Low Expression of IL-15 and NKT in Tumor Microenvironment Predicts Poor Outcome of MYCN-Non-Amplified Neuroblastoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Processing
2.2. Neuroblastoma (NBL) Samples
2.3. Real-Time Reverse-Transcription Polymerase Chain Reaction
2.4. Statistical Analysis
3. Result
3.1. NKTs and IL-15 Expression Were Increased in the Tumor Microenvironment of MYCN-Non-Amplified NBL
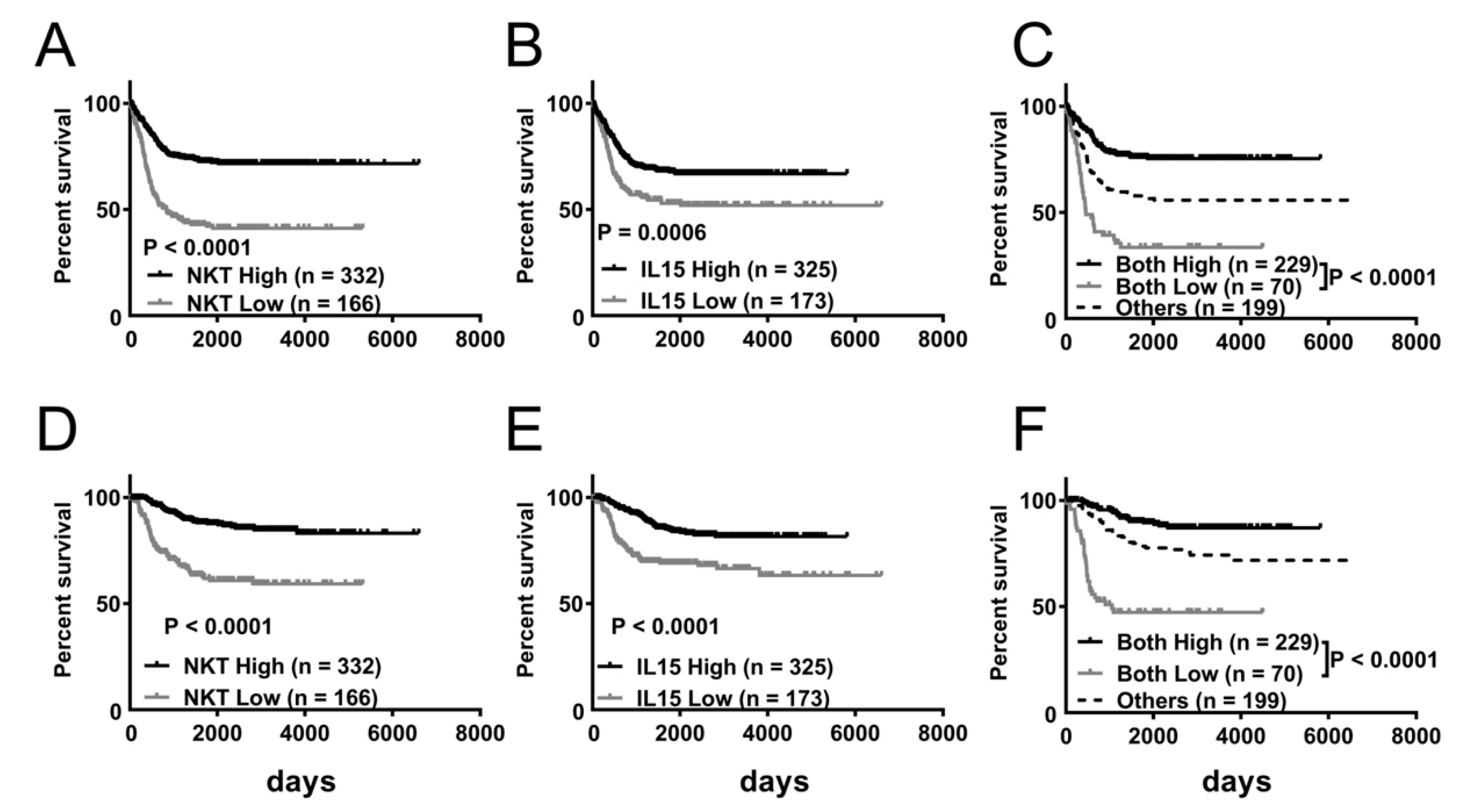
3.2. Lower NKT Immunoscore or IL-15 Expression Level Is Associated with Decreased Event-Free and Overall Survival in NBL Dataset
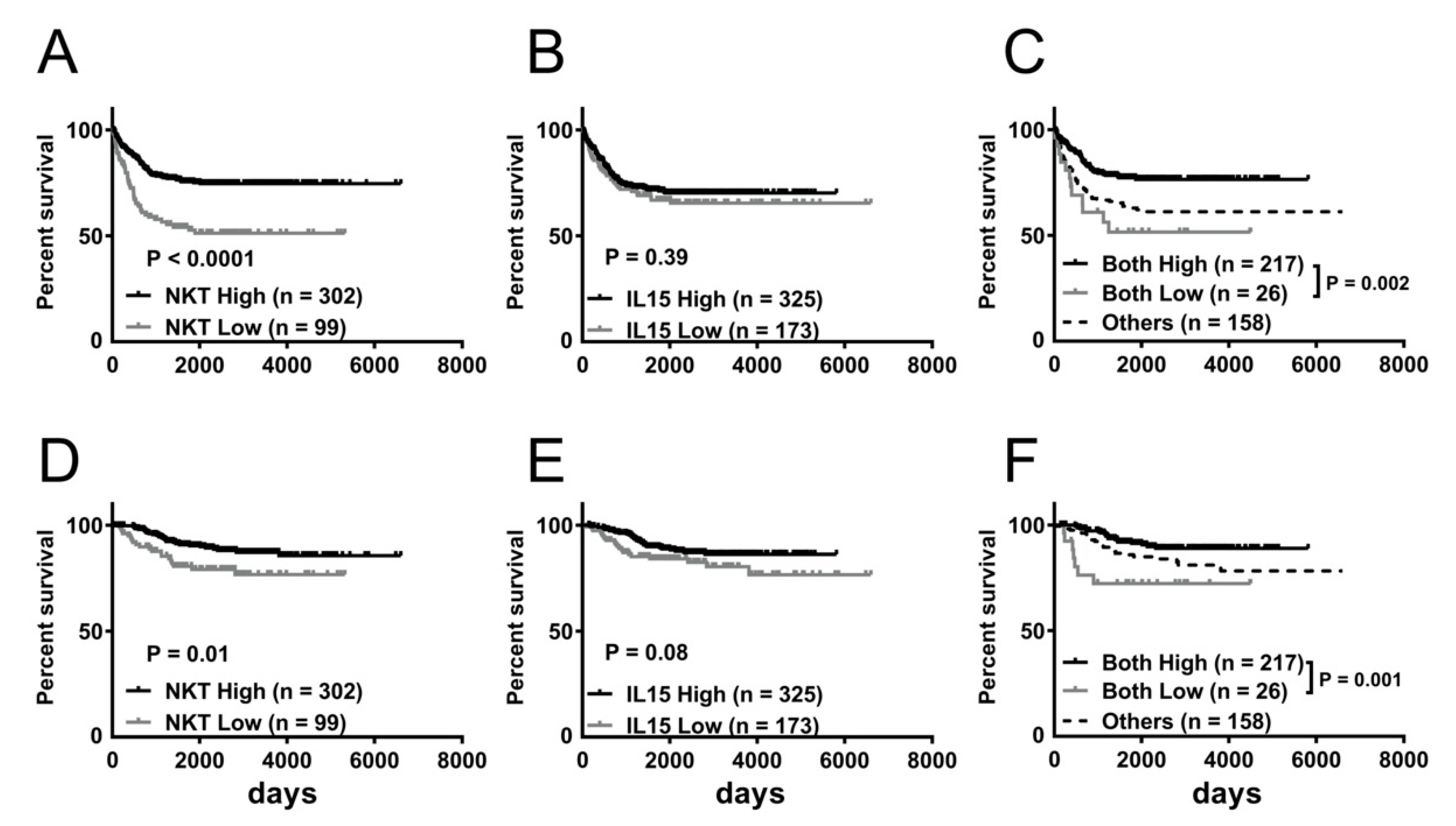
3.3. Survival Benefit of Greater Abundance of NKT Alone or in Combination with Higher IL-15 Expression in MYCN-Non-Amplified NBL
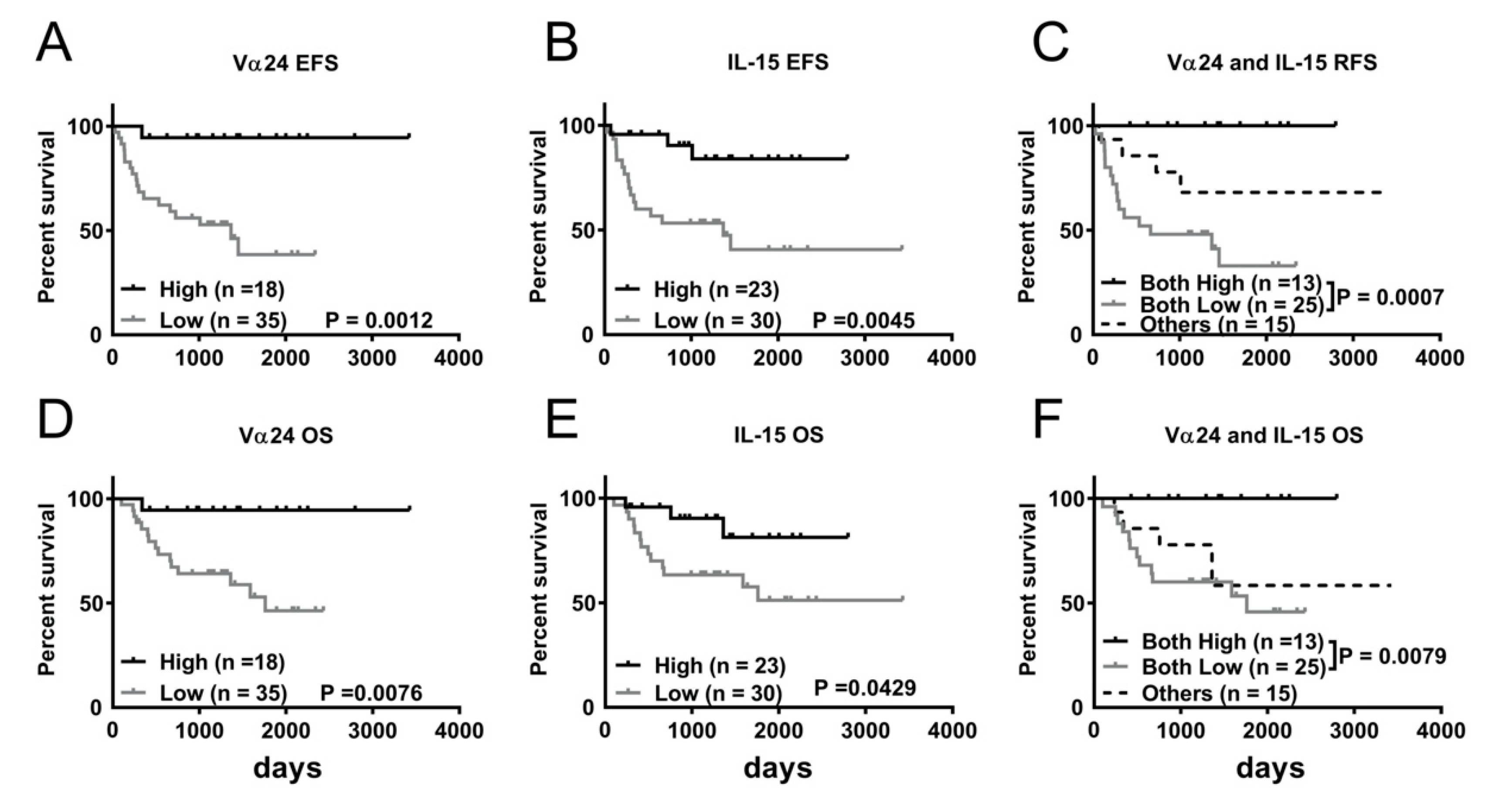
3.4. Lower Expression of Vα24 or IL-15 Is Associated with Decreased Overall Survival in NBL Patients
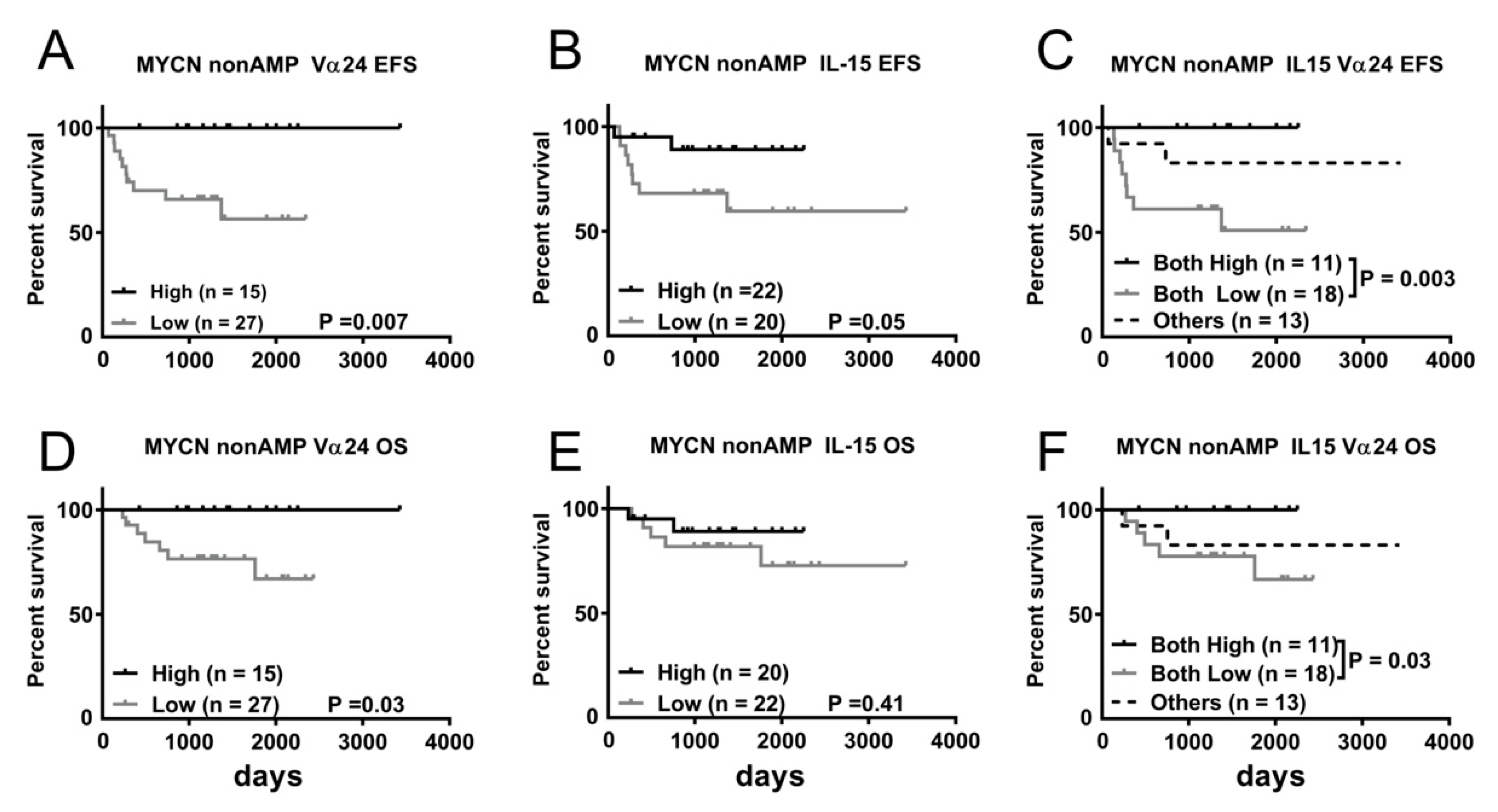
3.5. Lower Expression of Vα24 or IL-15 Is Associated with Inferior Overall Survival in MYCN-Non-Amplified NBL Patients
3.6. Lower NKT Immunoscore Is Associated with Inferior Overall Survival in MYCN-Amplified NBL Dataset
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stiller, C.A.; Parkin, D.M. International variations in the incidence of neuroblastoma. Int. J. Cancer 1992, 52, 538–543. [Google Scholar] [CrossRef]
- Pinto, N.R.; Applebaum, M.A.; Volchenboum, S.L.; Matthay, K.K.; London, W.B.; Ambros, P.F.; Nakagawara, A.; Berthold, F.; Schleiermacher, G.; Park, J.R.; et al. Advances in Risk Classification and Treatment Strategies for Neuroblastoma. J. Clin. Oncol. 2015, 33, 3008–3017. [Google Scholar] [CrossRef]
- Yu, A.L.; Gilman, A.L.; Ozkaynak, M.F.; London, W.B.; Kreissman, S.G.; Chen, H.X.; Smith, M.; Anderson, B.; Villablanca, J.G.; Matthay, K.K.; et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 2010, 363, 1324–1334. [Google Scholar] [CrossRef]
- Borriello, L.; Seeger, R.C.; Asgharzadeh, S.; DeClerck, Y.A. More than the genes, the tumor microenvironment in neuroblastoma. Cancer Lett. 2016, 380, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Blavier, L.; Yang, R.M.; DeClerck, Y.A. The Tumor Microenvironment in Neuroblastoma: New Players, New Mechanisms of Interaction and New Perspectives. Cancers 2020, 12, 2912. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Vo, K.T.; London, W.B.; Fischer, M.; Ambros, P.F.; Nakagawara, A.; Brodeur, G.M.; Matthay, K.K.; DuBois, S.G. Identification of patient subgroups with markedly disparate rates of MYCN amplification in neuroblastoma: A report from the International Neuroblastoma Risk Group project. Cancer 2016, 122, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Brodeur, G.M.; Seeger, R.C.; Schwab, M.; Varmus, H.E.; Bishop, J.M. Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage. Science 1984, 224, 1121–1124. [Google Scholar] [CrossRef]
- Tang, X.X.; Zhao, H.; Kung, B.; Kim, D.Y.; Hicks, S.L.; Cohn, S.L.; Cheung, N.K.; Seeger, R.C.; Evans, A.E.; Ikegaki, N. The MYCN enigma: Significance of MYCN expression in neuroblastoma. Cancer Res. 2006, 66, 2826–2833. [Google Scholar] [CrossRef]
- Zhang, P.; Wu, X.; Basu, M.; Dong, C.; Zheng, P.; Liu, Y.; Sandler, A.D. MYCN Amplification Is Associated with Repressed Cellular Immunity in Neuroblastoma: An In Silico Immunological Analysis of TARGET Database. Front. Immunol. 2017, 8, 1473. [Google Scholar] [CrossRef] [PubMed]
- Brandetti, E.; Veneziani, I.; Melaiu, O.; Pezzolo, A.; Castellano, A.; Boldrini, R.; Ferretti, E.; Fruci, D.; Moretta, L.; Pistoia, V.; et al. MYCN is an immunosuppressive oncogene dampening the expression of ligands for NK-cell-activating receptors in human high-risk neuroblastoma. Oncoimmunology 2017, 6, e1316439. [Google Scholar] [CrossRef]
- Erbe, A.K.; Wang, W.; Carmichael, L.; Kim, K.; Mendonca, E.A.; Song, Y.; Hess, D.; Reville, P.K.; London, W.B.; Naranjo, A.; et al. Neuroblastoma Patients’ KIR and KIR-Ligand Genotypes Influence Clinical Outcome for Dinutuximab-based Immunotherapy: A Report from the Children’s Oncology Group. Clin. Cancer Res. 2018, 24, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Mina, M.; Boldrini, R.; Citti, A.; Romania, P.; D’Alicandro, V.; De Ioris, M.; Castellano, A.; Furlanello, C.; Locatelli, F.; Fruci, D. Tumor-infiltrating T lymphocytes improve clinical outcome of therapy-resistant neuroblastoma. Oncoimmunology 2015, 4, e1019981. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.S.; Kuznetsov, I.B.; Zhang, S.; Song, Y.K.; Asgharzadeh, S.; Sindiri, S.; Wen, X.; Patidar, R.; Najaraj, S.; Walton, A.; et al. Clinically Relevant Cytotoxic Immune Cell Signatures and Clonal Expansion of T-Cell Receptors in High-Risk MYCN-Not-Amplified Human Neuroblastoma. Clin. Cancer Res. 2018, 24, 5673–5684. [Google Scholar] [CrossRef]
- Song, L.; Asgharzadeh, S.; Salo, J.; Engell, K.; Wu, H.W.; Sposto, R.; Ara, T.; Silverman, A.M.; DeClerck, Y.A.; Seeger, R.C.; et al. Vα24-invariant NKT cells mediate antitumor activity via killing of tumor-associated macrophages. J. Clin. Investig. 2009, 119, 1524–1536. [Google Scholar] [CrossRef]
- Song, L.; Ara, T.; Wu, H.W.; Woo, C.W.; Reynolds, C.P.; Seeger, R.C.; DeClerck, Y.A.; Thiele, C.J.; Sposto, R.; Metelitsa, L.S. Oncogene MYCN regulates localization of NKT cells to the site of disease in neuroblastoma. J. Clin. Investig. 2007, 117, 2702–2712. [Google Scholar] [CrossRef]
- Metelitsa, L.S.; Wu, H.W.; Wang, H.; Yang, Y.; Warsi, Z.; Asgharzadeh, S.; Groshen, S.; Wilson, S.B.; Seeger, R.C. Natural killer T cells infiltrate neuroblastomas expressing the chemokine CCL2. J. Exp. Med. 2004, 199, 1213–1221. [Google Scholar] [CrossRef]
- Bendelac, A.; Rivera, M.N.; Park, S.H.; Roark, J.H. Mouse CD1-specific NK1 T cells: Development, specificity, and function. Annu Rev. Immunol. 1997, 15, 535–562. [Google Scholar] [CrossRef]
- Xu, X.; Huang, W.; Heczey, A.; Liu, D.; Guo, L.; Wood, M.; Jin, J.; Courtney, A.N.; Liu, B.; Di Pierro, E.J.; et al. NKT Cells Coexpressing a GD2-Specific Chimeric Antigen Receptor and IL15 Show Enhanced In Vivo Persistence and Antitumor Activity against Neuroblastoma. Clin. Cancer Res. 2019, 25, 7126–7138. [Google Scholar] [CrossRef] [PubMed]
- Heinze, A.; Grebe, B.; Bremm, M.; Huenecke, S.; Munir, T.A.; Graafen, L.; Frueh, J.T.; Merker, M.; Rettinger, E.; Soerensen, J.; et al. The Synergistic Use of IL-15 and IL-21 for the Generation of NK Cells From CD3/CD19-Depleted Grafts Improves Their ex vivo Expansion and Cytotoxic Potential Against Neuroblastoma: Perspective for Optimized Immunotherapy Post Haploidentical Stem Cell Transplantation. Front. Immunol. 2019, 10, 2816. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, R.; Moustaki, A.; Norrie, J.L.; Brown, S.; Akers, W.J.; Shirinifard, A.; Dyer, M.A. Interleukin-15 Enhances Anti-GD2 Antibody-Mediated Cytotoxicity in an Orthotopic PDX Model of Neuroblastoma. Clin. Cancer Res. 2019, 25, 7554–7564. [Google Scholar] [CrossRef]
- Matsuda, J.L.; Gapin, L.; Sidobre, S.; Kieper, W.C.; Tan, J.T.; Ceredig, R.; Surh, C.D.; Kronenberg, M. Homeostasis of Vα14i NKT cells. Nat. Immunol. 2002, 3, 966–974. [Google Scholar] [CrossRef]
- Baev, D.V.; Peng, X.H.; Song, L.; Barnhart, J.R.; Crooks, G.M.; Weinberg, K.I.; Metelitsa, L.S. Distinct homeostatic requirements of CD4+ and CD4- subsets of Vα24-invariant natural killer T cells in humans. Blood 2004, 104, 4150–4156. [Google Scholar] [CrossRef]
- Aran, D.; Hu, Z.; Butte, A.J. xCell: Digitally portraying the tissue cellular heterogeneity landscape. Genome Biol. 2017, 18, 220. [Google Scholar] [CrossRef]
- Lin, R.J.; Lin, Y.C.; Chen, J.; Kuo, H.H.; Chen, Y.Y.; Diccianni, M.B.; London, W.B.; Chang, C.H.; Yu, A.L. microRNA signature and expression of Dicer and Drosha can predict prognosis and delineate risk groups in neuroblastoma. Cancer Res. 2010, 70, 7841–7850. [Google Scholar] [CrossRef]
- Huh, J.Y.; Kim, J.I.; Park, Y.J.; Hwang, I.J.; Lee, Y.S.; Sohn, J.H.; Lee, S.K.; Alfadda, A.A.; Kim, S.S.; Choi, S.H.; et al. A novel function of adipocytes in lipid antigen presentation to iNKT cells. Mol. Cell. Biol. 2013, 33, 328–339. [Google Scholar] [CrossRef]
- Gamero, A.M.; Ussery, D.; Reintgen, D.S.; Puleo, C.A.; Djeu, J.Y. Interleukin 15 induction of lymphokine-activated killer cell function against autologous tumor cells in melanoma patient lymphocytes by a CD18-dependent, perforin-related mechanism. Cancer Res. 1995, 55, 4988–4994. [Google Scholar] [PubMed]
- Gordy, L.E.; Bezbradica, J.S.; Flyak, A.I.; Spencer, C.T.; Dunkle, A.; Sun, J.; Stanic, A.K.; Boothby, M.R.; He, Y.W.; Zhao, Z.; et al. IL-15 regulates homeostasis and terminal maturation of NKT cells. J. Immunol. 2011, 187, 6335–6345. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.K.; Glaccum, M.; Brown, S.N.; Butz, E.A.; Viney, J.L.; Embers, M.; Matsuki, N.; Charrier, K.; Sedger, L.; Willis, C.R.; et al. Reversible defects in natural killer and memory CD8 T cell lineages in interleukin 15-deficient mice. J. Exp. Med. 2000, 191, 771–780. [Google Scholar] [CrossRef]
- Seeger, R.C.; Brodeur, G.M.; Sather, H.; Dalton, A.; Siegel, S.E.; Wong, K.Y.; Hammond, D. Association of multiple copies of the N-myc oncogene with rapid progression of neuroblastomas. N. Engl. J. Med. 1985, 313, 1111–1116. [Google Scholar] [CrossRef]
- Weiss, W.A.; Aldape, K.; Mohapatra, G.; Feuerstein, B.G.; Bishop, J.M. Targeted expression of MYCN causes neuroblastoma in transgenic mice. EMBO J. 1997, 16, 2985–2995. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Weiss, W.A. Neuroblastoma and MYCN. Cold Spring Harb. Perspect. Med. 2013, 3, a014415. [Google Scholar] [CrossRef]
- Layer, J.P.; Kronmuller, M.T.; Quast, T.; van den Boorn-Konijnenberg, D.; Effern, M.; Hinze, D.; Althoff, K.; Schramm, A.; Westermann, F.; Peifer, M.; et al. Amplification of N-Myc is associated with a T-cell-poor microenvironment in metastatic neuroblastoma restraining interferon pathway activity and chemokine expression. Oncoimmunology 2017, 6, e1320626. [Google Scholar] [CrossRef] [PubMed]
- Schwab, M.; Alitalo, K.; Klempnauer, K.H.; Varmus, H.E.; Bishop, J.M.; Gilbert, F.; Brodeur, G.; Goldstein, M.; Trent, J. Amplified DNA with limited homology to myc cellular oncogene is shared by human neuroblastoma cell lines and a neuroblastoma tumour. Nature 1983, 305, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Kohl, N.E.; Kanda, N.; Schreck, R.R.; Bruns, G.; Latt, S.A.; Gilbert, F.; Alt, F.W. Transposition and amplification of oncogene-related sequences in human neuroblastomas. Cell 1983, 35, 359–367. [Google Scholar] [CrossRef]
- Casey, S.C.; Baylot, V.; Felsher, D.W. MYC: Master Regulator of Immune Privilege. Trends Immunol. 2017, 38, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Casey, S.C.; Baylot, V.; Felsher, D.W. The MYC oncogene is a global regulator of the immune response. Blood 2018, 131, 2007–2015. [Google Scholar] [CrossRef]
- Marinkovic, D.; Marinkovic, T. The new role for an old guy: MYC as an immunoplayer. J. Cell. Physiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Blum, D.L.; Koyama, T.; M’Koma, A.E.; Iturregui, J.M.; Martinez-Ferrer, M.; Uwamariya, C.; Smith, J.A., Jr.; Clark, P.E.; Bhowmick, N.A. Chemokine markers predict biochemical recurrence of prostate cancer following prostatectomy. Clin. Cancer Res. 2008, 14, 7790–7797. [Google Scholar] [CrossRef]
- Vilsmaier, T.; Heidegger, H.H.; Schroder, L.; Trapp, E.; Zehni, A.Z.; Rack, B.; Janni, W.; Mahner, S.; Weissenbacher, T.; Jeschke, U.; et al. Interleukin 15 and Eotaxin correlate with the outcome of breast cancer patients vice versa independent of CTC status. Arch. Gynecol. Obstet. 2020. [Google Scholar] [CrossRef]
- Dong, Y.; Liu, Y.; Bai, H.; Jiao, S. Systematic assessment of the clinicopathological prognostic significance of tissue cytokine expression for lung adenocarcinoma based on integrative analysis of TCGA data. Sci. Rep. 2019, 9, 6301. [Google Scholar] [CrossRef]
- Fehniger, T.A.; Caligiuri, M.A. Interleukin 15: Biology and relevance to human disease. Blood 2001, 97, 14–32. [Google Scholar] [CrossRef] [PubMed]
- Frost, J.D.; Hank, J.A.; Reaman, G.H.; Frierdich, S.; Seeger, R.C.; Gan, J.; Anderson, P.M.; Ettinger, L.J.; Cairo, M.S.; Blazar, B.R.; et al. A phase I/IB trial of murine monoclonal anti-GD2 antibody 14.G2a plus interleukin-2 in children with refractory neuroblastoma: A report of the Children’s Cancer Group. Cancer 1997, 80, 317–333. [Google Scholar] [CrossRef]
- Waldmann, T.A. The biology of interleukin-2 and interleukin-15: Implications for cancer therapy and vaccine design. Nat. Rev. Immunol. 2006, 6, 595–601. [Google Scholar] [CrossRef]
- Van den Bergh, J.M.; Van Tendeloo, V.F.; Smits, E.L. Interleukin-15: New kid on the block for antitumor combination therapy. Cytokine Growth Factor Rev. 2015, 26, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, T.A. Interleukin-15 in the treatment of cancer. Expert Rev. Clin. Immunol. 2014, 10, 1689–1701. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Sun, C.; Landoni, E.; Metelitsa, L.; Dotti, G.; Savoldo, B. Eradication of Neuroblastoma by T Cells Redirected with an Optimized GD2-Specific Chimeric Antigen Receptor and Interleukin-15. Clin. Cancer Res. 2019, 25, 2915–2924. [Google Scholar] [CrossRef] [PubMed]
- Hishiki, T.; Mise, N.; Harada, K.; Ihara, F.; Takami, M.; Saito, T.; Terui, K.; Nakata, M.; Komatsu, S.; Yoshida, H.; et al. Invariant natural killer T infiltration in neuroblastoma with favorable outcome. Pediatr. Surg. Int. 2018, 34, 195–201. [Google Scholar] [CrossRef]
- Liu, D.; Song, L.; Wei, J.; Courtney, A.N.; Gao, X.; Marinova, E.; Guo, L.; Heczey, A.; Asgharzadeh, S.; Kim, E.; et al. IL-15 protects NKT cells from inhibition by tumor-associated macrophages and enhances antimetastatic activity. J. Clin. Investig. 2012, 122, 2221–2233. [Google Scholar] [CrossRef]
- Zhang, S.; Zhao, J.; Bai, X.; Handley, M.; Shan, F. Biological effects of IL-15 on immune cells and its potential for the treatment of cancer. Int. Immunopharmacol. 2021, 91, 107318. [Google Scholar] [CrossRef] [PubMed]
- Heczey, A.; Courtney, A.N.; Montalbano, A.; Robinson, S.; Liu, K.; Li, M.; Ghatwai, N.; Dakhova, O.; Liu, B.; Raveh-Sadka, T.; et al. Anti-GD2 CAR-NKT cells in patients with relapsed or refractory neuroblastoma: An interim analysis. Nat. Med. 2020, 26, 1686–1690. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.J.; Huang, J.R.; Tsai, Y.C.; Hung, J.T.; Wu, D.; Fujio, M.; Wong, C.H.; Yu, A.L. Potent immune-modulating and anticancer effects of NKT cell stimulatory glycolipids. Proc. Natl. Acad. Sci. USA 2007, 104, 10299–10304. [Google Scholar] [CrossRef] [PubMed]
- Hung, J.T.; Huang, J.R.; Yu, A.L. Tailored design of NKT-stimulatory glycolipids for polarization of immune responses. J. Biomed. Sci. 2017, 24, 22. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Number (%) |
|---|---|
| Age at diagnosis | |
| <1.5 years | 32 (60.4) |
| ≥1.5 years | 21 (39.6) |
| INSS stage | |
| 1 | 7 (13.2) |
| 2 | 10 (18.9) |
| 3 | 10 (18.9) |
| 4 | 20 (37.7) |
| 4s | 6 (11.3) |
| Risk group | |
| Low and intermediate | 30 (56.6) |
| High | 23 (43.4) |
| Histology a | |
| Favorable | 19 (35.8) |
| Unfavorable | 13 (24.5) |
| MYCN | |
| Non-amplified | 42 (79.2) |
| Amplified | 11 (20.7) |
| Progression/Event | |
| No | 34 (64.2) |
| Yes | 19 (35.8) |
| Death from disease | |
| Alive | 37 (69.8) |
| Dead | 16 (30.2) |
| Overall Survival | |||
|---|---|---|---|
| Variables | HR (95% CI) | Favorable/Unfavorable | p |
| Univariate analysis | |||
| Stage | 7.64 (2.42–24.15) | 1, 2, 3, 4S/4 | 0.001 |
| Risk group | 31.15 (4.09–237.38) | Low, Middle/High | 0.001 |
| Age at diagnosis_1.5 | 5.08 (1.63–15.79) | <1.5 years/≥1.5 years | 0.005 |
| Vα24 | 9.51 (1.26–72.03) | Low/High | 0.03 |
| IL-15 | 3.39 (0.97–11.93) | Low/High | 0.05 |
| Vα24 and IL-15 | 3.55 (1.14–11.01) | All Low/Others | 0.03 |
| Multivariate analysis | |||
| Stage | 5.04 (0.49–51.34) | 1, 2, 3, 4S/4 | 0.17 |
| Risk group | 95.60 (4.59–189.12) | Low, Middle/High | 0.003 |
| Age at diagnosis_1.5 | 1.62 (0.47–5.59) | <1.5 years/≥1.5 years | 0.45 |
| Vα24 | 6.21 (0.80–48.09) | Low/High | 0.08 |
| IL-15 | 4.18 (1.18–14.80) | Low/High | 0.027 |
| Vα24 and IL-15 | 8.14 (1.05–63.06) | All Low/Others | 0.045 |
| Event-Free Survival | |||
|---|---|---|---|
| Variables | HR (95% CI) | Favorable/Unfavorable | p |
| Univariate analysis | |||
| Stage | 3.69 (1.43–9.49) | 1, 2, 3, 4S/4 | 0.007 |
| Risk group | 6.63 (2.18–20.15) | Low, Middle/High | 0.001 |
| Age at diagnosis_1.5 | 3.85 (1.46–10.17) | <1.5 years/≥1.5 years | 0.006 |
| Vα24 | 13.24 (1.76–99.68) | Low/High | 0.012 |
| IL-15 | 5.00 (1.46–17.21) | Low/High | 0.011 |
| Vα24 and IL-15 | 5.50 (1.81–16.6) | All Low/Others | 0.003 |
| Multivariate analysis | |||
| Stage | 8.51 (0.83–87.84) | 1, 2, 3, 4S/4 | 0.07 |
| Risk group | 21.14 (1.79–249.09) | Low, Middle/High | 0.015 |
| Age at diagnosis_1.5 | 2.43 (0.73–8.08) | <1.5 years/≥1.5 years | 0.147 |
| Vα24 | 10.26 (1.33–79.36) | Low/High | 0.026 |
| IL-15 | 4.95 (1.43–17.12) | Low/High | 0.012 |
| Vα24 and IL-15 | 15.55 (1.99–121.41) | All Low/Others | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, Y.-M.; Hung, T.-H.; Tung, J.K.; Yu, J.; Hsu, Y.-L.; Hung, J.-T.; Yu, A.L. Low Expression of IL-15 and NKT in Tumor Microenvironment Predicts Poor Outcome of MYCN-Non-Amplified Neuroblastoma. J. Pers. Med. 2021, 11, 122. https://doi.org/10.3390/jpm11020122
Liao Y-M, Hung T-H, Tung JK, Yu J, Hsu Y-L, Hung J-T, Yu AL. Low Expression of IL-15 and NKT in Tumor Microenvironment Predicts Poor Outcome of MYCN-Non-Amplified Neuroblastoma. Journal of Personalized Medicine. 2021; 11(2):122. https://doi.org/10.3390/jpm11020122
Chicago/Turabian StyleLiao, Yu-Mei, Tsai-Hsien Hung, John K. Tung, John Yu, Ya-Ling Hsu, Jung-Tung Hung, and Alice L. Yu. 2021. "Low Expression of IL-15 and NKT in Tumor Microenvironment Predicts Poor Outcome of MYCN-Non-Amplified Neuroblastoma" Journal of Personalized Medicine 11, no. 2: 122. https://doi.org/10.3390/jpm11020122
APA StyleLiao, Y.-M., Hung, T.-H., Tung, J. K., Yu, J., Hsu, Y.-L., Hung, J.-T., & Yu, A. L. (2021). Low Expression of IL-15 and NKT in Tumor Microenvironment Predicts Poor Outcome of MYCN-Non-Amplified Neuroblastoma. Journal of Personalized Medicine, 11(2), 122. https://doi.org/10.3390/jpm11020122








