Benefits of Combining Physical Therapy with Occupational Therapy in Hip Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
- the prevention of the muscle atrophy process after immobilization;
- the prophylaxis of osteoporosis onset;
- maintaining muscle tone;
- optimizing breathing;
- improving muscle strength and joint mobility in pain-free circumstances or low pain intensity;
- improving stability in orthostatism and walking;
- no pain/can be ignored (44 points)
- slight, occasional, no compromise in activities (40 points)
- mild, no effect on ordinary activities, rarely moderate pain after unusual activities, uses aspirin (30 points)
- moderate, tolerable, causes some limitations in ordinary activities/work, may require pain medication occasionally that is stronger than aspirin (20 points)
- marked with serious limitations of activities (10 points)
- totally disabled, bedridden patient (0 points)
- none (11 points)
- slight (8 points)
- moderate (5 points)
- severe (0 points)
- unable to walk (0 points)
- none (11 points)
- cane for long walks (7 points)
- cane, full time (5 points)
- crutch (4 points)
- 2 canes (2 points)
- 2 crutches (1 point)
- unable to walk (0 points)
- unlimited (11 points)
- can walk 1 mile (8 points)
- can walk ½ mile (5 points)
- indoors only (2 points)
- from bed to chair (0 points)
- normally without banister (4 points)
- normally with banister (2 points)
- uses the stairs in any manner (1 point)
- not able to use the stairs (0 points)
- with ease (4 points)
- with difficulty (2 points)
- unable (0 points)
- comfortable on any chair, 1 h (5 points)
- on a highchair, ½ h (3 points)
- unable to sit on any chair (0 points)
- able to use public transportation (1)
- unable to use public transportation (0).
Statistical Analysis
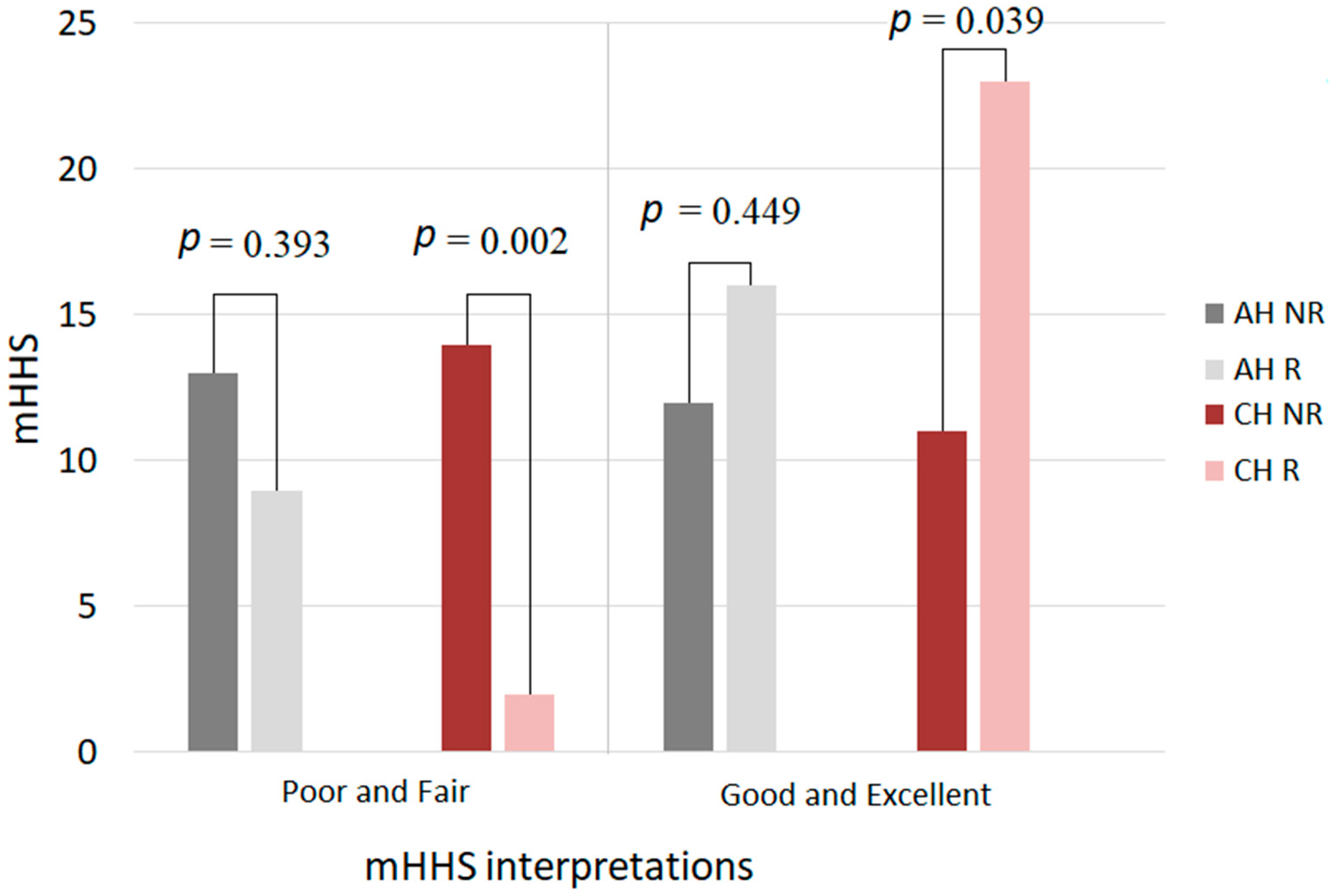
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kasnakova, P.; Ivanova, S.; Ivanov, K.; Petkova-Gueorguieva, E.; Gueorguiev, S.; Madzharov, V.; Mihaylova, A.; Petleshkova, P. Conservative therapy options for the treatment of coxarthrosis in the early stage of the condition. Biomed. Res. 2018, 29, 14. [Google Scholar] [CrossRef] [Green Version]
- Nazal, M.; Parsa, A.; Martin, S.D. Arthroscopic Diagnosis and Treatment of Chronic Hip Pain After Total Hip Arthroplasty and the Role of Anterior Capsule Disruption in Iliopsoas Tendinopathy. Orthop. J. Sports Med. 2019, 7, 2325967119854362. [Google Scholar] [CrossRef]
- Park, K.K.; Tsai, T.-Y.; Dimitriou, D.; Kwon, Y.-M. Three-dimensional in vivo difference between native acetabular version and acetabular component version influences iliopsoas impingement after total hip arthroplasty. Int. Orthop. 2015, 40, 1807–1812. [Google Scholar] [CrossRef] [PubMed]
- Skyttä, E.T.; Jarkko, L.; Antti, E.; Huhtala, H.; Ville, R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients A population based study from the Finnish Arthroplasty Register. Acta Orthop. 2011, 82, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Daras, M.; Macaulay, W. Total hip arthroplasty in young patients with osteoarthritis. Am. J. Orthop. 2009, 38, 125–129. [Google Scholar]
- Koenig, L.; Zhang, Q.; Austin, M.S.; Demiralp, B.; Fehring, T.K.; Feng, C.; Mather, R.C.I.I.I.; Nguyen, J.T.; Saavoss, A.; Springer, B.D.; et al. Estimating the Societal Benefits of THA After Accounting for Work Status and Productivity: A Markov Model Approach. Clin. Orthop. Relat. Res. 2016, 474, 2645–2654. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.-W.; Zi, Y.; Xiang, L.-B.; Wang, Y. Total hip arthroplasty: A review of advances, advantages and limitations. Int. J. Clin. Exp. Med. 2015, 8, 27–36. [Google Scholar]
- Boisgard, S.; Descamps, S.; Bouillet, B. Complex primary total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2013, 99, S34–S42. [Google Scholar] [CrossRef] [Green Version]
- Hwang, S.K. Experience of Complications of Hip Arthroplasty. Hip Pelvis 2014, 26, 207–213. [Google Scholar] [CrossRef]
- Madara, K.C.; Marmon, A.; Aljehani, M.; Hunter-Giordano, A.; Zeni, J.J.; Raisis, L. Progressive rehabilitation after total hip arthoplasty: A pilot and feasibility study. Int. J. Sports Phys. Ther. 2019, 14, 564–581. [Google Scholar] [CrossRef] [Green Version]
- Krastanova, M.S.; Ilieva, E.M.; Vacheva, D.E. Rehabilitation of Patients with Hip Joint Arthroplasty (Late Post-surgery Period—Hospital Rehabilitation). Folia Med. 2017, 59, 217–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnsley, L.; Barnsley, L.; Page, R. Are Hip Precautions Necessary Post Total Hip Arthroplasty? A Systematic Review. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 230–235. [Google Scholar] [CrossRef] [Green Version]
- Tetreault, M.W.; Akram, F.; Li, J.; Nam, D.; Gerlinger, T.L.; Della Valle, C.J.; Levine, B.R. Are Postoperative Hip Precautions Necessary After Primary Total Hip Arthroplasty Using a Posterior Approach? Preliminary Results of a Prospective Randomized Trial. J. Arthroplast. 2020, 35, S246–S251. [Google Scholar] [CrossRef]
- Judd, D.L.; Dennis, D.A.; Thomas, A.C.; Wolfe, P.; Dayton, M.R.; Stevens-Lapsley, J.E. Muscle strength and functional recovery during the first year after THA. Clin. Orthop. Relat. Res. 2014, 472, 654–664. [Google Scholar] [CrossRef] [Green Version]
- Ninomiya KHirakawa, K.; Ikeda, T.; Nakura, N.; Suzuki, K. Patients 10 years after total hip arthroplasty have the deficits in functional performance, physical activity, and high fall rate compared to healthy adults. Phys. Ther. Res. 2018, 21, 53–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czyżewska, A.; Glinkowski, W.M.; Walesiak, K.; Krawczak, K.; Cabaj, D.; Górecki, A. Effects of preoperative physiotherapy in hip osteoarthritis patients awaiting total hip replacement. Arch. Med. Sci. 2014, 10, 985–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coudeyre, E.; Jardin, C.; Givron, P.; Ribinik, P.; Revel, M.; Rannou, F. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann. Réadapt. Méd. Phys. 2007, 50, 189–197. [Google Scholar] [CrossRef]
- Monaco, M.D.; Vallero, F.; Tappero, R.; Cavanna, A. Rehabilitation after total hip arthroplasty: A systematic review of controlled trials on physical exercise programs. Eur. J. Phys. Rehabil. Med. 2009, 45, 303–317. [Google Scholar]
- Vogel, L.A.; Carotenuto, G.; Basti, J.J.; Levine, W.N. Physical Activity after Total Joint Arthroplasty. Sports Health 2011, 3, 441–450. [Google Scholar] [CrossRef] [Green Version]
- Kumar, P.; Sen, R.; Aggarwal, S.; Agarwal, S.; Rajnish, R.K. Reliability of Modified Harris Hip Score as a tool for outcome evaluation of Total Hip Replacements in Indian population. J. Clin. Orthop. Trauma. 2019, 10, 128–130. [Google Scholar] [CrossRef]
- Gupta, L.; Lal, M.; Aggarwal, V.; Rathor, L.P. Assessing functional outcome using modified Harris hip score in patients undergoing total hip replacement. Int. J. Orthop. Sci. 2018, 4, 1015–1017. [Google Scholar] [CrossRef]
- Modified Harris Hip Score. Available online: https://www.losangelessportssurgeon.com/pdf/modified-harris-hip-score.pdf (accessed on 24 September 2021).
- Okafor, L.; Chen, A.F. Patient satisfaction and total hip arthroplasty: A review. Arthroplasty 2019, 1, 6. [Google Scholar] [CrossRef] [Green Version]
- Graham, B.; Green, A.; James, M.; Katz, J.; Swiontkowski, M. Measuring patient satisfaction inorthopaedic surgery. J. Bone Jt. Surg. 2015, 97, 80–84. [Google Scholar] [CrossRef]
- Zagra, L. Advances in hip arthroplasty surgery: What is justified? EFORT Open Rev. 2017, 2, 171–178. [Google Scholar] [CrossRef]
- Hoorntje, A.; Janssen, K.Y.; Bolder, S.B.T.; Koenraadt, K.L.M.; Daams, J.G.; Blankevoort, L.; Kerkhoffs, G.M.M.J.; Kuijer, P.P.F.M. The Effect of Total Hip Arthroplasty on Sports and Work Participation: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 1695–1726. [Google Scholar] [CrossRef] [Green Version]
- Mark-Christensen, T.; Thorborg, K.; Kallemose, T.; Bandholm, T. Physical rehabilitation versus no physical rehabilitation after total hip and knee arthroplasties: Protocol for a pragmatic, randomized, controlled, superiority trial (The DRAW1 trial). F1000Research 2021, 10, 146. [Google Scholar] [CrossRef] [PubMed]
- Bozorgi, A.A.J.B.; Ghamkhar, L.; Kahlaee, A.H.; Sabouri, H. The Effectiveness of Occupational Therapy Supervised Usage of Adaptive Devices on Functional Outcomes and Independence after Total Hip Replacement in Iranian Elderly: A Randomized Controlled Trial. Occup. Ther. Int. 2015, 23, 143–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, T.O.; McCabe, C.; Lister, S.; Christie, S.P.; Cross, J. Rehabilitation implications during the development of the Norwich Enhanced Recovery Programme (NERP) for patients following total knee and total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2012, 98, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.; Orpen, N. Patients’ Perceptions of Preoperative Home-Based Occupational Therapy and/or Physiotherapy Interventions Prior to Total Hip Replacement. Br. J. Occup. Ther. 2010, 73, 461–469. [Google Scholar]
- Paunescu, F.; Didilescu, A.; Antonescu, D.M. Does Physiotherapy Contribute to the Improvement of Functional Results and of Quality of Life after Primary Total Hip Arthroplasty? Maedica 2014, 9, 49–55. [Google Scholar]
- Păunescu, F.; Didilescu, A.; Antonescu, D.M. Factors that may influence the functional outcome after primary total hip arthroplasty. Clujul Med. 2013, 86, 121–127. [Google Scholar] [PubMed]
- Papalia, R.; Campi, S.; Vorini, F.; Zampogna, B.; Vasta, S.; Papalia, G.; Fossati, C.; Torre, G.; Denaro, V. The Role of Physical Activity and Rehabilitation Following Hip and Knee Arthroplasty in the Elderly. J. Clin. Med. 2020, 9, 1401. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Q.; Mao, L.B.; Wu, J. Efficacy of exercise for improving functional outcomes for patients undergoing total hip arthroplasty: A meta-analysis. Medicine 2019, 98, e14591. [Google Scholar] [CrossRef] [PubMed]

| mHHS | AH_B_T0 | AH_B_T1 | CH_B_T0 | CH_B_T1 | AH_A_T0 | AH_A_T1 | CH_A_T0 | CH_A_T1 |
|---|---|---|---|---|---|---|---|---|
| Mean | 61.52 | 80.16 | 74.04 | 81.48 | 71.6 | 83.4 | 66.44 | 76.6 |
| Std. Deviation | 8.75 | 8.63 | 6.33 | 8.397 | 8.01 | 8.902 | 5.86 | 5.708 |
| Std. Error of Mean | 2.749 | 1.726 | 1.267 | 1.679 | 1.601 | 1.78 | 1.172 | 1.842 |
| Lower 95% CI of mean | 63.78 | 76.6 | 77.3 | 78.01 | 74.17 | 79.73 | 79.89 | 84.24 |
| Upper 95% CI of mean | 79.26 | 73.72 | 70.78 | 74.95 | 69.03 | 87.07 | 72.99 | 78.96 |
| D’Agostino and Pearson omnibus normality test | ||||||||
| K2 | 0.2223 | 0.2948 | 0.494 | 0.2387 | 0.7358 | 0.1762 | 0.2194 | 0.8226 |
| p value | 0.6891 | 0.5678 | 0.7812 | 0.6012 | 0.5252 | 0.9121 | 0.8961 | 0.7164 |
| Passed normality test (alpha = 0.05)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| p value summary | ns | ns | ns | ns | ns | ns | ns | ns |
| Shapiro–Wilk normality test | ||||||||
| W | 0.8406 | 0.7971 | 0.9597 | 0.8122 | 0.8774 | 0.9291 | 0.9667 | 0.7174 |
| p value | 0.5012 | 0.6102 | 0.4076 | 0.7904 | 0.8661 | 0.7701 | 0.562 | 0.6745 |
| Passed normality test (alpha = 0.05)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| p value summary | ns | ns | ns | ns | ns | ns | ns | ns |
| KS normality test | ||||||||
| KS distance | 0.2111 | 0.1366 | 0.1303 | 0.1315 | 0.2218 | 0.2833 | 0.1134 | 0.1796 |
| p value | 0.25 | 0.2 | 0.2 | 0.3 | 0.26 | 0.3 | 0.2 | 0.3 |
| Passed normality test (alpha = 0.05)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| p value summary | ns | ns | ns | ns | ns | ns | ns | ns |
| Coefficient of variation (%) | 37.11 | 40.77 | 37.09 | 40.31 | 33.37 | 35.67 | 34.16 | 36.59 |
| DSI_A | BMI_A | DSI_B | BMI_B | |
|---|---|---|---|---|
| Mean | 11.52 | 27.15 | 12.12 | 27.87 |
| Std. Deviation | 3.798 | 3.337 | 3.8 | 3.371 |
| Std. Error of Mean | 0.7596 | 0.6673 | 0.7601 | 0.6741 |
| Lower 95% CI of mean | 9.952 | 25.77 | 10.55 | 26.48 |
| Upper 95% CI of mean | 13.09 | 28.53 | 13.69 | 29.26 |
| D’Agostino and Pearson omnibus normality test | ||||
| K2 | 5.785 | 0.1668 | 2.978 | 0.342 |
| p value | 0.0554 | 0.92 | 0.2256 | 0.8428 |
| Passed normality test (alpha = 0.05)? | Yes | Yes | Yes | Yes |
| p value summary | ns | ns | ns | ns |
| Shapiro–Wilk normality test | ||||
| W | 0.8892 | 0.9822 | 0.9066 | 0.9781 |
| p value | 0.0107 | 0.9253 | 0.0256 | 0.8452 |
| Passed normality test (alpha = 0.05)? | No | Yes | No | Yes |
| p value summary | * | ns | * | ns |
| KS normality test | ||||
| KS distance | 0.2097 | 0.1182 | 0.1915 | 0.09876 |
| p value | 0.006 | 0.2 | 0.0187 | 0.2 |
| Passed normality test (alpha = 0.05)? | No | Yes | No | Yes |
| p value summary | ** | ns | * | ns |
| Coefficient of variation (%) | 32.97 | 12.29 | 31.36 | 12.09 |
| Parameter | Group A | Group B | p | OR | 95% CI |
|---|---|---|---|---|---|
| Age, M, SD | 58.64 ± 6.83 | 59 ± 5.39 | 0.837 * | – | – |
| Female, N (%) | 18 (72%) | 19 (76%) | 0.500 ** | 0.81 | 0.22–2.88 |
| Urban area, N (%) | 22 (88%) | 18 (68%) | 0.144 ** | 2.85 | 0.64–12.64 |
| DSI, M, SD | 11.52 ± 3.80 | 12 ± 3.80 | 0.657 * | – | – |
| BMI, M, SD | 30.53 ± 2.16 | 30 ± 1.80 | 0.350 * | – | – |
| mHHS | |||||
| AH, M, SD | 21.6 ± 18.00 | 21.52 ± 18.74 | 0.987 * | – | – |
| CH, M, SD | 46.44 ± 15.86 | 44.04 ± 16.33 | 0.600 * | – |
| mHHS | Group A | Group B | p |
|---|---|---|---|
| AH | – | ||
| poor result, N, % | 25 (100%) | 25 (100%) | 1 * |
| fair result, N, % | 0 (0%) | 0 (0%) | – |
| good result, N, % | 0 (0%) | 0 (0%) | – |
| excellent result, N, % | 0 (0%) | 0 (0%) | – |
| CH | |||
| poor result, N, % | 23 (92%) | 23 (92%) | 1 * |
| fair result, N, % | 2 (8%) | 2 (8%) | 1 * |
| good result, N, % | 0 (0%) | 0 (0%) | – |
| excellent result, N, % | 0 (0%) | 0 (0%) | – |
| Parameter for AH | Group B | Group A | p |
|---|---|---|---|
| Pain, M, SD | 41.12 ± 1.83 | 42.08 ± 2.03 | 0.027 |
| Function, M, SD | |||
| Limp | 9.44 ± 1.52 | 9.8 ± 1.5 | 0.092 |
| Distance walked Support | 9.56 ± 1.52 | 9.8 ± 1.5 | 0.212 |
| 8.76 ± 2.02 | 9.56 ± 1.95 | 0.028 | |
| Activities, M, SD | |||
| Stairs | 3.04 ± 1.01 | 3.28 ± 0.97 | 0.092 |
| Shoes and socks | 2.88 ± 1.01 | 3.44 ± 0.91 | 0.008 |
| Sitting | 4.36 ± 0.95 | 4.44 ± 0.91 | 0.331 |
| Public transportation | 1 ± 0 | 1 ± 0 | – |
| Parameter for CH | Group B | Group A | p |
|---|---|---|---|
| Pain, M, SD | 41.76 ± 2.03 | 43.52 ± 1.33 | <0.001 |
| Function, M, SD | |||
| Limp | 9.56 ±1.53 | 10.52 ± 1.12 | 0.004 |
| Distance walked Support | 9.56 ± 1.53 | 9.8 ± 1.50 | 0.212 |
| 8.76 ± 2.03 | 9.56 ± 1.96 | 0.028 | |
| Activities, M, SD | |||
| Stairs | 2.96 ± 1.02 | 3.28 ± 0.98 | 0.051 |
| Shoes and socks | 3.6 ± 0.82 | 4 ± 0 | 0.010 |
| Sitting | 4.28 ± 0.98 | 4.44 ± 0.92 | 0.212 |
| Public transportation | 1 ± 0 | 1 ± 0 | – |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcu, F.M.; Negrut, N.; Uivaraseanu, B.; Ciubara, A.; Lupu, V.V.; Dragan, F.; Lupu, A.; Ciubara, A.B. Benefits of Combining Physical Therapy with Occupational Therapy in Hip Arthroplasty. J. Pers. Med. 2021, 11, 1131. https://doi.org/10.3390/jpm11111131
Marcu FM, Negrut N, Uivaraseanu B, Ciubara A, Lupu VV, Dragan F, Lupu A, Ciubara AB. Benefits of Combining Physical Therapy with Occupational Therapy in Hip Arthroplasty. Journal of Personalized Medicine. 2021; 11(11):1131. https://doi.org/10.3390/jpm11111131
Chicago/Turabian StyleMarcu, Florin Mihai, Nicoleta Negrut, Bogdan Uivaraseanu, Anamaria Ciubara, Vasile Valeriu Lupu, Felicia Dragan, Ancuta Lupu, and Alexandru Bogdan Ciubara. 2021. "Benefits of Combining Physical Therapy with Occupational Therapy in Hip Arthroplasty" Journal of Personalized Medicine 11, no. 11: 1131. https://doi.org/10.3390/jpm11111131
APA StyleMarcu, F. M., Negrut, N., Uivaraseanu, B., Ciubara, A., Lupu, V. V., Dragan, F., Lupu, A., & Ciubara, A. B. (2021). Benefits of Combining Physical Therapy with Occupational Therapy in Hip Arthroplasty. Journal of Personalized Medicine, 11(11), 1131. https://doi.org/10.3390/jpm11111131







