | Bosworth H.B. et al., 2018 [18] | 429 | RCT | For self-management of patients with CV risk factors | Effective in the intervention of CV risk factors and self-management of patients with CVD |
| 16 | Joubert J. et al., 2014 [27] | 91 | Cross-sectional | Screening CV risk factorsat the community level | Effective in screening CV risk and sending data from a remote area |
| 17 | Brunetti N.D. et al., 2015 [20] | 3213 | Follow-up | Prehospital electrocardiogram screening and remote teleconsultations | Effective in detecting acute CVD via ECG |
| 18 | Wienert J. et al., 2019 [26] | 310 | RCT | For the intervention of health behavior related to CV risk | Effective in promoting a healthy lifestyle to reduce CV risk |
| 19 | Genevieve C. et al., 2020 [23] | 934 | RCT | Involving digital health with the integration of personal data of primary care | The study highlighted that EHR-integrated eHealth interventions have better potential to help the cognitive, affective, and behavioral characteristics of changing health behavior. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Battineni, G.; Sagaro, G.G.; Chintalapudi, N.; Amenta, F. The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. J. Pers. Med. 2021, 11, 658. https://doi.org/10.3390/jpm11070658
Battineni G, Sagaro GG, Chintalapudi N, Amenta F. The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. Journal of Personalized Medicine. 2021; 11(7):658. https://doi.org/10.3390/jpm11070658
Chicago/Turabian StyleBattineni, Gopi, Getu Gamo Sagaro, Nalini Chintalapudi, and Francesco Amenta. 2021. "The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review" Journal of Personalized Medicine 11, no. 7: 658. https://doi.org/10.3390/jpm11070658
APA StyleBattineni, G., Sagaro, G. G., Chintalapudi, N., & Amenta, F. (2021). The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. Journal of Personalized Medicine, 11(7), 658. https://doi.org/10.3390/jpm11070658









