Maintenance of Maternal Breastfeeding up to 6 Months: Predictive Models
Abstract
1. Introduction
2. Materials and Methods
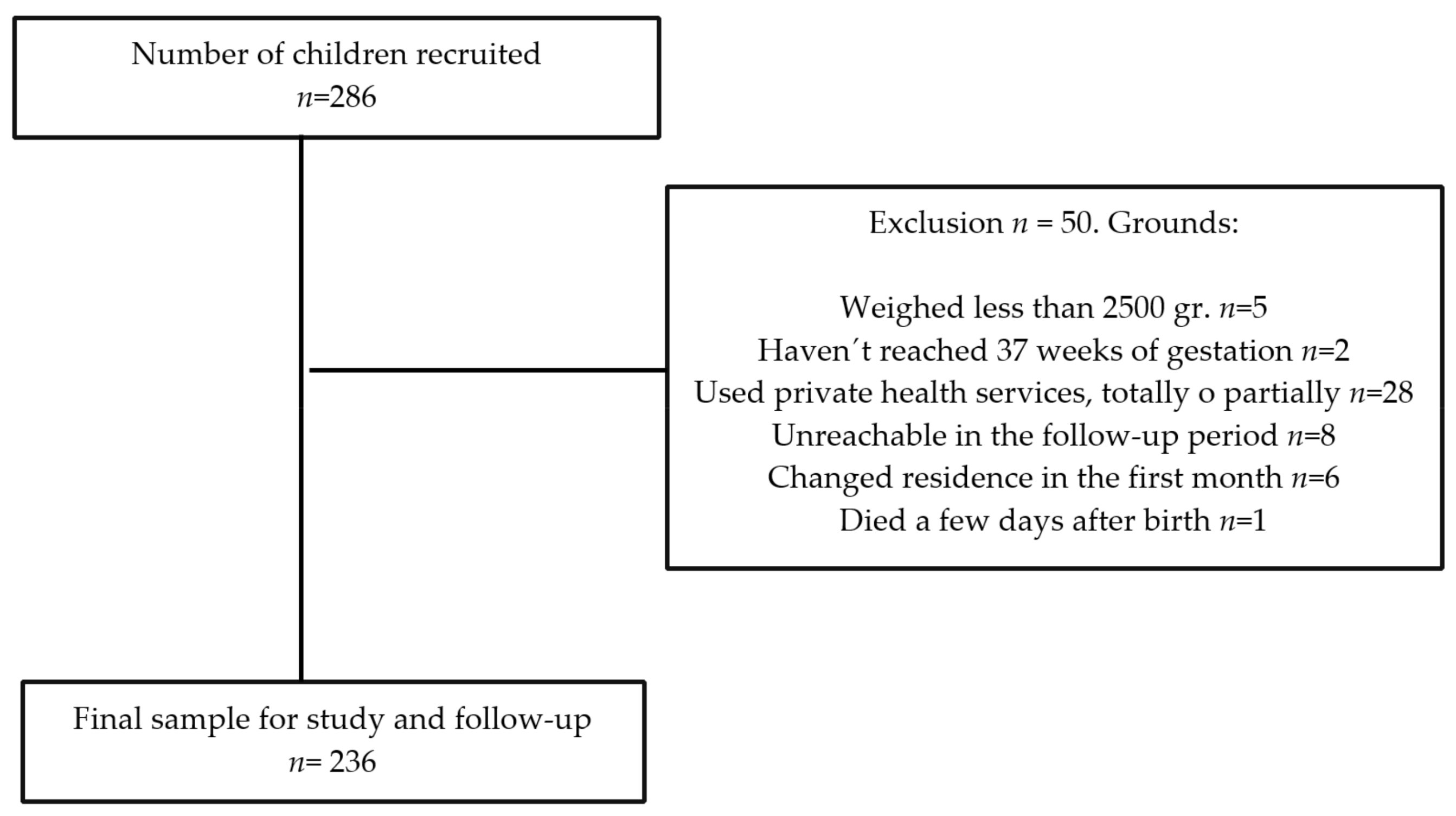
2.1. Study Setting and Sample
2.2. Study Variables
- (a)
- Cessation of EBF due to the introduction of solid foods, i.e., “by the recommendation of a health professional” or “the mother’s decision”;
- (b)
- Cessation of EBF due to the introduction of the bottle, i.e., “by recommendation of a health professional”, “influenced by the social or family environment”, “the child is not gaining weight according to the standard criteria for age”, “work reasons”, “the child is still hungry”, and” problems with breastfeeding”.
2.3. Measuring Procedures and Instruments
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
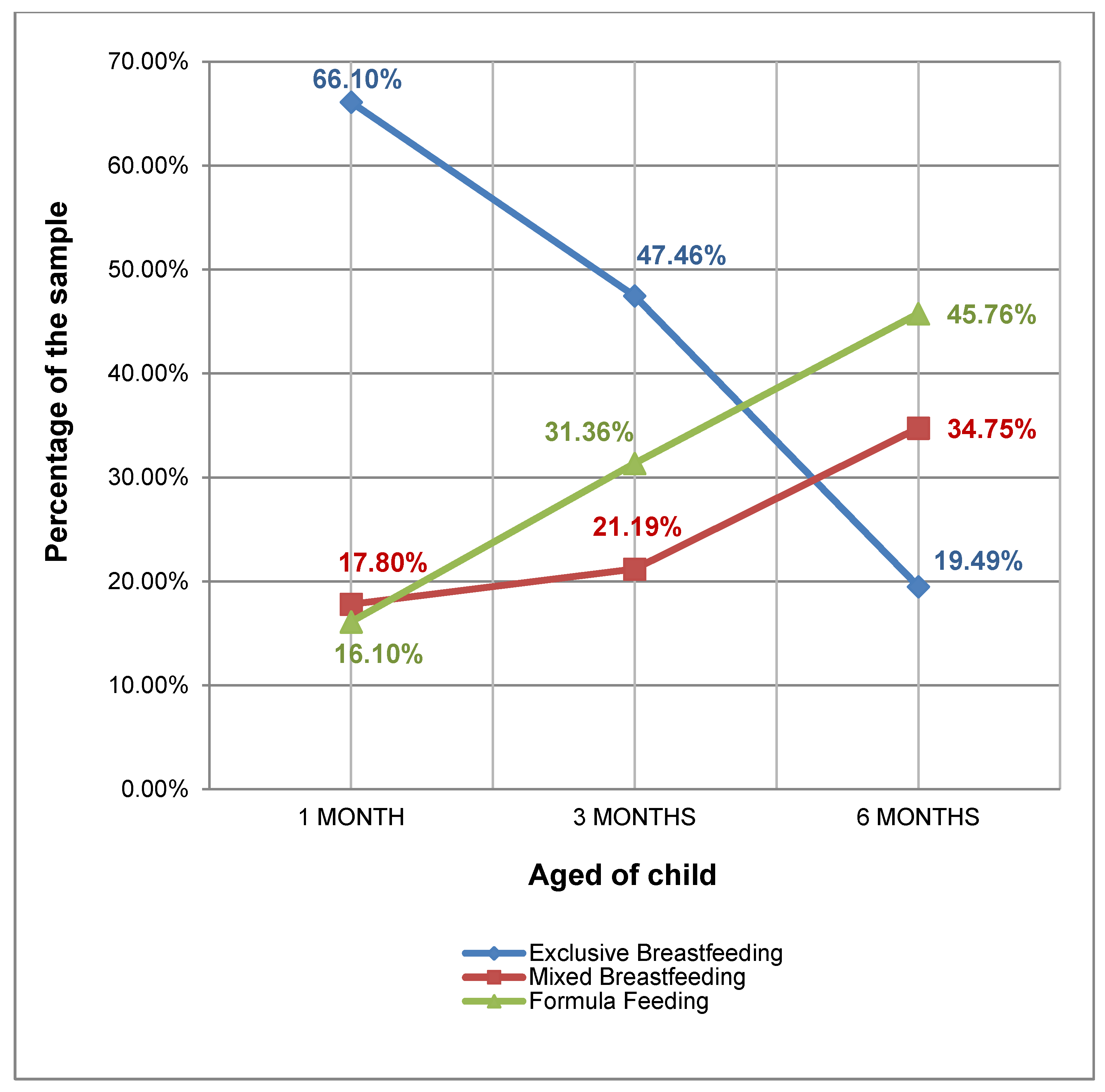
3.1. Maintenance of EBF
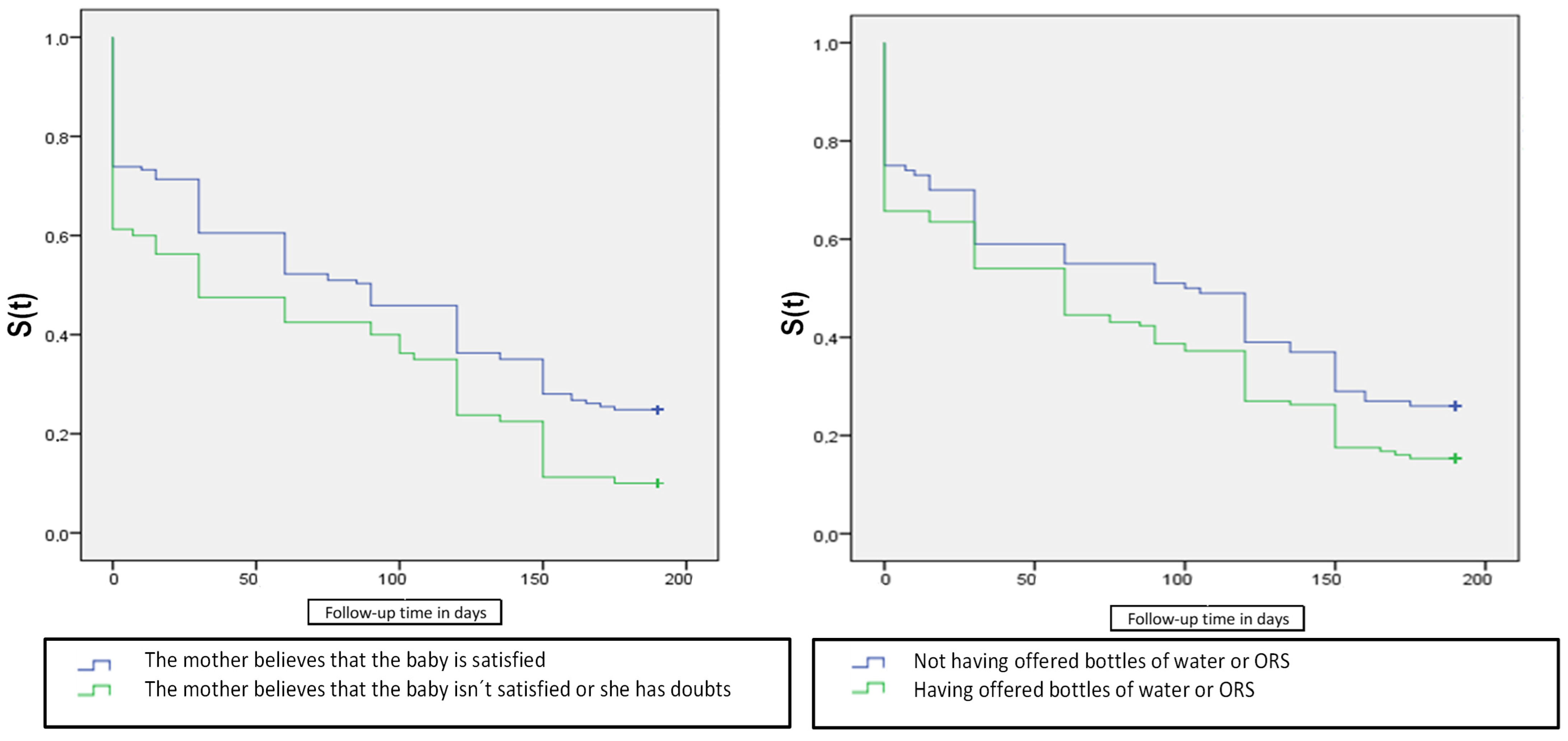
3.2. Early Cessation of EBF
4. Discussion
4.1. Prevalence of the Different Types of Breastfeeding Practiced in Our Setting
4.2. Epidemiological Factors
4.3. Relationship between the Reasons for Cessation and Duration of Exclusive Breastfeeding
4.4. Implications for Clinical Practice
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Part 2: Measurement; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Morales, E.; García-Esteban, R.; Guxens, M.; Guerra, S.; Mendez, M.; Moltó-Puigmartí, C.; Lopez-Sabater, M.C.; Sunyer, J. Effects of prolonged breastfeeding and colostrum fatty acids on allergic manifestations and infections in infancy. Clin. Exp. Allergy 2012, 42, 918–928. [Google Scholar] [CrossRef]
- Robinson, S.; Fall, C. Infant nutrition and later health: A review of current evidence. Nutrients 2012, 4, 859–874. [Google Scholar] [CrossRef]
- Brahm, P.; Valdes, V. Benefits of breastfeeding and risks associated with not breastfeeding. Rev. Chil. Pediatr. 2017, 88, 15–21. [Google Scholar]
- Gartner, L.M.; Morton, J.; Lawrence, R.A.; Naylor, A.J.; O’Hare, D.; Schanler, R.J.; Eidelman, A.I.; American Academy of Pediatrics Section on Breastfeedingl. Breastfeeding and the use of human milk. Pediatrics 2005, 115, 496–506. [Google Scholar]
- Holme, A.; MacArthur, C.; Lancashire, R. The effects of breastfeeding on cognitive and neurological development of children at 9 years. Child. Care Health Dev. 2010, 36, 583–590. [Google Scholar] [CrossRef]
- WHO; OPS/WHO Guatemala. First Series 2016 on Breastfeeding. Spanish Edition, Guatemala. Lancet 2016, 387, 475–504. [Google Scholar]
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; Franca, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Lancet Breastfeeding Series Group. Breastfeeding in the 21st Century: Epidemiology, mechanisms and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Bartick, M.; Reinhold, A. The burden of suboptimal breast feeding in the United States: A pediatric cost analysis. Pediatrics 2010, 125, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Santacruz-Salas, E.; Aranda-Reneo, I.; Hidalgo-Vega, Á.; Blanco-Rodriguez, J.M.; Segura-Fragoso, A. The Economic Influence of Breastfeeding on the Health Cost of Newborns. J. Hum. Lact. 2018. [Google Scholar] [CrossRef] [PubMed]
- WHO. Comprehensive Implementacion Plan. on Maternal Infant and Young Child. Nutritional; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- WHO; Unicef. Implementing the Global Strategy for Infant and Young Child. Feeding: Geneva, 3–5 February 2003: Meeting Report; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- OMS. World Health Organization. Global Nutrition Targets 2025: Breastfeeding Policy Brief. No. WHO/NMH/NHD/14.7. World Health Organization. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/149022/WHO_NMH_NHD_14.7_eng.pdf (accessed on 20 April 2021).
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L.M.; Victora, C.G. Lancet Breastfeeding Series Group. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387, 491–504. [Google Scholar] [CrossRef]
- Santacruz-Salas, E.; Aranda-Reneo, I.; Segura-Fragoso, A.; Cobo-Cuenca, A.I.; Laredo-Aguilera, J.A.; Carmona-Torres, J.M. Mothers’ Expectations and Factors Influencing Exclusive Breastfeeding during the First 6 Months. Int J. Environ. Res. Public Health 2019, 17, 77. [Google Scholar] [CrossRef]
- Villar, M.; Santa-Marina, L.; Murcia, M.; Amiano, P.; Gimeno, S.; Ballester, F.; Julvez, J.; Romaguera, D.; Fernández-Somoano, A.; Tardón, A.; et al. Social Factors Associated with Non-initiation and Cessation of Predominant Breastfeeding in a Mother–Child Cohort in Spain. Matern. Child. Health J. 2018, 22, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Lechosa-Muñiz, C.; Paz-Zulueta, M.; Sota, S.M.; de Adana Herrero, M.S.; del Rio, E.C.; Llorca, J.; Cabero-Perez, M.J. Factors associated with duration of breastfeeding in Spain: A cohort study. Int. Breastfeed. J. 2020, 15, 79. [Google Scholar] [CrossRef]
- Ruiz Poyato Pablo y Juan Miguel Martínez Galiano. Causas del abandono de la lactancia materna exclusiva en una zona básica urbana. Ene 2014, 8. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2014000200004&lng=es (accessed on 21 April 2021).
- Ballesta-Castillejos, A.; Gomez-Salgado, J.; Rodriguez-Almagro, J.; Ortiz-Esquinas, I.; Hernandez-Martinez, A. Relationship between maternal body mass index with the onset of breastfeeding and its associated problems: An online survey. Int. Breastfeed. J. 2020, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Ballesta-Castillejos, A.; Gómez-Salgado, J.; Rodríguez-Almagro, J.; Ortiz-Esquinas, I.; Hernández-Martínez, A. Factors that influence mothers’ prenatal decision to breastfeed in Spain. Int. Breastfeed. J. 2020, 15, 97. [Google Scholar] [CrossRef]
- Santacruz-Salas, E.; Segura-Fragoso, A.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M.; Pozuelo-Carrascosa, D.P.; Laredo-Aguilera, J.A. Factors Associated with the Abandonment of Exclusive Breastfeeding before Three Months. Children 2020, 7, 298. [Google Scholar] [CrossRef]
- Camargo Figuera, F.; Latorre Latorre, J.F.; Porras Carreño, J.A. Factores asociados al abandono de la lactancia materna exclusiva. Rev. Hacia Promoción Salud. 2011, 16, 56–72. [Google Scholar]
- Oribe, M.; Lertxundi, A.; Basterrechea, M.; Begiristain, H.; Santa Marina, L.; Villar, M.; Dorronsoro, M.; Amiano, P.; Ibarluzea, J. Prevalence of factors associated with the duration of exclusive breastfeeding during the first 6 months of life in the INMA birth cohort in Gipuzkoa. Gac Sanit. 2015, 29, 4–9. [Google Scholar] [CrossRef]
- Santo, L.C.D.E.; De Oliveira, L.D.; Giugliani, E.R.J. Factors associated with low incidence of exclusive breastfeeding for the first 6 months. Birth 2007, 34, 212–219. [Google Scholar] [CrossRef]
- AEP. Lactancia Materna en Cifras: Tasas de Inicio y Duración de la Lactancia en España y en Otros Países: Asociación Española de Pediatría. 2016. Available online: https://www.aeped.es/sites/default/files/documentos/201602-lactancia-materna-cifras.pdf (accessed on 8 May 2021).
- INE. Tipo de Lactancia Por Clase Social Basada en la Ocupación de la Persona de Referencia y Duración. 2011–2012 [Internet]. 2013. Available online: http://www.ine.es/jaxi/tabla.do?path=/t00/mujeres_hombres/tablas_1/l0/&file=d06003px&type=pcaxis&L=0 (accessed on 8 May 2021).
- WHO. 10 Facts About Breastfeeding Internet 2017 35. Available online: https://www.who.int/features/factfiles/breastfeeding/es/ (accessed on 20 April 2021).
- ENSE. Encuesta Nacional de Salud España 2017 [Internet]. Ministerio de Sanidad, Consumo y Bienestar Social 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_pres_wEBF.pdf (accessed on 20 April 2021).
- Alía, P.H.; Armenteros, P.C.; Pino Pino, N. Prevalencia y factores asociados de la lactancia materna exclusiva al alta en el Hospital Virgen de la Salud de Toledo. Matronas Hoy 2020, 8, 28–35. [Google Scholar]
- Alvarez Caballero, M.; Orozco Hechavarría, N.; Moreno Alvarez, A.; Marín Álvarez, T.; Tur Vaillant, I. Factores que influyeron en el abandono precoz de la lactancia materna en lactantes de un Grupo Básico de Trabajo. Rev. Médica Electrónica 2017, 39, 884–893. [Google Scholar]
- Balogun, O.O.; Dagvadorj, A.; Anigo, K.M.; Ota, E.; Sasaki, S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: A quantitative and qualitative systematic review. Matern. Child Nutr. 2015, 11, 433–451. [Google Scholar] [CrossRef]
- Chandrashekhar, T.S.; Joshi, H.S.; Binu, V.; Shankar, P.R.; Rana, M.S.; Ramachandran, U. Breast-feeding initiation and determinants of exclusive breast-feeding-a questionnaire survey in an urban population of western Nepal. Public Health Nutr. 2007, 10, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Yngve, A.; Sjöström, M. Breastfeeding determinants and a suggested framework for action in Europe. Public Health Nutr. 2001, 4, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Pinto, E.; Chaves, C.; Duarte, J.; Nelas, P.; Coutinho, E. Maternal Affection and Motivation for Breastfeeding. Procedia Soc. Behav. Sci. 2016, 217, 1028–1035. [Google Scholar] [CrossRef]
- Díaz-Gómez, N.M.; Ruzafa-Martínez, M.; Ares, S.; Espiga, I.; De Alba, C. Motivaciones y Barreras Perci-Bidas Por Las Mujeres Españolas en Relación a la Lactancia Materna. Revista Española de Salud Pública 2016, 90. Available online: https://scielo.isciii.es/scielo.php?pid=S1135-57272016000100416&script=sci_arttext&tlng=pt (accessed on 2 May 2021).
- Walker, M. Breastfeeding Management for the Clinician: Using the Evidence; Jones & Bartlett Publishers: Burlington, MA, USA, 2013. [Google Scholar]
- Roig, A.O.; Martínez, M.R.; García, J.C.; Hoyos, S.P.; Navidad, G.L.; Alvarez, J.C.F.; Pujalte, M.D.M.C.; González, R.G.D.L. Factors associated to breastfeeding cessation before 6 months. Rev. Lat. Am. Enferm. 2010, 18, 373–380. [Google Scholar] [CrossRef][Green Version]
- Erkkola, M.; Salmenhaara, M.; Kronberg-Kippilä, C.; Ahonen, S.; Arkkola, T.; Uusitalo, L.; Pietinen, P.; Veijola, R.; Knip, M.; Virtanen, S.M. Determinants of breast-feeding in a Finnish birth cohort. Public Health Nutr. 2010, 13, 504–513. [Google Scholar] [CrossRef]
- Cervera-Gasch, Á.; Mena-Tudela, D.; Leon-Larios, F.; Felip-Galvan, N.; Rochdi-Lahniche, S.; Andreu-Pejó, L.; González-Chordá, V.M. Female Employees’ Perception of Breastfeeding Support in the Workplace, Public Universities in Spain: A Multicentric Comparative Study. Int. J. Environ. Res. Public Health 2020, 17, 6402. [Google Scholar] [CrossRef] [PubMed]
- Renfrew, M.J.; McCormick, F.M.; Wade, A.; Quinn, B.; Dowswell, T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Wong, M.S.; Huanyu, M.; Wai, T.C. Effectiveness of educational and supportive intervention for primiparous women on breastfeeding related outcomes and breastfeeding self-efficacy: A systematic review and meta-analysis. Int. J. Nurs. Studies 2021, 103874. Available online: https://www.sciencedirect.com/science/article/pii/S0020748921000067?casa_token=FMJfaaYyIEoAAAAA:7Hle8fn214NHmemmTrCnGFbrbasNVtsn3fFZ2IqKCJWUglqCh51CI669A858vS4GfuopB8F_ (accessed on 18 April 2021). [CrossRef]
- Philipp, B.L.; Merewood, A.; Miller, L.W.; Chawla, N.; Murphy-Smith, M.M.; Gomes, J.S.; Cimo, S.; Cook, J.T. Baby-friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting. Pediatrics 2001, 108, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Navas, L. Causes of the Abandonment of Breastfeeding in Spain (2005–2015) Bibliographic Review. [Final degree project on the Internet]. [Nursing Faculty of Soria] University of Valladolid. 2019. Available online: http://uvadoc.uva.es/handle/10324/39125 (accessed on 24 April 2021).
- Vila-Candel, R.; Soriano-Vidal, F.J.; Murillo-Llorente, M.; Pérez-Bermejo, M.; Castro-Sánchez, E. Mantenimiento de la lactancia materna exclusiva a los 3 meses posparto: Experiencia en un departamento de salud de la Comunidad Valenciana. Atención Primaria 2019, 51, 91–98. [Google Scholar] [CrossRef]
| Variables | Not Exclusive Breastfeeding for 6 Months | Exclusive Breastfeeding for 6 Months | * p |
|---|---|---|---|
| n (%) | n (%) | ||
| Social and Individual Maternal, Infant O Mother–Child Factors | |||
| AGE OF THE MOTHER | |||
| Up to 30 years | 57 (30.16) | 13 (27.7) | 0.73 |
| >than 30 years | 132 (69.8) | 34 (72.3) | |
| NATIONALITY | |||
| Spanish | 155 (82.01) | 42 (89.4) | 0.23 |
| Foreign | 34 (17.99) | 5 (10.6) | |
| EDUCATION LEVEL | |||
| Primary school | 51 (26.98) | 14 (29.8) | 0.68 |
| Secondary school or higher | 138 (73.02) | 33 (70.2) | |
| LIVE WITH YOUR PARTNER | |||
| Yes | 183 (96.83) | 47 (100) | 0.18 |
| No | 6 (3.17) | 0 (0) | |
| MARITAL STATUS | |||
| Married or with partner | 114 (60.32) | 33 (70.2) | 0.19 |
| Other situations | 75 (39.68) | 14 (29.8) | |
| WORK SITUATION | |||
| Employed | 97 (51.32) | 18 (38.3) | 0.10 |
| Unemployed | 92 (48.68) | 29 (61.7) | |
| MATERNITY LEAVE | |||
| without maternity leave | 84 (44.44) | 26 (55.3) | 0.17 |
| on maternity leave | 105 (55.55) | 21 (44.7) | |
| SEX OF NEWBORN | |||
| Boy | 105 (55.55) | 21 (44.7) | 0.17 |
| Girl | 84 (44.44) | 26 (55.3) | |
| CLINICAL FEATURES | |||
| PREVIOUS NUMBER OF CHILDREN | |||
| Neither | 83 (44.15) | 23 (48.9) | 0.20 |
| Only one | 80 (42.33) | 22 (46.8) | |
| Two or more | 26 (13.76) | 2 (4.3) | |
| DAYS OF GESTATION | |||
| <280 | 101 (53.44) | 23 (48.9) | 0.55 |
| ≥280 | 88 (46.56) | 24 (51.1) | |
| ANESTHESIA | |||
| without anesthesia | 28 (14.81) | 5 (10.6) | 0.41 |
| with anesthesia | 161 (85.2) | 42 (89.4) | |
| BIRTH WEIGHT (kg) | |||
| ≤3.250 | 91 (48.1) | 21 (44.7) | 0.64 |
| >3.250 | 98 (51.9) | 26 (55.3) | |
| TYPE OF DELIVERY | |||
| Vaginal with or whitout instrumental | 145 (76.7) | 36 (76.6) | 0.97 |
| Cesarean section | 44 (23.3) | 11 (23.4) | |
| HAVE DECIDED ON THE TYPE OF LACTATION PRIOR TO DELIVERY | |||
| Yes, breastfeeding | 173 (91.5) | 47 (100) | 0.03 |
| They haven’t decided yet | 17 (8.9) | 0 (0.00) | |
| DECISION OF THE DURATION TO CONTINUE THE BREASTFEEDING | |||
| One month | 2 (1.1) | 0 (0) | 0.23 |
| Two months | 0 | 0 (0) | |
| Three months | 2 (1.1) | 0 (0) | |
| Between 3 and 6 month | 69 (36.5) | 11 (23.4) | |
| As long as the baby wants it | 18 (9.5) | 7 (14.9) | |
| As long as I can | 86 (45.5) | 29 (61.7) | |
| CHARACTERISTICS OF THE CLINICAL OR FAMILY ENVIRONMENT | |||
| BELIEVE THAT THE BABY IS HUNGRY | |||
| The baby is satisfied | 118 (62.4) | 39 (83) | 0.00 |
| The baby isn’t satisfied or I have doubts | 71 (37.6) | 8 (17) | |
| THEY OFFERED BOTTLES OF WATER OR ORS IN THE HOSPITAL | |||
| Yes | 73 (38.6) | 26 (55.3) | 0.04 |
| Not | 116 (61.4) | 21 (44.7) | |
| THEY OFFERED FORMULA FEEDING | |||
| Not | 53 (28.1) | 20 (42.6) | 0.06 |
| Yes | 136 (71.9) | 27 (57.4) | |
| INITIAL PRACTICE PROBLEMS WITH BREASTFEEDING | |||
| Not | 155 (82.1) | 36 (76.6) | 0.38 |
| Yes | 34 (17.9) | 11 (23.4) | |
| THEY SOLVED THE BREASTFEEDING PROBLEMS | |||
| Not | 81 (42.9) | 23 (48.9) | 0.47 |
| Yes | 108 (57.1) | 24 (51.1) | |
| BREASTFEEDING COUNSELLING | |||
| Not recivied or not necesary | 75 (39.7) | 13 (27.7) | 0.18 |
| Search itself | 25 (13.2) | 5 (10.6) | |
| Health profesional or support group | 89 (47.01) | 29 (61.7) | |
| COUPLE OPINION REGARDING BREASTFEEDING | |||
| Not in favor | 3 (1.6) | 0 (0) | 0.08 |
| In favor | 171 (90.5) | 47 (100) | |
| Indifferent | 15 (7.93) | 0 (0) | |
| Relationship beteween Use of Pacifier and Time Achieved of EBF | ||||
|---|---|---|---|---|
| Variables | n (%) | Time of EBF (Days) | SD | χ2 |
| USE OF THE PACIFIER | ||||
| Not use pacifier | 68 (28.8) | 118.9 | 69.14 | <0.001 |
| Start using in the first 29 days | 67 (28.4) | 57.19 | 67.42 | |
| Start using from the first 30 days | 101 (42.8) | 73.37 | 74.28 | |
| RELATIONSHIP BETEWEEN AVERAGE NUMBER OF DAYS OF PREGNANCY AND TIME ACHIEVED OF EBF | ||||
| VARIABLES | n (%) | Time of pregnancy (days) | SD | t |
| EBF 3 MONTHS | ||||
| NOT | 124 (52.5) | 275.23 | 8.6 | 0.001 |
| YES | 112 (47.45) | 277.93 | 7.6 | |
| EBF 6 MONTHS | ||||
| NOT | 190 (88.5) | 275.99 | 8.47 | 0.05 |
| YES | 46 (19.49) | 278.64 | 6.79 | |
| RELATIONSHIP BETEWEEN PRIOR EXPERIENCE IN EBF AND MAINTENANCE OF EBF 6 MONTHS | ||||
| VARIABLES | n (%) | Maintenance of EBF 6 months (OR) | CI 95% | p* |
| TIME OF EBF TO OTHERS PREVIOUS CHILDRENS | ||||
| No time | 4 (7.14) | Ref. | ||
| Until 6 months | 7 (13.73) | 2.205 | (0.59–8.22) | 0.239 |
| Over 6 months | 14 (40) | 8.902 | (2.60–30.4) | 0.00 |
| Influential Variables | OR | IC 95% | * p |
|---|---|---|---|
| BELIEVE THE BABY IS NOT SATISFIED OR HAVING DOUBTS | 2.96 | (0.149–768) | 0.01 |
| HAVING OFFERED BOTTLES OF WATER OR ORS | 0.52 | (1.000–3.707) | 0.05 |
| Reasons Aluded by the Mothers | n (%) | Average Days of EBF | SD | |
|---|---|---|---|---|
| Reasons for introducing artificial milk bottles | Health recommendation | 7 (2.9) | 115.7 | 41.3 |
| Influence of social or family environment | 11 (4.6) | 107.8 | 51.5 | |
| The baby does not weight gain according to standards | 4 (1.6) | 97.5 | 58.1 | |
| Labour problems | 24 (10.1) | 96.0 | 40.2 | |
| The baby gets hungry | 21 (8.9) | 76.7 | 51.9 | |
| Problems with breastfeeding | 27 (11.4) | 60.8 | 49.8 | |
| Reasons for introducing solid foods | Health recommendation | 84 (35.6) | 100.4 | 55.1 |
| She decides for herself | 7 (2.9) | 105.7 | 60.2 | |
| Reasons for Introducing Artificial Milk Bottles | n (%) | Average Days of EBF | SD | * p |
|---|---|---|---|---|
| Influence of social or family environment | 162 (68.6) | 88.9 | 81.3 | 0.05 |
| Labour problems | 26 (11) | 88.65 | 46.53 | |
| Health recommendation | 11 (4.7) | 73.64 | 66.56 | |
| Autoeficacy = The baby gets hungry + not sufficient weight gain according to standards | 38 (16.1) | 52.63 | 56.98 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santacruz-Salas, E.; Segura-Fragoso, A.; Pozuelo-Carrascosa, D.P.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M.; Laredo-Aguilera, J.A. Maintenance of Maternal Breastfeeding up to 6 Months: Predictive Models. J. Pers. Med. 2021, 11, 396. https://doi.org/10.3390/jpm11050396
Santacruz-Salas E, Segura-Fragoso A, Pozuelo-Carrascosa DP, Cobo-Cuenca AI, Carmona-Torres JM, Laredo-Aguilera JA. Maintenance of Maternal Breastfeeding up to 6 Months: Predictive Models. Journal of Personalized Medicine. 2021; 11(5):396. https://doi.org/10.3390/jpm11050396
Chicago/Turabian StyleSantacruz-Salas, Esmeralda, Antonio Segura-Fragoso, Diana P. Pozuelo-Carrascosa, Ana Isabel Cobo-Cuenca, Juan Manuel Carmona-Torres, and José Alberto Laredo-Aguilera. 2021. "Maintenance of Maternal Breastfeeding up to 6 Months: Predictive Models" Journal of Personalized Medicine 11, no. 5: 396. https://doi.org/10.3390/jpm11050396
APA StyleSantacruz-Salas, E., Segura-Fragoso, A., Pozuelo-Carrascosa, D. P., Cobo-Cuenca, A. I., Carmona-Torres, J. M., & Laredo-Aguilera, J. A. (2021). Maintenance of Maternal Breastfeeding up to 6 Months: Predictive Models. Journal of Personalized Medicine, 11(5), 396. https://doi.org/10.3390/jpm11050396











