Circulating p16-Positive and p16-Negative Tumor Cells Serve as Independent Prognostic Indicators of Survival in Patients with Head and Neck Squamous Cell Carcinomas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Tissue Immunohistochemistry Staining for p16 Expression Analysis
2.3. The Isolation and Identification of Circulating Tumor Cells via Microscopy
2.4. Analysis of p16 Expression in Circulating Tumor Cells via Flow Cytometry
2.5. Human Papillomavirus Genotyping
2.6. Statistical Analysis
3. Results
3.1. Patient Enrollment
3.2. The Identification of p16-Positive Circulating Tumor Cells in Cancer Patients
3.3. HPV Genotyping of Cancer Tissues and Circulating Tumor Cells
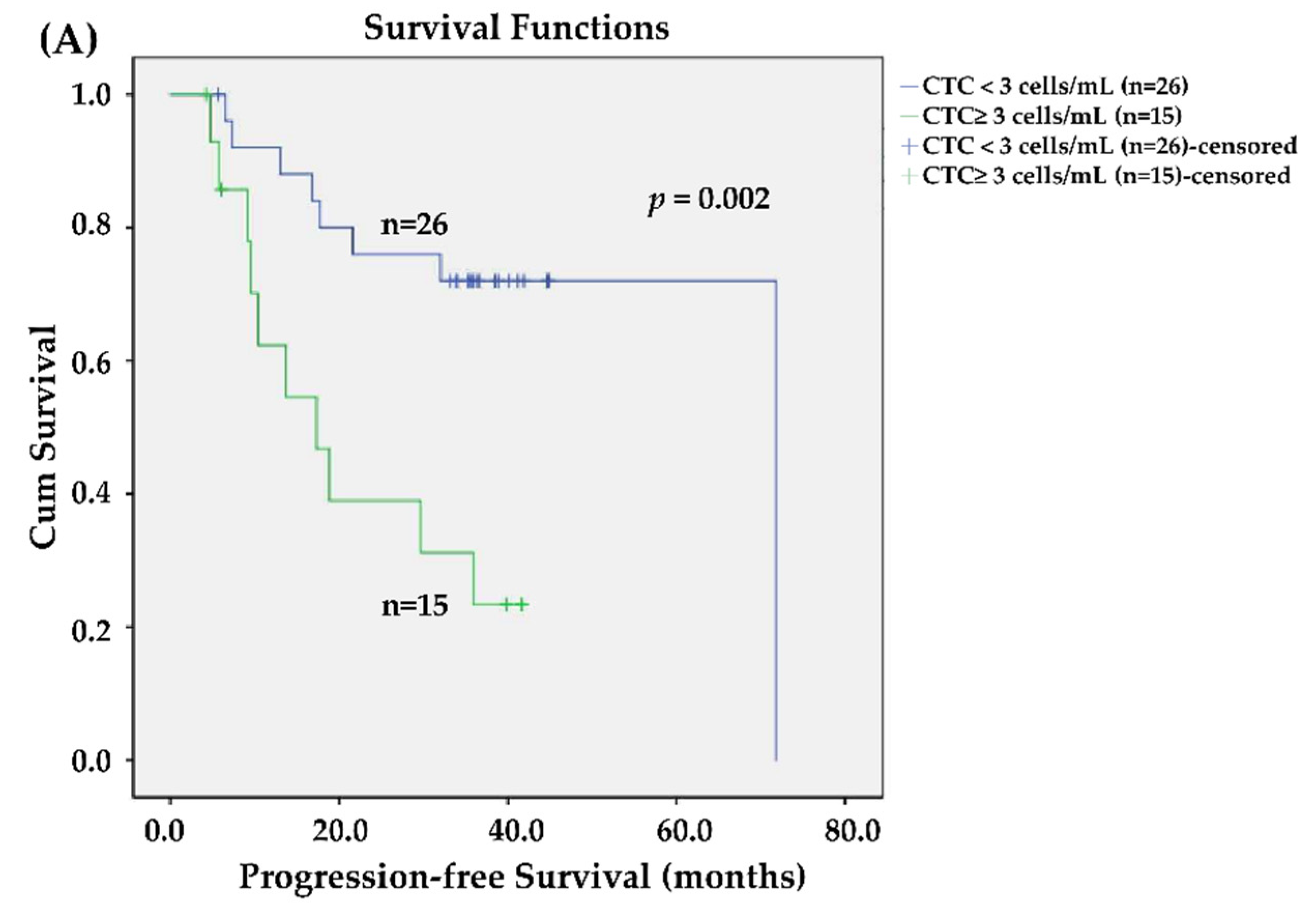
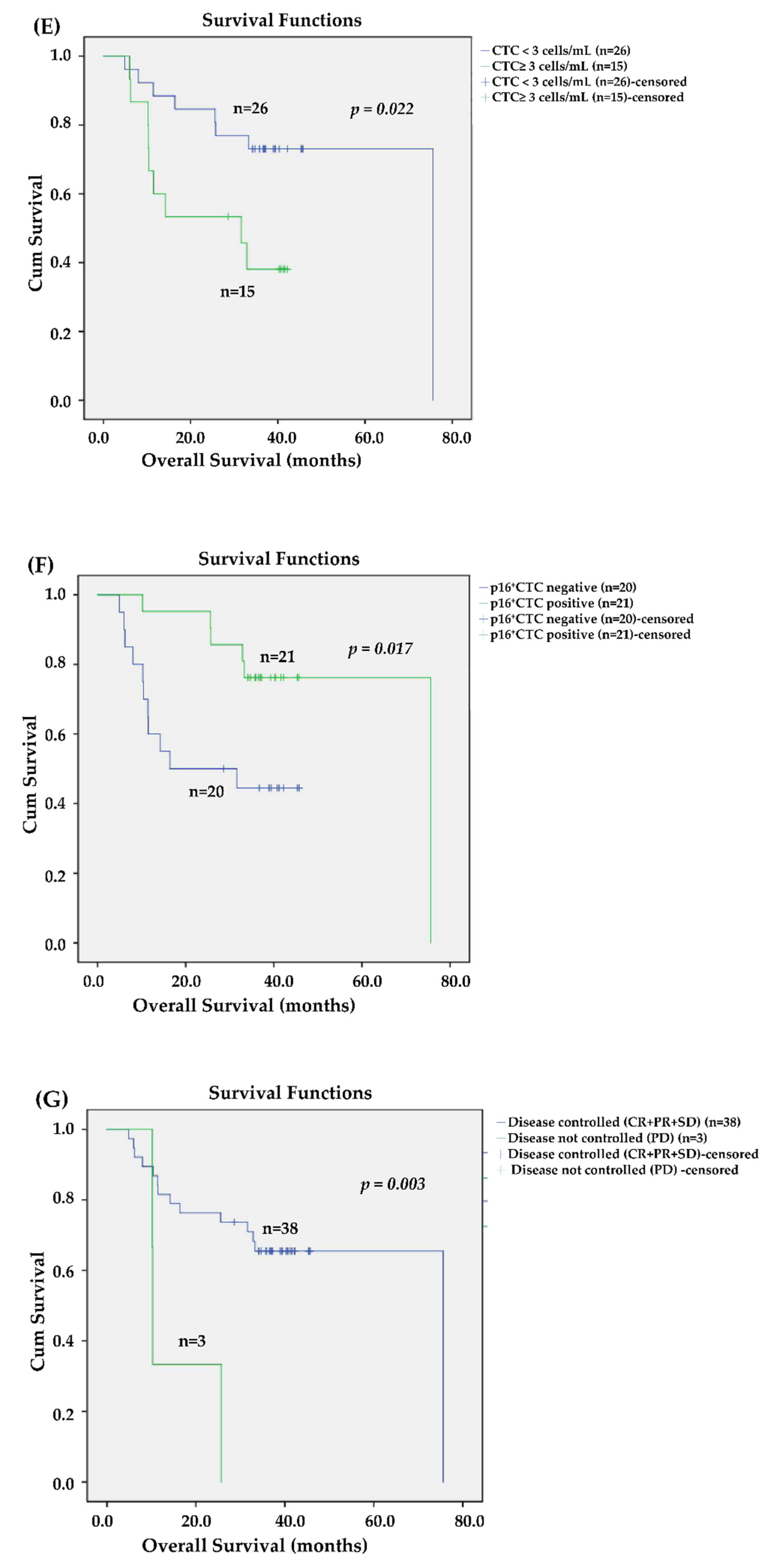
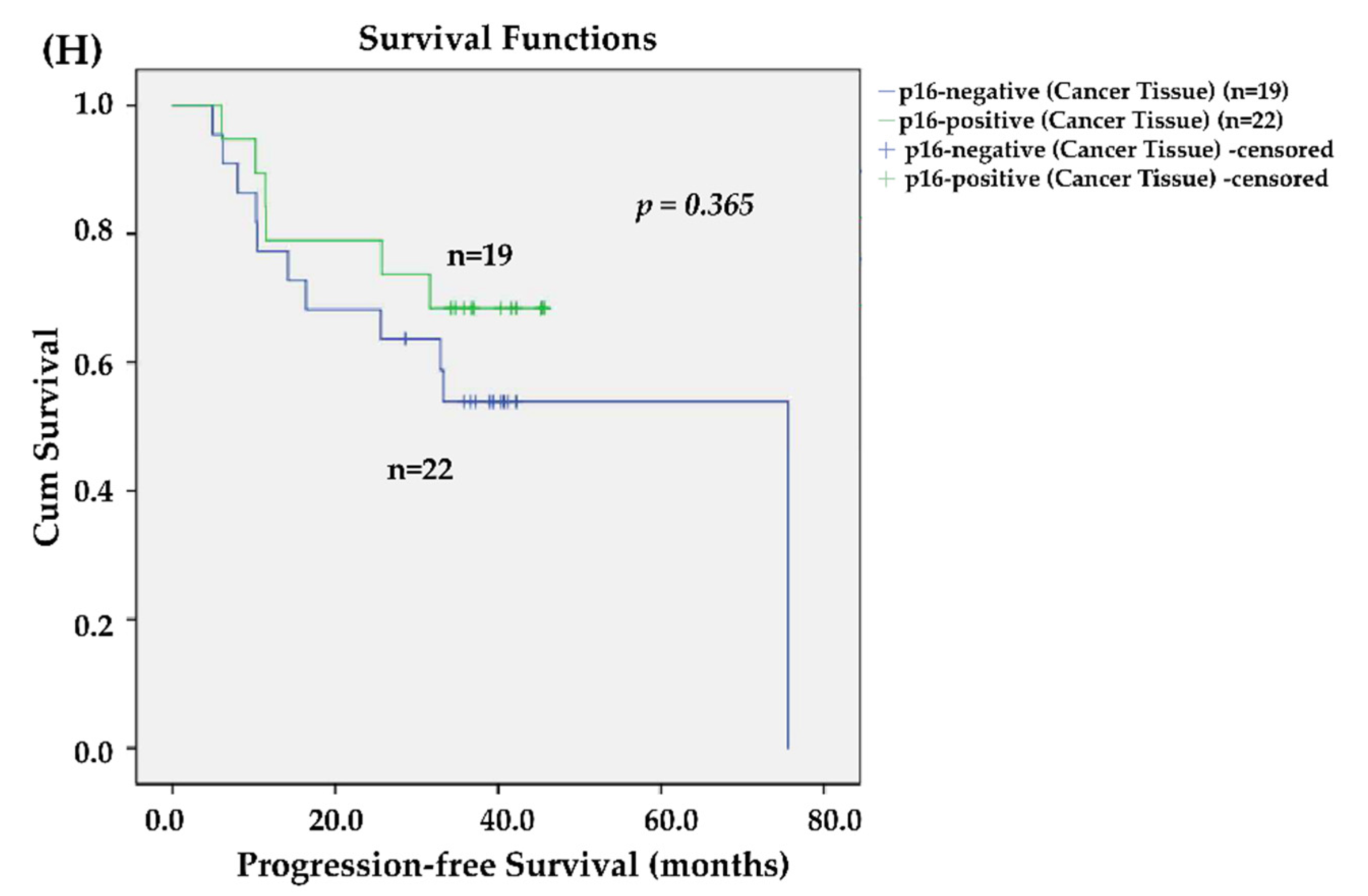
3.4. Effects of CTCs and p16-Positive CTCs on Survival
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Full name | Abbreviations |
| head and neck squamous cell carcinomas | HNSCC |
| human papillomavirus | HPV |
| circulating tumor cells | CTCs |
| confidence interval | CI |
| concurrent chemoradiotherapy | CCRT |
| American Joint Committee on Cancer | AJCC |
| response evaluation criteria in solid tumors | RECIST |
| complete remission | CR |
| partial response | PR |
| Stable disease | SD |
| progressive disease | PD |
| Immunohistochemistry staining | IHC |
| Progression-free survival | PFS |
| Overall survival | OS |
| Eastern Cooperative Oncology Group performance status | ECOG PS |
References
- McKaig, R.G.; Baric, R.S.; Olshan, A.F. Human papillomavirus and head and neck cancer: Epidemiology and molecular biology. Head Neck 1998, 20, 250–265. [Google Scholar] [CrossRef]
- Mork, J.; Lie, A.K.; Glattre, E.; Clark, S.; Hallmans, G.; Jellum, E.; Koskela, P.; Møller, B.; Pukkala, E.; Schiller, J.T. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 2001, 344, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.H.; Pawlita, M.; Michaud, D.S.; McClean, M.; Langevin, S.M.; Eliot, M.N.; Kelsey, K.T. Immune Response to HPV16 E6 and E7 Proteins and Patient Outcomes in Head and Neck Cancer. JAMA Oncol. 2017, 3, 178–185. [Google Scholar] [CrossRef]
- Ferreira, C.d.C.; Dufloth, R.; de Carvalho, A.C.; Reis, R.M.; Santana, I.; Carvalho, R.S.; Gama, R.R. Correlation of p16 immunohistochemistry with clinical and epidemiological features in oropharyngeal squamous-cell carcinoma. PLoS ONE 2021, 16, e0253418. [Google Scholar] [CrossRef]
- Fakhry, C.; Gillison, M.L. Clinical implications of human papillomavirus in head and neck cancers. J. Clin. Oncol. 2006, 24, 2606–2611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burbure, N.; Handorf, E.; Ridge, J.A.; Bauman, J.; Liu, J.C.; Giri, A.; Galloway, T.J. Prognostic significance of human papillomavirus status and treatment modality in hypopharyngeal cancer. Head Neck 2021, 43, 3042–3052. [Google Scholar] [CrossRef]
- Saito, Y.; Hayashi, R.; Iida, Y.; Mizumachi, T.; Fujii, T.; Matsumoto, F.; Beppu, T.; Yoshida, M.; Shinomiya, H.; Kamiyama, R. Optimization of therapeutic strategy for p16-positive oropharyngeal squamous cell carcinoma: Multi-institutional observational study based on the national Head and Neck Cancer Registry of Japan. Cancer 2020, 126, 4177–4187. [Google Scholar] [CrossRef]
- Patel, R.R.; Ludmir, E.B.; Augustyn, A.; Zaorsky, N.G.; Lehrer, E.J.; Ryali, R.; Trifiletti, D.M.; Adeberg, S.; Amini, A.; Verma, V. De-intensification of therapy in human papillomavirus associated oropharyngeal cancer: A systematic review of prospective trials. Oral Oncol. 2020, 103, 104608. [Google Scholar] [CrossRef]
- Iganej, S.; Beard, B.W.; Chen, J.; Buchschacher, G.L., Jr.; Abdalla, I.A.; Thompson, L.D.; Bhattasali, O. Triweekly carboplatin as a potential de-intensification agent in concurrent chemoradiation for early-stage HPV-associated oropharyngeal cancer. Oral Oncol. 2019, 97, 18–22. [Google Scholar] [CrossRef]
- Cohen, E.; Coviello, C.; Menaker, S.; Martinez-Duarte, E.; Gomez, C.; Lo, K.; Kerr, D.; Franzmann, E.; Leibowitz, J.; Sargi, Z. P16 and human papillomavirus in sinonasal squamous cell carcinoma. Head Neck 2020, 42, 2021–2029. [Google Scholar] [CrossRef]
- Shinn, J.R.; Davis, S.J.; Lang-Kuhs, K.A.; Rohde, S.; Wang, X.; Liu, P.; Dupont, W.D.; Plummer Jr, D.; Thorstad, W.L.; Chernock, R.D. Oropharyngeal Squamous Cell Carcinoma With Discordant p16 and HPV mRNA Results: Incidence and Characterization in a Large, Contemporary United States Cohort. Am. J. Surg. Pathol. 2021, 45, 951–961. [Google Scholar] [PubMed]
- Lifsics, A.; Groma, V.; Cistjakovs, M.; Skuja, S.; Deksnis, R.; Murovska, M. Identification of High-Risk Human Papillomavirus DNA, p16, and E6/E7 Oncoproteins in Laryngeal and Hypopharyngeal Squamous Cell Carcinomas. Viruses 2021, 13, 1008. [Google Scholar] [CrossRef] [PubMed]
- Nauta, I.H.; Heideman, D.A.; Brink, A.; van der Steen, B.; Bloemena, E.; Koljenović, S.; Baatenburg de Jong, R.J.; Leemans, C.R.; Brakenhoff, R.H. The unveiled reality of human papillomavirus as risk factor for oral cavity squamous cell carcinoma. Int. J. cancer 2021, 149, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Anzai, Y.; Brizel, D.M.; Bruce, J.Y.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J.; et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Lydiatt, W.M.; Patel, S.G.; O’Sullivan, B.; Brandwein, M.S.; Ridge, J.A.; Migliacci, J.C.; Loomis, A.M.; Shah, J.P. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 122–137. [Google Scholar] [CrossRef]
- Bryant, A.K.; Sojourner, E.J.; Vitzthum, L.K.; Zakeri, K.; Shen, H.; Nguyen, C.; Murphy, J.D.; Califano, J.A.; Cohen, E.E.; Mell, L.K. Prognostic role of p16 in nonoropharyngeal head and neck cancer. JNCI J. Natl. Cancer Inst. 2018, 110, 1393–1399. [Google Scholar] [CrossRef]
- Mariz, B.; Kowalski, L.P.; William, W.N., Jr.; de Castro, G., Jr.; Chaves, A.L.F.; Santos, M.; de Oliveira, T.B.; Araujo, A.L.D.; Normando, A.G.C.; Ribeiro, A.C.P.; et al. Global prevalence of human papillomavirus-driven oropharyngeal squamous cell carcinoma following the ASCO guidelines: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2020, 156, 103116. [Google Scholar] [CrossRef]
- Arsa, L.; Siripoon, T.; Trachu, N.; Foyhirun, S.; Pangpunyakulchai, D.; Sanpapant, S.; Jinawath, N.; Pattaranutaporn, P.; Jinawath, A.; Ngamphaiboon, N. Discrepancy in p16 expression in patients with HPV-associated head and neck squamous cell carcinoma in Thailand: Clinical characteristics and survival outcomes. BMC Cancer 2021, 21, 504. [Google Scholar] [CrossRef]
- Spector, M.E.; Farlow, J.L.; Haring, C.T.; Brenner, J.C.; Birkeland, A.C. The potential for liquid biopsies in head and neck cancer. Discov. Med. 2018, 25, 251. [Google Scholar]
- Balachandra, S.; Kusin, S.B.; Lee, R.; Blackwell, J.M.; Tiro, J.A.; Cowell, L.G.; Chiang, C.M.; Wu, S.Y.; Varma, S.; Rivera, E.L. Blood-based biomarkers of human papillomavirus–associated cancers: A systematic review and meta-analysis. Cancer 2021, 127, 850–864. [Google Scholar] [CrossRef]
- Economopoulou, P.; Koutsodontis, G.; Avgeris, M.; Strati, A.; Kroupis, C.; Pateras, I.; Kirodimos, E.; Giotakis, E.; Kotsantis, I.; Maragoudakis, P. HPV16 E6/E 7 expression in circulating tumor cells in oropharyngeal squamous cell cancers: A pilot study. PLoS ONE 2019, 14, e0215984. [Google Scholar] [CrossRef]
- Geraldine, O.; Wang, L.; Zlott, J.; Juwara, L.; Covey, J.M.; Beumer, J.H.; Cristea, M.C.; Newman, E.M.; Koehler, S.; Nieva, J.J. Intravenous 5-fluoro-2′-deoxycytidine administered with tetrahydrouridine increases the proportion of p16-expressing circulating tumor cells in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2020, 85, 979–993. [Google Scholar]
- Lefevre, A.C.; Pallisgaard, N.; Kronborg, C.; Wind, K.L.; Krag, S.R.P.; Spindler, K.G. The Clinical Value of Measuring Circulating HPV DNA during Chemo-Radiotherapy in Squamous Cell Carcinoma of the Anus. Cancers 2021, 13, 2451. [Google Scholar] [CrossRef] [PubMed]
- Asante, D.-B.; Calapre, L.; Ziman, M.; Meniawy, T.M.; Gray, E.S. Liquid biopsy in ovarian cancer using circulating tumor DNA and cells: Ready for prime time? Cancer Lett. 2020, 468, 59–71. [Google Scholar] [CrossRef] [PubMed]
- McShane, L.M.; Altman, D.G.; Sauerbrei, W.; Taube, S.E.; Gion, M.; Clark, G.M. Reporting recommendations for tumor marker prognostic studies (REMARK). J. Natl. Cancer Inst. 2005, 97, 1180–1184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsen, C.G.; Gyldenløve, M.; Jensen, D.; Therkildsen, M.; Kiss, K.; Norrild, B.; Konge, L.; Von Buchwald, C. Correlation between human papillomavirus and p16 overexpression in oropharyngeal tumours: A systematic review. Br. J. Cancer 2014, 110, 1587–1594. [Google Scholar] [CrossRef] [PubMed]
- Su, P.-J.; Wu, M.-H.; Wang, H.-M.; Lee, C.-L.; Huang, W.-K.; Wu, C.-E.; Chang, H.-K.; Chao, Y.-K.; Tseng, C.-K.; Chiu, T.-K. Circulating tumour cells as an independent prognostic factor in patients with advanced oesophageal squamous cell carcinoma undergoing chemoradiotherapy. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef]
- Hsieh, J.C.; Lin, H.C.; Huang, C.Y.; Hsu, H.L.; Wu, T.M.; Lee, C.L.; Chen, M.C.; Wang, H.M.; Tseng, C.P. Prognostic value of circulating tumor cells with podoplanin expression in patients with locally advanced or metastatic head and neck squamous cell carcinoma. Head Neck 2015, 37, 1448–1455. [Google Scholar] [CrossRef]
- Liao, C.J.; Hsieh, C.H.; Hung, F.C.; Wang, H.M.; Chou, W.P.; Wu, M.H. The Integration of a Three-Dimensional Spheroid Cell Culture Operation in a Circulating Tumor Cell (CTC) Isolation and Purification Process: A Preliminary Study of the Clinical Significance and Prognostic Role of the CTCs Isolated from the Blood Samples of Head and Neck Cancer Patients. Cancers 2019, 11, 783. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.Y.; Fu, J.Y.; Wu, C.F.; Hsieh, M.J.; Liu, Y.H.; Liu, H.P.; Hsieh, J.C.; Peng, Y.T. Malignancy Prediction Capacity and Possible Prediction Model of Circulating Tumor Cells for Suspicious Pulmonary Lesions. J. Pers. Med. 2021, 11, 444. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Lee, C.-L.; Wu, C.-F.; Fu, J.-Y.; Yang, C.-T.; Wen, C.-T.; Liu, Y.-H.; Liu, H.-P.; Hsieh, J.C.-H. Circulating Tumor Cells as a Tool of Minimal Residual Disease Can Predict Lung Cancer Recurrence: A longitudinal, Prospective Trial. Diagnostics 2020, 10, 144. [Google Scholar] [CrossRef] [Green Version]
- Ikoma, D.; Ichikawa, D.; Ueda, Y.; Tani, N.; Tomita, H.; Sai, S.; Kikuchi, S.; Fujiwara, H.; Otsuji, E.; Yamagishi, H. Circulating tumor cells and aberrant methylation as tumor markers in patients with esophageal cancer. Anticancer. Res. 2007, 27, 535–539. [Google Scholar]
- Zhang, X.; Li, H.; Yu, X.; Li, S.; Lei, Z.; Li, C.; Zhang, Q.; Han, Q.; Li, Y.; Zhang, K. Analysis of circulating tumor cells in ovarian cancer and their clinical value as a biomarker. Cell. Physiol. Biochem. 2018, 48, 1983–1994. [Google Scholar] [CrossRef]
- Kulasinghe, A.; Kapeleris, J.; Kimberley, R.; Mattarollo, S.R.; Thompson, E.W.; Thiery, J.P.; Kenny, L.; O’Byrne, K.; Punyadeera, C. The prognostic significance of circulating tumor cells in head and neck and non-small-cell lung cancer. Cancer Med. 2018, 7, 5910–5919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tada, H.; Takahashi, H.; Kuwabara-Yokobori, Y.; Shino, M.; Chikamatsu, K. Molecular profiling of circulating tumor cells predicts clinical outcome in head and neck squamous cell carcinoma. Oral Oncol. 2020, 102, 104558. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.M.; Wu, M.H.; Chang, P.H.; Lin, H.C.; Liao, C.D.; Wu, S.M.; Hung, T.M.; Lin, C.Y.; Chang, T.C.; Tzu-Tsen, Y. The change in circulating tumor cells before and during concurrent chemoradiotherapy is associated with survival in patients with locally advanced head and neck cancer. Head Neck 2019, 41, 2676–2687. [Google Scholar] [CrossRef] [PubMed]
- Garrel, R.; Mazel, M.; Perriard, F.; Vinches, M.; Cayrefourcq, L.; Guigay, J.; Digue, L.; Aubry, K.; Alfonsi, M.; Delord, J.-P. Circulating tumor cells as a prognostic factor in recurrent or metastatic head and neck squamous cell carcinoma: The CIRCUTEC prospective study. Clin. Chem. 2019, 65, 1267–1275. [Google Scholar] [CrossRef]
- Ng, S.P.; Bahig, H.; Wang, J.; Cardenas, C.E.; Lucci, A.; Hall, C.S.; Meas, S.; Sarli, V.N.; Yuan, Y.; Urbauer, D.L. Predicting treatment Response based on Dual assessment of magnetic resonance Imaging kinetics and Circulating Tumor cells in patients with Head and Neck cancer (PREDICT-HN): Matching ‘liquid biopsy’and quantitative tumor modeling. BMC Cancer 2018, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cho, J.K.; Lee, G.J.; Kim, H.D.; Moon, U.Y.; Kim, M.J.; Kim, S.; Baek, K.H.; Jeong, H.S. Differential impact of circulating tumor cells on disease recurrence and survivals in patients with head and neck squamous cell carcinomas: An updated meta-analysis. PLoS ONE 2018, 13, e0203758. [Google Scholar] [CrossRef]
- Hsieh, J.C.; Wang, H.M.; Wu, M.H.; Chang, K.P.; Chang, P.H.; Liao, C.T.; Liau, C.T. Review of emerging biomarkers in head and neck squamous cell carcinoma in the era of immunotherapy and targeted therapy. Head Neck 2019, 41 (Suppl S1), 19–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reimers, N.; Kasper, H.U.; Weissenborn, S.J.; Stutzer, H.; Preuss, S.F.; Hoffmann, T.K.; Speel, E.J.; Dienes, H.P.; Pfister, H.J.; Guntinas-Lichius, O.; et al. Combined analysis of HPV-DNA, p16 and EGFR expression to predict prognosis in oropharyngeal cancer. Int. J. Cancer 2007, 120, 1731–1738. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S., Jr.; Thorstad, W.L.; Chernock, R.D.; Haughey, B.H.; Yip, J.H.; Zhang, Q.; El-Mofty, S.K. p16 positive oropharyngeal squamous cell carcinoma: An entity with a favorable prognosis regardless of tumor HPV status. Am. J. Surg. Pathol. 2010, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bigelow, E.O.; Seiwert, T.Y.; Fakhry, C. Deintensification of treatment for human papillomavirus-related oropharyngeal cancer: Current state and future directions. Oral Oncol. 2020, 105, 104652. [Google Scholar] [CrossRef]
- Singhi, A.D.; Westra, W.H. Comparison of human papillomavirus in situ hybridization and p16 immunohistochemistry in the detection of human papillomavirus-associated head and neck cancer based on a prospective clinical experience. Cancer 2010, 116, 2166–2173. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhang, Y.; Bai, W.; Wang, B.; Wei, J.; Ji, R.; Xin, Y.; Dong, L.; Jiang, X. Feasibility of Immunohistochemical p16 Staining in the Diagnosis of Human Papillomavirus Infection in Patients With Squamous Cell Carcinoma of the Head and Neck: A Systematic Review and Meta-Analysis. Front. Oncol. 2020, 10, 524928. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.W.; D’Souza, G. Epidemiology of human papillomavirus-related head and neck cancer. Otolaryngol. Clin. North. Am. 2012, 45, 739–764. [Google Scholar] [CrossRef]
- Dok, R.; Glorieux, M.; Holacka, K.; Bamps, M.; Nuyts, S. Dual role for p16 in the metastasis process of HPV positive head and neck cancers. Mol. Cancer 2017, 16, 113. [Google Scholar] [CrossRef] [Green Version]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tan, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef] [Green Version]
- Wendt, M.; Romanitan, M.; Nasman, A.; Dalianis, T.; Hammarstedt, L.; Marklund, L.; Ramqvist, T.; Munck-Wikland, E. Presence of human papillomaviruses and p16 expression in hypopharyngeal cancer. Head Neck 2014, 36, 107–112. [Google Scholar] [CrossRef]
- Meshman, J.; Wang, P.C.; Chin, R.; John, M.S.; Abemayor, E.; Bhuta, S.; Chen, A.M. Prognostic significance of p16 in squamous cell carcinoma of the larynx and hypopharynx. Am. J. Otolaryngol. 2017, 38, 31–37. [Google Scholar] [CrossRef]
- Dalianis, T.; Grün, N.; Koch, J.; Vlastos, A.; Tertipis, N.; Nordfors, C.; Näsman, A.; Wendt, M.; Romanitan, M.; Bersani, C. Human papillomavirus DNA and p16INK4a expression in hypopharyngeal cancer and in relation to clinical outcome, in Stockholm, Sweden. Oral Oncol. 2015, 51, 857–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lassen, P.; Schou, M.; Overgaard, J.; Alsner, J. Correlation and prognostic impact of human papilloma virus and p16-expression in advanced hypopharynx and larynx cancer treated with definitive radiotherapy. Acta Oncol. 2021, 60, 646–648. [Google Scholar] [CrossRef] [PubMed]




| Characters | n | % |
|---|---|---|
| Age (median, range) in years | 55 (37–74) | |
| Sex | ||
| Female | 8 | 19.5% |
| Male | 33 | 80.5% |
| Tumor type | ||
| Oropharynx | 28 | 68.3% |
| Non-oropharynx a | 13 | 31.7% |
| ECOG PS | ||
| 0–1 | 32 | 78.0% |
| 2 | 9 | 22.0% |
| Tumor stage (AJCC 8th edition) b | ||
| II | 20 | 48.8% |
| III | 5 | 12.2% |
| IV | 16 | 39.0% |
| T classification | ||
| T1-2 | 28 | 68.3% |
| T3-4 | 13 | 31.7% |
| Lymph node Involvement | ||
| Negative (N0) | 11 | 26.8% |
| Positive (N1-3) | 30 | 73.2% |
| p16 status by IHC staining | 0.0% | |
| Negative (0–70%) | 22 | 53.7% |
| Positive (>70%) | 19 | 46.3% |
| CCRT completion | 41 | 100.0% |
| Disease Progression after CCRT | ||
| No | 19 | 46.3% |
| Yes | 22 | 53.7% |
| Cancer-related death c | ||
| No | 27 | 65.9% |
| Yes | 14 | 34.1% |
| Circulating tumor cells (CTCs) detection rate | ||
| p16-positive CTCs (p16posEpCAMposHoechstpos) | 21 | 51.2% |
| p16-negative CTCs (p16negEpCAMposHoechstpos) d | 20 | 48.8% |
| Tissue IHC p16 Negative | Tissue IHC p16 Positive | p-Value | Tissue IHC p16 Negative AND HPV Genotyping Negative | Tissue IHC p16 Positive OR HPV Genotyping Positive | p-Value | |
|---|---|---|---|---|---|---|
| p16pos CTC Negative | 13 | 7 | 0.155 | 13 | 7 | 0.019 * |
| p16pos CTC Positive | 9 | 12 | 6 | 15 |
| Progression-Free Survival | Overall Survival | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis * | |||||||||
| Factors | p | HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) |
| Age | 0.135 | 0.957 | (0.904–1.014) | 0.003 | 0.909 | (0.852–0.969) | 0.338 | 0.973 | (0.920–1.029) | |||
| Sex (female vs. male) | 0.262 | 2.328 | (0.532–10.195) | 0.371 | 1.967 | (0.447–8.659) | ||||||
| Tumor type (ORX vs. non-ORX) | 0.924 | 0.95 | (0.334–2.707) | 0.415 | 1.524 | (0.553–4.198) | ||||||
| T classification (cT1-2 vs. cT3-4) | 0.975 | 0.985 | (0.374–2.592) | 0.548 | 1.350 | (0.506–3.600) | ||||||
| N classification | 0.421 | 1.214 | (0.758–1.944) | 0.968 | 0.991 | (0.624–1.574) | ||||||
| ECOG PS | 0.171 | 0.377 | (0.093–1.523) | 0.248 | 0.439 | (0.109–1.775) | ||||||
| Best response of CCRT (Non-responders vs. responders) | 0.104 | 1.535 | (0.916–2.573) | 0.038 | 1.738 | 1.031–2.927 | 0.114 | 1.499 | (0.907–2.475) | |||
| Tissue p16 IHC (Positive vs. negative) | 0.099 | 0.415 | (0.146–1.180) | 0.369 | 0.629 | (0.228–1.731) | ||||||
| p16neg CTC (Positive vs. negative) | 0.005 | 4.029 | (1.522–10.668) | 0.003 | 5.497 | 1.818–16.615 | 0.029 | 3.037 | (1.123–8.213) | |||
| p16pos CTC (Positive vs. negative) | 0.018 | 0.300 | (0.110–0.816) | 0.003 | 0.176 | 0.056–0.554 | 0.024 | 0.294 | (0.102–0.852) | 0.024 | 0.294 | (0.102–0.852) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, P.-H.; Wang, H.-M.; Kuo, Y.-C.; Lee, L.-Y.; Liao, C.-J.; Kuo, H.-C.; Hsu, C.-L.; Liao, C.-T.; Lin, S.H.-C.; Huang, P.-W.; et al. Circulating p16-Positive and p16-Negative Tumor Cells Serve as Independent Prognostic Indicators of Survival in Patients with Head and Neck Squamous Cell Carcinomas. J. Pers. Med. 2021, 11, 1156. https://doi.org/10.3390/jpm11111156
Chang P-H, Wang H-M, Kuo Y-C, Lee L-Y, Liao C-J, Kuo H-C, Hsu C-L, Liao C-T, Lin SH-C, Huang P-W, et al. Circulating p16-Positive and p16-Negative Tumor Cells Serve as Independent Prognostic Indicators of Survival in Patients with Head and Neck Squamous Cell Carcinomas. Journal of Personalized Medicine. 2021; 11(11):1156. https://doi.org/10.3390/jpm11111156
Chicago/Turabian StyleChang, Pei-Hung, Hung-Ming Wang, Yung-Chia Kuo, Li-Yu Lee, Chia-Jung Liao, Hsuan-Chih Kuo, Cheng-Lung Hsu, Chun-Ta Liao, Sanger Hung-Chi Lin, Pei-Wei Huang, and et al. 2021. "Circulating p16-Positive and p16-Negative Tumor Cells Serve as Independent Prognostic Indicators of Survival in Patients with Head and Neck Squamous Cell Carcinomas" Journal of Personalized Medicine 11, no. 11: 1156. https://doi.org/10.3390/jpm11111156
APA StyleChang, P.-H., Wang, H.-M., Kuo, Y.-C., Lee, L.-Y., Liao, C.-J., Kuo, H.-C., Hsu, C.-L., Liao, C.-T., Lin, S. H.-C., Huang, P.-W., Wu, T. M.-H., & Hsieh, J. C.-H. (2021). Circulating p16-Positive and p16-Negative Tumor Cells Serve as Independent Prognostic Indicators of Survival in Patients with Head and Neck Squamous Cell Carcinomas. Journal of Personalized Medicine, 11(11), 1156. https://doi.org/10.3390/jpm11111156







