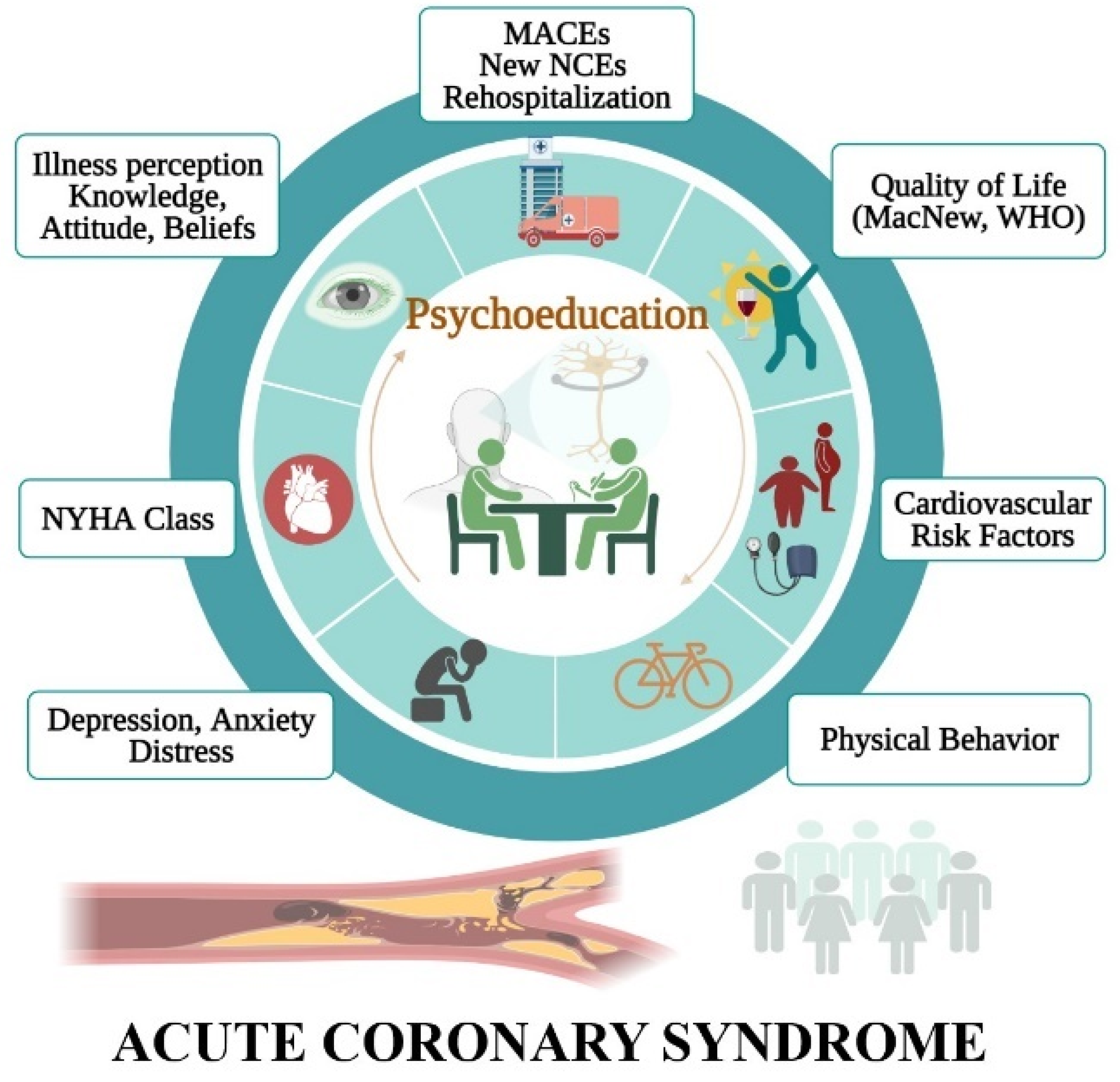
Relationships between Psychoeducational Rehabilitation and Health Outcomes—A Systematic Review Focused on Acute Coronary Syndrome
Abstract
1. Introduction
1.1. Background/Rationale
1.2. Objectives
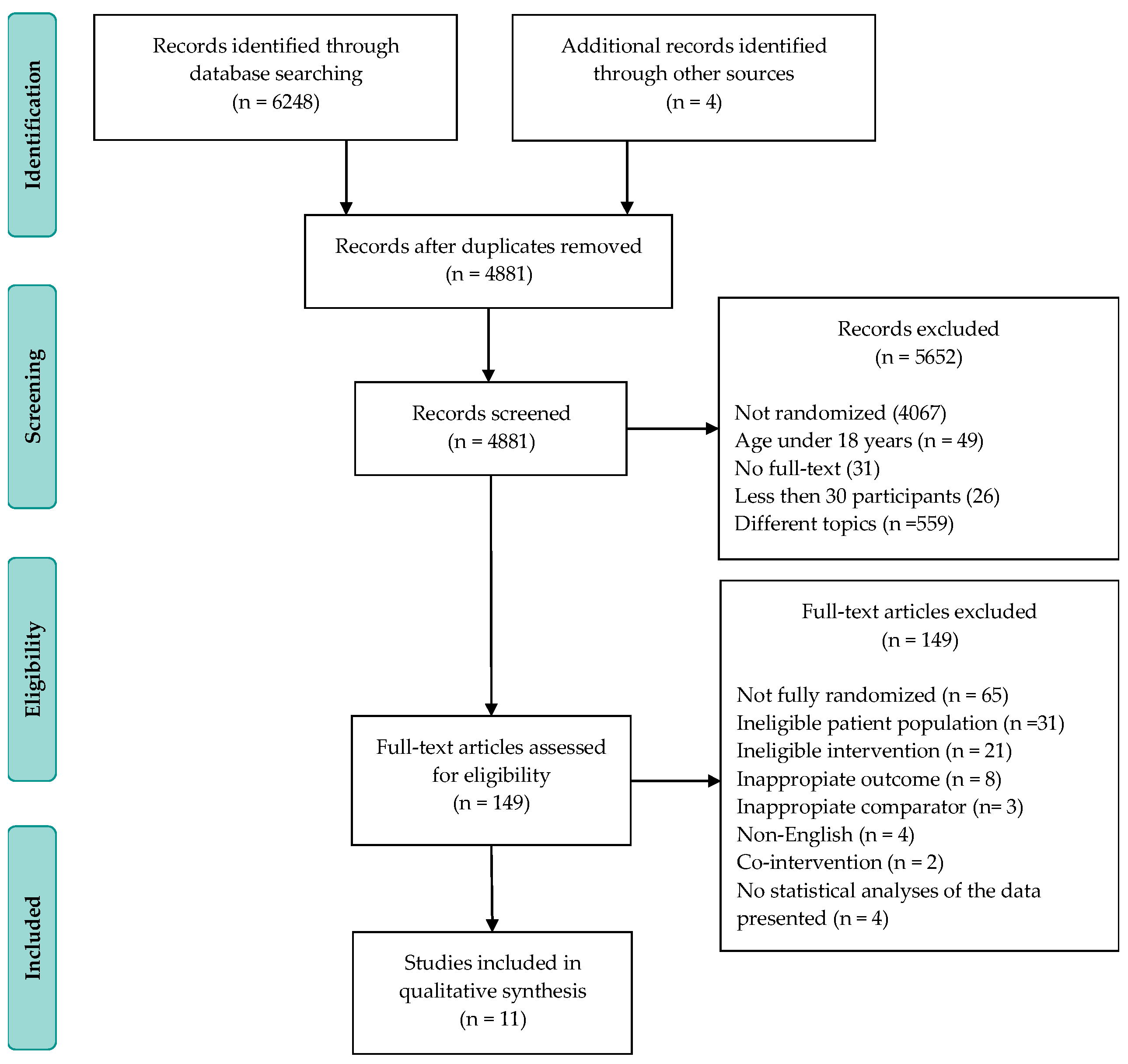
2. Materials and Methods
2.1. Electronic Search Strategy
2.2. Study Selection
- Study type: randomized controlled trials;
- Language: English;
- Types of participants: adults of all ages who have been diagnosed with an acute coronary syndrome;
- Types of interventions: psychotherapy, mental fitness, education during hospitalization for the acute event, interpersonal counseling, short-term psychological intervention, motivational interviewing, and positive psychology. Studies were included if they reported a randomized controlled trial for a psychotherapeutic and educational intervention administered by experienced and trained physicists, psychologists, or nurses for adults of all ages;
- Outcome: all-cause rehospitalization, quality of life evaluation, the control of the cardiovascular risk factors, the exercise capacity, and the adherence to the cardiac rehabilitation program, but also the understanding and the attitude towards the disease, as well as the effects on psychological and medical symptoms;
- Follow-up duration: without restrictions; if a study was reported in several publications, all follow-up results were taken into account.
2.3. Study Appraisal
2.4. Data Extraction
2.5. Bias Assessment and Quality of Evidence
3. Results
3.1. The Impact on Morbidity
3.1.1. Major Adverse Cardiovascular Events
3.1.2. New Non-Cardiovascular Events
3.1.3. Rehospitalization
3.2. Health-Related Quality of Life
3.3. Cardiovascular Risk Factors
3.4. Physical Behavior
3.5. Psychological Variables
3.5.1. Depression and Anxiety
3.5.2. Distress
3.5.3. Positive Affect
3.5.4. Coping Strategies, Self-Esteem, and Health Locus of Control
3.6. Illness Variables
3.6.1. Cardiac Symptomatology
3.6.2. Illness Perception
3.6.3. Knowledge, Attitude, and Beliefs about Illness
4. Discussion
4.1. Summary of Evidence
4.2. Limitations
5. Conclusions and Future Perspectives
Supplementary Materials
Author Contributions
Registration and Protocol
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ibanez, B.; Roque, D.; Price, S. The year in cardiovascular medicine 2020: Acute coronary syndromes and intensive cardiac care. Eur. Heart J. 2021, 42, 884–895. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Crea, F.; Libby, P. Acute Coronary Syndromes. Circulation 2017, 136, 1155–1166. [Google Scholar] [CrossRef]
- Kumar, A.; Cannon, C.P. Acute coronary syndromes: Diagnosis and management, part I. Mayo Clin. Proc. 2009, 84, 917–938. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.R.; Adamson, P.D.; Mills, N.L. Assessment and classification of patients with myocardial injury and infarction in clinical practice. Heart 2017, 103, 10. [Google Scholar] [CrossRef] [PubMed]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.E.; Schmid, J.-P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 2047487320913379. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Corrà, U.; Benzer, W.; Bjarnason-Wehrens, B.; Dendale, P.; Gaita, D.; McGee, H.; Mendes, M.; Niebauer, J.; Zwisler, A.D.; et al. Secondary prevention through cardiac rehabilitation: From knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J. Am. Coll Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Reid, J.; Ski, C.F.; Thompson, D.R. Psychological Interventions for Patients with Coronary Heart Disease and Their Partners: A Systematic Review. PLoS ONE 2013, 8, e73459. [Google Scholar] [CrossRef]
- Nicholson, A.; Kuper, H.; Hemingway, H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur. Heart J. 2006, 27, 2763–2774. [Google Scholar] [CrossRef]
- Roest, A.M.; Martens, E.J.; Denollet, J.; de Jonge, P. Prognostic Association of Anxiety Post Myocardial Infarction with Mortality and New Cardiac Events: A Meta-Analysis. Psychosom. Med. 2010, 72, 563–569. [Google Scholar] [CrossRef]
- Price, K.J.; Gordon, B.A.; Bird, S.R.; Benson, A.C. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? Eur. J. Prev. Cardiol. 2016, 23, 1715–1733. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Sherwood, A.; Smith, P.J.; Watkins, L.; Mabe, S.; Kraus, W.E.; Ingle, K.; Miller, P.; Hinderliter, A. Enhancing Cardiac Rehabilitation with Stress Management Training. Circulation 2016, 133, 1341–1350. [Google Scholar] [CrossRef]
- Kira, G.; Doolan-Noble, F.; Humphreys, G.; Williams, G.; O’Shaughnessy, H.; Devlin, G. A national survey of cardiac rehabilitation services in New Zealand: 2015. N. Z. Med. J. 2016, 129, 50–58. [Google Scholar]
- McPhillips, R.; Salmon, P.; Wells, A.; Fisher, P. Cardiac Rehabilitation Patients’ Accounts of Their Emotional Distress and Psychological Needs: A Qualitative Study. J. Am. Heart Assoc. 2019, 8, e011117. [Google Scholar] [CrossRef]
- Lichtman Judith, H.; Bigger, J.T.; Blumenthal James, A.; Frasure-Smith, N.; Kaufmann Peter, G.; Lespérance, F.; Mark Daniel, B.; Sheps David, S.; Taylor, C.B.; Froelicher Erika, S. Depression and Coronary Heart Disease. Circulation 2008, 118, 1768–1775. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Sorgente, A.; Castelnuovo, G. Integrating Motivational Interviewing with Brief Strategic Therapy for Heart Patients. Procedia Soc. Behav. Sci. 2015, 165, 136–143. [Google Scholar] [CrossRef][Green Version]
- Reid, R.D.; Morrin, L.I.; Higginson, L.A.; Wielgosz, A.; Blanchard, C.; Beaton, L.J.; Nelson, C.; McDonnell, L.; Oldridge, N.; Wells, G.A.; et al. Motivational counselling for physical activity in patients with coronary artery disease not participating in cardiac rehabilitation. Eur. J. Prev. Cardiol. 2012, 19, 161–166. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Corrà, U.; Adamopoulos, S.; Benzer, W.; Bjarnason-Wehrens, B.; Cupples, M.; Dendale, P.; Doherty, P.; Gaita, D.; Höfer, S.; et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2014, 21, 664–681. [Google Scholar] [CrossRef]
- Anderson, L.; Brown, J.P.; Clark, A.M.; Dalal, H.; Rossau, H.K.; Bridges, C.; Taylor, R.S. Patient education in the management of coronary heart disease. Cochrane Database Syst. Rev. 2017, 6, Cd008895. [Google Scholar] [CrossRef] [PubMed]
- Dusseldorp, E.; van Elderen, T.; Maes, S.; Meulman, J.; Kraaij, V. A meta-analysis of psychoeducational programs for coronary heart disease patients. Health Psychol. 1999, 18, 506–519. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; Stossel, C.; Maurice, J. Psychosocial Interventions for Patients with Coronary Artery Disease: A Meta-analysis. Arch. Intern. Med. 1996, 156, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.H.; Anderson, L.; Jenkinson, C.E.; Whalley, B.; Rees, K.; Davies, P. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 2017, 4, CD002902. [Google Scholar] [CrossRef]
- Rees, K.; Bennett, P.; West, R.; Davey, S.G.; Ebrahim, S. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 2004, Cd002902. [Google Scholar] [CrossRef]
- Whalley, B.; Rees, K.; Davies, P.; Bennett, P.; Ebrahim, S.; Liu, Z.; West, R.; Moxham, T.; Thompson, D.R.; Taylor, R.S. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 2011, Cd002902. [Google Scholar] [CrossRef]
- Norlund, F.; Lissåker, C.; Wallert, J.; Held, C.; Olsson, E.M. Factors associated with emotional distress in patients with myocardial infarction: Results from the SWEDEHEART registry. Eur. J. Prev. Cardiol. 2018, 25, 910–920. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Chiavarino, C.; Cavallero, E.; Rabellino, D.; Palumbo, L.; Bianchino, C.; Gaita, F.; Bergerone, S.; Bara, B.G. Mental Fitness for patients with acute coronary syndrome: A randomized clinical trial. Br. J. Health Psychol. 2016, 21, 584–599. [Google Scholar] [CrossRef]
- Davidson, K.W.; Rieckmann, N.; Clemow, L.; Schwartz, J.E.; Shimbo, D.; Medina, V.; Albanese, G.; Kronish, I.; Hegel, M.; Burg, M.M. Enhanced Depression Care for Patients with Acute Coronary Syndrome and Persistent Depressive Symptoms. Arch. Intern. Med. 2010, 170, 600–608. [Google Scholar] [CrossRef]
- Fernandes, A.C.; McIntyre, T.; Coelho, R.; Prata, J.; Maciel, M.J. Brief psychological intervention in phase I of cardiac rehabilitation after acute coronary syndrome. Rev. Port. Cardiol. 2017, 36, 641–649. [Google Scholar] [CrossRef]
- Fernandes, A.C.; McIntyre, T.; Coelho, R.; Prata, J.; Maciel, M.J. Impact of a brief psychological intervention on lifestyle, risk factors and disease knowledge during phase I of cardiac rehabilitation after acute coronary syndrome. Rev. Port. Cardiol. 2019, 38, 361–368. [Google Scholar] [CrossRef]
- Huffman, J.C.; Feig, E.H.; Millstein, R.A.; Freedman, M.; Healy, B.C.; Chung, W.-J.; Amonoo, H.L.; Malloy, L.; Slawsby, E.; Januzzi, J.L.; et al. Usefulness of a Positive Psychology-Motivational Interviewing Intervention to Promote Positive Affect and Physical Activity After an Acute Coronary Syndrome. Am. J. Cardiol. 2019, 123, 1906–1914. [Google Scholar] [CrossRef]
- Nasiri, Z.; Alavi, M.; Ghazavi, Z.; Rabiei, K. The effectiveness of mindfulness-based intervention on perceived stress and perception of disease in patients with acute coronary syndrome. J. Educ. Health Promot. 2020, 9, 130. [Google Scholar] [CrossRef]
- Norlund, F.; Wallin, E.; Olsson, E.M.G.; Wallert, J.; Burell, G.; Von Essen, L.; Held, C. Internet-Based Cognitive Behavioral Therapy for Symptoms of Depression and Anxiety Among Patients with a Recent Myocardial Infarction: The U-CARE Heart Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e88. [Google Scholar] [CrossRef]
- O’Brien, F.; McKee, G.; Mooney, M.; O’Donnell, S.; Moser, D. Improving knowledge, attitudes and beliefs about acute coronary syndrome through an individualized educational intervention: A randomized controlled trial. Patient Educ. Couns. 2014, 96, 179–187. [Google Scholar] [CrossRef]
- O’Neil, A.; Taylor, B.; Hare, D.L.; Sanderson, K.; Cyril, S.; Venugopal, K.; Chan, B.; Atherton, J.J.; Hawkes, A.; Walters, D.L.; et al. Long-term efficacy of a tele-health intervention for acute coronary syndrome patients with depression: 12-month results of the MoodCare randomized controlled trial. Eur. J. Prev. Cardiol. 2015, 22, 1111–1120. [Google Scholar] [CrossRef]
- Oranta, O.; Luutonen, S.; Salokangas, R.K.; Vahlberg, T.; Leino-Kilpi, H. The outcomes of interpersonal counselling on depressive symptoms and distress after myocardial infarction. Nord. J. Psychiatry 2010, 64, 78–86. [Google Scholar] [CrossRef]
- Oranta, O.; Luutonen, S.; Salokangas, R.K.; Vahlberg, T.; Leino-Kilpi, H. The effects of interpersonal counselling on health-related quality of life after myocardial infarction. J. Clin. Nurs. 2011, 20, 3373–3382. [Google Scholar] [CrossRef] [PubMed]
- Oranta, O.; Luutonen, S.; Salokangas, R.K.; Vahlberg, T.; Leino-Kilpi, H. Depression-focused interpersonal counseling and the use of healthcare services after myocardial infarction. Perspect. Psychiatr. Care 2012, 48, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Pristipino, C.; Roncella, A.; Pasceri, V.; Speciale, G. Short-TErm Psychotherapy IN Acute Myocardial Infarction (STEP-IN-AMI) Trial: Final Results. Am. J. Med. 2019, 132, 639–646.e635. [Google Scholar] [CrossRef] [PubMed]
- Roncella, A.; Pristipino, C.; Cianfrocca, C.; Scorza, S.; Pasceri, V.; Pelliccia, F.; Denollet, J.; Pedersen, S.S.; Speciale, G. One-year results of the randomized, controlled, short-term psychotherapy in acute myocardial infarction (STEP-IN-AMI) trial. Int. J. Cardiol. 2013, 170, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Sunamura, M.; Ter Hoeve, N.; van den Berg-Emons, R.J.G.; Geleijnse, M.L.; Haverkamp, M.; Stam, H.J.; Boersma, E.; van Domburg, R.T. Randomised controlled trial of two advanced and extended cardiac rehabilitation programmes. Heart 2018, 104, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Ter Hoeve, N.; Sunamura, M.; Stam, H.J.; Boersma, E.; Geleijnse, M.L.; Van Domburg, R.T.; Van Den Berg-Emons, R.J.G. Effects of two behavioral cardiac rehabilitation interventions on physical activity: A randomized controlled trial. Int. J. Cardiol. 2018, 255, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Kubzansky, L.D.; Huffman, J.C.; Boehm, J.K.; Hernandez, R.; Kim, E.S.; Koga, H.K.; Feig, E.H.; Lloyd-Jones, D.M.; Seligman, M.E.P.; Labarthe, D.R. Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1382–1396. [Google Scholar] [CrossRef]
- Massey, C.N.; Feig, E.H.; Duque-Serrano, L.; Huffman, J.C. Psychological Well-Being and Type 2 Diabetes. Curr. Res. Diabetes Obes. J. 2017, 4, 555641. [Google Scholar] [CrossRef]
- Sreenivasan, J.; Khan, M.S.; Khan, S.U.; Hooda, U.; Aronow, W.S.; Panza, J.A.; Levine, G.N.; Commodore-Mensah, Y.; Blumenthal, R.S.; Michos, E.D. Mental health disorders among patients with acute myocardial infarction in the United States. Am. J. Prev. Cardiol. 2021, 5, 100133. [Google Scholar] [CrossRef]
- Amadio, P.; Zarà, M.; Sandrini, L.; Ieraci, A.; Barbieri, S.S. Depression and Cardiovascular Disease: The Viewpoint of Platelets. Int. J. Mol. Sci. 2020, 21, 7560. [Google Scholar] [CrossRef]
- Byars, S.G.; Inouye, M. Genome-Wide Association Studies and Risk Scores for Coronary Artery Disease: Sex Biases. In Sex-Specific Analysis of Cardiovascular Function; Kerkhof, P.L.M., Miller, V.M., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 627–642. [Google Scholar]
- Haider, A.; Bengs, S.; Luu, J.; Osto, E.; Siller-Matula, J.M.; Muka, T.; Gebhard, C. Sex and gender in cardiovascular medicine: Presentation and outcomes of acute coronary syndrome. Eur. Heart J. 2020, 41, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
| Authors and Year of Publication | Enrollment Place (No. of Centers) and Time | No. of Patients F/M (No.) | Mean Age Years (SD) | Education (Mean, No.) | Timing and Setting |
|---|---|---|---|---|---|
| Chiavarino et al., 2016 [31] | Italy (1) 2-year period | 118 17/101 | 56.5 (8.70) | 10.3 ± 4.0 years | 8 months Hospital |
| Davidson et al., 2010 [32] | USA (5) Between 1 January 2005 and 29 February 2008 | 157 108/49 | 61.2 (10.6) | 13.1 ± 3.8 years | 15 months Hospital |
| Fernandes et al., 2017, 2018 [33,34] | Portugal (1) 6-month period | 121 37/84 | 61.77 (12.11) versus 66.11 (12.61) | <4 years: 25 4 years: 50 4–12 years: 31 >12 years: 15 | 2 months Hospital |
| Huffman et al., 2019 [35] | USA (1) Between May 2017 and April 2018 | 47 11/36 | 60.80 (10.7) | Not specified | 6 months Telephone |
| Nasiri et al., 2020 [36] | Iran (1) Between September 2018 and July 2019 | 64 26/38 | 52.7 (10.94) | Elementary: 12 Cycle degree: 18 Diploma: 14 Associate degree: 2 Bachelor’s degree: 10 | 1 month Hospital |
| Norlund et al., 2018 [37] | Sweden (25) Between September 2013 and December 2016 | 239 80/159 | 58.4 (9.0) versus 60.8 (7.8) | Elementary: 48 High school: 91 University: 100 | 3.5 months Internet-based portal |
| O’Brien et al., 2014 [38] | Dublin (5) Between October 2007 and October 2009 | 1136 316/820 | 62.65 (12.3) | Little formal/primary: 404 Second level: 509 Third level: 222 | 12 months Hospital |
| O’Neil et al., 2015 [39] | Australia (6) Between December 2009 and February 2011 | 121 30/91 | 61.0 (10.2) versus 58.9 (10.7) | High School: 67 Diploma/trade: 23 Bachelor’s/Master’s: 19 | 12 months Hospital Telephone |
| Oranta et al., 2010–1012 [40,41,42] | Finland (1) Between September 2004 and January 2007 | 103 30/73 | < 60 years: 45 60–75 years: 58 | Professional Education: 41 Grade II Education: 39 College-level Education: 18 University Education: 5 Profession Worker: 62 Official: 25 Businessman: 16 | 18 months Hospital Telephone |
| Pristipino et al., 2019 [43] | Italy (1) Between June 2005 and January 2011 | 45 10/35 | 55 (9) versus 55 (8) | Not specified | 5 years Hospital |
| Roncella et al., 2013 [44] | 12 months Hospital | ||||
| Sunamura et al., 2017 [45] | Netherlands (10) Between November 2011 and August 2014 | 615 124/491 | 57.5 (9.2) versus 57.4 (9.3) | Low = 19 Intermediate = 319 High = 139 | 18 months Hospital Outpatient |
| Ter Hoeve et al., 2018 [46] | 324 64/260 | 58.8 (9) versus 59.1 (9) | Low = 16 Intermediate = 198 High = 78 |
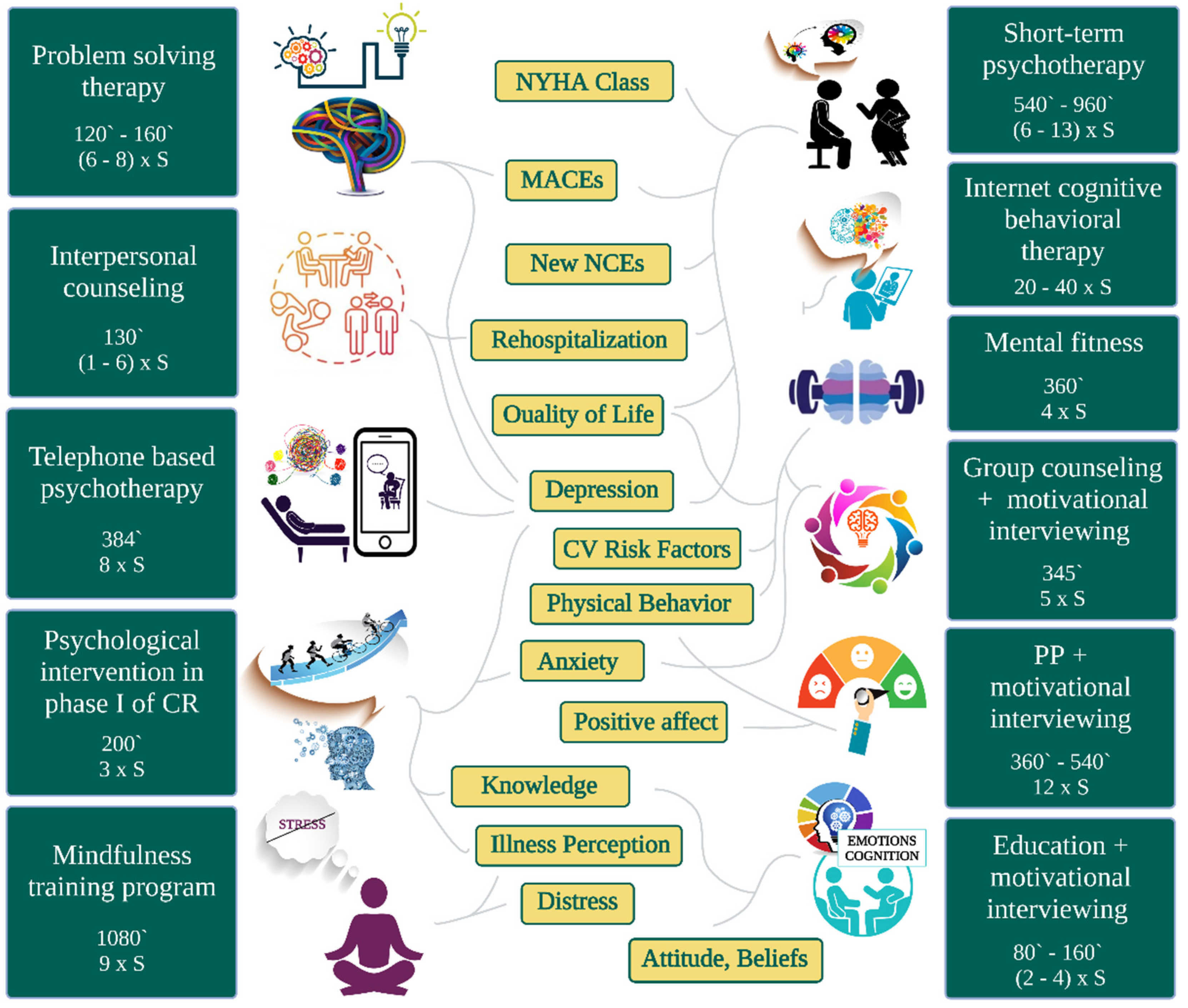
| RCT | Type | Description | Delivered by | Dose | Comparator |
|---|---|---|---|---|---|
| Minutes (No. of Sessions) | |||||
| Chiavarino et al. [31] | Mental fitness | The sessions were conducted in small groups and lasted 90 min. The intervention was focused on emotions and thoughts. The protocol was based on cognitive theory, being designed for patients with ACS and adapted to the individual power of control of perceptions. The program contained cognitive strategies so that patients were trained to understand and confront the event they were experiencing. | Two specifically trained clinical psychologists | 360 (4) | Usual care |
| Davidson et al. [32] | Problem-solving therapy | The meetings were weekly, in person, or on the phone, each visit lasting 30–45 min. The intervention focused on solving the problem. The protocol was based on increasing the patients’ skills. Participants were taught to assess and expose each psychosocial problem. Pleasant regular activities tailored to each patient were encouraged. | Clinical nurse specialist, psychologist, social worker, and/or psychiatrist | 120–160 (6–8) | Usual care |
| Fernandes et al. [33,34] | Brief psychological intervention in phase I of cardiac rehabilitation | The program was made up of three sessions: education on ACS and cardiac rehabilitation, promotion of psychosocial adjustment in post-ACS rehabilitation (cognitive behavioral strategies for reducing stress and anxiety, education for disease awareness and confidence, promoting adaptive coping, self-monitoring, planning, and family involvement in coping after discharge) and follow-up after hospital discharge. | Session 1: psychologist, cardiologist Sessions 2 and 3: psychologist | 200 (3) | Usual care |
| Huffman et al. [35] | Positive psychology exercises combined with motivational interviewing | The sessions were weekly, delivered by phone, with a duration of 30–45 min each, for a period of 12 weeks. The intervention was composed of two components: a positive psychology component (focused on completing activities based on positive psychology and their application in everyday life) and a motivational interviewing component (used for goal setting to specifically promote physical activity). | Study interventionist | 360–540 (12) | Positive psychology exercises alone |
| Nasiri et al. [36] | Mindfulness training program | The meetings were weekly and lasted 2 h each. The intervention focused on the stress perceived after the acute coronary event and on understanding the disease. | NS | 1080 (9) | Usual care |
| Norlund et al. [37] | Internet-based cognitive behavioral therapy | The intervention included 10 modules with different themes adapted to patients with MI: managing worry, fear, and avoidance, behavioral activation, problem solving, communication skills, applied relaxation training, managing negative thoughts, coping with insomnia, values in life, and relapse prevention. Each module consisted of 2–4 treatment steps. Each treatment stage provided psychoeducation in the form of an electronic text (PDF) along with 1–2 homework assignments. Patients also benefited from additional material and videos that exemplified coping strategies. In addition, patients had access to a discussion board where they could communicate with other patients. | Licensed psychologists | NM (20–40) | Treatment as usual |
| O’Brien et al. [38] | Individualized education session delivered using motivational interviewing techniques | The meetings were monthly, each visit lasting 40 min. The first session was delivered within 2–4 days of hospital admission at the bedside or in a room off the ward. The intervention consisted of face-to-face education sessions, tailored to the patient’s needs and impact of the disease on the patient’s cognition and emotions. Through motivational training, patients were encouraged to act promptly and appropriately to seek medical attention if required. | NS | 80–160 (2–4) | Usual care |
| O’Neil et al. [39] | Telephone-based psychotherapy | The sessions took place over the phone for 6 months, with an average duration of 48.4 min per session. Intervention sessions were delivered most intensively over the first 3 months. The goal of the program was depression management and cardiovascular risk reduction. The components of the psychological intervention were: motivational interviewing, goal setting, behavioral activation, and cognitive restructuring. | Master’s level qualified psychologists | 384 (8) | Usual medical care |
| Oranta et al. [40,41,42] | Interpersonal counseling | The content of the intervention was modified for MI patients to take from 1 to 6 sessions (mean 4.6, SD 1.24, mode 5), consisting of:
| Psychiatric nurse trained for one day in the practice of interpersonal counseling | 130 (1–6) | Standard care after MI |
| Pristipino et al. [43] Roncella et al. [44] | Short-term psychotherapy | Individual psychotherapy: 3 to 10 sessions of 1 h with each including personal history elaboration, body language insights, relaxation techniques, and dream analysis. Group psychotherapy: 5 sessions, 2 h each including the same items of individual sessions plus couple analysis, medical/psychological education, and music therapy. | Single psychotherapist | 540–960 (6–13) | Usual care |
| Sunamura et al., 2017 [45] Ter Hoeve et al., 2018 [46] | Group counseling sessions delivered using motivational interviewing technique | The intervention was structured in 3 group counseling sessions, face to face, regarding the physical activity performed. Each session lasted 75 min. In addition, patients participated in 2 more face-to-face group sessions at 3 and 9 months. Each of these sessions consisted of behavioral counseling on heart-healthy lifestyle lasting 1 h per session. | Physiotherapist trained in motivational interviewing | 345 (5) | Standard cardiac rehabilitation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cojocariu, S.A.; Maștaleru, A.; Sascău, R.A.; Stătescu, C.; Mitu, F.; Cojocaru, E.; Trandafir, L.M.; Leon-Constantin, M.-M. Relationships between Psychoeducational Rehabilitation and Health Outcomes—A Systematic Review Focused on Acute Coronary Syndrome. J. Pers. Med. 2021, 11, 440. https://doi.org/10.3390/jpm11060440
Cojocariu SA, Maștaleru A, Sascău RA, Stătescu C, Mitu F, Cojocaru E, Trandafir LM, Leon-Constantin M-M. Relationships between Psychoeducational Rehabilitation and Health Outcomes—A Systematic Review Focused on Acute Coronary Syndrome. Journal of Personalized Medicine. 2021; 11(6):440. https://doi.org/10.3390/jpm11060440
Chicago/Turabian StyleCojocariu, Sabina Alexandra, Alexandra Maștaleru, Radu Andy Sascău, Cristian Stătescu, Florin Mitu, Elena Cojocaru, Laura Mihaela Trandafir, and Maria-Magdalena Leon-Constantin. 2021. "Relationships between Psychoeducational Rehabilitation and Health Outcomes—A Systematic Review Focused on Acute Coronary Syndrome" Journal of Personalized Medicine 11, no. 6: 440. https://doi.org/10.3390/jpm11060440
APA StyleCojocariu, S. A., Maștaleru, A., Sascău, R. A., Stătescu, C., Mitu, F., Cojocaru, E., Trandafir, L. M., & Leon-Constantin, M.-M. (2021). Relationships between Psychoeducational Rehabilitation and Health Outcomes—A Systematic Review Focused on Acute Coronary Syndrome. Journal of Personalized Medicine, 11(6), 440. https://doi.org/10.3390/jpm11060440









