Early Vitamin C, Hydrocortisone, and Thiamine Treatment for Septic Cardiomyopathy: A Propensity Score Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Septic Cardiomyopathy
2.3. Treatment Protocol
2.4. Data Collection and Definitions
2.5. Statistical Analysis
3. Results
3.1. Propensity Score Analysis
3.2. Changes in Clinical Parameters
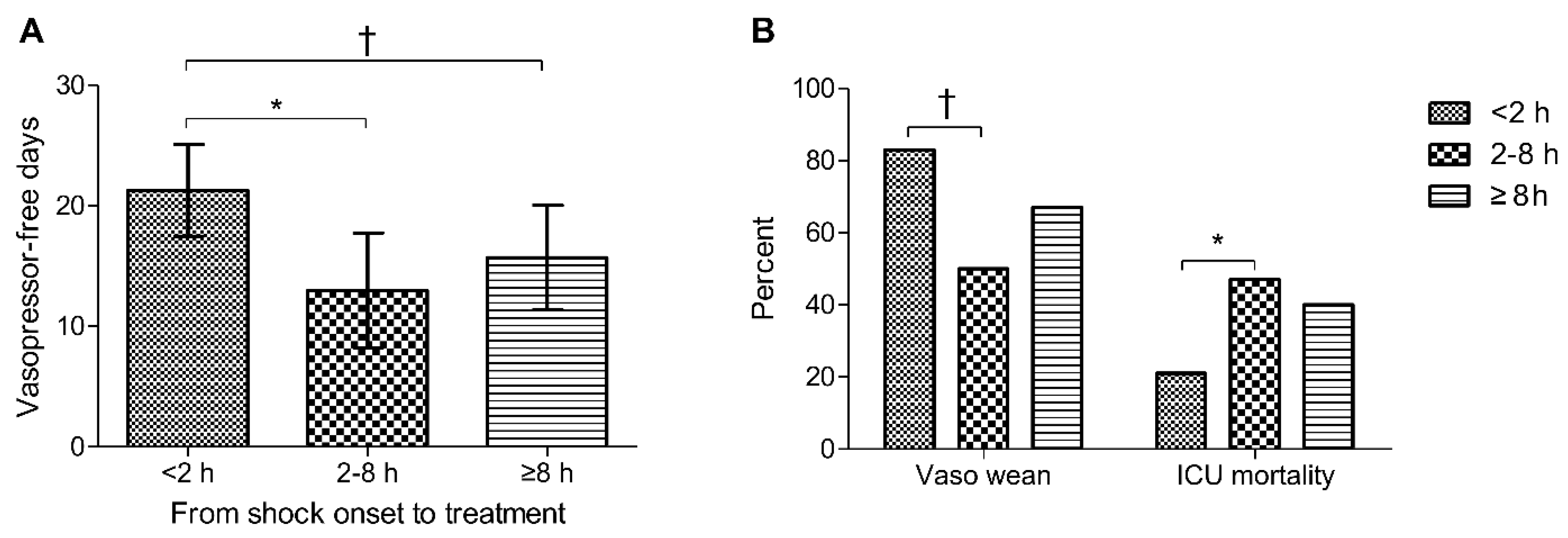
3.3. Vasopressor Weaning and ICU Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Geri, G.; Vignon, P.; Aubry, A.; Fedou, A.L.; Charron, C.; Silva, S.; Repessé, X.; Vieillard-Baron, A. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: A post hoc analysis. Intensive Care Med. 2019, 45, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Suffredini, A.F.; Fromm, R.E.; Parker, M.M.; Brenner, M.; Kovacs, J.A.; Wesley, R.A.; Parrillo, J.E. The cardiovascular response of normal humans to the administration of endotoxin. N. Engl. J. Med. 1989, 321, 280–287. [Google Scholar] [CrossRef]
- Vincent, J.L.; Bakker, J.; Marecaux, G.; Schandene, L.; Kahn, R.J.; Dupont, E. Administration of anti-TNF antibody improves left ventricular function in septic shock patients. Results of a pilot study. Chest 1992, 101, 810–815. [Google Scholar] [CrossRef]
- Rudiger, A.; Singer, M. Mechanisms of sepsis-induced cardiac dysfunction. Crit. Care Med. 2007, 35, 1599–1608. [Google Scholar] [CrossRef]
- Morelli, A.; Ertmer, C.; Westphal, M.; Rehberg, S.; Kampmeier, T.; Ligges, S.; Orecchioni, A.; D’Egidio, A.; D’Ippoliti, F.; Raffone, C.; et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: A randomized clinical trial. JAMA 2013, 310, 1683–1691. [Google Scholar] [CrossRef]
- Ukkonen, H.; Saraste, M.; Akkila, J.; Knuuti, M.J.; Lehikoinen, P.; Nagren, K.; Lehtonen, L.; Voipio-Pulkki, L.M. Myocardial efficiency during calcium sensitization with levosimendan: A noninvasive study with positron emission tomography and echocardiography in healthy volunteers. Clin. Pharmacol. Ther. 1997, 61, 596–607. [Google Scholar] [CrossRef]
- Antcliffe, D.B.; Santhakumaran, S.; Orme, R.M.L.; Ward, J.K.; Al-Beidh, F.; O’Dea, K.; Perkins, G.D.; Singer, M.; McAuley, D.F.; Mason, A.J.; et al. Levosimendan in septic shock in patients with biochemical evidence of cardiac dysfunction: A subgroup analysis of the LeoPARDS randomised trial. Intensive Care Med. 2019, 45, 1392–1400. [Google Scholar] [CrossRef] [PubMed]
- Oudemans-van Straaten, H.M.; Spoelstra-de Man, A.M.; de Waard, M.C. Vitamin C revisited. Crit. Care 2014, 18, 460. [Google Scholar] [CrossRef]
- Carr, A.C.; Shaw, G.M.; Fowler, A.A.; Natarajan, R. Ascorbate-dependent vasopressor synthesis: A rationale for vitamin C administration in severe sepsis and septic shock? Crit. Care 2015, 19, 418. [Google Scholar] [CrossRef]
- Fujii, T.; Deane, A.M.; Nair, P. Metabolic support in sepsis: Corticosteroids and vitamins: The why, the when, the how. Curr. Opin. Crit. Care 2020, 26, 363–368. [Google Scholar] [CrossRef] [PubMed]
- de Andrade, J.A.A.; Gayer, C.R.M.; Nogueira, N.P.A.; Paes, M.C.; Bastos, V.; Neto, J.; Alves, S.C., Jr.; Coelho, R.M.; da Cunha, M.G.A.T.; Gomes, R.N.; et al. The effect of thiamine deficiency on inflammation, oxidative stress and cellular migration in an experimental model of sepsis. J. Inflamm. 2014, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Luethi, N.; Young, P.J.; Frei, D.R.; Eastwood, G.M.; French, C.J.; Deane, A.M.; Shehabi, Y.; Hajjar, L.A.; Oliveira, G.; et al. Effect of Vitamin C, Hydrocortisone, and Thiamine vs Hydrocortisone Alone on Time Alive and Free of Vasopressor Support Among Patients With Septic Shock: The VITAMINS Randomized Clinical Trial. JAMA 2020, 323, 423–431. [Google Scholar] [CrossRef]
- Iglesias, J.; Vassallo, A.V.; Patel, V.V.; Sullivan, J.B.; Cavanaugh, J.; Elbaga, Y. Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis: The ORANGES Trial. Chest 2020, 158, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, A.; Huang, D.T.; Hou, P.C.; Gong, J.; Doshi, P.B.; Grossestreuer, A.V.; Andersen, L.W.; Ngo, L.; Sherwin, R.L.; Berg, K.M.; et al. Effect of Ascorbic Acid, Corticosteroids, and Thiamine on Organ Injury in Septic Shock: The ACTS Randomized Clinical Trial. JAMA 2020, 324, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Sevransky, J.E.; Rothman, R.E.; Hager, D.N.; Bernard, G.R.; Brown, S.M.; Buchman, T.G.; Busse, L.W.; Coopersmith, C.M.; DeWilde, C.; Ely, E.W.; et al. Effect of Vitamin C, Thiamine, and Hydrocortisone on Ventilator- and Vasopressor-Free Days in Patients With Sepsis: The VICTAS Randomized Clinical Trial. JAMA 2021, 325, 742–750. [Google Scholar] [CrossRef]
- Kim, W.Y.; Jung, J.W.; Choi, J.C.; Shin, J.W.; Kim, J.Y. Subphenotypes in Patients with Septic Shock Receiving Vitamin C, Hydrocortisone, and Thiamine: A Retrospective Cohort Analysis. Nutrients 2019, 11, 2976. [Google Scholar] [CrossRef]
- Lin, H.; Wang, W.; Lee, M.; Meng, Q.; Ren, H. Current Status of Septic Cardiomyopathy: Basic Science and Clinical Progress. Front. Pharmacol. 2020, 11, 210. [Google Scholar] [CrossRef]
- Landesberg, G.; Jaffe, A.S.; Gilon, D.; Levin, P.D.; Goodman, S.; Abu-Baih, A.; Beeri, R.; Weissman, C.; Sprung, C.L.; Landesberg, A. Troponin elevation in severe sepsis and septic shock: The role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit. Care Med. 2014, 42, 790–800. [Google Scholar] [CrossRef]
- Charpentier, J.; Luyt, C.E.; Fulla, Y.; Vinsonneau, C.; Cariou, A.; Grabar, S.; Dhainaut, J.F.; Mira, J.P.; Chiche, J.D. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit. Care Med. 2004, 32, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Russell, J.A.; Walley, K.R.; Singer, J.; Gordon, A.C.; Hébert, P.C.; Cooper, D.J.; Holmes, C.L.; Mehta, S.; Granton, J.T.; Storms, M.M.; et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N. Engl. J. Med. 2008, 358, 877–887. [Google Scholar] [CrossRef] [PubMed]
- de Grooth, H.J.; Elbers, P.W.G.; Vincent, J.L. Vitamin C for Sepsis and Acute Respiratory Failure. JAMA 2020, 323, 792. [Google Scholar] [CrossRef]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [PubMed]
- Rosenbaum, P.R.; Dubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Seung, K.B.; Park, D.W.; Kim, Y.H.; Lee, S.W.; Lee, C.W.; Hong, M.K.; Park, S.W.; Yun, S.C.; Gwon, H.C.; Jeong, M.H.; et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N. Engl. J. Med. 2008, 358, 1781–1792. [Google Scholar] [CrossRef] [PubMed]
- Desai, R.J.; Franklin, J.M. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: A primer for practitioners. BMJ 2019, 367, l5657. [Google Scholar] [CrossRef]
- Haileselassie, B.; Su, E.; Pozios, I.; Niño, D.F.; Liu, H.; Lu, D.Y.; Ventoulis, I.; Fulton, W.B.; Sodhi, C.P.; Hackam, D.; et al. Myocardial oxidative stress correlates with left ventricular dysfunction on strain echocardiography in a rodent model of sepsis. Intensive Care Med. Exp. 2017, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Li, W.W.; Du, H.; Zhao, Z.F.; Liu, F.; Lu, J.C.; Yang, X.C.; Cui, W. Role of Vitamin C in Cardioprotection of Ischemia/Reperfusion Injury by Activation of Mitochondrial KATP Channel. Chem. Pharm. Bull. 2016, 64, 548–557. [Google Scholar] [CrossRef]
- Barabutis, N.; Khangoora, V.; Marik, P.E.; Catravas, J.D. Hydrocortisone and Ascorbic Acid Synergistically Prevent and Repair Lipopolysaccharide-Induced Pulmonary Endothelial Barrier Dysfunction. Chest 2017, 152, 954–962. [Google Scholar] [CrossRef]
- Azari, O.; Kheirandish, R.; Azizi, S.; Farajli Abbasi, M.; Ghahramani Gareh Chaman, S.; Bidi, M. Protective Effects of Hydrocortisone, Vitamin C and E Alone or in Combination against Renal Ischemia-Reperfusion Injury in Rat. Iran. J. Pathol. 2015, 10, 272–280. [Google Scholar]
- Gritsenko, D.; Papadopoulos, J.; Altshuler, D.; Lee, Y.I.; Altshuler, J. The Unsung Hero: Role of Thiamine in the ‘Vitamin C Cocktail’. Chest 2017, 152, 678. [Google Scholar] [CrossRef]
- Hemila, H.; Chalker, E. Reanalysis of the Effect of Vitamin C on Mortality in the CITRIS-ALI Trial: Important Findings Dismissed in the Trial Report. Front. Med. 2020, 7, 590853. [Google Scholar] [CrossRef]
- Lachin, J.M. Worst-rank score analysis with informatively missing observations in clinical trials. Control. Clin. Trials 1999, 20, 408–422. [Google Scholar] [CrossRef]
- Fowler, A.A., 3rd; Truwit, J.D.; Hite, R.D.; Morris, P.E.; DeWilde, C.; Priday, A.; Fisher, B.; Thacker, L.R., 2nd; Natarajan, R.; Brophy, D.F.; et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients With Sepsis and Severe Acute Respiratory Failure: The CITRIS-ALI Randomized Clinical Trial. JAMA 2019, 322, 1261–1270. [Google Scholar] [CrossRef]
- Fowler, A.A., 3rd; Fisher, B.J.; Kashiouris, M.G. Vitamin C for Sepsis and Acute Respiratory Failure-Reply. JAMA 2020, 323, 792–793. [Google Scholar] [CrossRef]
- Marik, P.E.; Khangoora, V.; Rivera, R.; Hooper, M.H.; Catravas, J. Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest 2017, 151, 1229–1238. [Google Scholar] [CrossRef]
- Frommelt, M.A.; Kory, P.; Long, M.T. Letter on Update to the Vitamin C, Thiamine, and Steroids in Sepsis (VICTAS) Protocol. Trials 2020, 21, 350. [Google Scholar] [CrossRef]
- Groesdonk, H.H.; Sander, M.; Heringlake, M. Levosimendan in Sepsis. N. Engl. J. Med. 2017, 376, 798. [Google Scholar]
- Hemila, H.; Chalker, E. Vitamin C may reduce the duration of mechanical ventilation in critically ill patients: A meta-regression analysis. J. Intensive Care 2020, 8, 15. [Google Scholar] [CrossRef]
- Kim, W.Y.; Jo, E.J.; Eom, J.S.; Mok, J.; Kim, M.H.; Kim, K.U.; Park, H.K.; Lee, M.K.; Lee, K. Combined vitamin C, hydrocortisone, and thiamine therapy for patients with severe pneumonia who were admitted to the intensive care unit: Propensity score-based analysis of a before-after cohort study. J. Crit. Care 2018, 47, 211–218. [Google Scholar] [CrossRef]
- Zhang, J.; Rao, X.; Li, Y.; Zhu, Y.; Liu, F.; Guo, G.; Luo, G.; Meng, Z.; De Backer, D.; Xiang, H.; et al. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann. Intensive Care 2021, 11, 5. [Google Scholar] [CrossRef]
- Shahreyar, M.; Fahhoum, R.; Akinseye, O.; Bhandari, S.; Dang, G.; Khouzam, R.N. Severe sepsis and cardiac arrhythmias. Ann. Transl. Med. 2018, 6, 6. [Google Scholar] [CrossRef]
- Alhamdi, Y.; Abrams, S.T.; Cheng, Z.; Jing, S.; Su, D.; Liu, Z.; Lane, S.; Welters, I.; Wang, G.; Toh, C.H. Circulating Histones Are Major Mediators of Cardiac Injury in Patients With Sepsis. Crit. Care Med. 2015, 43, 2094–2103. [Google Scholar] [CrossRef]
- Huang, D.T.; Ramirez, P. Biomarkers in the ICU: Less is more? Yes. Intensive Care Med. 2021, 47, 94–96. [Google Scholar] [CrossRef]

| Treatment Group (n = 59) | Control Group (n = 59) | p | |
|---|---|---|---|
| Age, years | 77 (71–83) | 76 (66–82) | 0.51 |
| Male sex | 32 (54) | 26 (44) | 0.27 |
| Body mass index, kg/m2 | 21.3 (19.5–23.4) | 21.0 (18.5–23.5) | 0.63 |
| Comorbidities | |||
| Diabetes | 21 (36) | 26 (44) | 0.35 |
| Chronic heart failure | 6 (10) | 6 (10) | >0.99 |
| Chronic lung disease | 9 (15) | 9 (15) | >0.99 |
| Liver cirrhosis | 6 (10) | 6 (10) | >0.99 |
| Chronic kidney disease | 11 (19) | 13 (22) | 0.65 |
| Malignancy | 12 (20) | 8 (14) | 0.33 |
| Immunosuppression | 12 (20) | 12 (20) | >0.99 |
| Cause of sepsis | |||
| Pneumonia | 26 (44) | 29 (49) | 0.58 |
| Urosepsis | 14 (24) | 17 (29) | 0.53 |
| Gastrointestinal/biliary | 14 (24) | 17 (29) | 0.53 |
| Nosocomial infection | 20 (34) | 18 (31) | 0.69 |
| ARDS | 5 (8) | 6 (10) | 0.75 |
| SOFA score | 12 (10–14) | 12 (9–14) | 0.93 |
| Mechanical ventilation | 40 (68) | 35 (59) | 0.34 |
| Renal replacement therapy | 24 (41) | 23 (39) | 0.85 |
| Vital signs & laboratory data | |||
| Body temperature, °C | 37.2 (36.8–38.1) | 37.3 (36.8–37.9) | 0.72 |
| Mean arterial pressure, mmHg | 61 (54–66) | 60 (53–67) | 0.68 |
| Respiratory rate, breaths/min | 28 (25–33) | 28 (24–34) | 0.60 |
| Bicarbonate, mEq/L | 17.5 (13.8–19.2) | 16.9 (13.1–20.8) | 0.49 |
| Creatinine, mg/dL | 1.6 (1.1–2.2) | 1.7 (1.1–2.3) | 0.78 |
| Platelet count, 1000/mm3 | 132 (79–197) | 117 (61–178) | 0.48 |
| Total bilirubin, mg/dL | 0.8 (0.5–1.8) | 0.7 (0.4–1.2) | 0.17 |
| C-reactive protein, mg/L | 140 (91–274) | 132 (89–248) | 0.84 |
| Lactate, mmol/L | 4.7 (2.5–6.7) | 3.5 (1.9–6.9) | 0.33 |
| Cardiac troponin I, ng/L | 163 (62–722) | 211 (91–737) | 0.29 |
| Brain natriuretic peptide, pg/mL | 458 (242–943) | 318 (144–988) | 0.48 |
| Norepinephrine equivalent dose, μg/min | 14.7 (5.4–24.7) | 10.5 (5.4–21.2) | 0.67 |
| Echocardiography (n = 29/n = 28) 1 | |||
| Ejection fraction, % | 34 (31–42) | 39 (32–45) | 0.67 |
| Arrhythmia | 20 (34) | 12 (20) | 0.10 |
| Treatment Group (n = 29) | Control Group (n = 28) | p | |
|---|---|---|---|
| LV ejection fraction, % | 34 (31–42) | 39 (28–45) | 0.79 |
| Mitral E wave, cm/s | 80.0 (62.0–95.0) | 65.5 (51.5–89.0) | 0.15 |
| Mitral E’ wave, cm/s | 5.0 (4.0–7.0) | 5.0 (4.0–6.2) | 0.54 |
| E/E′ ratio | 16.0 (11.2–17.8) | 12.1 (10.4–17.0) | 0.39 |
| Stroke volume, mL | 24 (22–35) | 27 (24–33) | 0.59 |
| Cardiac output, L/min | 2.8 (2.3–3.1) | 3.0 (2.3–3.7) | 0.24 |
| Cardiac index, L/min/m2 | 1.7 (1.5–1.9) | 2.0 (1.5–2.4) | 0.08 |
| Treatment Group (n = 59) | Control Group (n = 59) | p | |
|---|---|---|---|
| Primary outcome | |||
| ICU mortality | 19 (32) | 27 (46) | 0.13 |
| Secondary outcomes | |||
| Vasopressor weaning | 39 (66) | 36 (61) | 0.57 |
| Vasopressor-free days at day 28 | 16.6 ± 12.1 | 15.0 ± 12.3 | 0.37 |
| Ventilator weaning (n = 40/n = 35) 1 | 21 (53) | 9 (26) | 0.02 |
| Ventilator-free days at day 28 | 11.4 ± 11.3 | 5.4 ± 9.7 | 0.02 |
| Superinfection | 6 (10) | 13 (22) | 0.08 |
| Crude | Propensity-Adjusted | PS-Matched | IPTW-Matched | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted HR (95% CI) | p | Adjusted HR (95% CI) | p | Adjusted HR (95% CI) | p | Adjusted HR (95% CI) | p | |
| ICU mortality | 0.57 (0.35–0.93) | 0.02 | 0.60 (0.34–1.08) | 0.09 | 0.55 (0.30–0.99) | 0.047 | 0.67 (0.45–1.00) | 0.048 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-T.; Jung, S.-Y.; Baek, M.S.; Shin, J.; Kim, W.-Y. Early Vitamin C, Hydrocortisone, and Thiamine Treatment for Septic Cardiomyopathy: A Propensity Score Analysis. J. Pers. Med. 2021, 11, 610. https://doi.org/10.3390/jpm11070610
Lee M-T, Jung S-Y, Baek MS, Shin J, Kim W-Y. Early Vitamin C, Hydrocortisone, and Thiamine Treatment for Septic Cardiomyopathy: A Propensity Score Analysis. Journal of Personalized Medicine. 2021; 11(7):610. https://doi.org/10.3390/jpm11070610
Chicago/Turabian StyleLee, Min-Taek, Sun-Young Jung, Moon Seong Baek, Jungho Shin, and Won-Young Kim. 2021. "Early Vitamin C, Hydrocortisone, and Thiamine Treatment for Septic Cardiomyopathy: A Propensity Score Analysis" Journal of Personalized Medicine 11, no. 7: 610. https://doi.org/10.3390/jpm11070610
APA StyleLee, M.-T., Jung, S.-Y., Baek, M. S., Shin, J., & Kim, W.-Y. (2021). Early Vitamin C, Hydrocortisone, and Thiamine Treatment for Septic Cardiomyopathy: A Propensity Score Analysis. Journal of Personalized Medicine, 11(7), 610. https://doi.org/10.3390/jpm11070610






