Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females
Abstract
:1. Introduction
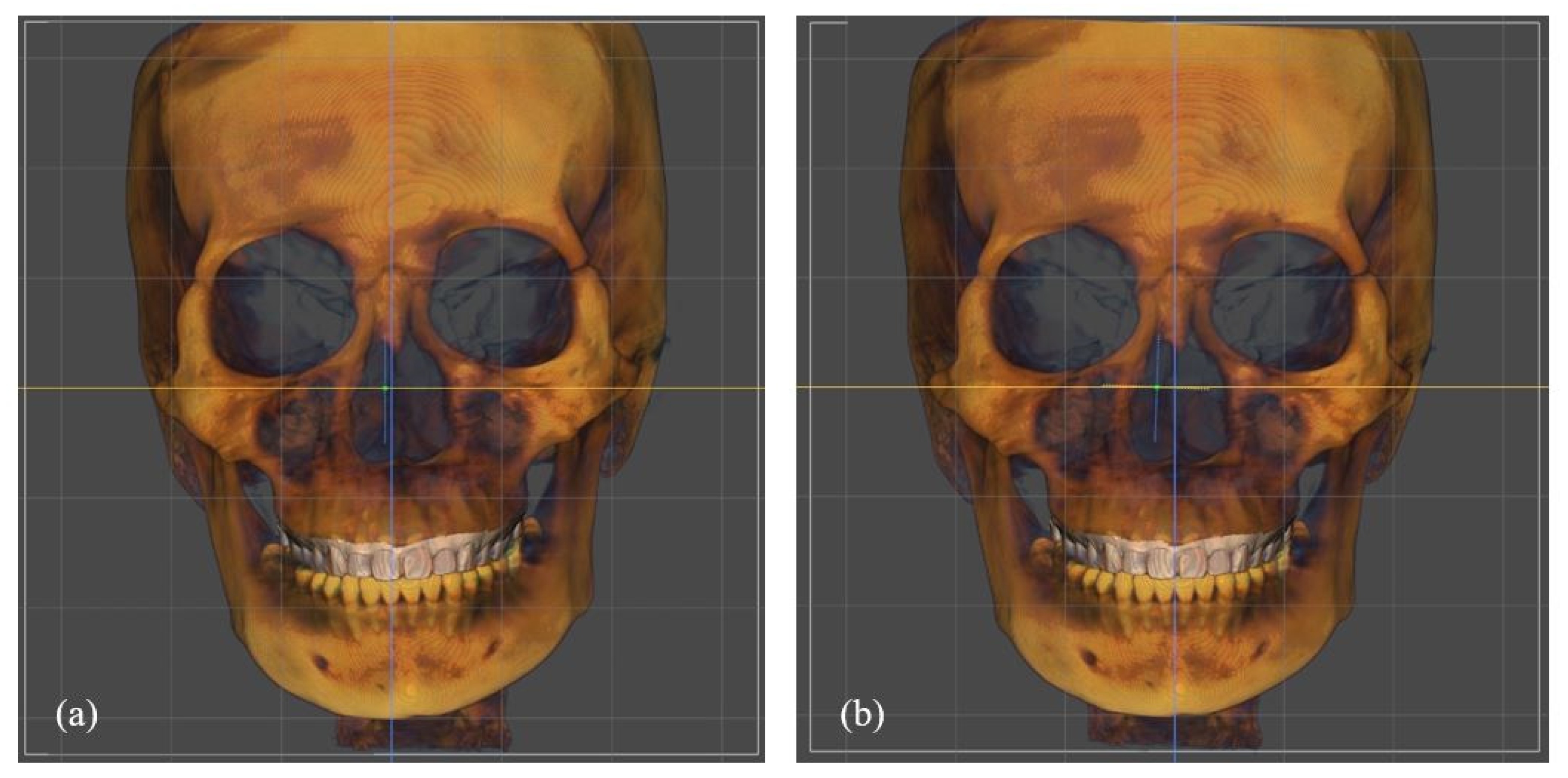
2. Materials and Methods
2.1. Sample
2.2. Profile Analysis
2.3. Statistical Analysis
2.4. Error Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Downs, W.B. Variations in facial relationships; their significance in treatment and prognosis. Am. J. Orthod. 1948, 34, 812–840. [Google Scholar] [CrossRef]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Steiner, C.C. Cephalometrics in clinical practice. Angle Orthod. 1959, 29, 8–29. [Google Scholar]
- Tweed, C.H. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am. J. Orthod. Oral Surg. 1946, 32, 175–230. [Google Scholar] [CrossRef]
- Sassouni, V. Diagnosis and treatment planning via roentgenographic cephalometry. Am. J. Orthod. 1958, 44, 433–463. [Google Scholar] [CrossRef]
- Ricketts, R.M. Perspectives in the clinical application of cephalometrics. The first fifty years. Angle Orthod. 1981, 51, 115–150. [Google Scholar]
- Da Silveira, H.L.; Silveira, H.E. Reproducibility of cephalometric measurements made by three radiology clinics. Angle Orthod. 2006, 76, 394–399. [Google Scholar]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 1. Landmark identification. Am. J. Orthod. 1971, 60, 111–127. [Google Scholar] [CrossRef]
- Richardson, A. An investigation into the reproducibility of some points, planes, and lines used in cephalometric analysis. Am. J. Orthod. 1966, 52, 637–651. [Google Scholar] [CrossRef]
- Dibbets, J.M.; Nolte, K. Effect of magnification on lateral cephalometric studies. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 196–201. [Google Scholar] [CrossRef]
- Cox, N.H.; Van der Linden, F.P. Facial harmony. Am. J. Orthod. 1971, 60, 175–183. [Google Scholar] [CrossRef]
- Arnett, G.W.; Jelic, J.S.; Kim, J.; Cummings, D.R.; Beress, A.; Worley, C.M., Jr.; Chung, B.; Bergman, R. Soft tissue cephalometric analysis: Diagnosis and treatment planning of dentofacial deformity. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 239–253. [Google Scholar] [CrossRef]
- Jacobson, A.; Jacobson, R.L. Radiographic cephalometry from basics to 3-d imaging. In Radiographic Cephalometry, 2nd ed.; Quintessence Publishing Co, Inc.: Chicago, IL, USA, 2006; p. 246. [Google Scholar]
- Boas, F.E.; Fleischmann, D. CT artifacts: Causes and reduction techniques. Imaging Med. 2012, 4, 229–240. [Google Scholar] [CrossRef] [Green Version]
- Gateno, J.; Xia, J.J.; Teichgraeber, J.F. New 3-dimensional cephalometric analysis for orthognathic surgery. J. Oral Maxillofac. Surg. 2011, 69, 606–622. [Google Scholar] [CrossRef] [Green Version]
- Harrell, W.E., Jr.; Hatcher, D.C.; Bolt, R.L. In search of anatomic truth: 3-dimensional digital modeling and the future of orthodontics. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 325–330. [Google Scholar] [CrossRef]
- Popat, H.; Richmond, S.; Drage, N.A. New developments in: Three-dimensional planning for orthognathic surgery. J. Orthod. 2010, 37, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Kolokitha, O.E.; Topouzelis, N. Cephalometric methods of prediction in orthognathic surgery. J. Maxillofac. Oral Surg. 2011, 10, 236–245. [Google Scholar] [CrossRef] [Green Version]
- Bruynseels, K.; Santoni de Sio, F.; van den Hoven, J. Digital Twins in Health Care: Ethical Implications of an Emerging Engineering Paradigm. Front. Genet. 2018, 9, 31. [Google Scholar] [CrossRef]
- Gribel, B.F.; Gribel, M.N.; Frazao, D.C.; McNamara, J.A., Jr.; Manzi, F.R. Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod. 2011, 81, 26–35. [Google Scholar] [CrossRef]
- Van Vlijmen, O.J.; Maal, T.; Berge, S.J.; Bronkhorst, E.M.; Katsaros, C.; Kuijpers-Jagtman, A.M. A comparison between 2D and 3D cephalometry on CBCT scans of human skulls. Int. J. Oral Maxillofac. Surg. 2010, 39, 156–160. [Google Scholar] [CrossRef]
- Andrews, L.F.; Andrews, W.A. Syllabus of the Andrews Orthodontic Philosophy, 9th ed.; Lawrence, F., Ed.; Andrews: San Diego, CA, USA, 2001; pp. 19–21. [Google Scholar]
- Resnick, C.M.; Kim, S.; Yorlets, R.R.; Calabrese, C.E.; Peacock, Z.S.; Kaban, L.B. Evaluation of Andrews’ Analysis as a Predictor of Ideal Sagittal Maxillary Positioning in Orthognathic Surgery. J. Oral Maxillofac. Surg. 2018, 76, 2169–2176. [Google Scholar] [CrossRef] [Green Version]
- Andrews, W.A. AP relationship of the maxillary central incisors to the forehead in adult white females. Angle Orthod. 2008, 78, 662–669. [Google Scholar] [CrossRef] [Green Version]
- Gidaly, M.P.; Tremont, T.; Lin, C.P.; Kau, C.H.; Souccar, N.M. Optimal antero-posterior position of the maxillary central incisors and its relationship to the forehead in adult African American females. Angle Orthod. 2019, 89, 123–128. [Google Scholar] [CrossRef] [Green Version]
- Schlosser, J.B.; Preston, C.B.; Lampasso, J. The effects of computer-aided anteroposterior maxillary incisor movement on ratings of facial attractiveness. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J. Lip posture and its significance in treatment planning. Am. J. Orthod. 1967, 53, 262–284. [Google Scholar] [CrossRef]
- Spradley, F.L.; Jacobs, J.D.; Crowe, D.P. Assessment of the anteroposterior soft-tissue contour of the lower facial third in the ideal young adult. Am. J. Orthod. 1981, 79, 316–325. [Google Scholar] [CrossRef]
- Steiner, C.C. The use of cephalometrics as an aid to planning and assessing orthodontic treatment: Report of a case. Am. J. Orthod. 1960, 46, 721–735. [Google Scholar] [CrossRef]
- McNamara, J.A., Jr. A method of cephalometric evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef]
- Tulloch, C.; Phillips, C.; Dann, C. Cephalometric measures as indicators of facial attractiveness. Int. J. Adult Orthod. Orthognath. Surg. 1993, 8, 171. [Google Scholar]
- Oh, H.S.; Korn, E.L.; Zhang, X.; Liu, Y.; Xu, T.; Boyd, R.; Baumrind, S. Correlations between cephalometric and photographic measurements of facial attractiveness in Chinese and US patients after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 762.e1–762.e14, discussion 762–763. [Google Scholar] [CrossRef]
- Schulze, D.; Heiland, M.; Thurmann, H.; Adam, G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac. Radiol. 2004, 33, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Tsiklakis, K.; Donta, C.; Gavala, S.; Karayianni, K.; Kamenopoulou, V.; Hourdakis, C.J. Dose reduction in maxillofacial imaging using low dose Cone Beam CT. Eur. J. Radiol. 2005, 56, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Farman, A.G.; Scarfe, W.C. Development of imaging selection criteria and procedures should precede cephalometric assessment with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 257–265. [Google Scholar] [CrossRef]
- Kang, J.Y.; Kim, K.W.; Lim, S.H. The reliability of the cephalogram generated from cone-beam CT. Korean J. Orthod. 2007, 37, 391–399. [Google Scholar]
- Kumar, V.; Ludlow, J.; Soares Cevidanes, L.H.; Mol, A. In vivo comparison of conventional and cone beam CT synthesized cephalograms. Angle Orthod. 2008, 78, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Naini, F.B.; Manouchehri, S.; Al-Bitar, Z.B.; Gill, D.S.; Garagiola, U.; Wertheim, D. The maxillary incisor labial face tangent: Clinical evaluation of maxillary incisor inclination in profile smiling view and idealized aesthetics. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhayek, S.; Alsalem, M.; Alotaibi, Y.; Omair, A. Evaluation of facial appearance in patients with repaired cleft lip and palate: Comparing the assessment of laypeople and healthcare professionals. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 5. [Google Scholar] [CrossRef] [Green Version]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D cephalometry on reduced FOV CBCT: Skeletal class assessment through AF-BF on Frankfurt plane-validity and reliability through comparison with 2D measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.L. CBCT dosimetry: Orthodontic considerations. In Seminars in Orthodontics; Elsevier: Amsterdam, The Netherlands, 2009; Volume 15, pp. 14–18. [Google Scholar]
- Fourie, Z.; Damstra, J.; Gerrits, P.O.; Ren, Y. Evaluation of anthropometric accuracy and reliability using different three-dimensional scanning systems. Forensic Sci. Int. 2011, 207, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Honrado, C.P.; Larrabee, W.F., Jr. Update in three-dimensional imaging in facial plastic surgery. Curr. Opin. Otolaryngol. Head Neck Surg. 2004, 12, 327–331. [Google Scholar] [CrossRef]
- Kim, J.W.; Kim, J.C.; Jeong, C.G.; Cheon, K.J.; Cho, S.W.; Park, I.Y.; Yang, B.E. The accuracy and stability of the maxillary position after orthognathic surgery using a novel computer-aided surgical simulation system. BMC Oral Health 2019, 19, 18. [Google Scholar] [CrossRef]
- Naini, F.B.; Gill, D.S. Facial aesthetics: 2. Clinical assessment. Dent. Update 2008, 35, 159–170. [Google Scholar] [CrossRef]
- Hwang, H.S.; Kim, W.S.; McNamara, J.A. Ethnic differences in the soft tissue profile of Korean and European-American adults with normal occlusions and well-balanced faces. Angle Orthod. 2002, 72, 72–80. [Google Scholar]
- Paek, I.C.; Bowman, D.; Klapper, L. A cephalometric study of of Korean adults. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 54–59. [Google Scholar] [CrossRef]
- Salonen, L.; Mohlin, B.; Gotzlinger, B.; Hellden, L. Need and demand for orthodontic treatment in an adult Swedish population. Eur. J. Orthod. 1992, 14, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Burgersdijk, R.; Truin, G.J.; Frankenmolen, F.; Kalsbeek, H.; van’t Hof, M.; Mulder, J. Malocclusion and orthodontic treatment need of 15-74-year-old Dutch adults. Community Dent. Oral Epidemiol. 1991, 19, 64–67. [Google Scholar] [CrossRef]
- Tod, M.A.; Taverne, A.A. Prevalence of malocclusion traits in an Australian adult population. Aust. Orthod. J. 1997, 15, 16–22. [Google Scholar] [PubMed]
- Yoo, Y.K.; Lee, H.K. A study on the prevalence of malocclusion in 2,378 Yonsei university students. Korean J. Orthod. 1971, 2, 35–40. [Google Scholar]
- Lee, K.S.; Chung, K.R.; Ko, J.H.; Koo, C.H. Occlusal variations in the posterior and anterior segments of the teeth. Korean J. Orthod. 1980, 10, 71–79. [Google Scholar]



| Group | Measurement | Mean | SD | R 1 | p-Value |
|---|---|---|---|---|---|
| Control group | Incisor position | 7.28 | 0.75 | 0.96 | <0.001 * |
| (n = 25) | Forehead inclination | 17.62 | 0.06 | 0.91 | <0.001 * |
| Study group | Incisor position | 9.42 | 0.04 | 0.99 | <0.001 * |
| (n = 25) | Forehead inclination | 14.16 1 | 0.65 | 0.92 | <0.001 * |
| Group | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Control group (n = 25) | 6.7 | 4.1 | 0 | 14.8 |
| Study group (n = 25) | 9.3 | 4.9 | 1.2 | 20.4 |
| Measurement | Control | Study | p-Value |
|---|---|---|---|
| Position, mm | 6.7 | 9.3 | 0.04 |
| Forehead inclination, ° | 17.5 | 13.6 | 0.02 |
| Group | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Control group (n = 25) | 17.5 | 5.6 | 3.7 | 25.5 |
| Study group (n = 25) | 13.6 | 5.9 | 1.2 | 19.4 |
| Group | Position, mm | Inclination, ° | r 1 | p-Value |
|---|---|---|---|---|
| Control group (n = 25) | 6.7 | 17.5 | 0.384 | 0.05 |
| Study group (n = 25) | 9.3 | 9.42 1 | 0.379 | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, S.-W.; Byun, S.-H.; Yi, S.; Jang, W.-S.; Kim, J.-C.; Park, I.-Y.; Yang, B.-E. Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females. J. Pers. Med. 2021, 11, 203. https://doi.org/10.3390/jpm11030203
Cho S-W, Byun S-H, Yi S, Jang W-S, Kim J-C, Park I-Y, Yang B-E. Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females. Journal of Personalized Medicine. 2021; 11(3):203. https://doi.org/10.3390/jpm11030203
Chicago/Turabian StyleCho, Seoung-Won, Soo-Hwan Byun, Sangmin Yi, Won-Seok Jang, Jong-Cheol Kim, In-Young Park, and Byoung-Eun Yang. 2021. "Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females" Journal of Personalized Medicine 11, no. 3: 203. https://doi.org/10.3390/jpm11030203
APA StyleCho, S.-W., Byun, S.-H., Yi, S., Jang, W.-S., Kim, J.-C., Park, I.-Y., & Yang, B.-E. (2021). Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females. Journal of Personalized Medicine, 11(3), 203. https://doi.org/10.3390/jpm11030203







